Abstract
The optimal management strategy for patent ductus arteriosus in preterm infants remains a topic of debate. Available evidence for a treatment strategy might be biased by the delayed spontaneous closure of the ductus arteriosus in preterm infants, which appears to depend on patient characteristics. We performed a systematic review of all literature on PDA studies to collect patient characteristics and reported numbers of patients with a ductus arteriosus and spontaneous closure. Spontaneous closure rates showed a high variability but were lowest in studies that only included preterm infants with gestational ages below 28 weeks or birth weights below 1,000 g (34% on day 4; 41% on day 7) compared to studies that also included infants with higher gestational ages or higher birth weights (up to 55% on day 3 and 78% on day 7). The probability of spontaneous closure of the ductus arteriosus keeps increasing until at least 1 week after birth which favors delayed treatment of only those infants that do not show spontaneous closure. Better prediction of the spontaneous closure of the ductus arteriosus in the individual newborn is a key factor to find the optimal management strategy for PDA in preterm infants.
Keywords: patent ductus arteriosus, spontaneous closure, preterm infants, systematic review, VLBW, ELBW
Introduction
After preterm birth, the ductus arteriosus often remains open. Patent ductus arteriosus (PDA) in preterm infants has been associated with prolonged ventilation, bronchopulmonary dysplasia (BPD), and necrotizing enterocolitis potentially caused by pulmonary overcirculation and systemic hypoperfusion (1). It is unclear if these associations reflect a causal relationship or if PDA is a marker of poor condition and outcome, because outcomes of well-designed and controlled trials are still awaited (2). Treatment options include fluid restriction, pharmacological intervention with non-steroidal anti-inflammatory drugs (NSAIDs) or paracetamol, or closing the duct by surgical ligation or heart catheterization. All of these therapeutic options have their side-effects or specific risks in preterm infants. As a consequence, there is an ongoing worldwide discussion about the optimal management of PDA in preterm infants (3). This discussion is complicated by the lack of extensive knowledge on the (patho)physiology of the ductus arteriosus in preterm infants.
Intrauterine, the ductus arteriosus is needed and remains open due to the hypoxic fetal environment and by prostaglandins E2 (PGE2) produced by the placenta (4). Vasodilatation is further enhanced by nitric oxide (NO) produced by the wall of the ductus arteriosus (5). Upon term birth, the ductus arteriosus normally closes within hours. This is the result of different complex physiologic mechanisms that include changes in pulmonary and systemic vascular resistance, increase in arterial oxygen pressure, decreasing levels of prostaglandins and changes in different mediators and growth factors (6). After preterm birth, however, the ductus arteriosus frequently remains patent. Even after functional closure of the ductus arteriosus, either spontaneous or by pharmacological treatment, it might re-open in preterm infants afterwards caused by infection or increased inflammation (7).
Although the high levels of prostaglandins produced by the placenta also drop after preterm birth, the ductus arteriosus seems to remain much more sensitive to both PGE2 and NO in preterm infants compared to term born infants, due to increased expression of—and binding to—prostaglandin receptors in the ductal wall (5, 8). In addition to that, oxygenation and vascular resistance after preterm birth are hampered by an immature cardiovascular system and insufficient breathing whereas oxygen targets are decreased to prevent retinopathy of prematurity (9).
A substantial part of the preterm infants with PDA still seems to show delayed ductus closure without any intervention (10). The advantage of a wait-and-see PDA treatment strategy above intervention in the 1st days after birth (<72 h) may be that only those newborns without spontaneous ductus arteriosus closure are exposed to treatment and its potential side effects. On the other hand, early treatment strategy may be favored because the pharmacological closure rate seems to be highest on the 1st days of life (11, 12). Despite the limited studies on delayed treatment with NSAIDs and paracetamol, this late treatment seems less effective (13, 14). NSAIDs and paracetamol may enhance the spontaneous closure process. Therefore, the discussion on management of PDA in preterm infants cannot neglect the spontaneous closure, although a clear overview of the spontaneous closure rates is yet lacking. In this study, we aimed to provide such an overview of all available data from PDA studies to investigate and analyze the rates of spontaneous closure of the PDA.
Methods
To retrieve all relevant evidence on the physiological spontaneous ductus arteriosus closure in preterm infants, we performed a thorough literature search. All studies published after 1990 that met both of the following criteria were considered eligible: (1) trials of any form including randomized controlled trials (RCTs), controlled clinical trials, quasi experimental studies [(un)controlled before and after studies], prospective and retrospective cohort studies and case-control studies and (2) trials with a clearly described timing of echocardiography to identify the presence or absence of a ductus arteriosus. Case series and case reports were excluded, as well as studies that reported on spontaneous closure after discharge. To examine spontaneous closure of the PDA, data on spontaneous closure before any intervention were collected and analyzed.
Search Strategy
A literature search was performed in collaboration with an experienced librarian. The search was done in MEDLINE, EMBASE, Cochrane central, Web of science, and Google Scholar until 2018 and included only English written articles. The following search terms were used “patent ductus arteriosus,” “PDA,” “preterm,” “VLBW,” and/or “prematurity.” A more detailed search strategy for each library is available in Supplementary File 1.
The retrieved titles, abstracts, and full text were screened by two independent reviewers (JdK and FvB) to assess their eligibility according to pre-established criteria. Duplicate publications were excluded. The data extraction was done by the same two independent reviewers (JdK and FvB). Discrepancies were either resolved by discussion or by consulting a third reviewer (SS).
Data Synthesis
We developed a data extraction sheet, pilot-tested it on 10 randomly-selected included studies, and refined it accordingly. One review author (JdK) extracted the following data from included studies and the second author (FvB) checked the extracted data. Disagreements were resolved by discussion between the two review authors; if no agreement could be reached, it was planned a third author (SS) would decide. The data that was used included the following: total number of included neonates, their gestational age and birth weight, timing of the echocardiographic evaluation, and the number of neonates with closed ductus arteriosus at those times. Because only baseline reports of the occurrence of PDA were included, before any intervention for PDA was initiated, no bias of individual studies was expected.
Articles were categorized based on the inclusion criteria that were used in the studies for gestational age (GA) and birth weight (BW). Based on frequently used inclusion cut-off values of GA and BW, four different groups were defined prior to data collection: group 1: GA < 28 weeks and/or BW < 1,000 g, group 2: GA < 30 weeks and/or BW < 1,250 g, group 3: GA < 32 weeks and/or BW < 1,500 g, and group 4: GA < 37 weeks and/or BW < 2,500 g. If only GA or BW was given as inclusion criterion, this determined the category of the article, if both GA and BW were given as inclusion criteria, GA was leading for categorization. Studies were only included in one group: those included in group 1 were not included in groups 2–4, studies in group 2 were not included in group 3 and 4, and studies in group 3 were not included in group 4.
Data Analysis
The primary outcome of this systematic review was the rate of spontaneous closure of the ductus arteriosus in preterm infants as evaluated by echocardiography. A closed ductus arteriosus is defined as a ductus arteriosus that shows complete closure or no doppler flow on echocardiography as reported in the original reports. The closure rate was calculated as the part of patients with a closed ductus within a certain cohort (number of patients with a closed ductus divided by the total number of patients) at a time-point. To further explore how the observed trends were correlated to the maturational status of the patient, different subgroup analyses were performed for the different GA and BW groups.
R Software (V 3.5.1) was used in R Studio (V 1.1.643) to group, summarize, and visualize the data. The percentage of patients with PDA was plotted against postnatal age. To differentiate spontaneous closure between the different GA and BW groups, a linear smoothed line weighted by the total number of patients of each study was drawn. Mean percentages of patients with PDA of studies that performed an echocardiography on postnatal day 3 (between 72 and 95.9 h) and day 7 (between 168 and 191.9 h) were calculated, and were weighted by the number of patients in each study. These time-points were included because the ductus is mostly evaluated during the 1st days of life (<72 h) and administered courses of pharmacotherapy normally take 3 or 6 days.
Results
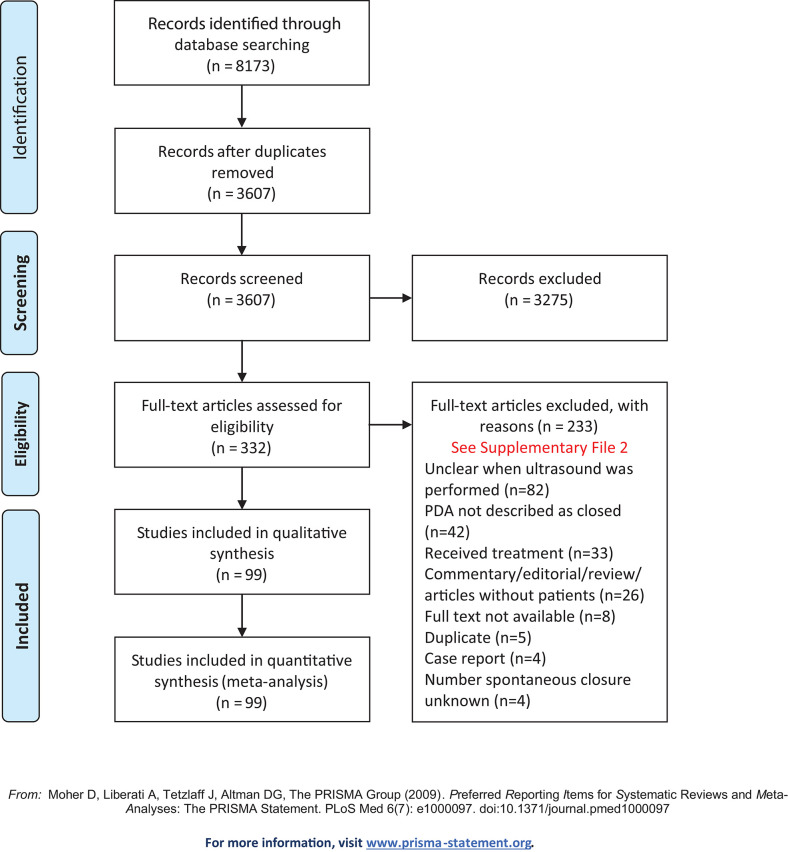
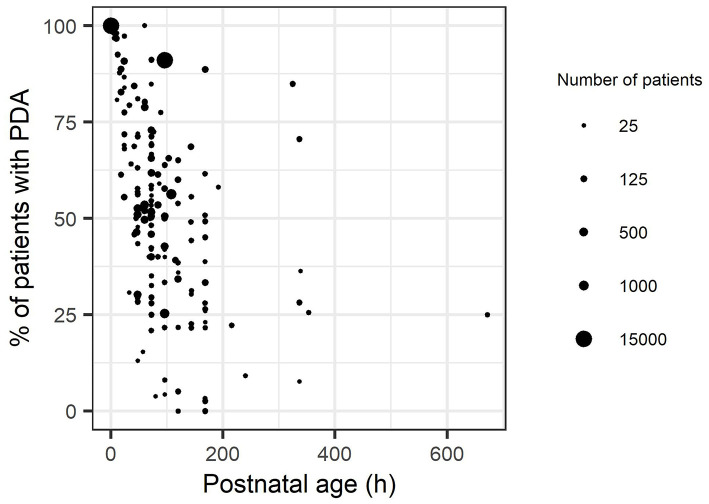
Our literature search resulted in a retrieval of 8,173 records. After removing the duplicates 3,607 remained. Reading of the titles and abstracts resulted in 332 eligible articles. The arguments for exclusion of 233 articles after full text screening are listed in Supplementary File 2. The clinical characteristics of the included studies are summarized in Supplementary File 3. All studies were published between 1990 and 2018. Ninety-nine articles with a total of 29,532 patients were included in the analysis. In Figure 1, a flow diagram is presented of the studies retrieved for this review. Figure 2 presents the reported percentages of patients with a PDA for each individual study with increasing postnatal ages. On PNA day 3 (all reported outcomes observed between 72 and 96 h of life), the mean reported percentage of patients that experienced spontaneous closure of the ductus arteriosus weighted by the number of patients was 47% (range 9–96%). On PNA day 7 (168–192 h) this percentage increased to 61% (11–100%).
Figure 1.
Flow diagram of the studies retrieved for this review.
Figure 2.
Reported percentages of closure of patent ductus arteriosus of all included studies, up to a postnatal age of 28 days. Each dot represents a reported percentage, whose size represents the square root of the total number of patients of that observation.
Subgroup Analysis
In Table 1, the reported characteristics of all studies are presented per group, as well as the percentages of PDA closure at postnatal age days 3 and 7 and the studies and number of patients these are based on.
Table 1.
Summary of reported mean or median gestational age and birthweight of the included studies, and reported percentages of PDA closure at postnatal age days 3 and 7.
| Group 1 | Group 2 | Group 3 | Group 4 | All studies | |
|---|---|---|---|---|---|
| Inclusion criteria | GA < 28 weeks and/or birth weight <1,000 g | GA < 30 weeks and/or birth weight <1,250 g | GA < 32 weeks and/or birth weight <1,500 g | GA < 37 weeks and/or birth weight <2,500 g | |
| Number of studies | 11 | 20 | 49 | 19 | 99 |
| Total number of patients | 17,156 | 2,980 | 6,946 | 2,450 | 29,532 |
| Gestational Age | |||||
| Mean (weeks) [median (range)] (n) | 26.0 [25.5–26.6] (8) | 28.0 [26.2–28.8] (13) | 28.4 [26.0–30.0] (22) | 30.8 [30.2–31.1] (7) | 28.1 [25.5–31.2] (50) |
| Median [median (range)] | – | 28.0 [–] (2) | 29 [27–31] (15) | 31.0 [28.1–31.0] (5) | 29.0 [27.0–31.0] (22) |
| Not reported (n) | 3 | 5 | 12 | 7 | 27 |
| Birth weight | |||||
| Mean [median (range)] | 818 [802–851] (8) | 1,028 [(797–1,259] (13) | 112 [794–1,371] (22) | 1,543 [1,355–1,917] (7) | 1,082 [794–1,917] (50) |
| Median [median (range)] | – | 1,060–1,062 (2) | 1,160 [980–1,595] (15) | 1,475 [950–1,640] (5) | 1,160 [950–1,640] (22) |
| Not reported (n) | 3 | 5 | 12 | 7 | 27 |
| Postnatal age of cardiac ultrasound | |||||
| Median postnatal age in h (range) | 72 (18–1,464) | 72 (5–672) | 79 (6–3,864) | 72 (24–1,632 | 72 (5–3,864) |
| Percentage of PDA closure at postnatal age 3 (72–95.9 h) | |||||
| Weighted mean percentage of patients with PDA (range) | 34% (9–71) | 47% (33–98) | 48% (22–65) | 55% (15–79) | 47% (9–96) |
| Number of studies with reported percentage | 6 | 9 | 16 | 8 | 39 |
| Total number of patients | 646 | 978 | 1,709 | 621 | 3,954 |
| Study references | (15–20) | (21–29) | (30–45) | (46–53) | (15–53) |
| Percentage of PDA closure at postnatal age 7 (168–191.9 h) | |||||
| Weighted mean percentage of patients with PDA (range) | 41% (11–97) | 77 % (–) | 63% (38–100) | 78% (67–97) | 61% (11–100) |
| Number of studies with reported percentage | 2 | 1 | 8 | 5 | 16 |
| Total number of patients | 228 | 26 | 550 | 181 | 985 |
| Study references | (18, 54) | (24) | (30, 33, 43, 55–59) | (46, 50, 60–62) | (18, 24, 30, 33, 43, 46, 50, 54–62) |
Separated by groups based on inclusion criteria.
Eleven different articles were included in group 1 which contained preterm infants with a gestational age under 28 weeks and/or birth weight under 1,000 g (15–20, 54, 63–66). The median of reported mean or median GAs of the 17,156 patients in group 1 was 26.0 (range of mean/median 25.5–26.6) weeks. The median birth weight was 832 (range of medians 802–851) g. Exact numbers for gestational ages and birth weights were not available for three studies (19, 63, 66). Two of the 11 studies performed multiple cardiac ultrasounds to evaluate the PDA, ranging from 24 h until 61 days of postnatal age (15, 18). Seven of the 11 studies performed their first ultrasound at day 3 after birth.
Twenty articles were included in group 2 (GA < 30 weeks and/or BW < 1,250 g) (11, 21–29, 67–76). The median of the reported mean or median GA of the 2,980 patients in group 2 was 28.0 (range 26.2–28.8). The median of the reported mean or median birth weight was 1,028 (range 797–1,259) g. The exact gestational ages and birth weights were not available for four studies (28, 29, 69, 74). Seven of the 20 studies performed multiple cardiac ultrasounds to evaluate the PDA (21, 24, 25, 27, 67, 72, 73). The echocardiography was performed between 5 h and 28 days of postnatal age in all studies.
Forty-nine studies that included a total of 6,946 patients were eligible for group 3 (GA < 32 weeks and/or BW < 1,500 g) (30–45, 55–59, 77–103, 132). The median GA was 28.6 (range 26–31) weeks. The median birth weight was 1,120 (range 794–1,595) g. Exact gestational ages and birth weights were not available for nine studies (35, 38, 41, 42, 44, 85, 96, 100, 104). Multiple cardiac ultrasounds where performed in 14 of the 49 studies and were performed between 6 and 338 h of postnatal age.
Nineteen studies used GA < 37 weeks and/or birthweight < 2,500 g as inclusion criteria (group 4), in which a total of 2,450 patients were included (46–53, 60–62, 105–112). The median gestational age was 30.9 (range 28.1–31.2) weeks. The median birth weight was 1,479 (range 950–1,917) g. Gestational ages and/or birth weights were not available for six studies (47, 50, 53, 105, 107, 109). Six of the 19 studies performed multiple cardiac ultrasounds at varying post-natal ages between 24 and 168 h.
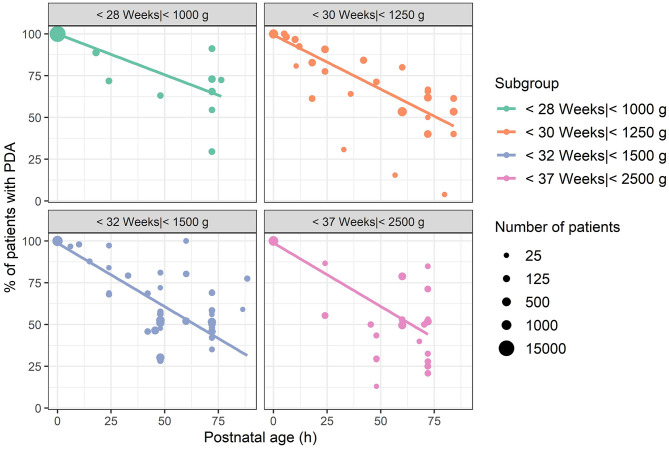
In Figures 3 and 4 the reported percentage of preterm infants with PDA are presented for each subgroup with a postnatal age up to 3 and 7 days, respectively. To account for the large differences in number of patients (range 18–15,971), the size of the dots is scaled by the square root of the number of patients. At postnatal age day 3 (72–95.9 h), mean percentage of PDA closure was 34% for group 1, weighted by the number of patients in each study (range 9–71%). In group 2, this percentage was 47% (33–98%), and in group 3 this was 48% (22–65%). In group 4, the weighted mean was 55% at PNA 3 (15–97%).
Figure 3.
Reported percentages of patients with patent ductus arteriosus up to a postnatal age of 4 days, grouped by mean or median gestational age or birthweight if gestational age was unreported. Each dot represents one observation at the reported postnatal age. The size of the dots represents square root of the number of patients of each observation. Lines represent a linear smooth weighted by the number of patients of each observation.
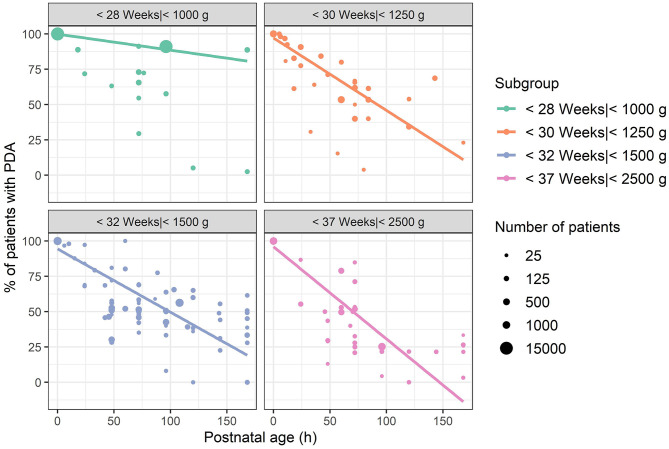
Figure 4.
Reported percentages of patients with patent ductus arteriosus up to a postnatal age of 8 days, grouped by mean or median gestational age or birthweight if gestational age was unreported. Each dot represents one observation at the reported postnatal age. The size of the dots represents square root of the number of patients of each observation. Lines represent a linear smooth weighted by the number of patients of each observation.
At PNA 7, the weighted average of patients with a closed PDA was 41% for group 1 (11–97%). Of group 2, only one study was available with a reported percentage of closure at PNA 7, which was 77% (20 of 26 patients) (24). In group 3, the weighted average closure was 63% (38–100%) at PNA day 7, and for group 4 this was 78% (67–97%). Comparing Figures 2–4 clearly show that with increasing postnatal ages the spontaneous closure continuous and PDA rates decrease. This is most obvious in the studies that also included the oldest groups of infants.
Discussion
In this review, spontaneous closure rates of the ductus arteriosus in preterm neonates were systematically evaluated in 99 studies that represented 29,532 patients. As expected, we observed increasing rates of ductus closure with post-natal age and higher spontaneous closure rates in studies that also included patients with higher gestational ages. Spontaneous closure, however, occurs not only in the 1st day of life, but continues throughout the 1st week of life. Our systematic review revealed 34% spontaneous closure on the 3rd day of life (72–96 h) in the studies that only included the youngest group of infants (<28 weeks of GA and/or birthweight <1,000 g). If older infants were also included in studies, these closure rates increased up to 55%. At PNA day 7 (168–192 h) the ductus arteriosus was closed in 41% of the newborns in studies of the youngest infants and up to 78% in the studies that also included older gestational age groups. Because of a lack of detailed reports in the individual studies on subgroups of patients and the lack of longitudinal assessment of the ductus arteriosus we were unable to provide a mathematical function of spontaneous ductus closure in preterm infants. Such a function that could predict spontaneous closure in an individual patient would be an ultimate goal to guide PDA management in individual patients. High quality datasets with repeated echocardiographic assessments of neonatal patients treated in current neonatal intensive care units are needed first.
Studies that reported on PDA showed large heterogeneity, not only in included patient populations, but also in the definition of a hemodynamically significant PDA (hsPDA) (113). It is quite clear that the significance of a PDA is not only determined by the diameter of the ductus, as was used in the current review, but also by the pulmonary vascular resistance. The lack of consensus on the definition of a hsPDA is partly based on the lack of validated echocardiographic markers and cutoff values. van Laere et al. (114) proposed to standardize essential echocardiographic measurements for the assessment of hemodynamic significance of a PDA. These consist of evaluation of the ductus arteriosus itself (including the diameter, flow direction, and velocity), indices of pulmonary overcirculation (La:Ao, left pulmonary artery diastolic flow) and indices of systemic shunt effect (flow pattern in aorta descendens, tructus coeliacus, or middle cerebral artery) (114). The LA:Ao ratio, ductal diameter and diastolic flow in the left pulmonary artery are easy to measure and seem the most accurate and easy to determine markers for a hsPDA (115). In our aim to select those infants that would not show spontaneous closure and might actually need PDA treatment these markers would be useful.
Currently, there is no international consensus on PDA management. It is unclear if, how and when PDA in preterm infants should be treated. More specifically, it is unclear if PDA needs treatment because it is unknown which preterm infants might benefit more from treatment than others. Therefore, prophylaxis, early treatment (<24 h), late treatment (72 h), symptomatic treatment and wait and see strategies are currently used alongside each other (116). Better knowledge on the spontaneous closure and physiology of the ductus arteriosus in preterm infants may help to determine the optimal management strategy. This is even more important as prophylactic as well as therapeutic treatment strategies are associated with risks for adverse effects, such as intraventricular hemorrhages and decreased renal function that might have severe consequences in these vulnerable patients. Treatment of the PDA, pharmacologically or surgically, should therefore be reserved for those patients who may benefit from it.
Next to the ongoing discussion on the type of drug being either ibuprofen, indomethacin, or acetaminophen (117–124), the timing of treatment initiation varies widely between studies, and might explain reported differences in efficacy. As spontaneous ductus closure increases with PNA, part of ductus closure reported in prophylactic and early treatment studies may be due to spontaneous closure rather than drug treatment. Efficacy of PDA pharmacotherapy seems to decrease, with post-natal age, even if dosages are increased with PNA to correct for increased clearance with age (10, 13). This suggests either a certain window of opportunity for PDA treatment during the physiological process that is involved in the spontaneous closure of the ductus arteriosus or the need for higher drug exposures at older ages. Such a window can only be identified if the rate of spontaneous closure is well-characterized, and efficacy studies can correct for the chance of spontaneous closure.
With the current review, we have summarized the evidence that spontaneous closure is less likely to occur in preterm neonates with the lowest gestational ages. Nevertheless, in another significant number of preterm infants the ductus arteriosus although delayed, closes spontaneously within the first 150 h of life. The presented review was limited by the lack of detailed reports of PDA for different gestational age groups in the included studies. While the literature was systematically reviewed we were unfortunately unable to provide statistical analysis due to complexity of outcome data. This also resulted in overlap of patients in the different groups. All studies only had an upper limit of gestational age and/or bodyweight without a lower limit for gestational age/weight. As a consequence, the gestational age/weight range of inclusion criteria of the included studies increases from group 1 to 4. Therefore, the actual difference in the occurrence of spontaneous closure between different GA groups is bigger than observed in the present study. As other widely used measures for ductus closure, such as LA:Ao ratio were mostly missing, we defined a closed ductus as a ductus that was visually closed or when there was no doppler flow visible on echocardiography. As discussed previously, a better definition of a hsPDA might be desirable and might lead to a more precise estimation of incidence- and closure-rates. In this study, we presented the relationships between spontaneous closure rate and PNA as linear relationships. In reality, the spontaneous closure rate is probably highest on the 1st day and decreases with an asymptotic shape since in some patients the spontaneous closure will not occur, or the percentage of patients with PDA might even go up if the ductus arteriosus reopens. With the available data, it is not possible to determine whether the reported numbers of PDA at high postnatal ages (Figure 2) are due to non-closure or re-opening because seventy of the 99 articles performed only one echocardiography. Therefore, there were insufficient data to study potential reopening of the ductus arteriosus in this review. The patency of the ductus arteriosus is regulated by the balance of vasodilating (prostaglandin E2, nitric oxide) and vasoconstrictor (oxygen) factors (6). Preterm neonates are more sensitive to the vasodilating factors compared to the term neonates (5). There is some evidence suggesting that genetic variations may play a role in the occurrence of PDA in preterm infants. In a large cohort of 1,013 preterm neonates Dagle et al. (125) found that several single nucleotide polymorphisms that were associated with PDA. For future meta-analyses, it might thus be of interest to include genetic variations to determine their influence on spontaneous closure.
Our systematic review was based on the assumption that gestational age is a more important factor compared to birthweight for patent ductus arteriosus in preterm infants. Villamor-Martinez et al. (126) showed that small for gestational age (SGA) infants showed a significantly reduced risk of PDA, but their review was complicated by the heterogeneity of studies. As SGA infants also show a much higher clearance of ibuprofen compared to appropriate weight for age newborns these patients form a special population that need additional attention in future PDA studies (127).
A next step could be to find markers to repeatedly monitor closure and pathophysiology of the ductus arteriosus. These could include the continuously available perfusion index to identify a hemodynamic significant PDA (51, 128) or urinary prostaglandine levels (129). Neutrophil gelatinase-associated lipocalin and heart-type fatty acid-binding protein are two peptides that can be measured in urine and also appear to be promising future markers to quantify the effect of a PDA on systemic perfusion, which makes the ductus arteriosus more hemodynamic significant (130, 131). Relevant risk factors could help to predict those patients whose ductus arteriosus will remain open and for whom pharmacological treatment might be needed.
Spontaneous closure rates increase with both gestational age and postnatal age. This review showed that in 34% of the most premature infants (GA < 28 weeks and/or BW < 1,000 g), the ductus arteriosus had spontaneously closed on the 3rd day of life (72–96 h). This increased to 41% at PNA day 7. As patients with a GA < 28 weeks have the lowest chance of spontaneous closure of the ductus arteriosus in the 1st days of life, studies on PDA management should therefore focus on these most premature patients.
Data Availability Statement
The original contributions presented in the study are included in the article's Supplementary Material, further inquiries can be directed to the corresponding author.
Author Contributions
JK is responsible for the study design, data collection and extraction, and writing and editing the article. AE is responsible for the data analysis and writing the article. SV helped with the analysis and edited the manuscript. FB performed the data collection and extraction. RF supervised the design and edited the manuscript. IR supervised the design and edited the manuscript. SS supervised the study design, data collection, and contributed with the editing of the article. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank W. G. Kramer for his help in the literature search.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2020.00541/full#supplementary-material
References
- 1.Clyman RI. The role of patent ductus arteriosus and its treatments in the development of bronchopulmonary dysplasia. Semin Perinatol. (2013) 37:102–7. 10.1053/j.semperi.2013.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hundscheid T, Onland W, Overmeire B, Van Dijk P, Kaam AHLC, Van Dijkman KP, et al. Early treatment versus expectative management of patent ductus arteriosus in preterm infants: a multicentre, randomised, non-inferiority trial in Europe (BeNeDuctus trial). BMC Pediatr. (2018) 18:262. 10.1186/s12887-018-1215-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laughon M, Bose C, Clark R. Treatment strategies to prevent or close a patent ductus arteriosus in preterm infants and outcomes. J Perinatol. (2007) 27:164–70. 10.1038/sj.jp.7211662 [DOI] [PubMed] [Google Scholar]
- 4.Hung YC, Yeh JL, Hsu JH. Molecular mechanisms for regulating postnatal ductus arteriosus closure. Int J Mol Sci. (2018) 19:1861. 10.3390/ijms19071861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hundscheid T, van den Broek M, van der Lee R, de Boode WP. Understanding the pathobiology in patent ductus arteriosus in prematurity-beyond prostaglandins and oxygen. Pediatr Res. (2019) 86:28–38. 10.1038/s41390-019-0387-7 [DOI] [PubMed] [Google Scholar]
- 6.Chiruvolu A, Jaleel MA. Pathophysiology of patent ductus arteriosus in premature neonates. Early Hum Dev. (2009) 85:143–6. 10.1016/j.earlhumdev.2008.12.006 [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez A, Sosenko IRS, Chandar J, Hummler H, Claure N, Bancalari E. Influence of infection on patent ductus arteriosus and chronic lung disease in premature infants weighing 1000 grams or less. J Pediatr. (1996) 128:470–8. 10.1016/S0022-3476(96)70356-6 [DOI] [PubMed] [Google Scholar]
- 8.Bardanzellu F, Neroni P, Dessì A, Fanos V. Paracetamol in patent ductus arteriosus treatment: efficacious and safe? Biomed Res Int. (2017) 2017:1438038. 10.1155/2017/1438038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Askie LM, Darlow BA, Davis PG, Finer N, Stenson B, Vento M, et al. Effects of targeting lower versus higher arterial oxygen saturations on death or disability in preterm infants. Cochrane Database Syst Rev. (2017) 2017:CD011190 10.1002/14651858.CD011190.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benitz WE, Fetus CON. Patent ductus arteriosus in preterm infants. Pediatrics. (2016) 137:1–6. 10.1542/peds.2015-3730 [DOI] [PubMed] [Google Scholar]
- 11.Aranda JV, Clyman R, Cox B, Van Overmeire B, Wozniak P, Sosenko I, et al. A randomized, double-blind, placebo- controlled trial on intravenous ibuprofen L-lysine for the early closure of nonsymptomatic patent ductus arteriosus within 72 hours of birth in extremely low-birth-weight infants. Am J Perinatol. (2009) 26:235–46. 10.1055/s-0028-1103515 [DOI] [PubMed] [Google Scholar]
- 12.Kluckow M, Jeffery M, Gill A, Evans N. A randomised placebo-controlled trial of early treatment of the patent ductus arteriosus. Arch Dis Child Fetal Neonatal Ed. (2014) 99:F99–104. 10.1136/archdischild-2013-304695 [DOI] [PubMed] [Google Scholar]
- 13.de Klerk JCA, van Paassen N, van Beynum IM, Flint RB, Reiss IKM, Simons SHP. Ibuprofen treatment after the first days of life in preterm neonates with patent ductus arteriosus. J Matern Neonatal Med. (2019) 1–7. 10.1080/14767058.2019.1667323. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 14.Roofthooft DWE, Van Beynum IM, Helbing WA, Reiss IKM, Simons SHP. Paracetamol for ductus arteriosus closure: not always a success story. Neonatology. (2013) 104:170. 10.1159/000353451 [DOI] [PubMed] [Google Scholar]
- 15.Rolland A, Shankar-Aguilera S, Diomandé D, Zupan-Simunek V, Boileau P. Natural evolution of patent ductus arteriosus in the extremely preterm infant. Arch Dis Child Fetal Neonatal Ed. (2015) 100:F55–8. 10.1136/archdischild-2014-306339 [DOI] [PubMed] [Google Scholar]
- 16.Narayanan M, Cooper B, Weiss H, Clyman RI. Prophylactic indomethacin: factors determining permanent ductus arteriosus closure. J Pediatr. (2000) 136:330–7. 10.1067/mpd.2000.103414 [DOI] [PubMed] [Google Scholar]
- 17.Gournay V, Roze JC, Kuster A, Daoud P, Cambonie G, Hascoet JM, et al. Prophylactic ibuprofen versus placebo in very premature infants: a randomised, double-blind, placebo-controlled trial. Lancet. (2004) 364:1939–44. 10.1016/S0140-6736(04)17476-X [DOI] [PubMed] [Google Scholar]
- 18.Dani C, Bertini G, Pezzati M, Poggi C, Guerrini P, Martano C, et al. Prophylactic ibuprofen for the prevention of intraventricular hemorrhage among preterm infants: a multicenter, randomized study. Pediatrics. (2005) 115:1529–35. 10.1542/peds.2004-1178 [DOI] [PubMed] [Google Scholar]
- 19.Erdeve O, Yurttutan S, Altug N, Ozdemir R, Gokmen T, Dilmen U, et al. Oral versus intravenous ibuprofen for patent ductus arteriosus closure: a randomised controlled trial in extremely low birthweight infants. Arch Dis Child Fetal Neonatal Ed. (2012) 97:F279–83. 10.1136/archdischild-2011-300532 [DOI] [PubMed] [Google Scholar]
- 20.Polat TB, Celik IH, Erdeve O. Early predictive echocardiographic features of hemodynamically significant patent ductus arteriosus in preterm VLBW infants. Pediatr Int. (2016) 58:589–94. 10.1111/ped.12915 [DOI] [PubMed] [Google Scholar]
- 21.Reller MD, Laird MR, Rice MJ, McDonald RW. Timing of ductal closure in very low birth weight premature infants without respiratory distress. J Pediatr. (1991) 119:976–7. 10.1016/S0022-3476(05)83060-4 [DOI] [PubMed] [Google Scholar]
- 22.Parikh R, Negrine RJS, Chikermane A, Rasiah SV, Ewer AK. Assessment of myocardial function in preterm infants with patent ductus arteriosus using tissue Doppler imaging. Cardiol Young. (2014) 25:70–5. 10.1017/S1047951113001595 [DOI] [PubMed] [Google Scholar]
- 23.Bin-Nun A, Mimouni FB, Fink D, Sela H, Hammerman C. Elevated nucleated red blood cells at birth predict hemodynamically significant patent ductus arteriosus. J Pediatr. (2016) 177:313–5. 10.1016/j.jpeds.2016.07.005 [DOI] [PubMed] [Google Scholar]
- 24.De Waal K, Phad N, Lakkundi A, Tan P. Post-transitional adaptation of the left heart in uncomplicated, very preterm infants. Cardiol Young. (2017) 27:1167–73. 10.1017/S1047951116002687 [DOI] [PubMed] [Google Scholar]
- 25.de Waal K, Phad N, Boyle A. Left atrium function and deformation in very preterm infants with and without volume load. Echocardiography. (2018) 35:1818–26. 10.1111/echo.14140 [DOI] [PubMed] [Google Scholar]
- 26.Kahvecioglu D, Erdeve O, Akduman H, Ucar T, Alan S, Çakir U, et al. Influence of platelet count, platelet mass index, and platelet function on the spontaneous closure of ductus arteriosus in the prematurity. Pediatr Neonatol. (2018) 59:53–7. 10.1016/j.pedneo.2017.01.006 [DOI] [PubMed] [Google Scholar]
- 27.Van Overmeire B, Allegaert K, Casaer A, Debauche C, Decaluwé W, Jespers A, et al. Prophylactic ibuprofen in premature infants: a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. (2004) 364:1945–9. 10.1016/S0140-6736(04)17477-1 [DOI] [PubMed] [Google Scholar]
- 28.Braulio R, Gelape CL, Araújo FD da R, Brandão KN, Abreu LDG, Costa PHN, et al. Indicadores para o tratamento cirúrgico na persistência do ducto arterial em neonatos prematuros na primeira semana de vida. Braz J Cardiovasc Surg. (2013) 28:504–8. 10.5935/1678-9741.20130082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oncel MY, Yurttutan S, Erdeve O, Uras N, Altug N, Oguz SS, et al. Oral paracetamol versus oral ibuprofen in the management of patent ductus arteriosus in preterm infants: A randomized controlled trial. J Pediatr. (2014) 164:510–4.e1. 10.1016/j.jpeds.2013.11.008 [DOI] [PubMed] [Google Scholar]
- 30.Skelton R, Evans N, Smythe J. A blinded comparison of clinical and echocardiographic evaluation of the preterm infant for patent ductus arteriosus. J Paediatr Child Health. (1994) 30:406–11. 10.1111/j.1440-1754.1994.tb00689.x [DOI] [PubMed] [Google Scholar]
- 31.Su BH, Watanabe T, Shimizu M, Yanagisawa M. Echocardiographic assessment of patent ductus arteriosus shunt flow pattern in premature infants. Arch Dis Child Fetal Neonatal Ed. (1997) 77:36–40. 10.1136/fn.77.1.F36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.El-Khuffash A, Barry D, Walsh K, Davis PG, Molloy EJ. Biochemical markers may identify preterm infants with a patent ductus arteriosus at high risk of death or severe intraventricular haemorrhage. Arch Dis Child Fetal Neonatal Ed. (2008) 93:407–13. 10.1136/adc.2007.133140 [DOI] [PubMed] [Google Scholar]
- 33.Nemerofsky SL, Parravicini E, Bateman D, Kleinman C, Polin RA, Lorenz JM. The ductus arteriosus rarely requires treatment in infants > 1000 grams. Am J Perinatol. (2008) 25:661–6. 10.1055/s-0028-1090594 [DOI] [PubMed] [Google Scholar]
- 34.Sangtawesin C, Sangtawesin V, Lertsutthiwong W, Kanjanapattanakul W, Khorana M, Ayudhaya JKN. Prophylaxis of symptomatic patent ductus arteriosus with oral ibuprofen in very low birth weight infants. J Med Assoc Thai. (2008) 91(Suppl 3):28–34. [PubMed] [Google Scholar]
- 35.Gokmen T, Erdeve O, Altug N, Oguz SS, Uras N, Dilmen U. Efficacy and safety of oral versus intravenous ibuprofen in very low birth weight preterm infants with patent ductus arteriosus. J Pediatr. (2011) 158:549–54. 10.1016/j.jpeds.2010.10.008 [DOI] [PubMed] [Google Scholar]
- 36.De Carolis MP, Romagnoli C, Polimeni V, Piersigilli F, Zecca E, Papacci P, et al. Prophylactic ibuprofen therapy of patent ductus arteriosus in preterm infants. Eur J Pediatr. (2000) 159:364–8. 10.1007/s004310051288 [DOI] [PubMed] [Google Scholar]
- 37.Sellmer A, Bjerre JV, Schmidt MR, McNamara PJ, Hjortdal VE, Høst B, et al. Morbidity and mortality in preterm neonates with patent ductus arteriosus on day 3. Arch Dis Child Fetal Neonatal Ed. (2013) 98:F505–10. 10.1136/archdischild-2013-303816 [DOI] [PubMed] [Google Scholar]
- 38.Akar S, Karadag N, Gokmen Yildirim T, Toptan HH, Dincer E, Tuten A, et al. Does platelet mass influence the effectiveness of ibuprofen treatment for patent ductus arteriosus in preterm infants? J Matern Neonatal Med. (2016) 29:3786–9. 10.3109/14767058.2016.1145207 [DOI] [PubMed] [Google Scholar]
- 39.Härkin P, Härmä A, Aikio O, Valkama M, Leskinen M, Saarela T, et al. Paracetamol accelerates closure of the ductus arteriosus after premature birth: a randomized trial. J Pediatr. (2016) 177:72–7.e2. 10.1016/j.jpeds.2016.04.066 [DOI] [PubMed] [Google Scholar]
- 40.Van Der Laan ME, Roofthooft MTR, Fries MWA, Berger RMF, Schat TE, Van Zoonen AGJF, et al. A hemodynamically significant patent ductus arteriosus does not affect cerebral or renal tissue oxygenation in preterm infants. Neonatology. (2016) 110:141–7. 10.1159/000445101 [DOI] [PubMed] [Google Scholar]
- 41.Demir N, Peker E, Ece I, Balahoroglu R, Tuncer O. Efficacy and safety of rectal ibuprofen for patent ductus arteriosus closure in very low birth weight preterm infants. J Matern Neonatal Med. (2017) 30:2119–25. 10.1080/14767058.2016.1238897 [DOI] [PubMed] [Google Scholar]
- 42.Sellmer A, Bech BH, Bjerre JV, Schmidt MR, Hjortdal VE, Esberg G, et al. Urinary neutrophil gelatinase-associated lipocalin in the evaluation of patent ductus arteriosus and AKI in very preterm neonates: a cohort study. BMC Pediatr. (2017) 17:7. 10.1186/s12887-016-0761-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yum SK, Moon CJ, Youn YA, Lee JY, Sung IK. Echocardiographic assessment of patent ductus arteriosus in very low birthweight infants over time: prospective observational study. J Matern Neonatal Med. (2018) 31:164–72. 10.1080/14767058.2016.1278207 [DOI] [PubMed] [Google Scholar]
- 44.Heyman E, Morag I, Batash D, Keidar R, Baram S, Berkovitch M. Closure of patent ductus arteriosus with oral ibuprofen suspension in premature newborns: a pilot study. Pediatrics. (2003) 112(5). 10.1542/peds.112.5.e354 [DOI] [PubMed] [Google Scholar]
- 45.Schmitz L, Stiller B, Koch H, Koehne P, Lange P. Diastolic left ventricular function in preterm infants with a patent ductus arteriosus: a serial Doppler echocardiography study. Early Hum Dev. (2004) 76:91–100. 10.1016/j.earlhumdev.2003.11.002 [DOI] [PubMed] [Google Scholar]
- 46.Shortland DB, Gibson NA, Levene MI, Archer LNJ, Evans DH, Shaw DE. Patent ductus arteriosus and cerebral circulation in preterm infants. Dev Med Child Neurol. (1990) 32:386–93. 10.1111/j.1469-8749.1990.tb16957.x [DOI] [PubMed] [Google Scholar]
- 47.Kulkarni VV, Dutta S, Sundaram V, Saini SS. Preterm thrombocytopenia and delay of ductus arteriosus closure. Pediatrics. (2016) 138:e20161627. 10.1542/peds.2016-1627 [DOI] [PubMed] [Google Scholar]
- 48.Babaei H, Nemati R, Daryoshi H. Closure of patent ductus arteriosus with oral acetaminophen in preterm neonates: a randomized trial. Biomed Res Ther. (2018) 5:2034–44. 10.15419/bmrat.v5i02.418 [DOI] [Google Scholar]
- 49.Bagheri MM, Bahman-Bijari B, Torabi-Nejad MH, Niknafs P, Mousavi H, Sabzevari F, et al. Is prophylactic parenteral paracetamol effective to diminish incidence of PDA in preterm neonates? A randomized trial. Iran J Pediatr. (2018) 28:10–3. 10.5812/ijp.11735 [DOI] [Google Scholar]
- 50.Ding Y, Wang X, Wu Y, Li H, Xu J, Wang X. Effects of prophylactic oral ibuprofen on the closure rate of patent ductus arteriosus in premature infants. Medicine. (2018) 97:1–8. 10.1097/MD.0000000000012206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Khositseth A, Muangyod N, Nuntnarumit P. Perfusion index as a diagnostic tool for patent ductus arteriosus in preterm infants. (2013) 104:250–4. 10.1159/000353862 [DOI] [PubMed] [Google Scholar]
- 52.Byung MC, Kee HL, Baik LE, Kee HY, Young SH, Chang SS, et al. Utility of rapid B-type natriuretic peptide assay for diagnosis of symptomatic patent ductus arteriosus in preterm infants. Pediatrics. (2005) 115:e255–61. 10.1542/peds.2004-1837 [DOI] [PubMed] [Google Scholar]
- 53.van Overmeire B, Brus F, van Acker KJ, van der Auwera JC, Schasfoort M, Elzenga NJ, et al. Aspirin versus indomethacin treatment of patent ductus arteriosus in preterm infants with respiratory distress syndrome. Pediatr Res. (1995) 38:886–91. 10.1203/00006450-199512000-00010 [DOI] [PubMed] [Google Scholar]
- 54.Liebowitz M, Clyman RI. Prophylactic indomethacin compared with delayed conservative management of the patent ductus arteriosus in extremely preterm infants: effects on neonatal outcomes. J Pediatr. (2017) 187:119–26.e1. 10.1016/j.jpeds.2017.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vieux R, Desandes R, Boubred F, Semama D, Guillemin F, Buchweiller MC, et al. Ibuprofen in very preterm infants impairs renal function for the first month of life. Pediatr Nephrol. (2010) 25:267–74. 10.1007/s00467-009-1349-9 [DOI] [PubMed] [Google Scholar]
- 56.Martinovici D, Vanden Eijnden S, Unger P, Najem B, Gulbis B, Maréchal Y. Early NT-proBNP is able to predict spontaneous closure of patent ductus arteriosus in preterm neonates, but not the need of its treatment. Pediatr Cardiol. (2011) 32:953–7. 10.1007/s00246-011-0020-y [DOI] [PubMed] [Google Scholar]
- 57.Letshwiti JB, Sirc J, O'Kelly R, Miletin J. Serial N-terminal pro-brain natriuretic peptide measurement as a predictor of significant patent ductus arteriosus in preterm infants beyond the first week of life. Eur J Pediatr. (2014) 173:1491–6. 10.1007/s00431-014-2350-2 [DOI] [PubMed] [Google Scholar]
- 58.Chen HL, Yang RC, Lee W-T, Lee PL, Hsu JH, Wu JR, et al. Lung function in very preterm infants with patent ductus arteriosus under conservative management: an observational study. BMC Pediatr. (2015) 15:1–6. 10.1186/s12887-015-0480-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Suzumura H, Nitta A, Tanaka G, Arisaka O. Diastolic flow velocity of the left pulmonary artery of patent ductus arteriosus in preterm infants. Pediatr Int. (2001) 43:146–51. 10.1046/j.1442-200x.2001.01365.x [DOI] [PubMed] [Google Scholar]
- 60.Nuntnarumit P, Chongkongkiat P, Khositseth A. N-terminal-pro-brain natriuretic peptide: a guide for early targeted indomethacin therapy for patent ductus arteriosus in preterm infants. Acta Paediatr Int J Paediatr. (2011) 100:1217–21. 10.1111/j.1651-2227.2011.02304.x [DOI] [PubMed] [Google Scholar]
- 61.Ding YJ, Han B, Yang B, Zhu M. NT-proBNP plays an important role in the effect of ibuprofen on preterm infants with patent ductus arteriosus. Eur Rev Med Pharmacol Sci. (2014) 18:2596–8. [PubMed] [Google Scholar]
- 62.Puddy VF, Amirmansour C, Williams AF, Singer DRJ. Plasma brain natriuretic peptide as a predictor of haemodynamically significant patent ductus arteriosus in preterm infants. Clin Sci. (2002) 103:75–7. 10.1042/cs1030075 [DOI] [PubMed] [Google Scholar]
- 63.Su BH, Lin HC, Chiu HY, Hsieh HY, Chen HH, Tsai YC. Comparison of ibuprofen and indometacin for early-targeted treatment of patent ductus arteriosus in extremely premature infants: a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed. (2008) 93:F94–9. 10.1136/adc.2007.120584 [DOI] [PubMed] [Google Scholar]
- 64.Candel-Pau J, Sillo Á, Salinas F, Redon E, Menduiña Q, Albert DC. Early versus conventional treatment for patent ductus arteriosus in preterm infants. Am J Perinatol. (2013) 30:289–96. 10.1055/s-0032-1324696 [DOI] [PubMed] [Google Scholar]
- 65.Steiner M, Salzer-Muhar U, Swoboda V, Unterasinger L, Baumgartner S, Waldhoer T, et al. Preterm infants who later require duct ligation show different vital signs and pH in early postnatal life. Acta Paediatr Int J Paediatr. (2015) 104:e7–13. 10.1111/apa.12814 [DOI] [PubMed] [Google Scholar]
- 66.Lee JH, Greenberg RG, Quek BH, Clark RH, Laughon MM, Smith PB, et al. Association between early echocardiography, therapy for patent ductus arteriosus, and outcomes in very low birth weight infants. Cardiol Young. (2017) 27:1732–9. 10.1017/S1047951117001081 [DOI] [PubMed] [Google Scholar]
- 67.Breatnach CR, Franklin O, James AT, McCallion N, El-Khuffash A. The impact of a hyperdynamic left ventricle on right ventricular function measurements in preterm infants with a patent ductus arteriosus. Arch Dis Child Fetal Neonatal Ed. (2017) 102:F446–50. 10.1136/archdischild-2016-311189 [DOI] [PubMed] [Google Scholar]
- 68.Elsayed Y, Seshia M, Baier RJ, Dakshinamurti S. Serial serum brain-type natriuretic peptide (BNP) identifies compromised blood flow in infants with hemodynamically significant patent ductus arteriosus. J Pediatr Neonatal Individ Med. (2017) 6:1–10. [Google Scholar]
- 69.Gomez-Pomar E, Makhoul M, Westgate PM, Ibonia KT, Patwardhan A, Giannone PJ, et al. Relationship between perfusion index and patent ductus arteriosus in preterm infants. Pediatr Res. (2017) 81:775–9. 10.1038/pr.2017.10 [DOI] [PubMed] [Google Scholar]
- 70.Romagnoli V, Pedini A, Santoni M, Scutti G, Colaneri M, Pozzi M, et al. Patent ductus arteriosus in preterm infants born before 30 weeks' gestation: high rate of spontaneous closure after hospital discharge. Cardiol Young. (2018) 28:995–1000. 10.1017/S1047951118000641 [DOI] [PubMed] [Google Scholar]
- 71.Küçük M, Bagci O, IGde M. The fate of patent ductus arteriosus is not affected by platelet count and mean platelet volume in premature infants < 32 gestational weeks. Turkiye Klin Cardiovasc Sci. (2018) 30:53–7. 10.5336/cardiosci.2018-62380 [DOI] [Google Scholar]
- 72.Ment LR, Oh W, Ehrenkranz RA, Philip AGS, Vohr B, Allan W, et al. Low-dose indomethacin and prevention of intraventricular hemorrhage: a multicenter randomized trial. Pediatrics. (1994) 93:543–50. [PubMed] [Google Scholar]
- 73.Groves AM, Kuschel CA, Knight DB, Skinner JR. Does retrograde diastolic flow in the descending aorta signify impaired systemic perfusion in preterm infants? Pediatr Res. (2008) 63:89–94. 10.1203/PDR.0b013e31815b4830 [DOI] [PubMed] [Google Scholar]
- 74.Kalra VK, DeBari VA, Zauk A, Kataria P, Myridakis D, Kiblawi F. Point-of-care testing for B-type natriuretic peptide in premature neonates with patent ductus arteriosus. Ann Clin Lab Sci. (2011) 41:131–7. [PubMed] [Google Scholar]
- 75.Alan S, Karadeniz C, Okulu E, Kilic A, Erdeve O, Ucar T, et al. Management of patent ductus arteriosus in preterm infants: clinical judgment might be a fair option. J Matern Neonatal Med. (2013) 26:1850–4. 10.3109/14767058.2013.801956 [DOI] [PubMed] [Google Scholar]
- 76.Dani C, Poggi C, Fontanelli G. Relationship between platelet count and volume and spontaneous and pharmacological closure of ductus arteriosus in preterm infants. Am J Perinatol. (2013) 30:359–64. 10.1055/s-0032-1324702 [DOI] [PubMed] [Google Scholar]
- 77.Koch J, Hensley G, Roy L, Brown S, Ramaciotti C, Rosenfeld CR. Prevalence of spontaneous closure of the ductus arteriosus in neonates at a birth weight of 1000 grams or less. Pediatrics. (2006) 117:1113–21. 10.1542/peds.2005-1528 [DOI] [PubMed] [Google Scholar]
- 78.Rakza T, Magnenant E, Klosowski S, Tourneux P, Bachiri A, Storme L. Early hemodynamic consequences of patent ductus arteriosus in preterm infants with intrauterine growth restriction. J Pediatr. (2007) 151:624–8. 10.1016/j.jpeds.2007.04.058 [DOI] [PubMed] [Google Scholar]
- 79.Strauss T, Pessach I, Jacoby E, Schushan-Eisen I, Mazkereth R, Kuint J. Carina angle measurements for diagnosis of patent ductus arteriosus in preterm infants. Neonatology. (2011) 99:224–30. 10.1159/000315862 [DOI] [PubMed] [Google Scholar]
- 80.Dhuper S, Kim R, Weichbrod L, Mahdi E, Shah N, Kona S, et al. NT-proBNP levels improve the ability of predicting a hemodynamically significant patent ductus arteriosus in very low-birth-weight infants. J Clin Neonatol. (2012) 1:82. 10.4103/2249-4847.96758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Desandes R, Jellimann JM, Rouabah M, Haddad F, Desandes E, Boubred F, et al. Echocardiography as a guide for patent ductus arteriosus ibuprofen treatment and efficacy prediction. Pediatr Crit Care Med. (2012) 13:324–7. 10.1097/PCC.0b013e31822882b5 [DOI] [PubMed] [Google Scholar]
- 82.Alyamac Dizdar E, Ozdemir R, Nur Sari F, Yurttutan S, Gokmen T, Erdeve O, et al. Low platelet count is associated with ductus arteriosus patency in preterm newborns. Early Hum Dev. (2012) 88:813–6. 10.1016/j.earlhumdev.2012.05.007 [DOI] [PubMed] [Google Scholar]
- 83.Sallmon H, Weber SC, Hüning B, Stein A, Horn PA, Metze BC, et al. Thrombocytopenia in the first 24 hours after birth and incidence of patent ductus arteriosus. Pediatrics. (2012) 130:e623–30. 10.1542/peds.2012-0499 [DOI] [PubMed] [Google Scholar]
- 84.Brunner B, Hoeck M, Schermer E, Streif W, Kiechl-Kohlendorfer U. Patent ductus arteriosus, low platelets, cyclooxygenase inhibitors, and intraventricular hemorrhage in very low birth weight preterm infants. J Pediatr. (2013) 163:23–8. 10.1016/j.jpeds.2012.12.035 [DOI] [PubMed] [Google Scholar]
- 85.Visconti LF, Morhy SS, Deutsch ADA, Tavares GMP, Wilberg TJM, Rossi F de S. Clinical and echocardiographic characteristics associated with the evolution of the ductus arteriosus in the neonate with birth weight lower than 1,500g. Einstein (Sao Paulo). (2013) 11:317–23. 10.1590/S1679-45082013000300010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Grass B, Baumann P, Arlettaz R, Fouzas S, Meyer P, Spanaus K, et al. Cardiovascular biomarkers pro-atrial natriuretic peptide and pro-endothelin-1 to monitor ductus arteriosus evolution in very preterm infants. Early Hum Dev. (2014) 90:293–8. 10.1016/j.earlhumdev.2014.03.002 [DOI] [PubMed] [Google Scholar]
- 87.Occhipinti F, De Carolis MP, De Rosa G, Bersani I, Lacerenza S, Cota F, et al. Correlation analysis between echocardiographic flow pattern and N-terminal-pro-brain natriuretic peptide for early targeted treatment of patent ductus arteriosus. J Matern Neonatal Med. (2014) 27:1800–4. 10.3109/14767058.2014.880879 [DOI] [PubMed] [Google Scholar]
- 88.Trevisanuto D, Zaninotto M, Lachin M, Altinier S, Plebani M, Ferrarese P, et al. Effect of patent ductus arteriosus and indomethacin treatment on serum cardiac troponin T levels in preterm infants with respiratory distress syndrome. Eur J Pediatr. (2000) 159:273–6. 10.1007/s004310050069 [DOI] [PubMed] [Google Scholar]
- 89.König K, Guy KJ, Drew SM, Barfield CP. B-type and N-terminal pro-B-type natriuretic peptides are equally useful in assessing patent ductus arteriosus in very preterm infants. Acta Paediatr Int J Paediatr. (2015) 104:e139–42. 10.1111/apa.12892 [DOI] [PubMed] [Google Scholar]
- 90.Breatnach CR, Franklin O, McCallion N, EL-Khuffash A. The effect of a significant patent ductus arteriosus on doppler flow patterns of preductal vessels: an assessment of the brachiocephalic artery. J Pediatr. (2017) 180:279–81.e1. 10.1016/j.jpeds.2016.09.029 [DOI] [PubMed] [Google Scholar]
- 91.Demir N, Peker E, Ece I, Agengin K, Bulan KA, Tuncer O. Is platelet mass a more significant indicator than platelet count of closure of patent ductus arteriosus? J Matern Neonatal Med. (2016) 29:1915–8. 10.3109/14767058.2015.1067296 [DOI] [PubMed] [Google Scholar]
- 92.Dix L, Molenschot M, Breur J, de Vries W, Vijlbrief D, Groenendaal F, et al. Cerebral oxygenation and echocardiographic parameters in preterm neonates with a patent ductus arteriosus: an observational study. Arch Dis Child Fetal Neonatal Ed. (2016) 101:F520–6. 10.1136/archdischild-2015-309192 [DOI] [PubMed] [Google Scholar]
- 93.Elsayed Y, Seshia M, Soni R, Buffo I, Baier RJ, McNamara PJ, et al. Pre-symptomatic prediction of morbitidies in preterm infants with patent ductus arteriosus by targeted neonatal echocardiography and brain-type natriuretic peptide. J Pediatr Neonatal Individ Med. (2016) 5:1–10. [Google Scholar]
- 94.Engür D, Deveci M, Türkmen MK. Early signs that predict later haemodynamically significant patent ductus arteriosus. Cardiol Young. (2016) 26:439–45. 10.1017/S1047951115000372 [DOI] [PubMed] [Google Scholar]
- 95.Mochammading, Kaban RK, Yanuarso PB, Djer MM. Prostaglandin E2 and patent ductus arteriosus in premature infants. (2016) 56:8–14. 10.14238/pi56.1.2016.02 [DOI] [Google Scholar]
- 96.Arlettaz R, Archer N, Wilkinson AR. Closure of the ductus arteriosus and development of pulmonary branch stenosis in babies of less than 32 weeks gestation. Arch Dis Child Fetal Neonatal Ed. (2001) 85. 10.1136/fn.85.3.F197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Oliveira AGS, Soares P, Flor-de-Lima F, Neves AL, Guimarães H. PDA management in VLBW infants: experience of a level III NICU. J Pediatr Neonatal Individ Med. (2016) 5:1–9. [Google Scholar]
- 98.Tauber K, Granina E, Doyle R, Munshi U. Gestational and postnatal age influence B-type natriuretic peptide level used in diagnosis of a hemodynamically significant patent ductus arteriosus in preterm infants. J Clin Neonatol. (2016) 5:143 10.4103/2249-4847.191241 [DOI] [Google Scholar]
- 99.Valerio E, Valente MR, Salvadori S, Frigo AC, Baraldi E, Lago P. Intravenous paracetamol for PDA closure in the preterm: a single-center experience. Eur J Pediatr. (2016) 175:953–66. 10.1007/s00431-016-2731-9 [DOI] [PubMed] [Google Scholar]
- 100.Ledo A, Aguar M, Núñez-Ramiro A, Saénz P, Vento M. Abdominal near-infrared spectroscopy detects low mesenteric perfusion early in preterm infants with hemodynamic significant ductus arteriosus. Neonatology. (2017) 112:238–45. 10.1159/000475933 [DOI] [PubMed] [Google Scholar]
- 101.Demirel G, Yılmaz A, Vatansever B, Tastekin A. Is high platelet distribution width in the first hours of life can predict hemodynamically significant patent ductus arteriosus in preterm newborns? J Matern Fetal Neonatal Med. (2020) 33:2049–53. 10.1080/14767058.2018.1536743 [DOI] [PubMed] [Google Scholar]
- 102.Van Overmeire B, Van De Broek H, Van Laer P, Weyler J, Vanhaesebrouck P. Early versus late indomethacin treatment for patent ductus arteriosus in premature infants with respiratory distress syndrome. J Pediatr. (2001) 138:205–11. 10.1067/mpd.2001.110528 [DOI] [PubMed] [Google Scholar]
- 103.Sanjeev S, Pettersen M, Lua J, Thomas R, Shankaran S, L'Ecuyer T. Role of plasma B-type natriuretic peptide in screening for hemodynamically significant patent ductus arteriosus in preterm neonates. J Perinatol. (2005) 25:709–13. 10.1038/sj.jp.7211383 [DOI] [PubMed] [Google Scholar]
- 104.Dix LML, Blok CA, Lemmers PMA, Van Der Aa N, Molenschot MC, Vreman HJ, et al. Early end-tidal carbon monoxide levels, patency of the ductus arteriosus and regional cerebral oxygenation in preterm infants. Neonatology. (2014) 105:161–5. 10.1159/000356167 [DOI] [PubMed] [Google Scholar]
- 105.Olukman O, Ozdemir R, Karadeniz C, Calkavur S, Mese T, Vergin C. Is there a relationship between platelet parameters and patency of ductus arteriosus in preterm infants? Blood Coagul Fibrinolysis. (2017) 28:8–13. 10.1097/MBC.0000000000000520 [DOI] [PubMed] [Google Scholar]
- 106.Khositseth A, Nuntnarumit P, Chongkongkiat P. Echocardiographic parameters of patent ductus arteriosus in preterm infants. Indian Pediatr. (2011) 48:773–8. 10.1007/s13312-011-0127-5 [DOI] [PubMed] [Google Scholar]
- 107.Lago P, Bettiol T, Salvadori S, Pitassi I, Vianello A, Chiandetti L, et al. Safety and efficacy of ibuprofen versus indomethacin in preterm infants treated for patent ductus arteriosus: a randomised controlled trial. Eur J Pediatr. (2002) 161:202–7. 10.1007/s00431-002-0915-y [DOI] [PubMed] [Google Scholar]
- 108.Khosroshahi AJ, Kianfar A, Aharanjani BM, Zanjani KS. Usefulness of serum brain natriuretic peptide level for screening hemodynamically significant patent ductus arteriosus in preterm neonates. Iran J Pediatr. (2014) 24:766–9. [PMC free article] [PubMed] [Google Scholar]
- 109.Van Overmeire B, Follens I, Hartmann S, Creten WL, Van Acker KJ. Treatment of patent ductus arteriosus with ibuprofen. Arch Dis Child Fetal Neonatal Ed. (1997) 76:1–6. 10.1136/fn.76.3.F179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nuntnarumit P, Khositseth A, Thanomsingh P. N-terminal probrain natriuretic peptide and patent ductus arteriosus in preterm infants. J Perinatol. (2009) 29:137–42. 10.1038/jp.2008.185 [DOI] [PubMed] [Google Scholar]
- 111.Terek D, Yalaz M, Ulger Z, Koroglu OA, Kultursay N. Medical closure of patent ductus arteriosus does not reduce mortality and development of bronchopulmonary dysplasia in preterm infants. J Res Med Sci. (2014) 19:1074–9. [PMC free article] [PubMed] [Google Scholar]
- 112.Mine K, Ohashi A, Tsuji S, Nakashima JI, Hirabayashi M, Kaneko K. B-type natriuretic peptide for assessment of haemodynamically significant patent ductus arteriosus in premature infants. Acta Paediatr Int J Paediatr. (2013) 102:347–52. 10.1111/apa.12273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zonnenberg I, De Waal K. The definition of a haemodynamic significant duct in randomized controlled trials: A systematic literature review. Acta Paediatr Int J Paediatr. (2012) 101:247–51. 10.1111/j.1651-2227.2011.02468.x [DOI] [PubMed] [Google Scholar]
- 114.van Laere D, van Overmeire B, Gupta S, El Khuffash A, Savoia M, McNamara PJ, et al. Application of NPE in the assessment of a patent ductus arteriosus. Pediatr Res. (2018) 84:46–56. 10.1038/s41390-018-0077-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.El Hajjar M, Vaksmann G, Rakza T, Kongolo G, Storme L. Severity of the ductal shunt: a comparison of different markers. Arch Dis Child Fetal Neonatal Ed. (2005) 90:419–22. 10.1136/adc.2003.027698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ngo S, Profit J, Gould JB, Lee HC. Trends in patent ductus arteriosus diagnosis and management for very low birth weight infants. Pediatrics. (2017) 139:e20162390. 10.1542/peds.2016-2390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lamp KC, Reynolds MS. Indomethacin for prevention of neonatal intraventricular hemorrhage. DICP. (1991) 25:1344–8. 10.1177/106002809102501213 [DOI] [PubMed] [Google Scholar]
- 118.Fowlie PW, Davis PG. Cochrane review: prophylactic intravenous indomethacin for preventing mortality and morbidity in preterm infants. Evidence Based Child Health A Cochrane Rev J. (2010) 5:416–71. 10.1002/ebch.526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Jensen EA, Dysart KC, Gantz MG, Carper B, Higgins RD, Keszler M, et al. Association between use of prophylactic indomethacin and the risk for bronchopulmonary dysplasia in extremely preterm infants. J Pediatr. (2017) 186:34–40.e2. 10.1016/j.jpeds.2017.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Pacifici GM. Differential renal adverse effects of ibuprofen and indomethacin in preterm infants: a review. Clin Pharmacol Adv Appl. (2014) 6:111–6. 10.2147/CPAA.S59376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ferguson JM. Pharmacotherapy for patent ductus arteriosus closure. Congenit Heart Dis. (2018) 14:52–6. 10.1111/chd.12715 [DOI] [PubMed] [Google Scholar]
- 122.Ohlsson A, Shah SS. Ibuprofen for the prevention of patent ductus arteriosus in preterm and/or low birth weight infants. Cochrane Database Syst Rev. (2020) 2020:1–60. 10.1002/14651858.CD004213.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Mitra S, Florez ID, Tamayo ME, Mbuagbaw L, Vanniyasingam T, Veroniki AA, et al. Association of placebo, indomethacin, ibuprofen, and acetaminophen with closure of hemodynamically significant patent ductus arteriosus in preterm infants a systematic review and meta-analysis. JAMA J Am Med Assoc. (2018) 319:1221–38. 10.1001/jama.2018.1896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Aikio O, Härkin P, Saarela T, Hallman M. Early paracetamol treatment associated with lowered risk of persistent ductus arteriosus in very preterm infants. J Matern Neonatal Med. (2014) 27:1252–6. 10.3109/14767058.2013.854327 [DOI] [PubMed] [Google Scholar]
- 125.Dagle JM, Ryckman KK, Spracklen CN, Momany M, Cotten CM, Levy J, et al. Genetic variants associated with patent ductus arteriosus in extremely preterm infants. (2019) 39:401–8. 10.1038/s41372-018-0285-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Villamor-Martinez E, Kilani MA, Degraeuwe PL, Clyman RI, Villamor E. Intrauterine growth restriction and patent ductus arteriosus in very and extremely preterm infants: a systematic review and meta-analysis. Front Endocrinol. (2019) 10:1–11. 10.3389/fendo.2019.00058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Engbers AGJ, Klerk JCA, De Flint RB, Völler S, Reiss IKM, Andriessen P, et al. Enantiomer specific pharmacokinetics of ibuprofen in preterm neonates with patent ductus arteriosus. (2020) 1–12. 10.1111/bcp.14298. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Terek D, Altun Koroglu O, Ulger Z, Yalaz M, Kultursay N. The serial changes of perfusion index in preterm infants with patent ductus arteriosus: is perfusion index clinically significant? Minerva Pediatr. (2016) 68:250–5. [PubMed] [Google Scholar]
- 129.Antonucci R, Cuzzolin L, Arceri A, Dessì A, Fanos V. Changes in urinary PGE2 after ibuprofen treatment in preterm infants with patent ductus arteriosus. Eur J Clin Pharmacol. (2009) 65:223–30. 10.1007/s00228-008-0586-3 [DOI] [PubMed] [Google Scholar]
- 130.Tosse V, Pillekamp F, Verde P, Hadzik B, Sabir H, Mayatepek E, et al. Urinary NT-proBNP, NGAL, and H-FABP may predict hemodynamic relevance of patent ductus arteriosus in very low birth weight infants. Neonatology. (2012) 101:260–6. 10.1159/000334826 [DOI] [PubMed] [Google Scholar]
- 131.Lavery AP, Meinzen-Derr JK, Anderson E, Ma Q, Bennett MR, Devarajan P, et al. Urinary NGAL in premature infants. Pediatr Res. (2008) 64:423–8. 10.1203/PDR.0b013e318181b3b2 [DOI] [PubMed] [Google Scholar]
- 132.El-Khuffash A, Higgins M, Walsh K, Molloy EJ. Quantitative assessment of the degree of ductal steal using celiac artery blood flow to left ventricular output ratio in preterm infants. Neonatology. (2008) 93:206–12. 10.1159/000110869 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article's Supplementary Material, further inquiries can be directed to the corresponding author.