Rheumatology key message
A positive squeeze test in clinically suspect arthralgia is associated with presence of subclinical synovitis.
Sir, The squeeze test (or compression test) is often used to quickly screen for arthritis in MCP and MTP joints. A positive test is traditionally assumed to indicate presence of synovitis [1]. Previous studies in early arthritis indeed showed that a positive squeeze test was associated with presence of swollen MCP and MTP joints, as well as with local MRI-detected inflammation [2]. The sensitivity of the test, with MRI-detected synovitis as reference, was 31–33% [2]. The field of early arthritis is moving towards identifying patients at risk for RA in the phase of arthralgia. MRI-detected subclinical inflammation has been shown to be predictive for RA development; of all inflammatory features, tenosynovitis had the strongest association [3]. We here aimed to assess if a positive squeeze test in patients with clinically suspect arthralgia (CSA) is associated with subclinical inflammation. We specifically hypothesized that it is associated with subclinical synovitis, in line with the original assumption of the test being a measure of synovitis. MRI-detected tenosynovitis was also studied, because we assumed that tenosynovitis at MCP or MTP level may also produce pain upon compression. Finally, we studied the association of the test with progression to inflammatory arthritis (IA).
Between April 2015 and October 2018, 315 patients were consecutively included in the Leiden CSA cohort; details are provided in the Supplementary material, section ‘Methods’, available at Rheumatology online. Inclusion criteria were recent-onset (<1 year) arthralgia of small joints and a clinical suspicion for progression to RA, which means that according to the pattern recognition of the rheumatologist at first visit, imminent RA was more likely than other diagnoses, as described previously [4]. All patients gave written informed consent. The study was approved by the local medical ethical committee. At baseline the squeeze test was performed; compression across the knuckles of MCP and MTP joints with the force of a firm handshake, as described previously [2]. Unilateral contrast-enhanced 1.5 T MRI of MCP (2–5) and MTP (1–5) joints was also made at baseline and scored by two trained readers for synovitis (according to RAMRIS [5]) and tenosynovitis (according to Haavardsholm et al. [6]). MRI scores were dichotomized with data from age-matched symptom-free controls as reference. A detailed scanning and scoring protocol and information on dichotomization is provided in the Supplementary material, section ‘Methods’, available at Rheumatology online. Follow-up ended when patients developed clinically apparent IA (determined at physical examination), or else after 2 years. Associations of the squeeze test and MRI data (data of same extremity at baseline) were studied with generalized estimating equations, to account for the fact that in every patient a hand and a foot was assessed. The association of the squeeze test with IA development was determined using Cox regression.
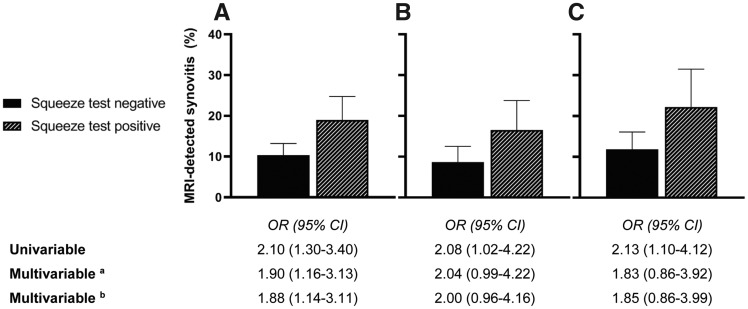
Flowchart and baseline characteristics are shown in the Supplementary material (Supplementary Fig. S1 and Supplementary Table S1, available at Rheumatology online). Fifty-one per cent of CSA patients had a positive squeeze test in MCP or MTP joints. In univariable analyses a positive test was associated with local subclinical synovitis [odds ratio (OR) 2.10 (95% CI 1.30–3.40), Fig. 1A] and tenosynovitis [OR 1.68 (95% CI 1.05–2.68); Supplementary Table S2, available at Rheumatology online]. In multivariable analyses including both inflammatory features only synovitis remained significant [OR 1.90 (95% CI 1.16–3.13), Fig. 1A], also after further correction for age and gender (Fig. 1A, Supplementary Table S2, available at Rheumatology online). Thus, a positive squeeze test is a measure of subclinical synovitis, with a sensitivity of 44% (95% CI 33–55%) and specificity of 72% (95% CI 68–76%). When analysing MCP and MTP joints separately, the squeeze test was also associated with subclinical synovitis [OR 2.08 (95% CI 1.02–4.22) and 2.13 (95% CI 1.10–4.12), respectively, in univariable analyses; Fig. 1B and C, Supplementary Table S2, available at Rheumatology online].
Fig. 1.
Squeeze test and MRI-detected synovitis in (A) MCP and MTP joints, (B) MCP joints and (C) MTP joints
Subclinical inflammation was considered present if the inflammatory feature was uncommon in symptom-free controls, i.e. present in <5% of symptom-free controls at the same location and in the same age category (<40, 40–59, ≥60). Error bars represent 95% CI. aAdjusted for tenosynovitis. bAdjusted for tenosynovitis, age and gender. OR: odds ratio.
A positive squeeze test in patients with CSA was not associated with IA development in Cox regression adjusted for age, gender, CRP and ACPA-status [hazard ratio (HR) 1.57 (95% CI 0.77–3.19); Supplementary Table S3, available at Rheumatology online]. This is consistent with the finding that subclinical synovitis was not associated with IA development in multivariable analysis adjusted for age, gender, CRP, ACPA status and subclinical tenosynovitis [HR 1.40 (95% CI 0.59–3.31)], whilst tenosynovitis was associated [HR 4.94 (95% CI 2.03–12.06); Supplementary Table S4, available at Rheumatology online].
The squeeze test is known for its association with synovitis in patients with clinically manifest arthritis. This study is the first to investigate the association with subclinical inflammation in the phase of CSA. We demonstrated that a positive test was indeed associated with presence of subclinical synovitis. The sensitivity was 44%; this indicates that subclinical synovitis was frequently missed by the squeeze test. For certainty on presence of subclinical synovitis imaging could be used. However, whilst MRI is more sensitive for detection of subclinical synovitis, it is also invasive and costly. In contrast, the squeeze test is easy to perform and free of costs, and therefore it can provide value as a first screening tool.
The squeeze test of the MCPs is, in combination with other clinical characteristics, part of the EULAR definition of arthralgia suspicious for progression to RA. This definition serves to identify this group of arthralgia patients and to distinguish them from arthralgia with other causes [7, 8].
A positive squeeze test within CSA was not significantly associated with IA development. This may seem counterintuitive, as we have shown that it is a test for subclinical synovitis and subclinical inflammation is predictive for IA. However, this is explained by the fact that the latter association is mainly driven by tenosynovitis, as was shown previously [3]. Also in current data synovitis was not significantly associated with IA development, in contrast to tenosynovitis.
In sum, the squeeze test is a simple test that, when positive in CSA, doubles the probability of presence of subclinical synovitis.
Funding: This work was supported by the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation programme (Starting grant, agreement No 714312), and the Dutch Arthritis Society.
Disclosure statement: The authors have declared no conflicts of interest.
Supplementary data
Supplementary data are available at Rheumatology online.
Supplementary Material
References
- 1. Firestein GS, Budd R, Gabriel SE, McInnes IB, O’Dell JR. Kelley’s textbook of rheumatology. Philadelphia, PA: Saunders/Elsevier, 2012. [Google Scholar]
- 2. van den Bosch WB, Mangnus L, Reijnierse M, Huizinga TW, van der Helm-van Mil AH. The diagnostic accuracy of the squeeze test to identify arthritis: a cross-sectional cohort study. Ann Rheum Dis 2015;74:1886–9. [DOI] [PubMed] [Google Scholar]
- 3. van Steenbergen HW, Mangnus L, Reijnierse M, Huizinga TW, van der Helm-van Mil AH. Clinical factors, anticitrullinated peptide antibodies and MRI-detected subclinical inflammation in relation to progression from clinically suspect arthralgia to arthritis. Ann Rheum Dis 2016;75:1824–30. [DOI] [PubMed] [Google Scholar]
- 4. van Steenbergen HW, van Nies JA, Huizinga TW, Bloem JL et al. Characterising arthralgia in the preclinical phase of rheumatoid arthritis using MRI. Ann Rheum Dis 2015;74:1225–32. [DOI] [PubMed] [Google Scholar]
- 5. Ostergaard M, Peterfy C, Conaghan P et al. OMERACT Rheumatoid Arthritis Magnetic Resonance Imaging Studies. Core set of MRI acquisitions, joint pathology definitions, and the OMERACT RA-MRI scoring system. JRheumatol 2003;30:1385–6. [PubMed] [Google Scholar]
- 6. Haavardsholm EA, Ostergaard M, Ejbjerg BJ, Kvan NP, Kvien TK. Introduction of a novel magnetic resonance imaging tenosynovitis score for rheumatoid arthritis: reliability in a multireader longitudinal study. Ann Rheum Dis 2007;66:1216–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. van Steenbergen HW, Aletaha D, Beaart-van de Voorde LJ et al. EULAR definition of arthralgia suspicious for progression to rheumatoid arthritis. Ann Rheum Dis 2017;76:491–6. [DOI] [PubMed] [Google Scholar]
- 8. Burgers LE, Siljehult F, Ten Brinck RM et al. Validation of the EULAR definition of arthralgia suspicious for progression to rheumatoid arthritis. Rheumatology (Oxford) 2017;56:2123–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.