Abstract
Left ventricular free wall rupture is one of the mechanical complications of acute myocardial infarction and it may result in cardiac tamponade as well as limiting itself by forming a pseudoaneurysm. In this report, a case of left ventricular free wall rupture and pseudoaneurysm that developed during the course of posterior myocardial infarction has been presented. Left ventricular free wall rupture and pseudoaneurysm were identified by three-dimensional transthoracic echocardiography and surgically repaired at a late stage.
Keywords: 3D echocardiography, acute myocardial infarction, complication, free wall rupture
Introduction
Left ventricular free wall rupture (LVFWR) is a rare but frequently fatal complication that may develop during the course of an acute myocardial infarction (AMI). Free wall rupture requires specific diagnostic, follow-up and therapeutic procedures. In this report, the diagnostic and therapeutic approaches including 3-D (three-dimensional) transthoracic echocardiography, primary percutaneous coronary artery intervention and late-stage pseudoaneurysm surgery have been presented for a case of subacute free wall rupture that developed during the course of a posterior myocardial infarction.
Case Report
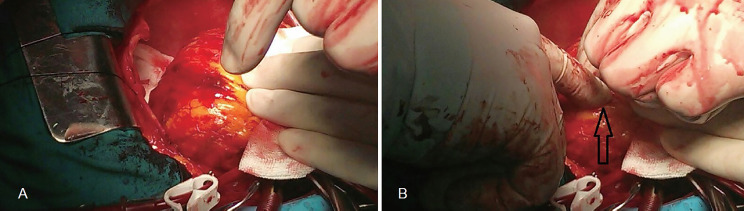
A 57-years old female patient with no previous history of cardiac disease was admitted to the coronary intensive care unit with the diagnosis of unstable angina pectoris. Her blood pressure was 110/70 mmHg and heart rate was 75/min. Electrocardiography (ECG) showed sinus rhythm and T inversion in leads D1 and aVL. Patient’s chest pain got better with medical therapy and she was not taken to emergency coronary angiography. Troponin I levels were normal at the 6th hour (troponin I: 0.02 ng/mL). Transthoracic Echocardiography (TTE) did not reveal any pathological finding. Eleven hours after admission, the patient once more experienced compressive and stabbing chest pain and became hemodynamically unstable. Her blood pressure was 85/45 mmHg and heart rate was 135/min. ECG showed ST segment depression in leads V1-V4, ST segment elevation of 2 mm in the posterior leads and minimal ST segment elevation in the lateral leads. Two-dimensional TTE demonstrated severe hypokinesis of the posterior and lateral segments, as well as mild to moderate pericardial effusion. There was no sign of cardiac tamponade. Three-dimensional TTE showed that posterior apical segment of the left ventricle was not continuous and a pseudoaneurysm was formed in this region (Vedio 1,2). The patient was immediately transferred to the coronary angiography (CAG) laboratory. CAG showed that the obtuse marginal coronary artery was totally obstructed, whereas no significant lesion was noted in the other coronary arteries. Blood flow was reestablished in the obtuse marginal coronary artery by primary percutaneous coronary intervention. During her hospitalization, the patient had been administered 300 mg acetylsalicylic acid and 300 mg clopidogrel orally, and she had received 6,000 IU subcutaneous enoxaparin injection 3 hours before the procedure. No additional antiaggregant or anticoagulant therapy was administered during the procedure. The patient’s chest pain disappeared and hemodynamics stabilized shortly after the procedure. ECG returned to normal. She was not administered anticoagulants during follow-up and her treatment was maintained by 100 mg/day acetylsalicylic acid and 75 mg/day clopidogrel. Troponin I level was 25.64 ng/mL during follow-up. The patient was monitored at the hospital for 22 days without any complication and later she was operated for pseudoaneurysm (linear suture of the pseudoaneurysm site) at the cardiovascular surgery department (Figure 1). Her follow-up 2-D and 3-D TTE examinations were normal (Video 3). The clinical course after hospital discharge is smooth without any cardiac complaints.
Figure 1. Intraoperative apical view of the pseudoaneurysm.
Video 1. Rupture and pseudoaneurysm formation in the apical segment of the left ventricle.
Video 2. Rupture and pseudoaneurysm formation in the apical segment of the left ventricle.
Video 3. Apical segment view after cardiac pseudoaneurysm surgery.
Discussion
LVFWR is a fatal complication that develops in 1-4% of the patients referring with AMI.[1] It is most commonly seen in women who had experienced their first transmural infarction. Additional risk factors include older age and hypertension that is not accompanied by hypertrophy.[2] It frequently develops between 3 to 6 days after an MI. However, LVFWR may also develop within the first few minutes following an AMI or even one month later.[3-5] The mechanism underlying rupture of the heart muscle is still controversial; it has been suggested to be due to the dissociation of the non-contractile infarcted region from the surrounding healthy and contractile region.[6]
Based on its clinical course, LVFWR is classified into three types as acute, subacute and chronic. Acute rupture results in death within minutes, due to massive bleeding into the pericardial cavity and tamponade. In case of subacute rupture, leakage to the pericardial cavity is limited by clots or pericardial adhesions. Clinically, patients with subacute rupture may represent with typical chest pain and be hemodynamically stable, but they may also be seen at the stage of irreversible cardiogenic shock. In case of chronic rupture, blood flow to the pericardial cavity is prevented by the pericardium through formation of a pseudoaneurysm.[7] Subacute and chronic ruptures may be surgically treated. The case of rupture presented in this report was subacute at onset, and became a chronic rupture with pseudoaneurysm formation during its clinical course.
Left ventricular pseudoaneurysm is defined as rupture of the myocardium. It is less common than a true aneurysm. Unlike a true aneurysm, the wall of the pseudoaneurysm is formed by thrombi and enveloping pericardial tissue with a narrow neck. The wall of a pseudoaneurysm lacks myocardial elements.[8] Two-dimensional TTE demonstrates the presence of pericardial fluid; however it is not successful in showing the localization of left ventricular rupture.[9] 3-D TTE, on the other hand, provides valuable information on the localization, orifice geometry and dimensions of the pseudoaneurysm.[10,11] Characterization of pseudoaneurysm by 3-D TTE serves as a guide during surgical procedures. In the case presented here, the localization and geometry of rupture could only be demonstrated by 3-D TTE.
Because of its propensity to rupture, it has been generally recommended that left ventricular pseudoaneurysm should be repaired surgically.[12] Ruptures develop in the necrotic tissue after an infarction. Tissue surrounding the necrotic region is edematous and fragile. Therefore, surgical repair is not easy. Rate of early postoperative mortality among patients who undergo surgical repair is 23-33%.[13] In the present case, we could not clarify whether the hemodynamic instability was due to free wall rupture or left ventricular pumping failure associated with acute ischemia. However, we continued to monitor the patient clinically and by TTE examination considering that the existing pericardial effusion did not collapse the right ventricle during diastole and the patient’s hemodynamic status returned to normal after primary percutaneous intervention.
In order to confirm the diagnosis and plan maintenance treatment, it is crucial to perform TTE examination during hospitalization of all patients who are being followed-up with the diagnosis of acute coronary syndrome. In particular, it is absolutely necessary to repeat TTE examination of the patients with an altered clinical course. Development of a previously absent pericardial effusion in an AMI patient should remind the physicians the possibility of cardiac free wall rupture.
The patient described here did not receive further anticoagulant therapy after the rupture was diagnosed. We believe that no progression of hemopericardium during follow-up may be associated with no further administration of anticoagulant therapy.
3-D TTE provides more explicit information than 2-D TTE to diagnose and follow-up a LVFWR, and it serves as a guide for surgery. Anticoagulant therapy management is extremely important during the follow-up of subacute LVFWR. We believe that the patients who are clinically stable can be monitored in an inpatient setting and undergo cardiac pseudoaneurysm surgery at a later stage.
References
- 1.Figueras J. Left ventricular free wall rupture: clinical presentation and management. Heart. 2000 May 01;83(5) doi: 10.1136/heart.83.5.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wehrens Xander H.T., Doevendans Pieter A. Cardiac rupture complicating myocardial infarction. International Journal of Cardiology. 2004 Jun;95(2-3) doi: 10.1016/j.ijcard.2003.06.006. [DOI] [PubMed] [Google Scholar]
- 3.POLLAK H., DIEZ W., SPIEL R., ENENKEL W., MLCZOCH J. Early diagnosis of subacute free wall rupture complicating acute myocardial infarction. European Heart Journal. 1993 May 01;14(5) doi: 10.1093/eurheartj/14.5.640. [DOI] [PubMed] [Google Scholar]
- 4.Park Seung Chul, Kim Jae Han, Kim Young Min, Kwak Sun Young, Yoon Buyng Ok, Oh Hung Sok, Oh Myung Jin, Kim Wan Sup, Lee Jin Woo, Hyon Min Su, Kim Sung Koo, Kwon Young Joo, Jeong Yoon Seop, Yum Wook. A Case of Early Developed Left Ventricular Free Wall Rupture Followed by Acute Inferior Myocardial Infarction Korean Circulation Journal. 1999;29(1) doi: 10.4070/kcj.1999.29.1.73. [DOI] [Google Scholar]
- 5.Akyıldız Elif Ülker, Çelik Safa, Ersoy Gökhan. İnfarkt sonrası gelişen kardiyak rüptürler; adli otopsi serisi. Anadolu Kardiyol Derg. 2007;7 [PubMed] [Google Scholar]
- 6.Hutchins Kenneth D., Skurnick Joan, Lavenhar Marvin, Natarajan Geetha A. Cardiac Rupture in Acute Myocardial Infarction. The American Journal of Forensic Medicine and Pathology. 2002 Mar;23(1) doi: 10.1097/00000433-200203000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Exadaktylos Nikolaos I., Kranidis Athanassios I., Argyriou Michalis O., Charitos Christos G., Andrikopoulos Georgios K. Left ventricular free wall rupture during acute myocardial infarction: early diagnosis and treatment Hellenic J Cardiol. 2002;43 [Google Scholar]
- 8.Vlodaver Z, Coe J I, Edwards J E. True and false left ventricular aneurysms. Propensity for the latter to rupture. Circulation. 1975 Mar;51(3) doi: 10.1161/01.cir.51.3.567. [DOI] [PubMed] [Google Scholar]
- 9.Frances Craig, Romero Anthony, Grady Deborah. Left ventricular pseudoaneurysm. Journal of the American College of Cardiology. 1998 Sep;32(3) doi: 10.1016/s0735-1097(98)00290-3. [DOI] [PubMed] [Google Scholar]
- 10.Little Stephen H., Ramasubbu Kumudha, Zoghbi William A. Real-time 3-Dimensional Echocardiography Demonstrates Size and Extent of Acute Left Ventricular Free Wall Rupture. Journal of the American Society of Echocardiography. 2007 May;20(5) doi: 10.1016/j.echo.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 11.Puri Timothy, Liu Zheng, Doddamani Sanjay, Coon Patrick D., Entwistle John W.C., Strong Michael, Vannan Mani. Three-Dimensional Echocardiography of Post-Myocardial Infarction Cardiac Rupture. Echocardiography. 2004 Apr;21(3) doi: 10.1111/j.0742-2822.2004.03085.x. [DOI] [PubMed] [Google Scholar]
- 12.Prêtre René, Linka André, Jenni Rolf, Turina Marko I. Surgical treatment of acquired left ventricular pseudoaneurysms. The Annals of Thoracic Surgery. 2000 Aug;70(2) doi: 10.1016/s0003-4975(00)01412-0. [DOI] [PubMed] [Google Scholar]
- 13.Purcaro Augusto, Costantini Carlo, Ciampani Nino, Mazzanti Marco, Silenzi Carla, Gili Alberto, Belardinelli Romualdo, Astolfi Daniel. Diagnostic Criteria and Management of Subacute Ventricular Free Wall Rupture Complicating Acute Myocardial Infarction. The American Journal of Cardiology. 1997 Aug;80(4) doi: 10.1016/s0002-9149(97)00385-8. [DOI] [PubMed] [Google Scholar]