Abstract
Risks and complications have been identified with dental implant failure though there is continuous innovation in implant systems and various interceptive treatment modalities. The success rate of dental implants has increased over a period of years as a treatment option for the rehabilitation of missing teeth. The dental implants are designed that best suits the various types of bone. Endosseous implants fail due to many reasons. Different reasons for the implant failure and their contributing factors have been discussed in this review article. A better understanding of the factors responsible for the implant failure will provide clinical decision-making and may enhance the field of implant dentistry. This article summarizes the factors causing implant failure. This paper presents the results of a survey of dentists practicing implant dentistry and updates regarding their knowledge of risk factors that they consider to be important for predicting dental implant failure.
Keywords: Dental implant, osseointegration, osteoradionecrosis, peri-implantitis, periodontitis
INTRODUCTION
The replacement of missing teeth by titanium dental implants is currently the gold standard in dental rehabilitation.[1,2] Different statistically analyzed factors associated with implant failure are age and sex,[3] smoking,[4] systemic diseases,[5,6] maxillary implant location, quantity and quality of bone,[7] and implant surface treatments and characteristics.[8] Immunological[9] and genetic factors[10] have also been reported to be associated with early implant failure. Periodontitis and cigarette smoking are associated with an increased rate of implant failure. It decreases the vascularity of local tissues and interrupts in healing, chemotaxis, and systemic immunity. Overall failure rates have been reported as 11% for smokers as compared to 5% for nonsmokers. Mellado-Valero et al.[11] found more failures in diabetic patients during the 1st year of functional loading. The failure of dental implant is seen in irradiated bone, excessive temperature elevation in bone during placement, leading to necrosis of the supporting bone around the implant[12] [Table 1 and Figure 1].
Table 1.
Conditions and factors contributing to implant health
| Conditions | Factors |
|---|---|
| Implant related | Previous history of failure |
| Surface roughness | |
| Surface purity and sterility | |
| Fitness discrepancies | |
| Exposure of implant into oral environment | |
| Mechanical factors | Premature loading |
| Occlusion trauma | |
| Dense hypovascular traumatized bone, comminuted bone | |
| Patient (local factors) | Oral hygiene status |
| Gingivitis/periodontitis | |
| Quantity and quality of adjacent bone | |
| Natural teeth proximity | |
| Periodontal status of natural teeth | |
| Impaction of foreign bodies | |
| Softtissue viability | |
| Patient (systemic factors) | Habits such as smoking, alcoholism |
| Prone to infection such as old age, malnourishment | |
| Diabetes | |
| Steroid therapy | |
| Chemotherapy/radiotherapy | |
| Hypersensitivity | |
| Surgical technique/environment | Traumatic surgical procedure |
| Overheating of surrounding bone due to handpiece | |
| Perioperative bacterial contamination |
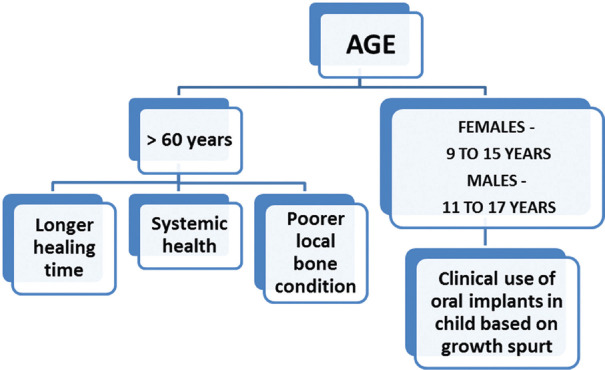
Figure 1.
Effect of age on implant health
Age factor
Age is considered as one of the important prognostic factors in implant success. Older patients are more prone to altered systemic health conditions, have poor local bone conditions and potentially longer healing times.[13] Moy et al.[14] studied that advanced age increases the risk of implant failure. Patients older than 60 years have an adverse outcome in two folds. Brocard et al.[15] studied cumulative success rates in a long-term follow-up study and concluded that patients older than 60 years hwwad less implant survival than usual. Implant submersion continues throughout adult life, and its rate varies with age. This process is much more conspicuous during the second and third decades of life when compared with the fourth and fifth.[16] The age at which growth is complete also varies widely from patient to patient.[17] The common growth spurt occurs at 12 years for girls and at 14 years for boys. However, this age can vary by as much as 6 years. Thus, when planning for the placement of dental implants in a child, this problematic age period extends from 9 to 15 years for girls and 11 to 17 years for boys.[18]
Mesial drift of teeth in the maxilla and mandible
The spontaneous mesial drift of teeth in the step dentition phase is well understood. There is about 5 mm mesial movement/drifting of teeth in the lateral segment of jaw (canine to the first molar) between 10 and 21 years of age. There is 2.5 mm buccal movement of incisors which may result in a loss of space in arch leading to crowd. Dental implant does not take part in this mesial drift of teeth. Thus, an implant can stop the mesial drift, resulting in an asymmetric arch. An implant in the anterior part cannot follow the teeth and will become more lingual with time. Depending on the facial growth pattern and further eruption of the teeth, vertical changes can still occur after puberty, though at a slower pace than during the active growth phase.[19] [Figure 2]
Figure 2.
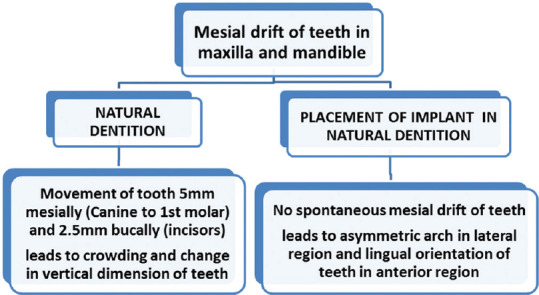
Effect of implant in Mesial drift of teeth in the maxilla and mandible
Oral hygiene and maintenance
The accumulation of bacterial plaque leads to gingivitis, periodontitis, and peri-implantitis. Furthermore, the presence of any symptoms of infection, radiographic evidence of peri-implant bone loss, and/or neuropathies reduced vascularity concomitant with parallel-oriented collagen fibers may be indicative of an ailing or failing implant.[20] This can be managed by the use of interproximal brushes penetrate 3 mm into the gingival sulcus or pocket. It also requires maintenance visit for the evaluation of prosthetic component for plaque and calculus, stability of the implant-abutment, peri-implant tissue margin, implant body, and radiographs after every 12–18 months.
Some other clinical conditions are association with oral lichen planus, parafunctional habits, and conventional flap versus flapless surgery or piezoelectric surgical technique, status of dentition, and deleterious effects of smoking habit [Table 2].
Table 2.
Clinical conditions affecting implant survival
| Higher success rate is seen in | Study done by |
|---|---|
| 100% survival rate of patient with oral lichen planus | Hernández et al., 2012[21] |
| Patients with nonparafunctional habits as compared to patients having parafunctional habits such as bruxism lead to fibrous encapsulation of implant | Glauser et al., 2001[22] |
| Conventional flap surgery as compared to flapless surgery | Sennerby et al., 2008[23] |
| Implants inserted with piezoelectric surgery split crest | Danza et al., 2009[24] |
| Dentulous dentition when compared to edentulous teeth | Kourtis et al., 2004[25] |
| Patients with no deleterious habits versus cigarette habit lead to delayed wound healing, inhibit cell proliferation and affects osteoblast function | Strietzel et al., 2007[26] |
Bruxism
Glauser et al. evaluated 41 patients who received 127 immediately loaded implants. Their results showed that implants in patients with bruxism were lost more frequently than those placed in patients with no parafunction (41% vs. 12%). The higher failure rate among the bruxers is due to uncontrolled functional loading of the implant, which leads to micro-motions above the critical limit, resulting in fibrous encapsulation of the implant instead of osseointegration. It was suggested that early or immediate loading is not detrimental for osseointegration unless excessive micro-motions occur at the bone-implant interface during the healing phase.[22]
The habit of cigarette smoking
Smoking affects the oral and general health of an individual. Smoking reduces leukocyte activity and causes reduced chemotactic migration rate and low phagocytic activity leading to low infection resistance and delayed wound healing. Smoking also decreases calcium absorption. Dental implants have a lower survival rate in smokers. Smoking affects osseointegration process by lowering blood flow rate due to increased peripheral resistance and platelet aggregation. Smoking residues are carbon monoxide and cyanide, which delay wound healing capacity and along with nicotine, inhibit cell proliferation rate.
Tobacco directly inhibits osteoblast function. Strietzel et al. reported that smoking affects implant prognosis with/without augmentations. Studies show significant marginal bone absorption in smokers when compared to nonsmokers.[26]
Loss of implant/graft material into the maxillary sinus
The immediate implant insertion in the unstable residual bone can lead to the loss of implant or graft material into the maxillary sinus affecting the natural ciliary movement in the maxillary sinus and mastication (<5 mm of bone). It can be managed surgically by different approaches, including intraoral, endoscopically, transnasal route, and bone reconstruction of maxilla.[27,28]
Bisphosphonate-related osteoradionecrosis
Bisphosphonates reside at active bone remodeling sites such as jaws causing surgical trauma to the alveolar bone during implant surgery and further increases the postoperative accumulation of the drug to the implanted site. Bisphosphonates interfere with the bone turnover and reduce the peri-implant bone resistance to oral flora, causing increased risk of peri-implantitis.[29,30,31]
Injury to adjacent tooth
The placement of implants along an improper axis or an excessively large implant can cause injury to adjacent tooth, resulting in nonvitality of the tooth. Dilacerated roots and excessive tilting in the mesiodistal direction obliterates the implant area and hinders the ideal implant placement. The interpretation of a radiograph with a guide pin of the depth of 5 mm facilitates angulation corrections of osteotomy.[32] Alternatively, differences between the apical and crestal interdental spaces due to mesial or distal tipping of the roots can be orthodontically corrected.[33]
Peri-implantitis
Peri-implantitis is a progressive inflammatory condition which affects the tissues surrounding an osseointegrated implant, leading to the loss of the supporting bone and implant failure. It is characterized by bleeding, suppuration, increased pocket probing depth, mobility of implant, and radiographical bone loss. This inflammatory process is more intense and, goes deeper and faster around the dental implant as compared to the inflammation around the adjacent natural tooth.[34] Cocci and nonmotile rods, the subgingival microflora causing peri-implantitis are the most important pathogens in the failure of dental implants. Soft laser irradiation is effective in the removal of the bacterial pathogens causing peri-implantitis.[35] Systemic antibiotics for Gram-negative anaerobes alters the microbial composition and clinically improves the condition over a 1-year period.[36] The local delivery devices such as Actisite which has fibers containing polymeric tetracycline hydrochloric acid can be used, which significantly reduces total anaerobic bacterial counts.[37]
Hyperglycemia
Hyperglycemia can also affect the osseointegration of dental implants. Hyperglycemia alters the response of the parathyroid hormone which helps in regulating the metabolism of phosphorus and calcium and inhibits osteoblastic differentiation. It affects bone matrix, its components, and adherence, growth, and accumulation of extracellular matrix. The normal glucose level following insulin treatment induces growth in bony matrix and osteoid formation. Hyperglycemia may reduce bone recovery by 40% following circular osteotomies. Treatment with insulin normalizes this recovery index, thus indicating that the bone healing deterioration is strongly related to poor diabetic control. Failures that occur after the second-phase surgery and during the 1st year of functional loading is due to microangiopathy arising as a complication of diabetes. This may compromise the vascularization of the flap, causing infection of soft tissue, and delayed wound healing.[38,39]
Irradiated bone
Irradiation therapy along with surgical excision is the treatment protocol generally employed for malignant tumors in the craniofacial region. The success rate of placement of dental implants in irradiated bone is 70%. Hyperbaric oxygen therapy in irradiated patients prior to implant therapy increases the success rate of implants.[40]
Osteoporotic patients
Osseointegration failure in osteoporotic patients is due to the decrease in bone mass and density.[41] Osteoporosis does not necessarily affect the maxillary and mandibular bones when diagnosed at one particular site of the skeleton.[42] Intravenous application of bisphosphonates is associated with osteonecrosis of the jaw. There are 63 cases of osteonecrosis of the jaw reported in cancer or osteoporotic patients. Implant treatment on patients having long-term bisphosphonates must be performed with caution.[43,44]
Corticosteroid therapy
Patients on systemic corticosteroid therapy are more prone to have reduced bone density, increased epithelial fragility, and immune suppression which in turn results in compromised osseointegration of the dental implant. In these cases, medical intervention and adrenal gland suppression rate should be observed.[45]
Immune deficiency
Patients with immune deficiency are more prone to infection and compromised tissue repair. According to recent studies, dental implant placement has been performed successfully in patients with stable immune status, HIV-positive cases with a sufficient number of CD4+ cells and using antiviral drugs.[46,47]
Bleeding disorders
Uncontrolled hemorrhage can be caused by platelet disorders, coagulant factors deficiency, and using anticoagulant drugs such as aspirin and warfarin.[48] It is due to platelet deficiency <50,000/mm3.[49] The most life-threatening adverse effect of dental implant placement in these patients is upper airway obstruction.[50]
Cardiovascular disorders
Cardiovascular diseases interfere with healing and osseointegration process, resulting in reduced fibroblast activity, impaired macrophage function, and decreased collagen synthesis.[51] These pathologies include hypertension, atherosclerosis, and congestive heart failure. Cardiovascular disease does not have a significant influence on the long-term success rate of dental implant treatment.[52]
Organ (heart/liver/renal) transplantation
Patients having transplanted organs undergo long-term immunesuppressant medications to prevent graft rejection. Cyclosporine A is usually given in combination with steroids (anti-inflammatory action). Cyclosporine may have a negative impact on mechanical retention and healing of bone around the dental implant.[53,54]
CONCLUSION
There is a need to increase the knowledge and awareness regarding the potential risk factors that could impact on implant failures to those who are practicing dental implantology. This can be achieved through continuous dental educational programs and workshops. Regular assessment of the theoretical and practical knowledge of implant dentistry is mandatory to improve their implant experience.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Buser D, Janner SF, Wittneben JG, Brägger U, Ramseier CA, Salvi GE. 10-year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: A retrospective study in 303 partially edentulous patients. Clin Implant Dent Relat Res. 2012;14:839–51. doi: 10.1111/j.1708-8208.2012.00456.x. [DOI] [PubMed] [Google Scholar]
- 2.Östman PO, Hellman M, Sennerby L. Ten years later. Results from a prospective single-centre clinical study on 121 oxidized (TiUnite™) brånemark implants in 46 patients. Clin Implant Dent Relat Res. 2012;14:852–60. doi: 10.1111/j.1708-8208.2012.00453.x. [DOI] [PubMed] [Google Scholar]
- 3.Eliasson A, Narby B, Ekstrand K, Hirsch J, Johansson A, Wennerberg A. A 5-year prospective clinical study of submerged and nonsubmerged paragon system implants in the edentulous mandible. Int J Prosthodont. 2010;23:231–8. [PubMed] [Google Scholar]
- 4.Sverzut AT, Stabile GA, de Moraes M, Mazzonetto R, Moreira RW. The influence of tobacco on early dental implant failure. J Oral Maxillofac Surg. 2008;66:1004–9. doi: 10.1016/j.joms.2008.01.032. [DOI] [PubMed] [Google Scholar]
- 5.Alsaadi G, Quirynen M, Komárek A, van Steenberghe D. Impact of local and systemic factors on the incidence of oral implant failures, up to abutment connection. J Clin Periodontol. 2007;34:610–7. doi: 10.1111/j.1600-051X.2007.01077.x. [DOI] [PubMed] [Google Scholar]
- 6.Alsaadi G, Quirynen M, Michiles K, Teughels W, Komárek A, van Steenberghe D. Impact of local and systemic factors on the incidence of failures up to abutment connection with modified surface oral implants. J Clin Periodontol. 2008;35:51–7. doi: 10.1111/j.1600-051X.2007.01165.x. [DOI] [PubMed] [Google Scholar]
- 7.van Steenberghe D, Jacobs R, Desnyder M, Maffei G, Quirynen M. The relative impact of local and endogenous patient-related factors on implant failure up to the abutment stage. Clin Oral Implants Res. 2002;13:617–22. doi: 10.1034/j.1600-0501.2002.130607.x. [DOI] [PubMed] [Google Scholar]
- 8.Bornstein MM, Halbritter S, Harnisch H, Weber HP, Buser D. A retrospective analysis of patients referred for implant placement to a specialty clinic: Indications, surgical procedures, and early failures. Int J Oral Maxillofac Implants. 2008;23:1109–16. [PubMed] [Google Scholar]
- 9.Kronström M, Svensson B, Erickson E, Houston L, Braham P, Persson GR. Humoral immunity host factors in subjects with failing or successful titanium dental implants. J Clin Periodontol. 2000;27:875–82. doi: 10.1034/j.1600-051x.2000.027012875.x. [DOI] [PubMed] [Google Scholar]
- 10.Leite MF, Santos MC, de Souza AP, Line SR. Osseointegrated implant failure associated with MMP-1 promotor polymorphisms (-1607 and -519) Int J Oral Maxillofac Implants. 2008;23:653–8. [PubMed] [Google Scholar]
- 11.Mellado-Valero A, Ferrer García JC, Herrera Ballester A, Labaig Rueda C. Effects of diabetes on the osseointegration of dental implants. Med Oral Patol Oral Cir Bucal. 2007;12:E38–43. [PubMed] [Google Scholar]
- 12.Mishra SK, Chowdhary R. Heat generated by dental implant drills during osteotomy-a review: Heat generated by dental implant drills. J Indian Prosthodont Soc. 2014;14:131–43. doi: 10.1007/s13191-014-0350-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wood MR, Vermilyea SG Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. A review of selected dental literature on evidence-based treatment planning for dental implants: Report of the committee on research in fixed prosthodontics of the academy of fixed prosthodontics. J Prosthet Dent. 2004;92:447–62. doi: 10.1016/j.prosdent.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 14.Moy PK, Medina D, Shetty V, Aghaloo TL. Dental implant failure rates and associated risk factors. Int J Oral Maxillofac Implants. 2005;20:569–77. [PubMed] [Google Scholar]
- 15.Brocard D, Barthet P, Baysse E, Duffort JF, Eller P, Justumus P, et al. A multicenter report on 1,022 consecutively placed ITI implants: A 7-year longitudinal study. Int J Oral Maxillofac Implants. 2000;15:691–700. [PubMed] [Google Scholar]
- 16.Schwartz-Arad D, Bichacho N. Effect of age on single implant submersion rate in the central maxillary incisor region: A long-term retrospective study. Clin Implant Dent Relat Res. 2015;17:509–14. doi: 10.1111/cid.12131. [DOI] [PubMed] [Google Scholar]
- 17.Koch G, Bergendal T, Kvint S, Johansson UB. Consensus Conference on Oral Implants in Young Patients. Göteborg, Sweden: Graphic Systems; 1996. [Google Scholar]
- 18.Hägg U. A Prospective Longitudinal Study of Swedish Urban Children [Thesis] Malmö, Sweden: Univ of Malmö; 1980. The Pubertal Growth Spurt and Maturity Indicators of Dental, Skeletal and Pubertal Development. [Google Scholar]
- 19.Björk A, Skieller V. Ann Arbor, MI: University of Michigan Press; 1976. Postnatal Growth and Development of the Maxillary Complex, Monograph 6, Craniofacial Growth Series; pp. 61–99. [Google Scholar]
- 20.Meffert RM. How to treat ailing and failing implants. Implant Dent. 1992;1:25–33. doi: 10.1097/00008505-199200110-00003. [DOI] [PubMed] [Google Scholar]
- 21.Hernández G, Lopez-Pintor RM, Arriba L, Torres J, de Vicente JC. Implant treatment in patients with oral lichen planus: A prospective-controlled study. Clin Oral Implants Res. 2012;23:726–32. doi: 10.1111/j.1600-0501.2011.02192.x. [DOI] [PubMed] [Google Scholar]
- 22.Glauser R, Rée A, Lundgren A, Gottlow J, Hämmerle CH, Schärer P. Immediate occlusal loading of brånemark implants applied in various jawbone regions: A prospective, 1-year clinical study. Clin Implant Dent Relat Res. 2001;3:204–13. doi: 10.1111/j.1708-8208.2001.tb00142.x. [DOI] [PubMed] [Google Scholar]
- 23.Sennerby L, Rocci A, Becker W, Jonsson L, Johansson LA, Albrektsson T. Short-term clinical results of Nobel direct implants: A retrospective multicentre analysis. Clin Oral Implants Res. 2008;19:219–26. doi: 10.1111/j.1600-0501.2007.01410.x. [DOI] [PubMed] [Google Scholar]
- 24.Danza M, Guidi R, Carinci F. Comparison between implants inserted into piezo split and unsplit alveolar crests. J Oral Maxillofac Surg. 2009;67:2460–5. doi: 10.1016/j.joms.2009.04.041. [DOI] [PubMed] [Google Scholar]
- 25.Kourtis SG, Sotiriadou S, Voliotis S, Challas A. Private practice results of dental implants. Part I: Survival and evaluation of risk factors part II: Surgical and prosthetic complications. Implant Dent. 2004;13:373–85. doi: 10.1097/01.id.0000148564.88384.de. [DOI] [PubMed] [Google Scholar]
- 26.Strietzel FP, Reichart PA, Kale A, Kulkarni M, Wegner B, Küchler I. Smoking interferes with the prognosis of dental implant treatment: A systematic review and meta-analysis. J Clin Periodontol. 2007;34:523–44. doi: 10.1111/j.1600-051X.2007.01083.x. [DOI] [PubMed] [Google Scholar]
- 27.Becker ST, Terheyden H, Steinriede A, Behrens E, Springer I, Wiltfang J. Prospective observation of 41 perforations of the schneiderian membrane during sinus floor elevation. Clin Oral Implants Res. 2008;19:1285–9. doi: 10.1111/j.1600-0501.2008.01612.x. [DOI] [PubMed] [Google Scholar]
- 28.Peleg M, Garg AK, Mazor Z. Predictability of simultaneous implant placement in the severely atrophic posterior maxilla: A 9-year longitudinal experience study of 2132 implants placed into 731 human sinus grafts. Int J Oral Maxillofac Implants. 2006;21:94–102. [PubMed] [Google Scholar]
- 29.Ruggiero SL, Dodson TB, Assael LA, Landesberg R, Marx RE, Mehrotra B, et al. American association of oral and maxillofacial surgeons position paper on bisphosphonate-related osteonecrosis of the jaws--2009 update. J Oral Maxillofac Surg. 2009;67:2–12. doi: 10.1016/j.joms.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 30.Khan AA, Sándor GK, Dore E, Morrison AD, Alsahli M, Amin F, et al. Canadian consensus practice guidelines for bisphosphonate associated osteonecrosis of the jaw. J Rheumatol. 2008;35:1391–7. [PubMed] [Google Scholar]
- 31.Bedogni A, Bettini G, Totola A, Saia G, Nocini PF. Oral bisphosphonate-associated osteonecrosis of the jaw after implant surgery: A case report and literature review. J Oral Maxillofac Surg. 2010;68:1662–6. doi: 10.1016/j.joms.2010.02.037. [DOI] [PubMed] [Google Scholar]
- 32.Greenstein G, Cavallaro J, Romanos G, Tarnow D. Clinical recommendations for avoiding and managing surgical complications associated with implant dentistry: A review. J Periodontol. 2008;79:1317–29. doi: 10.1902/jop.2008.070067. [DOI] [PubMed] [Google Scholar]
- 33.Annibali S, Ripari M, La Monaca G, Tonoli F, Cristalli MP. Local accidents in dental implant surgery: Prevention and treatment. Int J Periodontics Restorative Dent. 2009;29:325–31. [PubMed] [Google Scholar]
- 34.Lindhe J, Berglundh T, Ericsson I, Liljenberg B, Marinello C. Experimental breakdown of peri-implant and periodontal tissues. A study in the beagle dog. Clin Oral Implants Res. 1992;3:9–16. doi: 10.1034/j.1600-0501.1992.030102.x. [DOI] [PubMed] [Google Scholar]
- 35.Deppe H, Horch HH, Henke J, Donath K. Peri-implant care of ailing implants with the carbon dioxide laser. Int J Oral Maxillofac Implants. 2001;16:659–67. [PubMed] [Google Scholar]
- 36.Roos-Jansåker AM, Renvert S, Egelberg J. Treatment of peri-implant infections: A literature review. J Clin Periodontol. 2003;30:467–85. doi: 10.1034/j.1600-051x.2003.00296.x. [DOI] [PubMed] [Google Scholar]
- 37.Mombelli A, Feloutzis A, Brägger U, Lang NP. Treatment of peri-implantitis by local delivery of tetracycline.Clinical, microbiological and radiological results. Clin Oral Implants Res. 2001;12:287–94. doi: 10.1034/j.1600-0501.2001.012004287.x. [DOI] [PubMed] [Google Scholar]
- 38.He H, Liu R, Desta T, Leone C, Gerstenfeld LC, Graves DT. Diabetes causes decreased osteoclastogenesis, reduced bone formation, and enhanced apoptosis of osteoblastic cells in bacteria stimulated bone loss. Endocrinology. 2004;145:447–52. doi: 10.1210/en.2003-1239. [DOI] [PubMed] [Google Scholar]
- 39.Santana RB, Xu L, Chase HB, Amar S, Graves DT, Trackman PC. A role for advanced glycation end products in diminished bone healing in Type 1 diabetes. Diabetes. 2003;52:1502–10. doi: 10.2337/diabetes.52.6.1502. [DOI] [PubMed] [Google Scholar]
- 40.Granström G, Tjellström A, Brånemark PI. Osseointegrated implants in irradiated bone: A case-controlled study using adjunctive hyperbaric oxygen therapy. J Oral Maxillofac Surg. 1999;57:493–9. doi: 10.1016/s0278-2391(99)90059-9. [DOI] [PubMed] [Google Scholar]
- 41.Mombelli A, Cionca N. Systemic diseases affecting osseointegration therapy. Clin Oral Implants Res. 2006;17(Suppl 2):97–103. doi: 10.1111/j.1600-0501.2006.01354.x. [DOI] [PubMed] [Google Scholar]
- 42.Jacobs R, Ghyselen J, Koninckx P, van Steenberghe D. Long-term bone mass evaluation of mandible and lumbar spine in a group of women receiving hormone replacement therapy. Eur J Oral Sci. 1996;104:10–6. doi: 10.1111/j.1600-0722.1996.tb00039.x. [DOI] [PubMed] [Google Scholar]
- 43.Wang HL, Weber D, McCauley LK. Effect of long term oral bisphosphonates on implant wound healing: Literature review and a case report. J Periodontol. 2007;78:584–94. doi: 10.1902/jop.2007.060239. [DOI] [PubMed] [Google Scholar]
- 44.Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: A review of 63 cases. J Oral Maxillofac Surg. 2004;62:527–34. doi: 10.1016/j.joms.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 45.Bencharit S, Reside GJ, Howard-Williams EL. Complex prosthodontic treatment with dental implants for a patient with polymyalgia rheumatica: A clinical report. Int J Oral Maxillofac Implants. 2010;25:1241–5. [PubMed] [Google Scholar]
- 46.Mealey BL. Periodontal implications: Medically compromised patients. Ann Periodontol. 1996;1:256–321. doi: 10.1902/annals.1996.1.1.256. [DOI] [PubMed] [Google Scholar]
- 47.Stevenson GC, Riano PC, Moretti AJ, Nichols CM, Engelmeier RL, Flaitz CM. Short-term success of osseointegrated dental implants in HIV-positive individuals: A prospective study. J Contemp Dent Pract. 2007;8:1–0. [PubMed] [Google Scholar]
- 48.Benoliel R, Leviner E, Katz J, Tzukert A. Dental treatment for the patient on anticoagulant therapy: Prothrombin time value--what difference does it make? Oral Surg Oral Med Oral Pathol. 1986;62:149–51. doi: 10.1016/0030-4220(86)90036-8. [DOI] [PubMed] [Google Scholar]
- 49.Drews RE. Critical issues in hematology: Anemia, thrombocytopenia, coagulopathy, and blood product transfusions in critically ill patients. Clin Chest Med. 2003;24:607–22. doi: 10.1016/s0272-5231(03)00100-x. [DOI] [PubMed] [Google Scholar]
- 50.Givol N, Chaushu G, Halamish-Shani T, Taicher S. Emergency tracheostomy following life-threatening hemorrhage in the floor of the mouth during immediate implant placement in the mandibular canine region. J Periodontol. 2000;71:1893–5. doi: 10.1902/jop.2000.71.12.1893. [DOI] [PubMed] [Google Scholar]
- 51.Bradley JC. The clinical significance of age changes in the vascular supply to the mandible. Int J Oral Surg. 1981;10:71–6. [PubMed] [Google Scholar]
- 52.Hwang D, Wang HL. Medical contraindications to implant therapy: Part II: Relative contraindications. Implant Dent. 2007;16:13–23. doi: 10.1097/ID.0b013e31803276c8. [DOI] [PubMed] [Google Scholar]
- 53.Tarantino A, Montagnino G, Ponticelli C. Corticosteroids in kidney transplant recipients. Safety issues and timing of discontinuation. Drug Saf. 1995;13:145–56. doi: 10.2165/00002018-199513030-00002. [DOI] [PubMed] [Google Scholar]
- 54.Dumont RJ, Ensom MH. Methods for clinical monitoring of cyclosporin in transplant patients. Clin Pharmacokinet. 2000;38:427–47. doi: 10.2165/00003088-200038050-00004. [DOI] [PubMed] [Google Scholar]