Abstract
A 68-year-old woman presented with a 2-year history of worsening unsteady gait. Her neurological examination revealed peripheral neuropathy with lower limb sensory dominance. T2-weighted imaging revealed a disorder of the posterior cervical cord. Blood test findings revealed vitamin B12 deficiency, and gastroscopy revealed typical findings of autoimmune gastritis. She received vitamin B12 supplementation, but some peripheral neuropathy symptoms persisted due to longstanding vitamin B12 deficiency. Asymptomatic patients should undergo gastroscopy to detect autoimmune gastritis, as chronic vitamin B12 deficiency causes irreversible peripheral neuropathy.
Keywords: autoimmune gastritis, vitamin B12 deficiency, subacute combined degeneration of spinal cord, peripheral neuropathy
Introduction
Chronic atrophic gastritis is classified into two types: corporal autoimmune gastritis (type A gastritis) and antral atrophic gastritis associated with Helicobacter pylori infection (type B gastritis). The clinical characteristics of autoimmune gastritis are as follows: fundic gland atrophy, achlorhydria, hypergastrinemia, carcinoid tumors, vitamin B12 deficiency, anemia, and autoimmunity due to anti-gastric parietal cell antibody (1,2). Autoimmune gastritis is the primary cause of vitamin B12 deficiency. Vitamin B12 deficiency in autoimmune gastritis is caused by a deficiency of gastric intrinsic factor, which is produced in the gastric mucosa and is essential for the absorption of vitamin B12 in the ileum. Gastric intrinsic factor deficiency occurs because of massive atrophy of the corporal fundic mucosa and autoimmunity via anti-intrinsic factor antibodies (3).
Vitamin B12 is essential for nucleic acid synthesis in the erythrocytes and nerve cells; hence, its deficiency may cause anemia or neuropathy (4). If the diagnosis and treatment of neuropathy caused by vitamin B12 deficiency are delayed, the neuropathy may become irreversible (5).
We herein report the rare case of a patient who experienced subacute combined degeneration of the spinal cord caused by chronic vitamin B12 deficiency due to autoimmune gastritis.
Case Report
A 68-year-old Japanese woman with no medical history had experienced unsteady gait starting 2 years prior to presentation, and her symptoms had been worsening. When she visited our hospital, she could not walk without help.
Her neurological examination findings were as follows: loss of bilateral lower limb deep tendon reflexes, thermal nociception in both feet, and loss of pallesthesia. Her body swung significantly in the standing position, and she had a small stride with left and right swaying when walking. Nerve conduction studies revealed disorders in the conduction velocity of both motor nerves (the right ulnar and bilateral tibial and peroneal nerves) and sensory nerves (the right median and bilateral tibial and peroneal nerves). These findings indicated peripheral neuropathy with lower limb sensory dominance. Head and neck magnetic resonance imaging showed high-intensity areas in the posterior cervical cord at C2 through C6 on T2-weighted images, which are typical findings of subacute combined degeneration of the spinal cord (Fig. 1A). Thyroid enlargement was also revealed in the same examination (Fig. 1B). Her blood test findings revealed a vitamin B12 deficiency, which we considered to be the likely cause of her peripheral neuropathy. Furthermore, her anti-thyroid peroxidase antibody and thyroglobulin levels were elevated, although the thyroid-stimulating hormone and free T4 levels were almost within the reference range. Gastroscopy findings revealed massive atrophy in the corporal area locally. There were no findings suggesting gastric cancer or carcinoid (Fig. 2).
Figure 1.
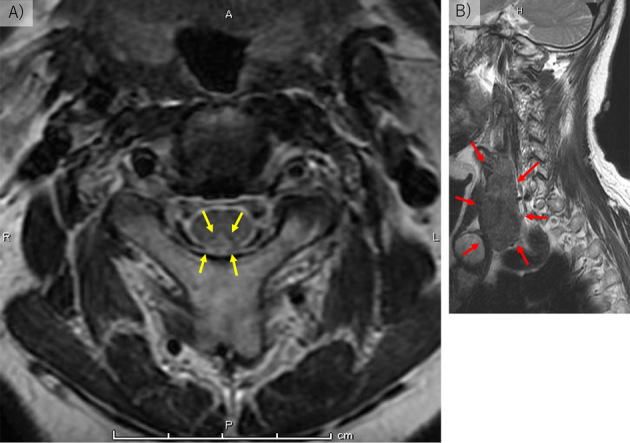
Head and neck magnetic resonance imaging. A: T2-weighted images showing high-intensity areas in the posterior areas at C2 through C6 (yellow arrows). B: Thyroid enlargement (red arrows).
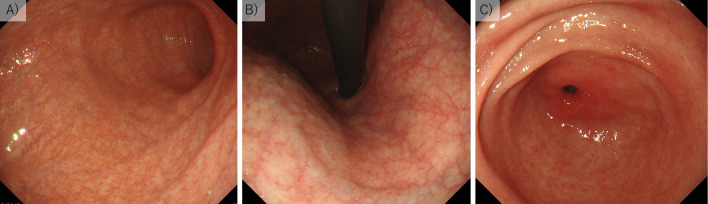
Figure 2.
Gastroscopy findings. A and B: Massive atrophic gastritis at the fundic gland area of the stomach. C: Absence of atrophic gastritis at the gastric antrum. These are typical findings of autoimmune gastritis. There was no evidence of gastric cancer or carcinoid.
An immediate urease test (PyloriTek; Sekisui Medical, Tokyo, Japan) for Helicobacter pylori infection and an anti-Helicobacter pylori antibody test (E-Plate Eiken H pylori antibody; Eiken, Tokyo, Japan) were both negative. The test for anti-gastric parietal cell antibodies was positive, and that for anti-intrinsic factor was negative. Blood gastrin levels had increased significantly (>3,000 pg/mL). Her detailed blood test results are shown in Table 1. She had no digestive symptoms and had not taken any stomach medicine (including proton pump inhibitors). She had never undergone esophagogastroduodenoscopy before this investigation.
Table 1.
Detailed Blood Test Results.
| Items (unit) | Measured value | Reference value range in Osaka Medical College Hospital | ||
|---|---|---|---|---|
| White blood cell counts (/µL) | 4,490 | 3,300-8,600 | ||
| Red blood cell counts (/µL) | 302×104* | 386-492×104 | ||
| Hemoglobin (g/dL) | 11.2* | 11.6-14.8 | ||
| Mean corpuscular value (fL) | 109.8* | 83.6-98.2 | ||
| Mean corpuscular hemoglobin (pg) | 37.3* | 27.5-33.2 | ||
| Platelet count (/µL) | 16.3×104 | 15.8-34.8×104 | ||
| Anti-gastric parietal cell antibody | 40×* | negative | ||
| Anti-intrinsic factor antibody | negative | negative | ||
| Vitamin B12 (pg/mL) | <50*† | 180-914 | ||
| Folic acid (ng/mL) | 13.7 | >4.0 | ||
| Anti-Helicobacterpylori antibody (U/mL) | <3† | <10 | ||
| Thyroid stimulating hormone (µIU/mL) | 3.430 | 0.500-5.000 | ||
| Free T4 (ng/dL) | 0.81* | 0.90-1.70 | ||
| Anti-thyroid peroxidase antibody (IU/mL) | 170* | <16 | ||
| Thyroglobulin (ng/mL) | 501.90* | 1.40-78.00 | ||
| Gastrin (pg/mL) | >3,000 *† | <200 | ||
| Anti-glutamic acid decarboxylase antibody (U/mL) | <5.0 | <5.0 |
*: outside the reference range; †: outside the range of detection
Our final diagnoses were as follows: 1) autoimmune gastritis, 2) vitamin B12 deficiency, 3) subacute combined degeneration of the spinal cord, and 4) chronic thyroiditis. She was treated with 1,500 μg/day of methylcobalamin orally every day and 500 μg intramuscularly every 3 months; however, some symptoms of peripheral neuropathy persisted because of the long duration of vitamin B12 deficiency before the treatment was initiated.
Discussion
In this report, autoimmune gastritis and its subsequent complications were diagnosed in our patient; this is a very rare case. A few studies have reported cases with similar conditions in other countries (6-8). To our knowledge, this was the third paper reporting such a case from Japan. The previous reports were a case of autoimmune gastritis with an extremely unbalanced diet (9) and a case of autoimmune gastritis coexisting with gastric cancer (10); thus, this present case is the first from Japan in which autoimmune gastritis alone caused subacute degeneration of the spinal cord.
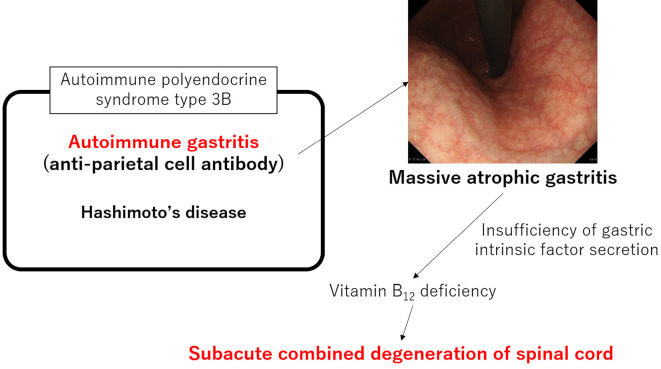
Although we have experience with cases of peripheral nerve disorders caused by vitamin B12 deficiency, it is rare to see a case of disorders of the posterior cervical cord associated with autoimmune gastritis. The diagnostic criteria for autoimmune gastritis have not yet been clearly defined. In the present case, we diagnosed the autoimmune gastritis based on the following findings: gastroscopic findings (massive atrophy in the corporal area locally), positive anti-gastric parietal cell antibody test, and hypergastrinemia. Furthermore, the patient had autoimmune polyendocrine syndrome (APS) as an underlying condition. APS is a syndrome in which an autoimmune thyroid disease, such as Hashimoto’s disease (chronic thyroiditis) or Graves' disease (Basedow's disease), is associated with other autoimmune endocrine disorders as well as non-endocrine autoimmune diseases (Table 2). The present case fit APS type 3B, as Hashimoto's disease was complicated with autoimmune gastritis. Fig. 3 shows the mechanism involved in the present case.
Table 2.
Types of Autoimmune Polyendocrine Syndrome.
| Type | Associated diseases |
|---|---|
| Type 1 | Hashimoto’s disease or Graves’s disease, Addison’s disease, hypoparathyroidism, and chronic mucocutaneous candidiasis |
| Type 2 (Schmidt’s syndrome) | Hashimoto’s disease or Graves’s disease, and Addison’s disease |
| Carpenter’s syndrome | Hashimoto’s disease or Graves’s disease, Addison’s disease, and type 1 diabetes mellitus |
| Type 3A | Hashimoto’s disease or Graves’s disease, and type 1 diabetes mellitus |
| Type 3B | Hashimoto’s disease or Graves’s disease, and autoimmune gastritis |
| Type 3C | Hashimoto’s disease or Graves’s disease, and autoimmune hemolytic anemia or immune thrombocytopenia |
Figure 3.
Mechanism underlying the subacute combined degeneration of the spinal cord caused by autoimmune gastritis, as reported in this case.
The causes of vitamin B12 deficiency can be divided into three classes: nutritional deficiency; malabsorption syndromes; and other gastrointestinal causes, specifically post-gastrectomy, atrophic gastritis, extreme vegetarianism, pregnancy, and ileocecal lesions (5). In addition, the long-term use of a proton pump inhibitor has been reported to cause vitamin B12 deficiency because of malabsorption (11).
The mechanism underlying vitamin B12 deficiency caused by atrophic gastritis, which is similar to the present case, is thought to be insufficiency of gastric intrinsic factor secretion from parietal cells. When massive atrophic gastritis (including autoimmune gastritis) is detected, vitamin B12 deficiency should be suspected. Autoimmune gastritis is not a rare disease; the prevalence of autoimmune gastritis in asymptomatic individuals undergoing medical checkups has been reported recently to be 0.49% in Japan (12). However, this disease is easily missed by endoscopists with little experience. In the present case, if the patient had undergone screening gastroscopy as part of a medical checkup, had been diagnosed with autoimmune gastritis, and had initiated treatment for vitamin B12 deficiency at an early stage, she might not have suffered any aftereffects. Although some autoimmune gastritis patients without vitamin B12 deficiency have been reported, monitoring vitamin B12 in the blood serum may still be necessary for such patients.
When esophagogastroduodenoscopy is performed as part of a routine medical checkup in asymptomatic people, whether or not autoimmune gastritis is present should be investigated. The early diagnosis of autoimmune gastritis, before it causes vitamin B12 deficiency, may prevent irreversible neuropathy.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Strickland RG, Mackay IR. A reappraisal of the nature and significance of chronic atrophic gastritis. Am J Dig Dis 18: 426-440, 1973. [DOI] [PubMed] [Google Scholar]
- 2.Okazaki K, Ohana M, Oshima C, et al. Interaction of Helicobacter pylori-induced follicular gastritis and autoimmune gastritis in BALB/c mice with post-thymectomy autoimmune gastritis. J Gastroenterol 38: 1131-1137, 2003. [DOI] [PubMed] [Google Scholar]
- 3.Stabler SP. Clinical practice. Vitamin B12 deficiency. N Engl J Med 368: 149-160, 2013. [DOI] [PubMed] [Google Scholar]
- 4.Lam JR, Schneider JL, Zhao W, Corley DA. Proton pump inhibitor and histamine 2 receptor antagonist use and vitamin B12 deficiency. JAMA 310: 2435-2442, 2013. [DOI] [PubMed] [Google Scholar]
- 5.Oh R, Brown DL. Vitamin B12 deficiency. Am Fam Physician 67: 979-986, 2003. [PubMed] [Google Scholar]
- 6.Sun W, Li G, Lai Z, et al. Subacute combined degeneration of the spinal cord and hydrocephalus associated with vitamin B12 deficiency. World Neurosurg 128: 277-283, 2019. [DOI] [PubMed] [Google Scholar]
- 7.Zhang N, Li RH, Ma L, et al. Subacute combined degeneration, pernicious anemia and gastric neuroendocrine tumor occured simultaneously caused by autoimmune gastritis. Front Neurosci 13: 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hughes JW, Muegge BD, Tobin GS, et al. High-risk gastric pathology and prevalent autoimmune diseases in patients with pernicious anemia. Endocr Pract 23: 1297-1303, 2017. [DOI] [PubMed] [Google Scholar]
- 9.Shibuki T, Kawazoe H, Tominaga N, et al. A case of subacute combined degeneration of spinal cord due to autoimmune gastritis with an extreme unbalanced diet. Intern Med NAIKA (Nankodo) 116: 895-899, 2015. [Google Scholar]
- 10.Hirata A, Nomoto N, Konno S, et al. Subacute combined degeneration of the spinal cord concomitant with gastric cancer. Intern Med 45: 875-877, 2006. [DOI] [PubMed] [Google Scholar]
- 11.Marcuard SP, Albernaz L, Khazanie PG. Omeprazole therapy causes malabsorption of cyanocobalamin (vitamin B12). Ann Intern Med 120: 211-215, 1994. [DOI] [PubMed] [Google Scholar]
- 12.Notsu T, Adachi K, Mishiro T, et al. Prevalence of autoimmune gastritis in individuals undergoing medical checkups in Japan. Intern Med 58: 1817-1823, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]