The coronavirus disease 2019 (COVID-19) pandemic has significantly impacted the well-being of children as a result of the widespread closure of schools. Throughout the summer, states have allowed the reopening of many businesses, including restaurants, bars, retail locations, and amusement parks, including in locations experiencing surges in cases. Meanwhile, many school districts across the country began the fall semester in a partially or completely virtual fashion.
A growing body of evidence suggests a return to in-person learning can be accomplished safely, particularly for young children. Throughout the pandemic, childcare centers serving school-age children have successfully operated without significant outbreaks, even in high prevalence areas.1 , 2 In other countries where school has been in session, reports of cases of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection in schools generally show little to no secondary spread.3 Initial evidence suggests that the school environment does not contribute to community transmission of the novel coronavirus in the same way that it does for other respiratory viruses such as influenza.4 When outbreaks have occurred among school-age children, these have generally reflected a lack of adherence to recommended mitigation strategies.5
National organizations have issued guidance on how to safely return to school in the fall of 2020.6 , 7 Key recommended elements include daily symptom screening, physical distancing, cohorting, masking for students and staff, enhanced hand hygiene, directed environmental cleaning, increased ventilation, and careful tracking of student locations and contacts to enable contact identification when an infectious case is identified. The ability of individual schools to implement these strategies is likely to vary based on school size, age of students, financial resources, community support, and access to consultation with health experts.
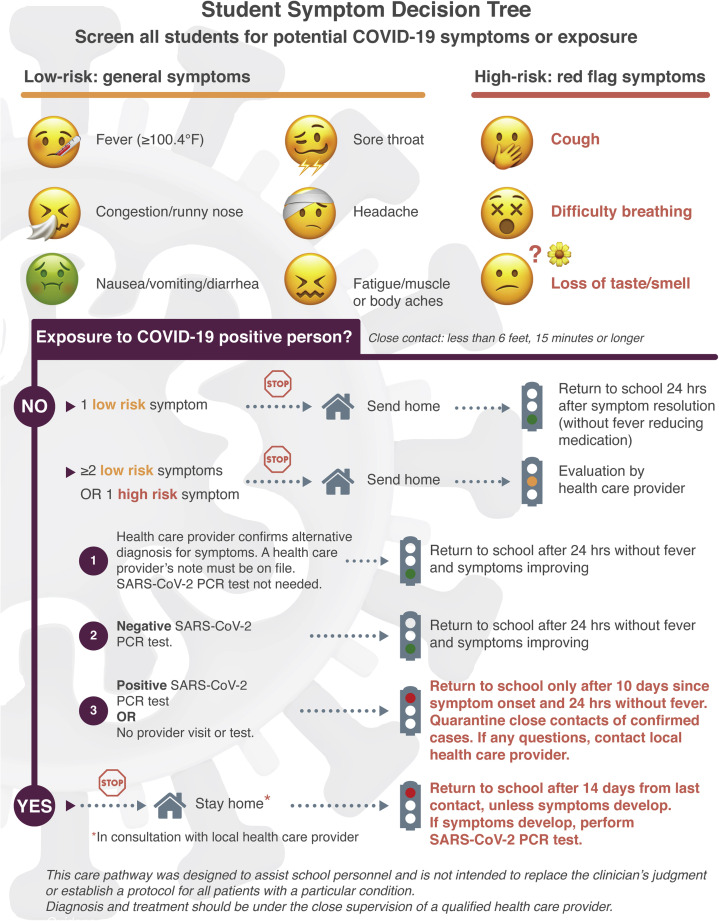
To provide support to our local school community, a group of pediatric infectious diseases experts and pediatric healthcare providers (MD/DO and nurse practitioners) collaborated to develop a series of algorithms addressing aspects of COVID-19 and schools (Figure and http://wupaarc.wustl.edu/COVID-19-and-Children/Algorithms-for-Clinicians-and-Schools). Included in the algorithms are a symptom decision tree for parents, students, and administrators; an algorithm for school nurses; protocols to assist in school contact tracing; and detailed algorithms for healthcare providers on how to approach students with SARS-CoV-2 symptoms or exposure. The goal of these algorithms is to provide practical guidance for children experiencing symptoms and the algorithms represent a balancing act between excluding potentially infectious students from the school environment and the educational disruption experienced by students who are kept out of the classroom.
Figure.
Student symptom decision tree. PCR, polymerase chain reaction.
Three algorithms on the site (one for parents, one for school personnel, and one for healthcare providers) address symptomatic illness in schoolchildren. Many of the symptoms of infection with SARS-CoV-2 overlap with the clinical presentation of other more common infections of childhood. However, some symptoms may be more specific to COVID-19 (anosmia and ageusia), more serious (difficulty breathing), or may be more likely to lead to transmission (cough). Thus, the student symptom decision tree labels cough, difficulty breathing, or loss of taste or smell as high risk. These symptoms should always require a visit with a healthcare provider and/or a test for SARS-CoV-2. Students with other single symptoms, such as headache or diarrhea, likely can be observed for resolution of symptoms without the need for a dedicated SARS-CoV-2 nasopharyngeal swab test. However, should students exhibit multiple or persistent symptoms, this should also prompt evaluation by a healthcare provider and/or testing for SARS-CoV-2.
The last algorithm provides an approach to a positive case occurring in a school. Careful identification of close contacts of an infectious case protects the school community by decreasing the chances of secondary transmission and should be viewed as a public health success when tracing and action occur in a timely fashion. Only excluding students who are close contacts, rather than dismissing entire classes or schools, decreases the number of students who experience educational disruption and should be the goal of careful contact identification.
One key component of returning children to the classroom and the practical functionality of these algorithms is readily available and timely SARS-CoV-2 testing and resulting action. As pediatricians encounter children brought to their offices with just a day or two of nonspecific respiratory symptoms, generally it will not be possible to distinguish between SARS-CoV-2 and other viral infections. In this case, if pediatricians are able to obtain accurate molecular testing for SARS-CoV-2 with results in 1-3 days, children can confidently return to school when symptom free, knowing they are unlikely to transmit this virus to others. Additional in-office antigen testing may also play an important role in returning children to the classroom in an expedited fashion, but one must consider the false-positive rates of the currently available tests in rendering decisions. Until the performance of such tests in children at low risk of SARS-CoV-2 infection is established, it may be advisable to consider a positive result as indeterminate (ie, not leading to action) until confirmation by a polymerase chain reaction test. The local availability and timeliness of testing will undoubtedly impact the effectiveness of these algorithms.
Overall, these algorithms provide practical guidance to students, parents, school nurses, administrators, and community pediatricians. They foster confidence in the school community that there is a plan in place to deal with these complex situations. Of course, we must be adaptable as more is learned about this particular virus, available testing and resources, and the practical application of these guidelines. A national mechanism to collect data on the usage and effectiveness of these algorithms, perhaps through the Clinical and Translational Science Awards network or the American Association of Pediatrics, could prove useful in continuing to support schools as healthy places as more and more students return to in-person learning. Additionally, real-time evaluation of the effectiveness of these algorithms must occur in partnership with our schools and local pediatric healthcare providers to crystallize the new knowledge obtained as children return to in-person schooling. This novel coronavirus will be with us for years to come. These plans are the first of many steps in balancing the health and education of our children.
Acknowledgments
We thank the Washington University Pediatric and Adolescent Ambulatory Research Consortium (WU PAARC) for their discussions in the formation of these algorithms. We also thank Dan Cooper, MD, the UC Irvine—Children's Hospital of Orange County Healthy School Restart Working Group, the Orange County Health Care Agency (OCHCA), and Michelle DeHaven, RN.
Footnotes
Funded by the NIHNCATSCTSA (UL1 TR001414 [to Dan Cooper, MD at UC Irvine]) for the development and illustration of the student screening algorithm. The NIH had no role in the development of these algorithms. The authors declare no conflicts of interest.
References
- 1.Link-Gelles R., Dellagrotta A.L., Molina C., Clyne A., Campagna K., Lanzieri T.M. Limited secondary transmission of SARS-CoV-2 in child care programs — Rhode Island, June 1–July 31, 2020. MMWR. 2020;69:2019–2021. doi: 10.15585/mmwr.mm6934e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kamenentz A., (NPR) What parents can learn from child care centers that stayed open during lockdowns. www.npr.org/2020/06/24/882316641/what-parents-can-learn-from-child-care-centers-that-stayed-open-during-lockdowns
- 3.Yung C.F., Kam K., Nadua K.D., Chong C.Y., Tan N.W.H., Li J., et al. Novel coronavirus 2019 transmission risk in educational settings. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa794. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Viner R.M., Russell S.J., Croker H., Packer J., Ward J., Stansfield C., et al. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health. 2020;4:397–400. doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stein-Zamir C., Abramson N., Shoob H., Libal E., Bitan M., Cardash T., et al. A large COVID-19 outbreak in a high school 10 days after schools' reopening, Israel, May 2020. Euro Surveill. 2020;25:2001352. doi: 10.2807/1560-7917.ES.2020.25.29.2001352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Center for Disease Control and Prevention, “Operating Schools during COVID-19: CDC’s Considerations.” https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/schools.html. Accessed October 6, 2020.
- 7.American Academy of Pediatrics, “COVID-19 Planning Considerations: Guidance for School Re-Entry.” https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/covid-19-planning-considerations-return-to-in-person-education-in-schools/. Accessed October 6, 2020.