Abstract
Introduction
Antenatal care (ANC) is a vital mechanism for women to obtain close attention during pregnancy and prevent death-related issues. Moreover, it improves the involvement of women in the continuum of health care and to survive high-risk pregnancies. This study was conducted to determine the prevalence of and identify the associated factors of eight or more ANC contacts in Nigeria.
Methods
We used a nationally representative cross-sectional data from Nigeria Demographic and Health Survey—2018. A total sample of 7,936 women were included in this study. Prevalence was measured in percentages and the factors for eight or more ANC contacts were examined using multilevel multivariable binary logistic regression model. The level of significance was set at P<0.05.
Results
The prevalence of eight or more ANC contacts in Nigeria was approximately 17.4% (95% CI: 16.1%-18.7%). Women with at least secondary education were 2.46 times as likely to have eight or more ANC contacts, when compared with women with no formal education. Women who use media were 2.37 times as likely to have eight or more ANC contacts, when compared with women who do not use media. For every unit increase in the time (month) of ANC initiation, there was 53% reduction in the odds of eight or more ANC contacts. Rural women had 60% reduction in the odds of eight or more ANC contacts, when compared with their urban counterparts. Women from North East and North West had 74% and 79% reduction respectively in the odds of eight or more ANC contacts, whereas women from South East, South South and South West were 2.68, 5.00 and 14.22 times respectively as likely to have eight or more ANC contacts when compared with women from North Central.
Conclusion
The coverage of eight or more ANC contacts was low and can be influenced by individual-, household-, and community-level factors. There should be concerted efforts to improve maternal socioeconomic status, as well as create awareness among key population for optimal utilization of ANC.
Introduction
The fifth Millennium Development Goal (MDG-5) sought to reduce maternal mortality by 75% between 1990 and 2015 [1]. However, while there were significant improvements such as a 45% reduction in maternal mortality ratio, and a 12% increase in skilled birth attendance by 2015, death from pregnancy and childbirth continued globally [2]. Transitioning from the MDGs in 2015 [3], the Sustainable Development Goals (SDGs) aim to reduce maternal mortality by 2030 to less than 70 per 100,000 live births [4]. However, in 2015, about 303,000 deaths occurred around the world resulting from pregnancy and childbirth, with a majority of these deaths occurring in low resource settings [2,5]. This staggering estimate in maternal mortality contravenes the third goal in SDGs which focus to ensure healthy lives and promote well-being for all at all ages [4].
Sub-Saharan Africa (SSA) disproportionately contributes to global maternal death, where about 196,000 maternal deaths occurred in 2015 [2]. The lifetime risk of dying from pregnancy and childbirth is 1 in 37 in resource-constrained settings as compared with high-income countries, where the lifetime risk of maternal death is 1 in 7,800 [2,5]. These figures raise important, yet critical questions as to whether any progress has been achieved in SSA thus far. Interestingly, ANC remains a prominent measure for improving maternal health outcomes and provided by skilled births attendants to ensure positive health outcomes for mothers and children [6]. In 2002, WHO recommended a goal-orientated approach to ANC to improve quality of care and increase ANC coverage, specifically in resource-constrained settings [7]. The FANC model was commonly referred to as the basic ANC model and included four ANC visits occurring between 8 and 12 weeks of gestation, between 24 and 26 weeks, at 32 weeks, and between 36 and 38 weeks respectively [7]. Recognizing the benefits of increased ANC contacts, in 2016, the World Health Organization (WHO) recommended eight ANC contacts in the place of focused ANC (FANC) model, to ensure better pregnancy experience [8].
Although Nigeria adopted the previous WHO FANC model, which recommended one visit during each trimester of gestation and a final visit immediately preceding delivery for women without pregnancy-related complications or risk factors, still only 52% of women made all four recommended visits in 2013 [9]. This raises concerns regarding the adoption and implementation of the WHO new guideline, which recommends that the number of contacts for a woman be increased from four to eight.
In spite of the FANC model institutionalized in-country over a decade, it is worrisome to note that Nigeria currently accounts for about 20% of global maternal deaths [10]. Moreover, numerous factors have been attributed to the underutilization of ANC services, such as far distance of the health facilities from clients, lack of transportation and out-of-pocket spending for healthcare, maternal age, religious background, parity, health insurance coverage, ethnicity, marital status, involvement in labour force, education and accessibility to health information [11–16]. In addition, multifactorial inequalities in access to healthcare, impact of environmental, economic, socio-demographic and political factors have contributed to poor health outcomes for women of reproductive age especially in poor resource settings [17]. Studies have identified community-level factors associated with ANC visits, these include rural-urban residential status, years of education/rate of women’s literacy, income score/ poverty rate, geographical region, community exposure to newspaper, television, community education and wealth concentration, antenatal care service availability and readiness [13,18,19]. Largely, these factors were examined to determine their association with eight or more ANC contacts in Nigeria. To the best of our knowledge, there is no study on the coverage and factors of eight ANC in Nigeria that used data collected after the launched of the WHO new guideline. In this study, we aimed to assess the individual, household and community-level factors associated with eight or more ANC contacts.
Methods
Data source
We used a nationally representative cross-sectional data. The individual woman questionnaire in Nigeria Demographic and Health Survey (NDHS) was analyzed in this study. A total sample of 7,936 women of reproductive age who became pregnant and had given birth after the new guideline of eight ANC contacts was endorsed were included in this study. The 2018 NDHS is the sixth survey of its kind to be implemented by the National Population Commission (NPC). Data collection took place from 14 August to 29 December 2018. The sample was selected using a stratified, two-stage cluster design, with Enumeration Areas (EAs) as the sampling units for the first stage. The complete listing of households carried out in each of the 1,389 selected EAs, an approximate number of 30 households was selected in every cluster resulting to a total of 41,821 women were interviewed during the survey, yielding a response rate of 99%. A total sample of 7,936 women of reproductive age who became pregnant and had given birth after the new guideline of eight or more ANC contacts was endorsed by WHO [8], were included in this study.
In particular, NDHS 2018 used a three-stage sampling stratification, in which respondents were first stratified by urban versus rural dwelling, and EAs were then selected randomly within each stratum. Finally, households within each EA were then selected for the survey using equal probability sampling. This three-stage sampling method was taken into account in the computation of survey weights, applied to ensure the representativeness of the sample with regard to the general population. The sampling frame used for the 2018 NDHS is the Population and Housing Census of the Federal Republic of Nigeria (NPHC), which was conducted in 2006 by the National Population Commission. The sample for the 2018 NDHS was a stratified sample selected in two stages. Stratification was achieved by separating each of the 36 states and the Federal Capital Territory into urban and rural areas. In total, 74 sampling strata were identified. Data for this study are derived from the individual female data for analysis. The DHS project, funded primarily by the United States Agency for International Development (USAID) with support from other donors and host countries, has conducted over 230 nationally representative and internationally comparable household surveys in more than 80 countries since its inception in 1984. The data is available in the public domain and accessed at; http://dhsprogram.com/data/available-datasets.cfm. Details of DHS sampling procedure has been reported previously [20].
Variables selection and measurement
Outcome
The frequency of ANC contacts with doctors, nurses and midwives was measured dichotomously; less than eight ANC contacts vs. eight or more ANC contacts. The WHO ANC guideline recommendations mapped to the eight recommended contacts, presents a summary framework for the 2016 WHO ANC model in support of a positive pregnancy experience [8,21,22].
Individual-level factors
Family mobility: internal immigrant (if a respondent lived in the current location in less than 5 years) vs. native (if a respondent had lived in the current location at least 5 years). Religious background: Christianity, Islam and African Traditional Religion (ATR)/others. Literacy: cannot read at all, able to read only part of a sentence and able to read whole sentence. Total number of children ever born: 1–2, 3–4 and over 4 children. Women’s knowledge level was measured using; educational attainment, read newspaper/magazines, listen to radio, watch television and use internet [23]. Using Principal Component Analysis (PCA), the standardized z-score was used to disentangle the overall assigned scores to low, medium and high. Maternal educational attainment: no formal education, primary and secondary or higher education. Media use was measured dichotomously (yes vs. no) if a respondent used any or newspaper/magazine, radio, television or internet irrespective of the frequency levels, "almost every day", "at least once a week", and "less than once a week" as yes/use and the response level "not at all" as no/not use [24]. Maternal age: 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49. Wanted child when became pregnant: then, later and wanted no more. Health insurance: covered vs. not covered. Marital status: never in union, currently married/living with a partner and formerly in union. Employment status: working vs. not working. Family type: monogyny vs. polygyny. Intimate partner violence: yes (if a woman had physical, sexual or emotional violence) vs. no (otherwise). Women’s autonomy was measured using PCA for selected items: person who usually decides on respondent's health care, person who usually decides on large household purchases and person who usually decides on visits to family or relatives [25]. The standardized z-score was then used to disentangle the overall assigned scores to low, medium and high. Time to ANC initiation (in months).
Household-level factors
Sex of household headship was male vs. female. Household size was based on the total number of individuals who resided together and grouped as: 1–4, 5–8 and over 8 persons. Household wealth quintiles: PCA was used to assign the wealth indicator weights. This procedure assigned scores and standardized the wealth indicator variables such as; bicycle, motorcycle/scooter, car/truck, main floor material, main wall material, main roof material, sanitation facilities, water source, radio, television, electricity, refrigerator, cooking fuel, furniture, number of persons per room. The factor coefficient scores (factor loadings) and z-scores were calculated. For each household, the indicator values were multiplied by the loadings and summed to produce the household’s wealth index value. The standardized z-score was used to disentangle the overall assigned scores to; poorest/poorer/middle/richer/richest categories [26,27]. In creating household wealth index, rural-urban differences was adjusted for and used in the analysis. As a response to criticism that a single wealth index is too urban in its construction and not able to distinguish the poorest of the poor from other poor households, the new variable created to provide an urban- and rural-specific wealth index was utilized.
Community-level factors
We used EAs to represent communities prominently because the DHS did not collect aggregate-level data at the community level. Hence, community-level variables included in the analysis were based on women’s characteristics particularly those that have implications for accessing ANC. Cultural norms about wife-beating was created by aggregating responses from women in each community. Here, we used the items: “beating justified if wife goes out without telling husband”, “beating justified if wife neglects the children”, “beating justified if wife argues with husband”, “beating justified if wife refuses to have sex with husband” and “beating justified if wife burns the food”. Finally, a binary variable was created for acceptance of wife beating [28]. Maternal residential status was measured as: urban vs. rural. Geographical region was categorized thus: North Central, North East, North West, South East, South South and South West.
Furthermore, aggregate community-level variables were constructed by aggregating individual level characteristics at the community (cluster) level and categorization of the aggregate variables was done as low or high based on the distribution of the proportion values calculated for each community. If the aggregate variable was normally distributed mean value and if not normally distributed median value was used as cut off point for the categorization. Community-level poverty was categorized as high if the proportion of women from the two lowest wealth quintiles in a given community was 43–100% and low if the proportion was 0–42%. Community-level media use was categorized as high if the proportion was 60–100% and as low if the proportion of women who use media in the community was 0–59%. Community-level illiteracy was categorized as high if proportion of women who cannot read at all was 67–100% and as low if the proportion of women who cannot read at all was 0–66%. Community-level urban residence was categorized as high if proportion of women who reside in urban area was greater than 1–100% and as low if the proportion of women who reside in urban area was 0%. Community-level women’s autonomy was categorised as high if the proportion of women who had at least moderate autonomy was 61–100% and categorized as low if the proportion was between 0–60%. This approach was used in a previous study [29,30].
Ethical consideration
In this study, we utilized population-based secondary datasets available in public domain/ online with all identifier information removed. The authors were granted access to use the data by MEASURE DHS/ICF International. DHS Program is consistent with the standards for ensuring the protection of respondents’ privacy. ICF International ensures that the survey complies with the U.S. Department of Health and Human Services regulations for the respect of human subjects. No further approval was required for this study. More details about data and ethical standards are available at http://goo.gl/ny8T6X.
Statistical analysis
The survey (‘svy’) module was used to adjust for stratification, clustering and sampling weights to compute the estimates of eight or more ANC contacts. The prevalence of eight or more ANC contacts was explored using percentage. A cut-off of 0.7 was used to determine multicollinearity known to cause major concerns in the logit model [31]. Consequently, maternal literacy and knowledge were excluded from the model as they were found to have positive interdependence with educational attainment which was therefore retained in the model. Other significant variables from Chi-square test or student’s t-test at 25% level of significance were retained in the logit model in the absence of multicollinearity.
A multivariable multilevel binary logistic regression model was used to estimate the fixed and random effects of the factors associated with eight or more ANC contacts. We specified a 3-level model for binary response reporting eight or more ANC contacts, for women (at level 1), in a household (at level 2) from an Enumeration Area (at level 3). We constructed five models. The first model, an empty or unconditional model without any explanatory variables, was specified to decompose the amount of variance that existed between community and household levels. The null or empty model is important for understanding the community and households’ variations, and we used it as the reference to estimate how much household and community factors were able to explain the observed variations. In addition, we used it to justify the use of multilevel statistical framework, because if the community variance was not significant in the empty model, it advised to use the single-level logistic regression. The second model contained only individual-level factors, the third model contained only household-level factors, and the fourth model contained only community-level factors. Finally, the fifth model simultaneously controlled for individual, household and community level factors (Full model). Statistical significance was determined at p< 0.05. The Bayesian and Akaike Information Criterions were used to select the best model out of the five models. A lower value on Akaike or Bayesian Information Criterion indicates a better fit of the model [32]. Data analysis was conducted using Stata Version 14 (StataCorp., College Station, TX, USA).
Fixed and random effects
The results of fixed effects (measures of association) were reported as adjusted odds ratios (AORs) with their 95% confidence interval (CI). The probable contextual effects were measured by the Intra-class Correlation (ICC) and Median Odds Ratio (MOR) [33]. We measured the similarity between respondents in the same household and within the same community using ICC. The ICC represents the percentage of the total variance in the probability of eight or more ANC contacts that is related to the household and community level, i.e. measure of clustering of odds of eight or more ANC contacts in the same household and community. The MOR measures the second or third level (household or community) variance as odds ratio and estimates the probability of eight or more ANC contacts that can be attributed to household and community context. MOR equal to one indicates no household or community variance. Conversely, the higher the MOR, the more important are the contextual effects for understanding the probability of eight or more ANC contacts. The ICC was calculated by the linear threshold according to the formula used by Snijders and Bosker [34], whereas the MOR is a measure of unexplained cluster heterogeneity.
Results
Sample characteristics
Based on the results from Table 1, approximately 26.1% (95% CI: 23.1%-29.3%) of native women reported eight or more ANC contacts. Similarly, about 33.1% (95% CI: 30.7%-35.5%) of Christian women, 36.1% (95% CI: 33.5%-38.8%) of women who are able to read whole sentence, 23.0% (95% CI: 21.0%-25.1%) of women who had ever given birth to at most two children, 35.6% (95% CI: 33.1%-38.2%) of women with high knowledge, 34.0% (95% CI: 31.8%-36.3%) of women with at least secondary education, 25.2% (95% CI: 23.3%-27.0%) of women who use media had eight or more ANC contacts respectively. Furthermore, about 22.7% (95% CI: 20.0%-25.7%) of women aged 30–34 years, 39.3% (95% CI: 30.0%-49.4%) of women covered by health insurance, 21.1% (95% CI: 19.5%-22.9%) of women who participated in labour force, 21.0% (95% CI: 19.8%-23.0%) of women in monogyny, 24.0% (95% CI: 21.6%-26.7%) of women with no history of intimate partner’s violence, 31.3% (95% CI: 28.6%-34.1%) of women with high autonomy had eight or more ANC contacts respectively. See the table below for further details.
Table 1. Prevalence of eight or more ANC contacts across women’s characteristics, NDHS—2018.
| Variable | Number of women (%) | Weighted eight or more ANC contacts; % (95%CI) | P |
|---|---|---|---|
| Family mobility | <0.001* | ||
| Internal immigrant | 1267 (16.5) | 26.1 (23.1–29.3) | |
| Native | 6392 (83.5) | 14.8 (13.5–16.2) | |
| Religion | <0.001* | ||
| Christianity | 3048 (38.4) | 33.1 (30.7–35.5) | |
| Islam | 4820 (60.7) | 9.1 (7.9–10.4) | |
| ATR/others | 68 (0.9) | 7.2 (1.5–27.8) | |
| Literacy | <0.001* | ||
| Cannot read at all | 4678 (59.0) | 7.2 (6.2–8.3) | |
| Able to read parts of sentence | 1383 (17.4) | 27.3 (24.2–30.7) | |
| Able to read whole sentence | 1874 (23.6) | 36.1 (33.5–38.8) | |
| Number of children ever born | <0.001* | ||
| 1–2 | 2903 (36.6) | 23.0 (21.0–25.1) | |
| 3–4 | 2279 (28.7) | 19.2 (17.1–21.6) | |
| 4+ | 2754 (34.7) | 10.2 (8.8–11.8) | |
| Women’s knowledge | <0.001* | ||
| Low | 3059 (38.5) | 2.8 (2.1–3.7) | |
| Moderate | 2386 (30.1) | 17.6 (15.5–19.8) | |
| High | 2491 (31.4) | 35.6 (33.1–38.2) | |
| Educational attainment | <0.001* | ||
| No formal education | 3558 (44.8) | 3.8 (3.0–4.8) | |
| Primary | 1202 (15.2) | 16.5 (13.8–19.5) | |
| Secondary+ | 3176 (40.0) | 34.0 (31.8–36.3) | |
| Media use | <0.001* | ||
| No | 3176 (40.0) | 5.3 (4.3–6.4) | |
| Yes | 4760 (60.0) | 25.2 (23.3–27.0) | |
| Women’s age | <0.001* | ||
| 15–19 | 698 (8.8) | 8.0 (6.1–10.5) | |
| 20–24 | 1871 (23.6) | 14.9 (13.0–17.0) | |
| 25–29 | 2258 (28.4) | 18.7 (16.7–20.8) | |
| 30–34 | 1598 (20.1) | 22.7 (20.0–25.7) | |
| 35–39 | 1004 (12.7) | 18.7 (15.9–21.8) | |
| 40–44 | 405 (5.1) | 14.8 (10.7–20.0) | |
| 45–49 | 102 (1.3) | 11.5 (5.7–21.9) | |
| Wanted child when became pregnant | <0.001* | ||
| Then | 6920 (87.2) | 16.5 (15.2–18.0) | |
| Later | 790 (10.0) | 23.2 (20.1–26.7) | |
| No more | 226 (2.8) | 23.9 (17.4–32.0) | |
| Health insurance | <0.001* | ||
| Not covered | 7789 (98.1) | 17.0 (15.7–18.3) | |
| Covered | 147 (1.9) | 39.3 (30.0–49.4) | |
| Marital Status | 0.847 | ||
| Never in union | 212 (2.7) | 17.7 (12.4–24.8) | |
| Currently married/living with a partner | 7588 (95.6) | 17.3 (16.0–18.7) | |
| Formerly in union | 136 (1.7) | 19.6 (11.8–30.8) | |
| Employment status | <0.001* | ||
| Not working | 2926 (36.9) | 11.0 (9.6–12.6) | |
| Working | 5010 (63.1) | 21.1 (19.5–22.9) | |
| Family type | <0.001* | ||
| Monogyny | 5345 (70.6) | 21.0 (19.8–23.0) | |
| Polygyny | 2222 (29.4) | 8.2 (6.8–9.8) | |
| Intimate partner violence | 0.066* | ||
| No | 1471 (60.0) | 24.0 (21.6–26.7) | |
| Yes | 980 (40.0) | 20.2 (17.4–23.4) | |
| Women’s autonomy | <0.001* | ||
| Low | 3255 (42.9) | 8.9 (7.6–10.2) | |
| Moderate | 2156 (28.4) | 16.3 (14.4–18.6) | |
| High | 2177 (28.7) | 31.3 (28.6–34.1) | |
| Time of antenatal care initiation (in months)a | <0.001* | ||
| <eight ANC contacts | 4595 | 5.0±1.5 | |
| Eight or more ANC contacts | 1300 | 3.7±1.4 | |
| Household headship | <0.001* | ||
| Male | 7245 (91.3) | 16.5 (15.2–17.8) | |
| Female | 691 (8.7) | 27.6 (23.8–31.8) | |
| Household wealth quintile | <0.001* | ||
| Poorest | 1689 (21.3) | 8.1 (6.6–10.0) | |
| Poorer | 1710 (21.6) | 10.8 (9.0–13.0) | |
| Middle | 1656 (20.9) | 14.9 (12.5–17.8) | |
| Richer | 1524 (19.2) | 20.1 (17.2–23.5) | |
| Richest | 1357 (17.1) | 37.6 (33.9–41.4) | |
| Household size | <0.001* | ||
| 1–4 | 2303 (29.0) | 24.4 (21.9–27.1) | |
| 5–8 | 3562 (44.9) | 18.9 (17.2–20.7) | |
| 8+ | 2071 (26.1) | 6.9 (5.6–8.3) | |
| Residential status | <0.001* | ||
| Urban | 2623 (33.1) | 31.2 (28.6–33.9) | |
| Rural | 5313 (66.9) | 9.4 (8.3–10.5) | |
| Geographical region | <0.001* | ||
| North Central | 1365 (17.2) | 14.5 (12.1–17.1) | |
| North East | 1692 (21.3) | 3.5 (2.6–4.7) | |
| North West | 2497 (31.5) | 3.7 (2.8–4.8) | |
| South East | 871 (11.0) | 35.6 (31.4–40.1) | |
| South South | 734 (9.2) | 36.1 (31.2–41.2) | |
| South West | 777 (9.8) | 61.0 (55.6–66.2) | |
| Cultural norm for wife beating | <0.001* | ||
| No | 5303 (66.8) | 22.2 (20.5–24.2) | |
| Yes | 2633 (33.2) | 7.7 (6.4–9.1) | |
| Community-level poverty | <0.001* | ||
| Low | 3922 (49.4) | 28.2 (25.6–30.9) | |
| High | 4014 (50.6) | 5.9 (4.9–7.0) | |
| Community-level media use | <0.001* | ||
| Low | 3981 (50.2) | 5.7 (4.5–7.1) | |
| High | 3955 (49.8) | 29.0 (26.8–31.4) | |
| Community-level illiteracy | <0.001* | ||
| Low | 3741 (47.1) | 32.5 (30.1–34.9) | |
| High | 4195 (52.9) | 4.7 (3.8–5.7) | |
| Community-level urban residence | <0.001* | ||
| Low | 5313 (66.9) | 9.4 (8.3–10.5) | |
| High | 2623 (33.1) | 31.2 (28.6–33.9) | |
| Community-level women’s autonomy | <0.001* | ||
| Low | 4050 (51.0) | 8.6 (7.3–10.1) | |
| High | 3886 (49.0) | 26.8 (24.5–29.3) |
*Significant at p<0.25; a = mean ± standard deviation
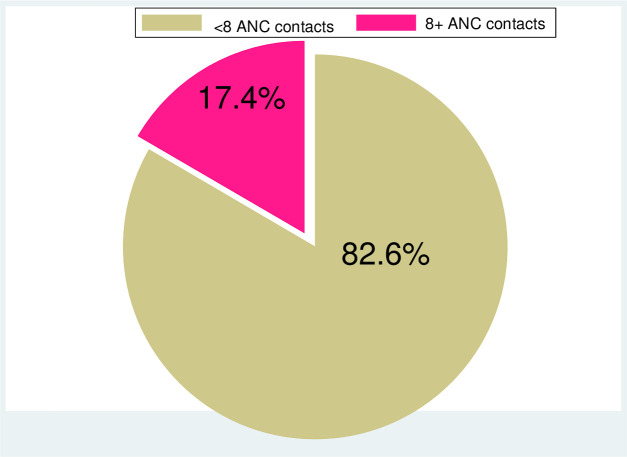
Prevalence of eight or more ANC contacts in Nigeria
Result from Fig 1 showed the prevalence of eight or more ANC contacts in Nigeria. Approximately 17.4% (95% CI: 16.1%-18.7%) had the optimal ANC contacts as recommended in the new WHO eight ANC guideline.
Fig 1. Prevalence of eight or more ANC contacts in Nigeria.
Measures of variations (random effects) and model fit statistics
In Table 2, Model V (full model) was selected as the most suitable due to the least AIC and BIC values (1371.30 and 1611.81 respectively). The variations in the odds of eight or more ANC contacts across communities (σ2 = 1.32; SE = 0.22) and households (σ2 = 0.01; SE = 4.16) were estimated. Results from Median Odds Ratio became the evidence of community contextual factors shaping eight or more ANC contacts. It was estimated that if a women moved to another community or household with a higher probability of eight or more ANC contacts, the median increase in their odds of eight or more ANC contacts would be 3.51 with ICC of 34.5%. MOR equal to unity, indicated no household variance given ICC of 0.0%. In both community and household levels, the explained variances were about 78.3% and 99.8% respectively. This implied that large amount of variances in eight or more ANC contacts have been explained by the household-level factors. Furthermore, VPC for community and household levels were estimated to 18.1% and 72.7% respectively.
Table 2. Random effect estimates of individual-, household- and community-level factors associated with eight or more ANC contacts in Nigeria.
| Random-effect | Model I | Model II | Model III | Model IV | Model V |
|---|---|---|---|---|---|
| Community-level | |||||
| Variance (SE) | 6.09 (1.06)* | 1.68 (0.22)* | 2.71 (0.54)* | 1.43 (0.21)* | 1.32 (0.22) |
| VPC | 43.8% | 30.2% | 39.6% | 19.4% | 18.1% |
| Explained variance (PCV) | Reference | 72.4% | 55.5% | 76.5% | 78.3% |
| MOR | 330 | 4.98 | 13.25 | 3.91 | 3.51 |
| ICC | 63.0% | 46.3% | 53.1% | 25.6% | 34.5% |
| Household-level | |||||
| Variance (SE) | 4.31 (0.77)* | 1.48 x 10−06 (1.07) | 1.79 (0.68) | 1.63 (0.48) | 0.01 (4.16) |
| VPC | 29.2% | 61.6% | 31.3% | 41.9% | 72.7% |
| Explained variance (PCV) | Reference | 65.7% | 58.5% | 62.2% | 99.8% |
| MOR | 61.28 | 1.00 | 5.50 | 4.71 | 1.01 |
| ICC | 32.0% | 0.0% | 23.1% | 33.1% | 0.0% |
| Model fit statistics | |||||
| AIC | 5900.83 | 1553.01 | 5741.17 | 5077.92 | 1371.30 |
| BIC | 5921.73 | 1695.13 | 5810.84 | 5175.44 | 1611.81 |
Model I–empty null model, baseline model without any explanatory variables (unconditional model)
Model II–adjusted for only individual-level factors
Model III–adjusted for only household-level factors
Model IV–adjusted for only community-level factors
Model V–adjusted for individual-, household-, and community-level factors (full model)
VPC Variance Partition Coefficient, AIC Akaike's Information Criterion, BIC Bayesian Information Criterion, PCV Proportional Change in Variance, ICC Intra-class correlation
*Significant at p<0.05
Measures of associations (fixed effects)
Model V has been selected as the best model because it has the least AIC and BIC values (Table 2). Based on the results, women with at least secondary were 2.46 times as likely to have eight or more ANC contacts when compared with women with no formal education (AOR = 2.46; 95%CI: 1.21, 4.99) (Table 3). Furthermore, women who use media were 2.37 times as likely to have eight or more ANC contacts, when compared with women who do not use media (AOR = 2.37; 95%CI: 1.32, 4.24). In addition, for every unit increase in the time (month) of ANC initiation, there is 53% reduction in the odds of eight or more ANC contacts (AOR = 0.47; 95%CI: 0.40, 0.55). Rural women had 60% reduction in the odds of eight or more ANC contacts, when compared with their urban counterparts (AOR = 0.40; 95%CI: 0.24, 0.66). Geographical region was significantly associated with the odds of eight or more ANC contacts; women from North East and North West had 74% and 79% reduction in the odds of eight or more ANC contacts and women from South East, South South and South West were 2.68, 5.00 and 14.22 times as likely to have eight or more ANC contacts respectively, when compared with women from North Central.
Table 3. Fixed effect of individual-, household- and community-level factors associated with eight or more ANC contacts in Nigeria.
| Variable | Model I | Model II | Model III | Model IV | Model V |
|---|---|---|---|---|---|
| Individual level factors | |||||
| Family mobility | |||||
| Internal immigrant | 1.00 | 1.00 | |||
| Native | 1.13 (0.73–1.74) | 1.40 (0.91–2.15) | |||
| Religion | |||||
| Christianity | 1.00 | 1.00 | |||
| Islam | 0.62 (0.40–0.96)* | 1.26 (0.74–2.14) | |||
| ATR/others | 2.14 (0.18–24.95) | 1.56 (0.14–17.70) | |||
| Number of children ever born | |||||
| 1–2 | 1.00 | 1.00 | |||
| 3–4 | 1.01 (0.65–1.56) | 1.27 (0.76–2.10) | |||
| 4+ | 0.64 (0.36–1.15) | 1.27 (0.65–2.46) | |||
| Educational attainment | |||||
| No formal education | 1.00 | 1.00 | |||
| Primary | 3.69 (1.87–7.27)* | 1.93 (0.96–3.92) | |||
| Secondary+ | 6.02 (3.18–11.42)* | 2.46 (1.21–4.99)* | |||
| Media use | |||||
| No | 1.00 | 1.00 | |||
| Yes | 3.62 (2.15–6.09)* | 2.37 (1.32–4.24)* | |||
| Women’s age | |||||
| 15–19 | 1.00 | 1.00 | |||
| 20–24 | 1.78 (0.73–4.37) | 1.22 (0.49–3.04) | |||
| 25–29 | 2.05 (0.83–5.08) | 1.00 (0.40–2.51) | |||
| 30–34 | 2.47 (0.97–6.34) | 0.97 (0.37–2.55) | |||
| 35–39 | 2.78 (1.01–7.72)* | 1.09 (0.39–3.10) | |||
| 40–44 | 5.75 (1.59–20.79)* | 2.38 (0.65–8.73) | |||
| 45–49 | 3.78 (0.65–22.06) | 0.73 (0.11–4.78) | |||
| Wanted child when became pregnant | |||||
| Then | 1.00 | 1.00 | |||
| Later | 1.40 (0.82–2.41) | 1.32 (0.76–2.28) | |||
| No more | 1.64 (0.61–4.37) | 1.12 (0.43–2.92) | |||
| Health insurance | |||||
| Not covered | 1.00 | 1.00 | |||
| Covered | 0.74 (0.26–2.14) | 0.79 (0.28–2.25) | |||
| Employment status | |||||
| Not working | 1.00 | 1.00 | |||
| Working | 1.68 (1.10–2.58)* | 1.31 (0.85–2.03) | |||
| Family type | |||||
| Monogamy | 1.00 | 1.00 | |||
| Polygyny | 1.55 (0.92–2.62) | 1.61 (0.91–2.85) | |||
| Intimate partner violence | |||||
| No | 1.00 | 1.00 | |||
| Yes | 0.82 (0.57–1.18) | 1.32 (0.90–1.92) | |||
| Women’s autonomy | |||||
| Low | 1.00 | 1.00 | |||
| Moderate | 1.20 (0.74–1.93) | 1.04 (0.61–1.78) | |||
| High | 1.16 (0.73–1.84) | 0.78 (0.46–1.33) | |||
| Time of antenatal care initiation (in months) | 0.47 (0.41–0.55)* | 0.47 (0.40–0.55)* | |||
| Household-level factors | |||||
| Household headship | |||||
| Male | 1.00 | 1.00 | |||
| Female | 1.22 (0.83–1.80) | 0.87 (0.49–1.54) | |||
| Household wealth quintile | |||||
| Poorest | 1.00 | 1.00 | |||
| Poorer | 1.83 (1.12–2.99)* | 0.48 (0.23–0.97)* | |||
| Middle | 2.60 (1.46–4.65)* | 0.57 (0.27–1.18) | |||
| Richer | 4.34 (2.15–8.78)* | 0.61 (0.29–1.29) | |||
| Richest | 15.03 (4.99–45.26)* | 1.19 (0.53–2.65) | |||
| Household size | |||||
| 1–4 | 1.00 | 1.00 | |||
| 5–8 | 0.76 (0.57–1.01) | 0.88 (0.55–1.40) | |||
| 8+ | 0.32 (0.19–0.55)* | 1.08 (0.52–2.23) | |||
| Community-level factors | |||||
| Residential status | |||||
| Urban | 1.00 | 1.00 | |||
| Rural | 0.54 (0.38–0.77)* | 0.40 (0.24–0.66)* | |||
| Geographical region | |||||
| North Central | 1.00 | 1.00 | |||
| North East | 0.18 (0.09–0.36)* | 0.26 (0.11–0.60)* | |||
| North West | 0.18 (0.10–0.34)* | 0.21 (0.09–0.50)* | |||
| South East | 3.39 (1.93–5.94) | 2.68 (1.37–5.23)* | |||
| South South | 2.75 (1.61–4.69)* | 5.00 (2.40–10.40)* | |||
| South West | 18.77 (7.46–47.23)* | 14.22 (7.12–28.41)* | |||
| Cultural norm for wife beating | |||||
| No | 1.00 | 1.00 | |||
| Yes | 0.80 (0.60–1.06) | 0.76 (0.47–1.22) | |||
| Community-level poverty | |||||
| Low | 1.00 | 1.00 | |||
| High | 0.55 (0.37–0.82)* | 0.94 (0.52–1.73) | |||
| Community-level media use | |||||
| Low | 1.00 | 1.00 | |||
| High | 1.30 (0.88–1.92) | 0.60 (0.32–1.13) | |||
| Community-level illiteracy | |||||
| Low | 1.00 | 1.00 | |||
| High | 0.48 (0.31–0.73)* | 0.99 (0.54–1.82) | |||
| Community-level women’s autonomy | |||||
| Low | 1.00 | 1.00 | |||
| High | 1.13 (0.82–1.55) | 0.96 (0.57–1.63) |
Model I–empty null model, baseline model without any explanatory variables (unconditional model)
Model II–adjusted for only individual-level factors
Model III–adjusted for only household-level factors
Model IV–adjusted for only community-level factors
Model V–adjusted for individual-, household-, and community-level factors (full model)
*Significant at p<0.05
Discussion
Three years have passed since the endorsement of the minimum eight ANC contacts guideline. In Nigeria, this study stands in the frontline to determine eight or more ANC coverage and the factors that influence ANC contacts among women. Specifically, the guideline stipulates that the first ANC contact takes place within the first trimester of the pregnancy, that is, 12 weeks of gestation, while the next two contacts take place during the second trimester of the pregnancy that is between the 20th and 26th gestation weeks. About five contacts are due to take place during the third trimester, that is between 30th through the 40th week of gestation [35].
Our study revealed that 17.4% of women had the updated WHO recommendation of eight ANC contacts. This shows that compliance with the updated recommendation is low, probably because it may not have been adopted as a national policy. This study reported a higher prevalence than a previous study conducted using Benin population-based data which also examined the coverage of eight or more ANC visits [36]. Similarly, the observed prevalence is slightly higher than results from a previous multi-country study that revealed 15.3% of mothers had eight or more antenatal contacts; with the first contact in the first trimester of pregnancy. Unfortunately, that study utilized data collected before the endorsement of the eight ANC guideline [37]. Therefore, the basis for the eight or more ANC in that study is not certain. In another study, only 6.1% of mothers reported eight or more ANC contacts [38]. Also, the data used was collected before the endorsement of the WHO eight ANC guideline and the findings cannot be credited to the implementation or non-implementation of the guideline. Since the WHO recommendations were released in 2016 [8], it could be that before 2016, women who had eight or more ANC contacts were probably high-risk pregnancies that required close monitoring by a healthcare provider. With the new guideline [8,35], healthcare providers will have the basis to schedule a woman with normal pregnancy for eight or more contacts.
Among the individual-level factors examined, educational attainment, media use, and timing to ANC initiation were significantly associated with eight or more ANC contacts in Nigeria. The place of residence and geographical region were also significant factors at the community level. We found that education had a positive association with having eight or more ANC contacts. Women who had primary and secondary or higher education had increased odds of eight or more ANC contacts compared with women who had no formal education. Similarly, a study in Bangladesh found education to be positively associated with eight or more ANC contacts during pregnancy [38]. Studies that have examined 4 or more ANC contacts in different settings, have consistently reported that women with higher levels of education have a higher prevalence and greater odds of 4 or more ANC contacts [39–47]. Maternal education is associated with the use of basic maternal health services including ANC [40,48] and lack of formal education has been associated with under-utilization or non-use of ANC [12,49]. Maternal education can improve health care literacy; thus, they are more aware of danger signs and may be able to identify signs of pregnancy complications. Also educated women may be more appreciative of the advantages of utilizing health care services including ANC [41,50–53]. Furthermore, it can enhance women’s socioeconomic opportunities and status [52] decision-making power [41,52,54,55], and the confidence to take actions about their health [25,43,56].
In addition, media use and early timing to ANC initiation were significantly associated with eight or more ANC contacts. Previous studies have reported similar findings with regards to eight or more ANC contacts [38] and 4 or more ANC contacts [40,41,47,57,58]. Media access may improve women’s enlightenment positively and ANC utilization via health education and influences maternal health care seeking behaviour [41,59,60]; pregnant women who listen to the radio, watch the television or read the newspaper, are more likely to have important health information and messages about maternal health services and advantages of utilizing them [38,41,44,60]. This underscores the importance of social and behavioural change communication to increase awareness and create demand for the use of maternal health services [12]. Similarly, the findings from previous studies showed that women enlightenment and early ANC initiation were significantly associated with eight or more ANC contacts [36,61]. There is no doubt, that early booking for ANC would result in optimal number of ANC contacts during pregnancy as those who start early will have higher possibility of achieving optimal ANC visits.
At the community level, we found that having eight or more ANC contacts differed significantly between geographical regions of the country, with the highest proportions reported in the South West and the lowest was observed in the North East. Although there is paucity of studies that have examined eight or more ANC visits in Nigeria, previous studies that explored 4 or more ANC visits found a similar pattern of geographic variation, with higher levels of ANC use in the South West and South East, and lower levels of use in the Northern regions [11,16,39,62]. In their study, Adewuyi et al. found that the highest proportion of mothers that had 4 or more ANC visits were in Southwest of Nigeria; only 10.2% reported having less than 4 or more ANC contacts [12]. Differences in socioeconomic development, educational attainment, accessibility to health facilities may be responsible for the observed geographical variations [39,63]. Also, security challenges in parts of the North (insurgency) and South-South (militancy) may contribute to the observed variation [12,64,65].
Women residing in rural areas had reduction in eight or more ANC contacts compared with their urban counterparts. In a previous study, Islam et al reported similar finding [38]. Other studies of determinants of 4 or more ANC contacts have reported similar findings [12,41,43,45,47,66]. There are significant differentials in rural-urban utilization of maternal health services including ANC due to inequities in the distribution of accessible health resources between rural and urban areas [11,12,41,48,67]. Where facilities exist, they may be inaccessible due to poor road network, inefficient transport system or very far distances [12]. Furthermore, rural areas are inadequately financed, and it is difficult to attract and retain health workers in such places [11]. Also, women residing in rural areas may have lower socioeconomic status than their counterparts in urban areas, which might make utilization of ANC services less likely [45,68]. Women in rural areas may be more influenced by cultural beliefs and social norms that discourage utilization of skilled maternal care services [56].
This study provides empirical data on the coverage of the WHO recommended eight or more ANC contacts during pregnancy. This information can inform policy makers in drawing up national guidelines on ANC utilization, which are in line with WHO recommendations. However, designing the guidelines may not be enough to ensure adherence. Thus, there is need to ensure those guidelines reach the end-users, from the pre-service trainees to the in-service health workers. This study also highlights the gap in attainment of the recommended eight or more ANC contacts with regards to area of residence. Thus, ANC services should be provided to women residing in the hard-to-reach areas through establishment and strengthening of primary health care (PHC). Also making ANC services subsidized or free, for example through the basic health care provision fund, can serve as an incentive to encourage ANC attendance. Also important is the need for strategically designed health promotion programs that utilize locally contextualized social behaviour change communication (SBCC) messages to create awareness and increase demand for ANC services. As the present study explored the subject from the client’s perspective, future research can examine the demand-side factors of ANC contacts among women and/or ANC coverage from the health workers perspective, both quantitatively and qualitatively.
Strengths and limitations
The major strength of this study is that it has become the foremost population-based study on eight or more ANC contacts in Nigeria, therefore, it will serve as a stimulus and benchmark for further studies. In addition, the use of nationally representative data makes the findings generalizable to women of reproductive age in Nigeria. The use of data collected after the endorsement of the new eight or more ANC contacts, make this study of plausible conclusion. Conversely, the use of cross-sectional data established that only associations and no causal relationships are reported. In addition, we could not measure the sources of demand-side unobserved heterogeneity across the secondary data and this could cause some bias in our findings. The unavailability of relevant variables such as women’s perception and awareness of skilled maternal health care was a major limitation in the DHS data. Hence, we considered supply-side limitations of data to those issues related to health care delivery. More so, recall bias could have occurred in this study due to self-reported number of ANC contacts, except when ANC contacts were determined using hospital cards.
Conclusion
In this study, we have revealed that achievement of the WHO recommended eight or more ANC contacts was poor and can be influenced multilevel factors. Therefore, there is need for a national adoption of the WHO recommendation and to encourage implementation. There should be concerted efforts from health care stakeholders in the improvement of maternal socioeconomic status, as well as create awareness among the populace for optimal utilization of ANC. Interventions to improve ANC attendance should also target barriers linked with inequities and inequalities in ANC utilization as related to geographical residence.
Acknowledgments
The authors appreciate the MEASURE DHS project for the approval and access to the original data.
Data Availability
The data underlying the results presented in the study are available from The Demographic and Health Surveys Program (http://dhsprogram.com/data/available-datasets.cfm). The individual woman questionnaire from the 2018 Nigeria Demographic and Health Survey was analyzed in this study. The authors of the present study had no special access privileges in accessing these data sets.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Lomazzi M, Borisch B, Laaser U. The Millennium Development Goals: experiences, achievements and what’s next. Glob Health Action [Internet]. 2014. February 13 [cited 2020 Apr 26];7 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3926985/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization, UNICEF, United Nations, Department of Economic and Social Affairs, Population Division, World Bank. Trends in maternal mortality: 1990 to 2015: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division [Internet]. 2015 [cited 2019 Apr 3]. Available from: http://www.who.int/reproductivehealth/publications/monitoring/maternal-mortality-2015/en/
- 3.Kumar S, Kumar N, Vivekadhish S. Millennium Development Goals (MDGs) to Sustainable Development Goals (SDGs): Addressing Unfinished Agenda and Strengthening Sustainable Development and Partnership. Indian Journal of Community Medicine: Official Publication of Indian Association of Preventive & Social Medicine. 2016. March;41(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosa W. Transforming Our World: The 2030 Agenda for Sustainable Development. In: A New Era in Global Health [Internet]. New York, NY: Springer Publishing Company; 2017. [cited 2019 Feb 14]. Available from: http://connect.springerpub.com/lookup/doi/10.1891/9780826190123.ap02 [Google Scholar]
- 5.Alkema L, Chou D, Hogan D, Zhang S, Moller A-B, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. The Lancet. 2016. January;387(10017):462–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Downe S, Finlayson K, Tunçalp Ö, Gülmezoglu AM. Provision and uptake of routine antenatal services: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews [Internet]. 2019. [cited 2020 Jan 5]; Available from: https://www.readcube.com/articles/10.1002/14651858.CD012392.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO. WHO antenatal care randomized trial: manual for the implementation of the new model [Internet]. World Health Organization; 2002. [cited 2020 Feb 22]. Available from: https://apps.who.int/iris/handle/10665/42513 [Google Scholar]
- 8.World Health Organization, editor. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: World Health Organization; 2016. 152 p. [PubMed] [Google Scholar]
- 9.Nwosu CO, Ataguba JE. Socioeconomic inequalities in maternal health service utilisation: a case of antenatal care in Nigeria using a decomposition approach. BMC Public Health. 2019. December;19(1):1493 10.1186/s12889-019-7840-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO | Maternal health in Nigeria: generating information for action [Internet]. WHO. [cited 2020 Jan 5]. Available from: http://www.who.int/reproductivehealth/maternal-health-nigeria/en/
- 11.Fagbamigbe AF, Idemudia ES. Barriers to antenatal care use in Nigeria: evidences from non-users and implications for maternal health programming. BMC Pregnancy Childbirth. 2015. December;15(1):95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adewuyi EO, Auta A, Khanal V, Bamidele OD, Akuoko CP, Adefemi K, et al. Prevalence and factors associated with underutilization of antenatal care services in Nigeria: A comparative study of rural and urban residences based on the 2013 Nigeria demographic and health survey. Oh J, editor. PLoS ONE. 2018. May 21;13(5):e0197324 10.1371/journal.pone.0197324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adu J, Tenkorang E, Banchani E, Allison J, Mulay S. The effects of individual and community-level factors on maternal health outcomes in Ghana. Biemba G, editor. PLoS ONE. 2018. November 29;13(11):e0207942 10.1371/journal.pone.0207942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yaya S, Uthman OA, Amouzou A, Ekholuenetale M, Bishwajit G. Inequalities in maternal health care utilization in Benin: a population based cross-sectional study. BMC Pregnancy and Childbirth [Internet]. 2018. December [cited 2019 Feb 19];18(1). Available from: https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-018-1846-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yaya S, Bishwajit G, Ekholuenetale M, Shah V, Kadio B, Udenigwe O. Timing and adequate attendance of antenatal care visits among women in Ethiopia. Larson BA, editor. PLOS ONE. 2017. September 18;12(9):e0184934 10.1371/journal.pone.0184934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fagbamigbe AF, Idemudia ES. Wealth and antenatal care utilization in Nigeria: Policy implications. Health Care for Women International. 2017. January 2;38(1):17–37. 10.1080/07399332.2016.1225743 [DOI] [PubMed] [Google Scholar]
- 17.Kruk ME, Kujawski S, Moyer CA, Adanu RM, Afsana K, Cohen J, et al. Next generation maternal health: external shocks and health-system innovations. Lancet. 2016. November 5;388(10057):2296–306. 10.1016/S0140-6736(16)31395-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tegegne TK, Chojenta C, Getachew T, Smith R, Loxton D. Antenatal care use in Ethiopia: a spatial and multilevel analysis. BMC Pregnancy Childbirth. 2019. December;19(1):399 10.1186/s12884-019-2550-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huda TM, Chowdhury M, El Arifeen S, Dibley MJ. Individual and community level factors associated with health facility delivery: A cross sectional multilevel analysis in Bangladesh. Kamperman AM, editor. PLoS ONE. 2019. February 13;14(2):e0211113 10.1371/journal.pone.0211113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Corsi DJ, Neuman M, Finlay JE, Subramanian S. Demographic and health surveys: a profile. International Journal of Epidemiology. 2012. December 1;41(6):1602–13. 10.1093/ije/dys184 [DOI] [PubMed] [Google Scholar]
- 21.Tunçalp Ӧ., Pena-Rosas J, Lawrie T, Bucagu M, Oladapo O, Portela A, et al. WHO recommendations on antenatal care for a positive pregnancy experience-going beyond survival. BJOG: An International Journal of Obstetrics & Gynaecology. 2017. May;124(6):860–2. [DOI] [PubMed] [Google Scholar]
- 22.de Masi S, Bucagu M, Tunçalp Ö, Peña-Rosas JP, Lawrie T, Oladapo OT, et al. Integrated Person-Centered Health Care for All Women During Pregnancy: Implementing World Health Organization Recommendations on Antenatal Care for a Positive Pregnancy Experience. Glob Health Sci Pract. 2017. June 27;5(2):197–201. 10.9745/GHSP-D-17-00141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yaya S, Uthman OA, Ekholuenetale M, Bishwajit G. Women empowerment as an enabling factor of contraceptive use in sub-Saharan Africa: a multilevel analysis of cross-sectional surveys of 32 countries. Reproductive Health [Internet]. 2018. December [cited 2019 Mar 22];15(1). Available from: https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-018-0658-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Uthman OA, Lawoko S, Moradi T. Factors associated with attitudes towards intimate partner violence against women: a comparative analysis of 17 sub-Saharan countries. BMC Int Health Hum Rights. 2009. December;9(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tiruneh FN, Chuang K-Y, Chuang Y-C. Women’s autonomy and maternal healthcare service utilization in Ethiopia. BMC Health Serv Res. 2017. December;17(1):718 10.1186/s12913-017-2670-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rutstein SO, Staveteig S. Making the Demographic and Health Surveys Wealth Index Comparable. 2014;DHS Methodological Reports No. 9. Rockville, Maryland, USA: ICF International. [Google Scholar]
- 27.Hruschka DJ, Gerkey D, Hadley C. Estimating the absolute wealth of households. Bulletin of the World Health Organization. 2015. July 1;93(7):483–90. 10.2471/BLT.14.147082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Benebo FO, Schumann B, Vaezghasemi M. Intimate partner violence against women in Nigeria: a multilevel study investigating the effect of women’s status and community norms. BMC Women’s Health. 2018. December;18(1):136 10.1186/s12905-018-0628-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mekonnen ZA, Lerebo WT, Gebrehiwot TG, Abadura SA. Multilevel analysis of individual and community level factors associated with institutional delivery in Ethiopia. BMC Res Notes. 2015. December;8(1):376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ejembi CL, Dahiru T, Aliyu AA. Contextual factors influencing modern contraceptive use in Nigeria. 2015 [cited 2019 Apr 2]; Available from: https://dhsprogram.com/publications/publication-wp120-working-papers.cfm
- 31.Midi H, Sarkar SK, Rana S. Collinearity diagnostics of binary logistic regression model. Journal of Interdisciplinary Mathematics. 2010. June;13(3):253–67. [Google Scholar]
- 32.Spiegelhalter DJ, Best NG, Carlin BP, van der Linde A. Bayesian measures of model complexity and fit. J Royal Statistical Soc B. 2002. October;64(4):583–639. [Google Scholar]
- 33.Larsen K, Merlo J. Appropriate assessment of neighborhood effects on individual health: integrating random and fixed effects in multilevel logistic regression. Am J Epidemiol. 2005. January 1;161(1):81–8. 10.1093/aje/kwi017 [DOI] [PubMed] [Google Scholar]
- 34.Stawski RS. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling (2nd Edition). Structural Equation Modeling: A Multidisciplinary Journal. 2013. July 1;20(3):541–50. [Google Scholar]
- 35.WHO. WHO recommendation on antenatal care contact schedules. The WHO reproductive Health Libra. 2018;(March):1–7. [Google Scholar]
- 36.Ekholuenetale M, Nzoputam CI, Barrow A, Onikan A. Women’s enlightenment and early antenatal care initiation are determining factors for the use of eight or more antenatal visits in Benin: further analysis of the Demographic and Health Survey. J Egypt Public Health Assoc. 2020. December;95(1):13 10.1186/s42506-020-00041-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Benova L, Tunçalp Ö, Moran AC, Campbell OMR. Not just a number: examining coverage and content of antenatal care in low-income and middle-income countries. BMJ Global Health [Internet]. 2018. April 1 [cited 2020 Feb 3];3(2). Available from: https://gh.bmj.com/content/3/2/e000779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Islam MM, Masud MS. Determinants of frequency and contents of antenatal care visits in Bangladesh: Assessing the extent of compliance with the WHO recommendations. PLoS One [Internet]. 2018. September 27 [cited 2020 Feb 3];13(9). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6160162/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Babalola BI. Determinants of urban-rural differentials of antenatal care utilization in Nigeria. African Population Studies. 2014. September 22;28(3):1263–73. [Google Scholar]
- 40.Awoleye AF, Victor C, Alawode OA. Women autonomy and maternal healthcare services utilization among young ever-married women in Nigeria. Int J Nurs Midwifery. 2018. June 30;10(6):62–73. [Google Scholar]
- 41.Basha GW. Factors Affecting the Utilization of a Minimum of Four Antenatal Care Services in Ethiopia. Obstet Gynecol Int [Internet]. 2019. August 14 [cited 2020 Feb 15];2019. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6710775/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hijazi HH, Alyahya MS, Sindiani AM, Saqan RS, Okour AM. Determinants of antenatal care attendance among women residing in highly disadvantaged communities in northern Jordan: a cross-sectional study. Reproductive Health. 2018. June 7;15(1):106 10.1186/s12978-018-0542-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tekelab T, Chojenta C, Smith R, Loxton D. Factors affecting utilization of antenatal care in Ethiopia: A systematic review and meta-analysis. PLoS One [Internet]. 2019. April 11 [cited 2020 Feb 15];14(4). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6459485/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Islam MM, Masud MS. Health care seeking behaviour during pregnancy, delivery and the postnatal period in Bangladesh: Assessing the compliance with WHO recommendations. Midwifery. 2018. August 1;63:8–16. 10.1016/j.midw.2018.04.021 [DOI] [PubMed] [Google Scholar]
- 45.Okedo-Alex IN, Akamike IC, Ezeanosike OB, Uneke CJ. Determinants of antenatal care utilisation in sub-Saharan Africa: a systematic review. BMJ Open [Internet]. 2019. October 1 [cited 2020 Feb 5];9(10). Available from: https://bmjopen.bmj.com/content/9/10/e031890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tiruaynet K, Muchie KF. Determinants of utilization of antenatal care services in Benishangul Gumuz Region, Western Ethiopia: a study based on demographic and health survey. BMC Pregnancy and Childbirth. 2019. April 3;19(1):115 10.1186/s12884-019-2259-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim S, Kim S-Y. Exploring factors associated with maternal health care utilization in Chad. J Glob Health Sci. 2019;1:e31. [Google Scholar]
- 48.Banke-Thomas OE, Banke-Thomas AO, Ameh CA. Factors influencing utilisation of maternal health services by adolescent mothers in Low-and middle-income countries: a systematic review. BMC Pregnancy and Childbirth. 2017. February 16;17(1):65 10.1186/s12884-017-1246-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mustafa MH, Mukhtar AM. Factors associated with antenatal and delivery care in Sudan: analysis of the 2010 Sudan household survey. BMC Health Serv Res [Internet]. 2015. October 4 [cited 2020 Feb 15];15 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4592751/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ali SA, Dero AA, Ali SA, Ali GB. Factors affecting the utilization of antenatal care among pregnant women: A literature review. Journal of Pregnancy and Neonatal Medicine [Internet]. 2018. [cited 2020 Feb 3];2(2). Available from: https://www.alliedacademies.org/abstract/factors-affecting-the-utilization-of-antenatal-care-among-pregnant-women-a-literature-review-10793.html [Google Scholar]
- 51.Mumtaz S, Bahk J, Khang Y-H. Current status and determinants of maternal healthcare utilization in Afghanistan: Analysis from Afghanistan Demographic and Health Survey 2015. PLOS ONE. 2019. June 11;14(6):e0217827 10.1371/journal.pone.0217827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Weitzman A. The Effects of Women’s Education on Maternal Health: Evidence from Peru. Soc Sci Med. 2017. May;180:1–9. 10.1016/j.socscimed.2017.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Smith-Greenaway E. Maternal Reading Skills and Child Mortality in Nigeria: A Reassessment of Why Education Matters. Demography. 2013. October;50(5):1551–61. 10.1007/s13524-013-0209-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tsala Dimbuene Z, Amo-Adjei J, Amugsi D, Mumah J, Izugbara CO, Beguy D. Women’s education and utilization of maternal health services in Africa: a multi-country and socioeconomic status analysis. J Biosoc Sci. 2018. November;50(6):725–48. 10.1017/S0021932017000505 [DOI] [PubMed] [Google Scholar]
- 55.Shahabuddin ASM, Delvaux T, Abouchadi S, Sarker M, De Brouwere V. Utilization of maternal health services among adolescent women in Bangladesh: A scoping review of the literature. Trop Med Int Health. 2015. July;20(7):822–9. 10.1111/tmi.12503 [DOI] [PubMed] [Google Scholar]
- 56.Mekonnen T, Dune T, Perz J. Maternal health service utilisation of adolescent women in sub-Saharan Africa: a systematic scoping review. BMC Pregnancy and Childbirth. 2019. October 21;19(1):366 10.1186/s12884-019-2501-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Acharya D, Khanal V, Singh JK, Adhikari M, Gautam S. Impact of mass media on the utilization of antenatal care services among women of rural community in Nepal. BMC Res Notes [Internet]. 2015. August 12 [cited 2020 Feb 15];8 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4534014/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ousman SK, Mdala I, Thorsen VC, Sundby J, Magnus JH. Social Determinants of Antenatal Care Service Use in Ethiopia: Changes Over a 15-Year Span. Front Public Health [Internet]. 2019. [cited 2020 Feb 15];7 Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2019.00161/full [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Odesanya A, Hassan S, Olaluwoye D. Mass Media and Maternal Healthcare: A Critical Discourse. New Media and Mass Communication. 2015. January 1;63–71. [Google Scholar]
- 60.Sanda HU. Media Awareness and Utilization of Antenatal Care Services by Pregnant Women in Kano State- Nigeria. jsss. 2014. February 24;1(2):85. [Google Scholar]
- 61.Terefe AN, Gelaw AB. Determinants of Antenatal Care Visit Utilization of Child-Bearing Mothers in Kaffa, Sheka, and Bench Maji Zones of SNNPR, Southwestern Ethiopia. Health Services Research and Managerial Epidemiology. 2019. January 1;6:2333392819866620 10.1177/2333392819866620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dahiru T, Oche OM. Determinants of antenatal care, institutional delivery and postnatal care services utilization in Nigeria. Pan Afr Med J [Internet]. 2015. August 31 [cited 2020 Jan 6];21 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4633744/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sinai I, Anyanti J, Khan M, Daroda R, Oguntunde O. Demand for women’s health services in northern Nigeria: a review of the literature. African Journal of Reproductive Health. 2017. January 1;21(2):96–108. 10.29063/ajrh2017/v21i2.11 [DOI] [PubMed] [Google Scholar]
- 64.Chukwuma A, Ekhator-Mobayode UE. Armed conflict and maternal health care utilization: Evidence from the Boko Haram Insurgency in Nigeria. Social Science & Medicine. 2019. April;226:104–12. [DOI] [PubMed] [Google Scholar]
- 65.Solanke BL. Factors associated with use of maternal healthcare services during the Boko Haram insurgency in North-East Nigeria. Med Confl Surviv. 2018. September;34(3):158–84. 10.1080/13623699.2018.1511358 [DOI] [PubMed] [Google Scholar]
- 66.Amentie M, Abera M, Abdulahi M. Utilization of Antenatal Care Services and Influencing Factors among Women of Child Bearing Age in Assosa District, Benishangul Gumuz Regional State, West Ethiopia. 2015;10. [Google Scholar]
- 67.Goli S, Nawal D, Rammohan A, Sekher TV, Singh D. Decomposing the socioeconomic inequality in utilization of maternal health care services in selected countries of South Asia and sub-Saharan Africa. J Biosoc Sci. 2018;50(6):749–69. 10.1017/S0021932017000530 [DOI] [PubMed] [Google Scholar]
- 68.Fagbamigbe AF, Idemudia ES. Assessment of quality of antenatal care services in Nigeria: evidence from a population-based survey. Reprod Health [Internet]. 2015. September 18 [cited 2020 Feb 16];12 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4574449/ [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying the results presented in the study are available from The Demographic and Health Surveys Program (http://dhsprogram.com/data/available-datasets.cfm). The individual woman questionnaire from the 2018 Nigeria Demographic and Health Survey was analyzed in this study. The authors of the present study had no special access privileges in accessing these data sets.