Abstract
Objective
in elderly patients reduction and fixation of acetabular fractures showed poor outcomes in fracture patterns where cartilage comminution/impaction and/or femoral head dislocation are present; acute arthroplasty with standard uncemented hemispherical cups and posterior plating has been recently proposed, we report on its safety and effectiveness.
Methods
we used this technique to manage 67 displaced acetabular fracture but both column in patients older than 65 years old.
Results
fractures of posterior column and/or wall with severe cartilage involvement may be treated safely with acute THA.
Conclusions
Good results in complex fracture patterns may also be achieved.
Keywords: Acetabular fracture, THA, THR, ORIF, Plating, Fixation, Outcome, Quality of life
Highlights
-
•
Acute THA may be an option for displaced acetabular fracture in the elderly.
-
•
Hemispherical cups associated with posterior plating in selected patterns achieve good results.
-
•
Fixation should increase subsequent cup stability when fracture pattern impairs the peripheral grip of the cup.
-
•
The post-operative quality of life seems comparable to other traumatic surgeries, and even better than elective TKA.
-
•
No differences in terms of outcome have been reported between simple and complex fracture patterns.
1. Introduction
Acetabular fractures are commonly produced by high-energy traumas in young adults, nevertheless their incidence in people older than 60 years is constantly rising in the last two decades, reaching 25% of the total.1,2
The optimal treatment for displaced acetabular fractures is still widely debated along the hip surgeons. On one side, the classic conservative approach is performed through the open anatomical reduction and internal fixation (ORIF) of the joint, on the other hand acute total hip arthroplasty (THA) associated with reduction and fixation of the fracture may be a good option in selected patients. Acute THA may be preferred when fracture prognosis is poor with ORIF and a good stability of the THA components is achievable. Several specific factors involving both the patient (age, comorbidity) and the fracture patterns (comminution, impaction, fracture type, dislocation) were demonstrated as strictly related to the outcome of the ORIF. Hence, if a very poor prognosis is predictable, a selected group of patients can be effectively treated with acute hip replacement allowing a shorter time of no weight bearing and a better pain management.
Literature shows that THA performed for any traumatic reason use to behave significantly worse in terms of complications and durability, if compared to the elective surgery.3,4 However, only few studies focused on acute THA with hemispherical cups associated with posterior plating in acetabular fractures.2,5, 6, 7
Main aim of this study is to evaluate the safety and efficacy acute THA associated with posterior plating for a displaced acetabular fracture in patients older than 65 years old. Secondary aim was to compare the outcomes between fractures that involved only posterior wall and/or column (Fig. 1A–B) and fractures (that involved also the anterior column (transverse, T-shape, isolated anterior column, posterior column + hemitransverse anterior column) (Fig. 2A–B).
Fig. 1.
A. Preoperative xrays of a 79 years old male with a posterior wall fracture. B–C. Xrays at 5 years follow-up in anteroposterior and lateral views.
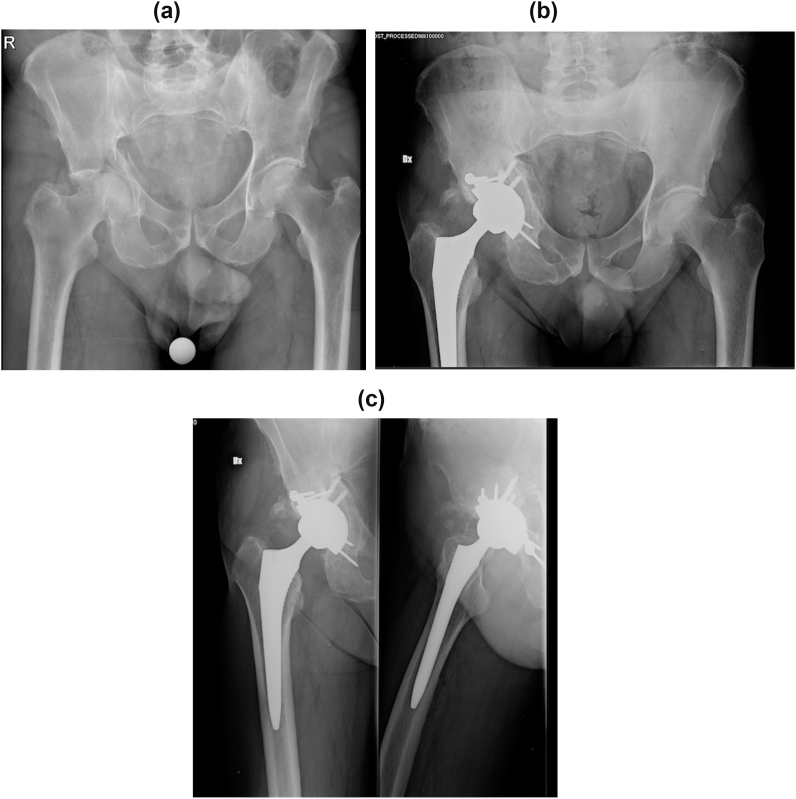
Fig. 2.
A. Preoperative xrays of an 82 years old male with T-shaped comminuted fracture B–C. Xrays at 2 years follow-up in anteroposterior and lateral views.
2. Patients and methods
The study was approved by the local ethical committee. Patients were asked to give their informed consent to the use of an unconventional technique when eligible.
Between 2013 and 2018, we used acute THA with/without posterior plating in all displaced fracture classified as posterior wall and/or column, transverse, T-shape, isolated anterior column, posterior column + hemitransverse anterior column that had poor prognosis of fracture according to Tannast's algorithm (chance of survival lower than 50% at 5 years).8 All those patients were included in this study if they were older than 65 years. Criteria of exclusion were: non operative cases, incomplete data and follow-up shorter than 6 months.
2.1. Methods
Medical records were reviewed and the following data were recorded: age, gender, date and time of admission to the emergency department (ER), height, weight, body max index (BMI) side of fracture (right or left), American Society of Anesthesiologists (ASA) score, medication before trauma, diagnosis (according to Letournel classification), associated lesions, Injury Severity Score (ISS), type of implant, date and time of surgery, surgical time, time for surgery, subsequent treatments, post-operative complications, length of hospitalization.9, 10, 11, 12
All patients were interviewed with Merle d’Aubigné and the EQ-5D-5L questionnaires regarding their actual and pre trauma conditions. We also investigated the incidence of post-discharge complications: patients were interviewed also about deep vein thrombosis, nerve palsies, pulmonary embolism, dislocations, infections and revisions.
2.2. Statistical analysis
All data were analyzed with standard descriptive statistics. Patients were classified in two groups: in group A were included all the fracture that involved only posterior wall and/or column while in group B all the fracture that involved also the anterior column (transverse, T-shape, isolated anterior column, posterior column + hemitransverse anterior column). Comparison between group A and B was performed with T test or Pearson's chi squared test according the type of analyzed variable. Groups were compared in terms of age, follow-up, surgical time, ASA score, postoperative EQ-5D-5L score, pre and post-operative Merlè D'aubigne score.
P values lower than 0.05 were considered statistically significant. All analyses were performed using Stata version 12 (Stata Corporation, College Station, Texas, USA).
2.3. Surgical technique
The ideal surgical approach should give a proper exposure of the acetabular cavity and facilitate the access to the peripheral structures, when fixation is needed. All patients were treated through a modified Kocher-Langenbeck approach and its less extensile modifications. The deep fascia was incised and the external rotators were exposed. Differently from the preservation surgery tendons were detached close to the greater trochanter. The femoral head was dislocated paying attention to avoid further dislocation of the fragments. The femoral head wasosteotomized and preserved as source for bone grafting. At this point a complete evaluation of the acetabular continence was performed and future acetabular coverage was estimated with the aid of a trial cup. The goal was to give a proper support to the cup. Posterior column and wall exposure is excellent with this approach, and reduction clamps could be easily positioned; a gross reduction was made while the articular surface congruence was overlooked. Single reconstruction plate with 3.5 mm cortical screws (Matta system, Stryker) was used, because it usually gives enough strength for fixation. If the fracture involved the anterior structures or had a transverse pattern with pelvic discontinuity, posterior double plating was used especially in osteoporotic patients, and when necessary, stability was increased with percutaneous screw in the anterior column; the anterior extension of the fracture was not fixed with a plate. If lamina's or anterior bone defect was present, autologous graft from the femoral head was used to prevent medial migration of the cup during impaction. All the patients were treated with standard hemispherical cups (R3 cup, Smith&Nephew) and press-fit uncemented standard stems (Polarstem, Smith&Nephew). No rings or cemented cups were used.
2.4. Standard intraoperative tests for cup stability were used
A standard protocol of 30 days of restricted weight-bearing was commonly applied, in order to promote some biological stabilization of the fracture. Combined hip flexion, adduction and internal rotation was restricted for 60 days. In marginal fractures with any involvement of the supporting structures of the acetabulum full weight-bearing was allowed.
3. Results
The initial cohort was composed by 67 patients. Five patients had a follow-up shorter than 1 year while seven patients were lost at follow-up. Mean follow-up was 27 months (range 6–53 months).
Mean age at surgery was 71 years (range 65–84). 39 patients (71%) were males, mean height was 1.69 m, mean weight was 71 kg, therefore mean BMI was 24.9 kg/m2. Mean ASA score was 2. Thirty patients were under medications at the time of trauma for other diseases.
Nine patients (24.2%) had an ISS>15 at arrival and were considered as multiple injured patients.
The fracture pattern distribution is shown in Table 1.
Table 1.
Fracture pattern distribution is shown.
| FRACTURE TYPE | NUMBER OF PATIENTS | PERCENTAGE |
|---|---|---|
| posterior wall | 21 | 38.2 |
| T type | 12 | 21.8 |
| Transverse | 9 | 16.4 |
| Transverse + posterior wall | 6 | 10.9 |
| isolated posterior column | 4 | 7.3 |
| posterior column plus anterior hemi-transverse | 2 | 3.6 |
| anterior column | 1 | 1.8 |
| TOTAL | 55 | 100.0 |
Three patients had an associated proximal femur fracture: two patients had a Pipkin type II femoral head fracture while one patient had a basicervical neck femur fracture.
Mean surgical time was 134 min (range 75–225 min).
In 26 patients THA implant was associated with a single plate fixation, in one patient two plates were used and in the remaining 23 patients no fixation devices were employed.
Mean length of hospitalization was 8.34 days (range 4–33 days).
Five patients had an impairment of sciatic nerve (10.53%): four lesions were present at arrival and did not recover while one was present only after surgery and fully recovered in 3 weeks.
One patient developed deep infection (2.63%) and treated with antibiotic therapy and surgical two-staged revision. One patient showed deep vein thrombosis in the peri-operative time (2.63%) successfully treated with medications.
One patient died during surgery because of pulmonary embolism.
Mean EQ-5D-5L score was 0.748 (range 0.049–1.000; CI 0.669–0.826).
Mean of pre operative Merle D'Aubignè score was 18 and mean score at follow-up was 15,84 (CI 14.91–16.77).
One patient reported a recurrent dislocation and successfully underwent a cup revision 6 months after surgery.
In one patient aseptic loosening of acetabular component was observed at two years and was successfully treated with acetabular revision.
Comparison between group A and B is shown in Table 2.
Table 2.
Comparison between group A (posterior wall and/or column) and group B (transverse, T-shape, isolated anterior column, posterior column + hemitransverse anterior column) is shown.
| GROUP A | GROUP B | p value | |
|---|---|---|---|
| age (years) | 70 | 71 | 0.8054 |
| mean follow-up (months) | 26 | 27 | 0.8909 |
| mean surgical time (minutes) | 100 | 156 | 0.0286* |
| ASA score | 2 | 2 | 0.8146 |
| preoperative Merlè D'aubigne score | 18 | 18 | not detectable |
| postoperative Merlè D'aubigne score | 15,2 | 16 | 0.4634 |
| postoperative EQ-5D-5L score | 0.67 | 0.77 | 0.2307 |
4. Discussion
The best treatment for displaced acetabular fractures in patients older than 65 years should be chosen according to several factors: patient's general condition, fracture prognosis, patient's expectations, need of rapid recovery and the risk of subsequent surgeries should be considered. The articular preservation should be pursued as far as possible, especially in younger and active patients. However, two main variables negatively influence the outcome of the ORIF: age and articular comminution.13 Elderly patients with acetabular cartilage impaction have the highest risk of failure.2,14 Furthermore, arthroplasties performed after an unsuccessful ORIF may be more challenging and burden by high rate of complications, mainly due to scar tissue and bone resorption.15, 16, 17 Our data suggest that acute THA with hemispherical cup associated with posterior plating (when necessary) is a good solution for those patients. Therefore, we routinely suggest hip replacement when a poor acetabular fracture prognosis is expected in patients over 65 years.
Our study confirms the result of previously published studies on acute THA implants: we agree that satisfying results may be obtained; however, the implants performances are poorer than elective THA.18
It is well known that the evaluation of post-traumatic patients is invariably affected by the pre-injury condition, so that healthy people use to experience a sensible decrease in their perceived quality of life after trauma, while for example arthritic patients will immediately improve their own status. Therefore, a direct standard comparison between an established procedure like elective THA with the acute post-traumatic THA may be heavily affected from this principle. Hence, we decided to apply a standardized measure of health-related quality of life, choosing the country specific EQ-5D-5L utility index, associated with a standard score as the Merle d’Aubignè.
The average post-operative EQ-5D-5L index found was 0.748. This value has to be referred to general population quality of life. If we consider the Italian norm data, adjusted for age (66-75y), the mean values for men and women were respectively 0.907 and 0.877.19,20 Our findings show that people underwent hip replacement for an acetabular fracture could have a moderate loss in quality of life, if compared to the general population. However, more accurate advices can be obtained if we look at the 12-months post-operatively values of the principal orthopedic surgeries. Elective THA shows a mean value of 0.8, which is close to our data. It's also interesting to notice that total knee arthroplasty show a postoperative value of 0.73, the same value of all the traumatic surgeries considered together. These findings suggest that the acute THA may result in a loss of quality of life if compared to the general population, but this reduction seems to be in line with other traumatic surgeries, and even moderately higher than people who sustained elective TKA.
When comparing the pre-op and post-op Merle d’Aubignè score, our data show a mean decrease of 2.16 points after acute THA, that is superior to the outcomes reported in literature with ORIF.21
Acetabular fixation prior to the cup positioning affected the surgeries duration; if this additional time wasn't performed the operation used to last slightly more than elective THA.
The complications rate found in our study is in line with the literature.22 Three patients required subsequent revision: one diabetic patient developed deep infection treated with two-stage revision, one patient had a recurrent dislocation treated with cup revision and one patient showed early cup mobilization due to fixation failure. The latter was revised with new fixation and cup repositioning. One patient had an intra-operative sciatic nerve palsy and fully recovered within four weeks from surgery.
Implants type should also be discussed: all patients were treated with common implants that are used routinely for elective surgery. The goal of the associated fixation techniques is to give an adequate peripheral stability for the press-fit cup, and its subsequent osteointegration. Therefore, according to our point of view, an interruption of the columns or a considerable involvement of the walls should be fixed with plate. No anatomical reduction is needed, but the main target is to achieve good stability. Sometimes femoral head autograft may be a valid option for reconstruction of segmental defects of the lamina or the anterior column. On the opposite, a minor engagement of the posterior wall, for example, may be treated as a standard THA implant.
Comparison between fractures that involved only posterior wall and/or column (Fig. 1A–B) and fractures that involved also the anterior column (transverse, T-shape, isolated anterior column, posterior column + hemitransverse anterior column) (Fig. 2A–B) did not show statistically significant differences but surgical time. Surgical time may be longer in more complex fracture often due to the challenging reduction. On the other hand, we did not found differences in the outcomes between easier and more complex fractures.
The main limits of this study are the retrospective nature, the relatively small cohort and the limited follow-up. On the other hand, only few studies reported on the safety and efficacy of this technique.
5. Conclusion
This study confirms that fractures of the posterior column and/or wall may be treated safely with acute THA in elderly patients with severe cartilage involvement, and clinical results appear to be in line with literature. We think that acute THA should be considered also for transverse, T-type, isolated anterior column, posterior column + anterior hemitransverse in eldery patients although relevant surgical skills are requested.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jor.2020.09.012.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Walley K.C., Appleton P.T., Rodriguez E.K. Comparison of outcomes of operative versus non-operative treatment of acetabular fractures in the elderly and severely comorbid patient. Eur J Orthop Surg Traumatol. 2017;27(5):689–694. doi: 10.1007/s00590-017-1949-1. [DOI] [PubMed] [Google Scholar]
- 2.Ferguson T.A., Patel R., Bhandari M., Matta J.M. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Jt Surg Br Vol. 2010;92(2):250–257. doi: 10.1302/0301-620X.92B2.22488. [DOI] [PubMed] [Google Scholar]
- 3.Morison Z., Moojen D.J.F., Nauth A. Total hip arthroplasty after acetabular fracture is associated with lower survivorship and more complications. Clin Orthop Relat Res. 2016;474(2):392–398. doi: 10.1007/s11999-015-4509-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schnaser E., Scarcella N.R., Vallier H.A. Acetabular fractures converted to total hip arthroplasties in the elderly. J Orthop Trauma. 2014;28(12):694–699. doi: 10.1097/bot.0000000000000145. [DOI] [PubMed] [Google Scholar]
- 5.Rickman M., Young J., Bircher M., Pearce R., Hamilton M. The management of complex acetabular fractures in the elderly with fracture fixation and primary total hip replacement. Eur J Trauma Emerg Surg. 2012;38(5):511–516. doi: 10.1007/s00068-012-0231-9. [DOI] [PubMed] [Google Scholar]
- 6.Salama W., Mousa S., Khalefa A. Simultaneous open reduction and internal fixation and total hip arthroplasty for the treatment of osteoporotic acetabular fractures. Int Orthop. 2017;41(1):181–189. doi: 10.1007/s00264-016-3175-6. [DOI] [PubMed] [Google Scholar]
- 7.Ortega-Briones A., Smith S., Rickman M. Acetabular fractures in the elderly: midterm outcomes of column stabilisation and primary arthroplasty. BioMed Res Int. 2017;2017:4651518. doi: 10.1155/2017/4651518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tannast M.M., Najibi S.S., Matta J.M. Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J Bone Joint Surg Am. 2012;94(17):1559–1567. doi: 10.2106/JBJS.K.00444. [DOI] [PubMed] [Google Scholar]
- 9.Keys A., Fidanza F., Karvonen M., Kimura N., Taylor H. Indices of relative weight and obesity (1972) Int J Epidemiol. 2014;43(3):655–665. doi: 10.1093/ije/dyu058. http://www.sciencedirect.com/science/article/pii/0021968172900276 Retrieved from. [DOI] [PubMed] [Google Scholar]
- 10.American Society of Anesthesiologists ASA physical status classification system. https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system
- 11.Letournel E. Acetabulum fractures: classification and management. Clin Orthop Relat Res. 1980;(151):81. [PubMed] [Google Scholar]
- 12.Baker S.P., O'Neill B., Haddon W., Long W.B. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. Mar 1974;14(3):187–196. PMID 4814394. [PubMed] [Google Scholar]
- 13.Liebergall M., Mosheiff R., Low J., Goldvirt M., Matan Y., Segal D. Acetabular fractures. Clinical outcome of surgical treatment. Clin Orthop Relat Res. 1999;366:205–216. [PubMed] [Google Scholar]
- 14.Jansson K.Å., Granath F. Health-related quality of life (EQ-5D) before and after orthopedic surgery. Acta Orthop. 2011;82(1):82–89. doi: 10.3109/17453674.2010.548026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stibolt R.D., Patel H.A., Huntley S.R., Lehtonen E.J., Shah A.B., Naranje S.M. Total hip arthroplasty for posttraumatic osteoarthritis following acetabular fracture: a systematic review of characteristics, outcomes, and complications. Chinese Journal of Traumatology - English Edition. 2018;21(3):176–181. doi: 10.1016/j.cjtee.2018.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giannoudis P.V., Grotz M.R., Papakostidis C., Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br. 2005;87:2–9. [PubMed] [Google Scholar]
- 17.Romness D.W., Lewallen D.G. Total hip arthroplasty after fracture of the acetabulum. Long-term results. J Bone Joint Surg Br. 1990;72:761–764. doi: 10.1302/0301-620X.72B5.2211750. [DOI] [PubMed] [Google Scholar]
- 18.Jauregui J.J., Clayton A., Kapadia B.H., Cherian J.J., Issa K., Mont M.A. Total hip arthroplasty for acute acetabular fractures: a review of the literature. Expet Rev Med Dev. 2015;12(3):287–295. doi: 10.1586/17434440.2015.1009828. [DOI] [PubMed] [Google Scholar]
- 19.Jansson K.Å., Granath F. Health-related quality of life (EQ-5D) before and after orthopedic surgery. Acta Orthop. 2011;82(1):82–89. doi: 10.3109/17453674.2010.548026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scalone L., Cortesi P.A., Ciampichini R., Cesana G., Mantovani L.G. Health related quality of life norm data of the general population in Italy: results using the EQ-5D-3L and EQ-5D-5L instruments. Epidemiology Biostatistics and Public Health. 2015;12(3) doi: 10.2427/11457. [DOI] [Google Scholar]
- 21.Giunta J.C., Tronc C., Kerschbaumer G. Outcomes of acetabular fractures in the elderly: a five year retrospective study of twenty seven patients with primary total hip replacement. Int Orthop. 2019 Oct;43(10):2383–2389. doi: 10.1007/s00264-018-4204-4. [DOI] [PubMed] [Google Scholar]
- 22.Kg M., Obakponovwe O., Bobak P., Pv G. Total hip arthroplasty after acetabular fracture: incidence of complications. World J Orthoped. 2014;5(3):336–343. doi: 10.1016/j.arth.2014.06.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.