Abstract
Objective
To test whether Minnesota's blended payment policy had differential effects on cesarean use and maternal morbidity among black women and white women in Minnesota, as compared to six control states.
Data sources/study setting
Claims data from births to Medicaid fee‐for‐service beneficiaries, 2006‐2012, in Minnesota (policy state) and six control states (Wisconsin, Iowa, Illinois, Oregon, Idaho, and Montana).
Study design
The key study intervention was Minnesota's blended payment policy, which established one single payment rate for uncomplicated vaginal and cesarean births in 2009. The primary outcome was cesarean birth, and secondary outcomes were maternal morbidity (composite), postpartum hemorrhage, and chorioamnionitis. Policy effects were assessed using race‐stratified comparative interrupted time series analysis.
Principal findings
Following policy implementation, cesarean use decreased among both black and white women in Minnesota compared to control states; this decline was larger among black women (−2.88 percent 3‐year cumulative decline, from a prepolicy cesarean rate of 22.2 percent) than among white women (−1.32 percent, P = .0013). Postpartum hemorrhage increased, with larger increases among black women (1.20 percent 3‐year cumulative increase), compared with white women (0.48 percent, P < .001) in Minnesota compared with control states.
Conclusions
Policy‐related declines in cesarean use after Minnesota's blended payment policy were larger in black women. Increases in postpartum hemorrhage signal potential unintended consequences of policy‐related cesarean reduction.
Keywords: cesarean birth, health policy, maternal outcomes
What this study adds.
Minnesota's Medicaid program adopted a blended payment policy in 2009 to curb financial incentives for overuse of cesarean birth, and cesarean use declined subsequent to this policy.
There are persistent racial/ethnic disparities in cesarean birth and maternal morbidity, and policies may affect inequities as well as overall population health.
Compared with 6 control states, Minnesota's blended payment policy was associated with a greater decline in cesarean use among Black women as compared to White women.
There were increases in postpartum hemorrhage in the postpolicy period in Minnesota that were greater among Black women than White women, signaling potential unintended policy effects.
1. INTRODUCTION
The rate of cesarean birth in the United States is widely acknowledged to be too high. 1 , 2 Cesarean birth is medically necessary in some clinical scenarios and can be a life‐saving procedure, but it also carries increased risks when used without a medical indication and/or at an early gestational age. These include risks for infants (eg, respiratory distress syndrome, admission to the neonatal intensive care unit 3 , 4 ) and birthing people (eg, infection, hysterectomy, venous thromboembolism 5 , 6 , 7 ). There are racial disparities in the rate of cesarean birth, with black women having a higher cesarean rate than their white counterparts (including cesarean birth without a medical indication). 8 , 9 , 10 , 11 It is unclear the extent to which racial disparities in cesarean birth may contribute to the heightened maternal morbidity and mortality rate for black people, compared with white people. 12 , 13 The cesarean rate has stabilized in recent years (32.0 percent in 2017), signaling that nationwide efforts to reduce primary cesarean and increase vaginal birth after cesarean might be realizing benefits. 14 Several policy actions have been proposed and implemented in the broad effort to safely reduce the cesarean rate, including policies at the level of institutions, health systems, and states. 15 , 16 , 17 , 18
One policy lever that has been shown to reduce cesarean use is the implementation of a blended payment policy. 19 A blended payment structure is a type of episode‐based payment model that provides one single payment fee for a given condition with multiple treatment options, regardless of the treatment used. In this case, the condition is uncomplicated childbirth. The blended payment approach is especially relevant to curb financial incentives for the more expensive care alternative (eg, cesarean birth 20 ) when there is no clearly superior treatment option among the choices available.
In 2009, Minnesota's Medicaid program implemented a blended payment policy—combining both professional services and facility fees into a single payment for uncomplicated births, whether cesarean or vaginal. 19 , 21 The single blended payment rate, effective on October 1 of 2009, was set to be “consistent with an increase in the proportion of births by vaginal delivery and a reduction in the percentage of births by cesarean section” in an effort to reduce payment incentives for cesarean when not medically necessary. After this date, uncomplicated births to Medicaid fee‐for‐service beneficiaries were reimbursed at the same rate regardless of mode of birth (vaginal or cesarean). Analysis of the Minnesota blended payment policy for uncomplicated births found that implementation of the policy was associated with a decrease in cesarean use and childbirth costs, compared to 6 control states with no policy change. 19 The policy‐related decrease in cesarean use amounted to more than 3 percentage points over three years (a relative decline of over 10 percent) and was not associated with any change in maternal morbidity (ie, a potential unintended consequence of such policies).
Policies affect not only average population health, but also inequities in health care and health outcomes. 22 Even general policies that are targeted at the overall population may affect population subgroups differently (eg, if members of marginalized groups are less likely to be reached by policy actions, or to access a novel intervention), such that disparities may be created or exacerbated even in the presence of overall health improvement. This has been observed, for example, among African Americans as it relates to digital diabetes monitoring and uptake of preexposure prophylaxis for HIV prevention among gay and bisexual men. 23 , 24 Several factors may explain this phenomenon, including inequitable health care access, different degrees of patient‐provider trust, and structural racism. 25 , 26 , 27 Conversely, general policies targeted at the entire population may reduce disparities, as has been documented in some smoking cessation interventions and hospital quality improvement efforts. 28 , 29
Building on prior work on the effect of the Minnesota blended payment policy for uncomplicated childbirth, we sought to assess its impact separately among white people and among black people who were Medicaid fee‐for‐service beneficiaries and who gave birth between 2006 and 2012 (inclusive). We analyzed both cesarean birth and maternal morbidity as key outcomes, and we compared Minnesota to six control states. Based on prior work documenting that rates of low‐risk cesarean birth are more sensitive to policy actions among black women, 10 we hypothesized that the postpolicy decline in cesarean birth would be greater among black women than among white women in Minnesota. Our hypothesis was based on the findings that a greater share of cesareans among black women are performed without medical indication 9 , 11 and are amenable to prevention. Changes in childbirth care have been documented to occur gradually rather than immediately in response to changes in policy and care recommendations, 10 , 30 , 31 so we hypothesized that reductions would accrue gradually in the postpolicy period, resulting in a potential trend change, rather than an immediate drop after the policy. Results from this analysis may help further explain how policies and social context (including structural racism) may translate into racial inequities, a topic of particular relevance in maternal health. 13 , 32 More importantly, these findings can direct ongoing and future policy interventions to improve maternal health, while reducing racial inequities in maternal care and outcomes.
2. METHODS
2.1. Data and study population
We used Medicaid Analytic Extract (MAX) files from three years before and after the 2009 payment change in Minnesota (ie, 2006‐2012). We compared outcomes among Minnesota beneficiaries to beneficiaries in six control states without a payment change (Wisconsin, Iowa, Illinois, Oregon, Idaho, and Montana). We chose these states as comparators because of similar geographic and/or demographic features, and because of data availability.
The analytic sample included maternal records from liveborn singleton deliveries among fee‐for‐service Medicaid beneficiaries. Births were the unit of analysis. Births are often billed to a health plan (here, Medicaid) in different ways depending on the hospital or the provider. To capture as many births as accurately as possible, we utilized the Kuklina et al 33 algorithm designed to identify births in inpatient claims data, which includes a range of both diagnosis codes and procedures codes, and also carefully excludes pregnancy‐ and labor‐related codes that do not end in childbirth. This approach utilized International Classification of Diseases, Ninth Revision (ICD‐9) diagnosis and procedure codes related to childbirth.
2.2. Variable measurement
2.2.1. Maternal race/ethnicity
We categorized maternal race/ethnicity according to race and ethnicity data available in the MAX data. Because the black/white disparity is the most pronounced and persistent racial/ethnic disparity in cesarean use and maternal health, 8 , 34 we focused this analysis on non‐Hispanic black and non‐Hispanic white women. We conceptualized of race as a social marker that identifies people at greater risk for given adverse exposures (eg, structural racism), rather than as a “risk factor” itself. 35 The final study population comprised maternal records corresponding to 426 998 births occurring in the study states between 2006 and 2012 (N = 16 336 in policy group, and N = 410 662 in control group).
2.2.2. Outcomes
We were interested in how the blended payment policy affected cesarean use among black and white women, and also in potential unintended consequences of the payment policy change. Therefore, our primary outcome was the proportion of cesarean births within each three‐month interval during our study period, stratified by maternal race. The proportion of cesarean births was calculated as a proportion of all births within each racial subgroup.
The secondary outcomes were maternal morbidities. First, we assessed the frequency of a composite maternal morbidity outcome, created based on previously published algorithms, that included postpartum hemorrhage, infection, anesthesia complications, organ failure, and other serious morbidities. 19 , 36 We were also interested in potential complications of decreased and delayed cesarean use, which increases the share of pregnant people who labor, and among laboring people increases the frequency of longer and/or more complicated labor (in part, because of a higher threshold for intervention). We separately analyzed two specific morbidities known to result from longer labor duration: postpartum hemorrhage and chorioamnionitis (uterine infection). The most common cause of postpartum hemorrhage is uterine atony, which occurs when the uterus does not contract appropriately after childbirth. Longer labor exhausts the ability of the uterus to contract. Similarly, longer duration of labor, especially with ruptured amniotic membranes, results in more opportunity for infection to occur. 37 , 38 Outcomes were defined using ICD‐9 codes (specific codes appear in the Appendix S1).
2.2.3. Covariates
We used data from the claims and enrollment files to define the following covariates: maternal age (20 and below, 21‐25, 26‐30, 31‐35, and 36 y and above), dual enrollment in both Medicaid and Medicare, and common clinical covariates. Clinical covariates were created based on ICD‐9 codes and included prior cesarean (654.20, 654.21, or 654.23), preterm delivery (644.2x), diabetes (648.0x, 648.8x, or 250.xx), hypertension in pregnancy (642.xx), placental complications (641.0x, 641.1x, 667), and fetal disproportion/obstruction of labor (653.xx, 660.xx). We excluded records with fetal malpresentation (652.xx) or multi‐fetal gestation (651, 651.0X, 651.1X, 651.2X, 651.3X, 651.4X, 651.5X, 651.6X, 651.8X, 651.9X), as they are commonly considered indications for cesarean birth and obstetric practice differs greatly for these categories of births..
2.3. Analysis
2.3.1. Unadjusted analysis approach
To enable comparison of policy effects among black and white women, we conducted analyses stratified by maternal race. Using chi‐square tests, we conducted descriptive analyses describing how outcomes for black Medicaid beneficiaries and white Medicaid beneficiaries differed between the control and policy states. We plotted quarterly rates of the primary study outcome (cesarean birth) and one secondary outcome (maternal morbidity composite) throughout the study period. We plotted outcomes among black beneficiaries in the policy state and control states, then among white beneficiaries in the policy state and control states, enabling visual comparison of policy effects among people of each race who gave birth during the study period.
2.3.2. Regression modeling approach
We employed a quasi‐experimental approach to assess for effects on black and white beneficiaries in the policy state (Minnesota) as compared to black and white beneficiaries in control states with no equivalent payment policy change. Building on the analytical framework of an earlier study of the effects of this policy on the overall population, 19 we conducted an interrupted time series (ITS) analysis with a control group, separately for each racial group. We opted to fit race‐stratified models because of the complexity of the race‐specific models, and the challenges of interpreting 3‐way interaction terms. To enable statistical comparison of the postpolicy slopes between black and white people, we fit a race‐pooled model (black and white) with a 3‐way interaction term between black race, policy state, and our effect of interest (the postpolicy quarterly time‐trend). The comparative interrupted time series approach combines the strengths of several quasi‐experimental approach (ie, ITS and difference‐in‐differences), by controlling for secular time trends before and after policy implementation, and comparing the policy group to a control group that is not exposed to a similar policy. 39 Although the policy was implemented at a single time (October 1, 2009), prior research on this policy and others has demonstrated gradual changes in childbirth care after implementation of policy changes, 10 , 19 , 30 , 31 so we targeted the postpolicy quarterly time‐trend as our effect of interest, rather than the postpolicy level difference.
Specifically, we conducted comparative ITS analysis comparing outcomes in the postpolicy period among black women (ie, black women in Minnesota as compared to black women in control states), then repeated this analysis among white women (comparing outcomes among white women in Minnesota to outcomes in white women in control states). Our modeling approach included main terms for policy state, temporal trends (quarterly), postpolicy temporal trends (quarterly), and the postpolicy period, as well as several interaction terms (policy state*time, policy state*postpolicy period, policy state*time after policy). We also controlled for the key covariates (described above). This approach described how outcomes changed among women of each race in the policy state as compared to the control states, controlling for temporal trends and covariates. To enable interpretation of results, we present results as quarterly postpolicy trends and the cumulative 3‐year policy “effect.” We opted to use quarters as the time interval of interest in order to create sufficient temporal granularity, while also preserving adequate sample size and event numbers in each interval (particularly for rarer outcomes, for example postpartum hemorrhage and chorioamnionitis). We conducted sensitivity analyses of our comparative ITS model; specifically, we considered alternative control states as the “policy state.” We repeated analysis on a restricted dataset (Minnesota births excluded), first treating Oregon as the policy state, and then Wisconsin.
This analysis was reviewed and approved by the Institutional Review Board at the University of Minnesota.
3. RESULTS
3.1. Study sample characteristics
The final analytic sample included 426 998 births during the study period, 16 336 in the policy state, and 410 662 in the control states. Among the 133 538 black women in our sample, 4600 gave birth in the policy state and 128 938 gave birth in the control states (Table 1). Among births to white people, 11 736 occurred in the policy state and 281 724 occurred in the controls states. The distribution of age and other covariates was largely similar between policy states and control states, except that there were a higher share of dually enrolled women in Minnesota (5.8 percent) as compared to control states (0.9 percent, P < .001). Black women in Minnesota were less likely to be in the youngest age groups as compared to black women in control states (eg, 24.5 percent 20 years old or younger in Minnesota compared to 33.1 percent in control states) and had a lower prevalence of hypertension (7.8 percent versus 9.3 percent in control states). There were few substantial differences between white women in the policy state and in the control states.
TABLE 1.
Demographic and health‐related characteristics of births in the policy state and control states, overall and by race (%)
| Combined Black and White women | Black women | White women | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Policy State (N = 16 336) | Control States (N = 410 662) | P‐value | Policy State (N = 4600) | Control States (N = 128 938) | P‐value | Policy State (N = 11 736) | Control States (N = 281 724) | P‐value | |
| Age group | |||||||||
| ≤20 | 22.8 | 27.4 | <.001 | 24.5 | 33.1 | <.001 | 22.1 | 24.7 | <.001 |
| 21‐25 | 34.8 | 37.4 | 30.8 | 34.6 | 36.4 | 38.6 | |||
| 26‐30 | 24.7 | 21.8 | 24.4 | 19.6 | 24.8 | 22.8 | |||
| 31‐35 | 12.0 | 9.4 | 13.0 | 8.9 | 11.6 | 9.6 | |||
| ≥36 | 5.8 | 4.1 | 7.4 | 3.9 | 5.2 | 4.2 | |||
| Race/ethnicity | |||||||||
| Non‐Hispanic white | 71.8 | 68.6 | <.001 | ||||||
| Non‐Hispanic black | 28.2 | 31.4 | |||||||
| Dual enrollee, Medicare/Medicaid | 5.8 | 0.9 | <.001 | 5.7 | 0.8 | <.001 | 5.8 | 0.9 | <.001 |
| Clinical conditions | |||||||||
| Prior cesarean | 12.7 | 13.5 | .006 | 15.5 | 13.6 | <.001 | 11.7 | 13.5 | <.001 |
| Preterm birth | 8.2 | 6.8 | <.001 | 8.9 | 8.2 | .08 | 7.9 | 6.2 | <.001 |
| Diabetes | 0.8 | 0.7 | .750 | 1.0 | 0.8 | .221 | 0.7 | 0.7 | .708 |
| Hypertension | 6.5 | 7.8 | <.001 | 7.8 | 9.3 | <.001 | 6.0 | 7.1 | <.001 |
| Placental complications | 0.9 | 0.9 | .83 | 0.9 | 0.9 | .87 | 0.9 | 0.9 | .87 |
| Obstruction of labor | 5.2 | 4.6 | <.001 | 4.5 | 3.5 | <.001 | 5.5 | 5.1 | .05 |
3.2. Unadjusted analysis
Black Medicaid beneficiaries had higher rates of cesarean birth in both the policy state (22.2 percent prepolicy) and control states (26.1 percent prepolicy period), compared to white beneficiaries in the policy state (19.3 percent prepolicy) and the control states (23.2 percent prepolicy period, Table 2). Maternal morbidity was notably higher in the policy state among both black women (24.9 percent, prepolicy) and white women (19.7 percent, prepolicy), as compared to the control states (15.8 percent for black women and 15.2 percent among white women, prepolicy period).
TABLE 2.
Prevalence of study outcomes in Minnesota and six control states during the prepolicy period and postpolicy period, by maternal race (%)
| Non‐Hispanic black women | Non‐Hispanic white women | |||||
|---|---|---|---|---|---|---|
| Prepolicy period | Postpolicy period | P‐value | Prepolicy period | Postpolicy period | P‐value | |
| Cesarean delivery | ||||||
| Policy state | 22.2 | 22.4 | .79 | 19.3 | 18.3 | .39 |
| Control states | 26.1 | 27.7 | <.001 | 23.2 | 24.6 | <.001 |
| Maternal morbidity composite | ||||||
| Policy state | 24.9 | 24.9 | .80 | 19.7 | 19.1 | .34 |
| Control states | 15.8 | 17.0 | <.001 | 15.2 | 15.5 | .01 |
| Postpartum hemorrhage/blood transfusion | ||||||
| Policy state | 4.8 | 5.4 | .28 | 3.5 | 3.6 | .87 |
| Control states | 2.3 | 2.8 | <.001 | 2.6 | 2.6 | .81 |
| Chorioamnionitis | ||||||
| Policy state | 2.5 | 3.6 | .05 | 1.4 | 1.6 | .39 |
| Control states | 2.2 | 2.3 | .27 | 1.2 | 1.2 | .32 |
Unadjusted temporal trends in cesarean birth among black women suggested a substantial decline during the postpolicy period in Minnesota (from approximately 26 to 20 percent) after a notable increase in the prepolicy period (from approximately 17 to 26 percent, Figure 1A). There was no similar trend among black women in control states, who exhibited a steady, relatively constant rate of cesarean birth during both the prepolicy and postpolicy periods (from approximately 25 to 29 percent by the end of the study period). Among white women in the policy state, there was a suggestion of a smaller decline in the cesarean rate postpolicy (in the range of 1 to 2 percentage points, from approximately 19 percent to 17 percent), although the trend in cesarean rate in white women in all states (Figure 1B) was less variable as compared to black women in Minnesota. Temporal trends in maternal morbidity appeared to be largely unchanged during the study period in both the policy state and control states. This relatively constant maternal morbidity rate was observed among both black women (Figure 2A) and white women (Figure 2B).
FIGURE 1.
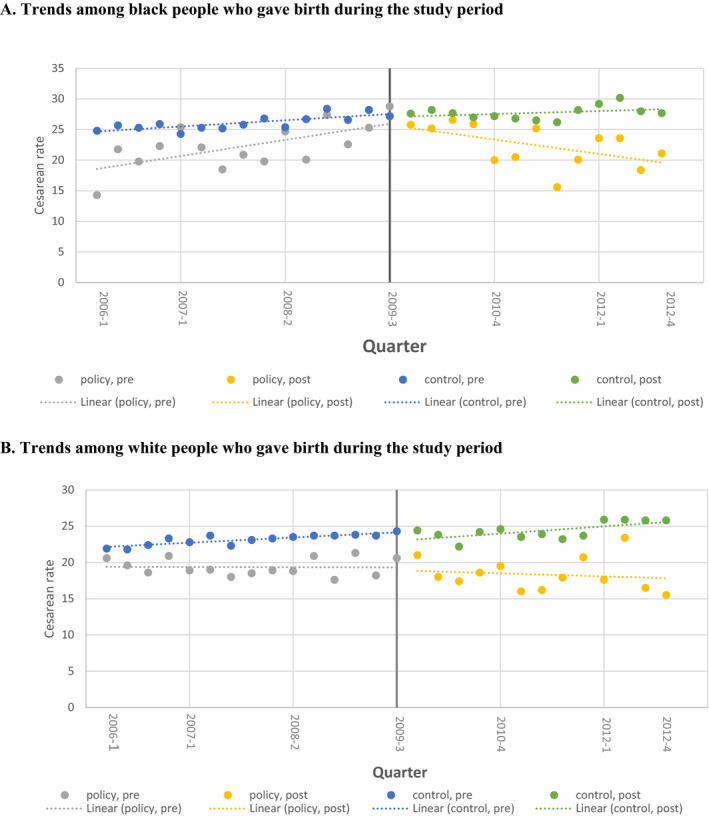
Quarterly trends in cesarean birth among Black (A) and White (B) Medicaid fee‐for‐service beneficiaries in Minnesota (Policy State) and six control states, 2006‐2012† [Color figure can be viewed at wileyonlinelibrary.com]
Note: A, Trends among BLACK people who gave birth during the study period. B, Trends among White people who gave birth during the study period.
†Heavy vertical bar indicates policy implementation (October 1, 2009)
FIGURE 2.
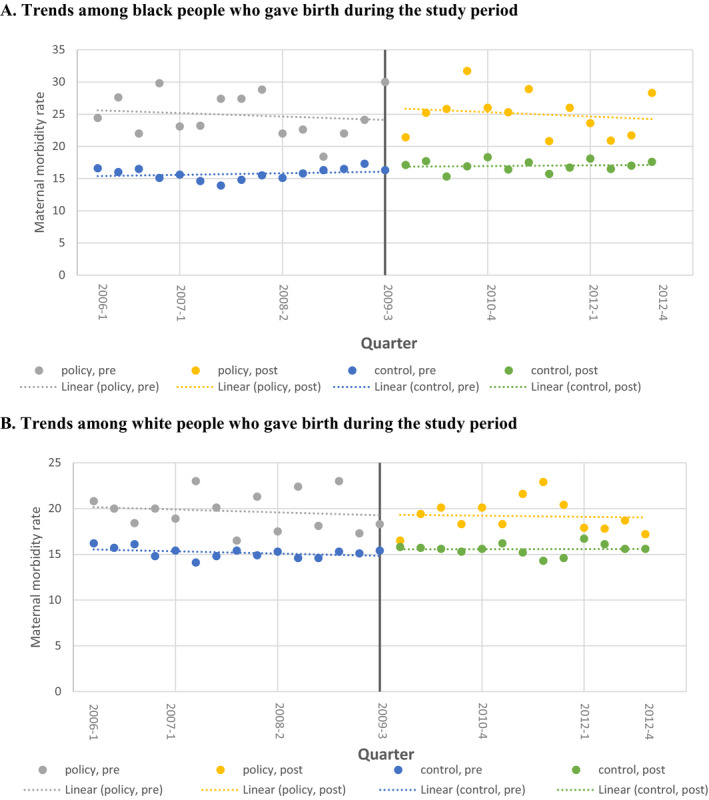
Quarterly trends in composite maternal morbidity among black (A) and white (B) Medicaid fee‐for‐service beneficiaries in Minnesota (Policy State) and six control states, 2006‐2012† [Color figure can be viewed at wileyonlinelibrary.com]
note: A, Trends among Black people who gave birth during the study period. B, Trends among White people who gave birth during the study period.
†Heavy vertical bar indicates policy implementation (October 1, 2009)
3.3. Comparative interrupted time series results
The comparative ITS approach we used to estimate adjusted policy effects quantified both a “level change” that expresses the one‐time magnitude of change associated with policy implementation (ie, in 2009), and also quarterly postpolicy trends in both policy states and the control state (Table 3). Only one level change result achieved statistical significance at the P < .05 level (a 0.58 percent immediate postpolicy increase in cesarean use among white women in Minnesota, compared to a −0.55 percent decrease among white women in control states, P = .04). The quarterly trend quantifies policy‐associated trends in outcomes over time in the policy state and corresponding trend changes occurring the control states and is our focus. We present both quarterly policy‐related changes and also the cumulative 3‐year policy‐related changes in outcomes for both black and white Medicaid beneficiaries. These regression results were consistent with trends observed in unadjusted analyses: There was a notable postpolicy decrease in cesarean birth among black beneficiaries in Minnesota (−0.24 percent quarterly decrease; 3‐year cumulative decrease of −2.88 percent, from a prepolicy cesarean rate of 22.2 percent), but an increase in cesarean rates among black women in control states during this same time period (0.16 percent quarterly change; 1.92 percent 3‐year cumulative increase; P < .001 comparing policy state to control states). Cesarean birth did decrease among white Medicaid beneficiaries in Minnesota (−1.32 percent 3‐year cumulative decrease from a prepolicy cesarean rate of 19.3 percent) compared with an increase in cesarean rates among white beneficiaries in control states (1.56 percent 3‐year cumulative change P = .003). As hypothesized, the policy‐associated decrease in cesarean rates among black women in Minnesota (ie, −2.88 percent cumulative change) was greater than the postpolicy cumulative decrease in cesarean use among white women in Minnesota (−1.32 percent, 3‐way interaction term P‐value = .0013).
TABLE 3.
Comparative interrupted time series analysis results describing quarterly trends and 3‐year cumulative effect in study outcomes during the postpolicy period (October 2009–December 2012)
| Baseline mean | Level change after policy a | P‐value for policy effect on level (policy vs. control states) | Quarterly trend change after policy a | P‐value for policy effect on trend (policy vs. control states) | Cumulative effect 3y after policy (quarterly trend * 12) | |
|---|---|---|---|---|---|---|
| Cesarean | ||||||
| Black women | ||||||
| Policy state | 22.2% | 0.56% | .28 | −0.24% | <.001 | −2.88% |
| Control states | 26.1% | −0.55% | 0.16% | 1.92% | ||
| White women | ||||||
| Policy state | 19.3% | 0.58% | .04 | −0.11% | .003 | −1.32% |
| Control states | 23.2% | −0.55% | 0.13% | 1.56% | ||
| Maternal morbidity composite | ||||||
| Black women | ||||||
| Policy state | 24.9% | −0.48% | .35 | 0.10% | .13 | 1.20% |
| Control states | 15.8% | −0.36% | 0.16% | 1.92% | ||
| White women | ||||||
| Policy state | 19.7% | −0.39% | .23 | 0.00% | .99 | 0.00% |
| Control states | 15.2% | −0.43% | 0.17% | 2.04% | ||
| Postpartum hemorrhage/blood transfusion | ||||||
| Black women | ||||||
| Policy state | 4.8% | −0.43% | .05 | 0.10% | <.001 | 1.20% |
| Control states | 2.3% | 0.03% | 0.02% | 0.24% | ||
| White women | ||||||
| Policy state | 3.6% | −0.16% | .25 | 0.04% | .04 | 0.48% |
| Control states | 2.6% | −0.05% | 0.03% | 0.36% | ||
| Chorioamnionitis | ||||||
| Black women | ||||||
| Policy state | 2.5% | 0.35% | .08 | −0.02% | .53 | −0.24% |
| Control states | 2.2% | −0.05% | 0.03% | 0.36% | ||
| White women | ||||||
| Policy state | 1.4% | −0.14% | .12 | −0.02% | .17 | −0.24% |
| Control states | 1.2% | −0.02% | 0.02% | 0.24% | ||
Models are adjusted for maternal age, dual enrollment, prior cesarean, preterm delivery, diabetes, hypertension in pregnancy, placental complications, fetal disproportion/obstruction of labor.
There were no significant policy‐associated changes observed in maternal morbidity in any racial group, nor did changes differ between the policy state and control states (eg, cumulative 1.20 percent change in black women in Minnesota and 1.92 percent change in black women in control states, P = .13; Table 3). Trends in chorioamnionitis were also small (ie, all < 0.5 percent cumulative 3‐year change) and did not differ between policy state and control states. In contrast, the rate of postpartum hemorrhage increased in black women in Minnesota in the postpolicy period (cumulative 3‐year change of 1.20 percent) as compared to black women in control states (0.24 percent, P < .001). A similar, smaller increase in postpartum hemorrhage was observed among white women in Minnesota postpolicy (0.48 percent) as compared to their white counterparts in control states during this time period (0.36 percent, P = .04 comparing white women in Minnesota to white women in control states; P < .001 for the 3‐way interaction term comparing the postpolicy trend in black women versus white women).
Sensitivity analyses of comparative ITS models treating Oregon and Wisconsin as the “policy state” revealed a small number of results that were statistically significant (P < .05). When Oregon was treated as the policy state, there appeared to be a “level change” at the mock postpolicy period (ie, beginning in October 2009), such that white women in Oregon experienced a slight increase in cesarean birth (0.78 percent), as compared to a decrease among women in “control states” (−0.59 percent, P = .006). White women in Wisconsin appeared to experience a significantly decreased trend in cesarean birth (cumulative 3‐year decrease, −2.28 percent) as compared to an increase for women in “control states” (cumulative 3‐year increase, 1.68 percent, P < .001).
4. DISCUSSION
A prior study established that Minnesota's blended payment policy for uncomplicated childbirth was associated with a significant decrease in cesarean use, and results from the current study suggest that policy effects were greater among black women. 19 We found that the policy‐related decline among black women (2.88 percent) was more than 2‐fold higher than the decline among white women (1.32 percent). This has important implications for understanding cesarean use, racial disparities in cesarean use, and how policy enactment and implementation may have important differential effects by race.
The current findings of differential effects of maternal health policy by race are consistent with results from an earlier study on racial disparities in elective early deliveries after Oregon's hard‐stop policy limiting these procedures. 10 That study showed that the rate of elective early cesarean decreased more among black women than among white women after policy implementation, leading to a narrowing of the black/white racial disparity. 10 This contrasts with a study of temporal trends in procedure use in New York City births, which found that both elective early delivery and low‐risk cesarean decreased among white women between 2008 and 2014, and not among Hispanic or African American women. 40 That study did not focus on changes in obstetric practice related to a specific policy, but it nonetheless highlights that results can be complex, conflicting, and dependent on local context.
It is logical that cesarean rates among black people would be more sensitive to policy effects, given the higher cesarean rate among this population (and the higher share of cesareans without a medical indication). 8 , 9 , 10 , 11 In particular, cesarean use increased substantially among black people in Minnesota before the blended payment policy; this prior trend influenced the degree of postpolicy decline in this population. Collectively, results from the current and prior studies suggest that policies aimed at decreasing unnecessary cesarean use overall may have the added benefit of reducing racial disparities. To support broad national efforts to address racial inequities in childbirth, maternity care experts recommend planning for and evaluation of quality improvement initiatives or policies with specific attention to maternal race. 12
4.1. Racial equity and racism as a determinant of maternal health
More research is needed on how racial inequities arise in the first place. Specifically, racism is a driving contributor to racial inequities in health in the US, including and especially maternal and perinatal health. 12 , 27 , 32 , 41 , 42 Racism may affect care and birth outcomes at many levels, including interactions between individuals (interpersonal racism) 43 , 44 and the allocation of opportunities and resource based on race via systems and policies (structural racism). 27 , 45 , 46 , 47 Prior work documents how racism affects clinical care in anesthesia and emergency medicine; more work is needed that explicitly names racism in childbirth care, rigorously measures it, and quantifies its effects on outcomes. 27 , 48 , 49 , 50 Disparities between black and white women in maternal health outcomes are longstanding and complex, and evidence is beginning to emerge to inform efforts to improve black maternal health. 51 , 52 , 53 , 54 Additionally, other racial inequities in maternal health, notably the elevated rate of maternal mortality among American Indian/Alaska Native people, require further attention in research and policy. 51 , 55
4.2. Unintended policy effects
Fully understanding the effects of policies requires attention to potential unintended policy effects. 56 , 57 Although this analysis produced reassuring results indicating that maternal morbidity and chorioamnionitis did not change after policy implementation, it is concerning that the rate of postpartum hemorrhage increased among black and white Medicaid beneficiaries in Minnesota following policy implementation. Several possibilities could explain these findings. Postpartum hemorrhage is a leading preventable cause of maternal death in the US, and initiatives to prevent and manage postpartum hemorrhage have resulted in increased reporting of postpartum hemorrhage. 58 , 59 , 60 Our data sources and analytic approach do not permit us to account for reporting trends related to secondary outcomes. Postpartum hemorrhage has a complex and heterogeneous etiology. The most common etiology is uterine atony, which is associated with labor, whether the result is vaginal or cesarean birth, 61 and longer duration of labor. 62 , 63 Decreased cesarean use requires greater tolerance of increased labor duration and also more complicated labors, on a population level, and could be resulting in increases in postpartum hemorrhage observed here. The increase in postpartum hemorrhage was also greater among black women (3‐way interaction term P‐value < .001), which may follow our trend observed trend in cesarean use or could reflect previously described disparities between black and white women in adverse obstetric outcomes and associated severe morbidities including postpartum hemorrhage. 64 , 65 This finding highlights that decision making related to labor management and childbirth care is complex and requires weighing risks and benefits. 7 Safe cesarean reduction necessitates engaging with this complexity and considering a variety of outcomes, intended and unintended. 1
4.3. Strengths and limitations
The strengths of this analysis include a strong quasi‐experimental approach using a control group and studying a unique policy intervention. In particular, using a comparative ITS analysis with a group of control states and assessing for postpolicy level changes as well as more gradual postpolicy temporal trends enabled us to detect results that might not have been evident using standard methods. This study also has some limitations that require consideration. Regarding unintended policy effects, intrapartum cesarean use is often indicated due to concerns about infant health, and these data only allowed for analysis of maternal complications. The inability to link maternal birth records with neonatal birth records prevented us from analyzing important neonatal outcomes such as birth asphyxia, birth trauma, and neonatal seizures. We also analyzed only records from a single birth. The focus on immediate postpartum complications (eg, postpartum hemorrhage) may actually under‐estimate the benefits of reduced cesarean use, given that longer‐term complications of cesarean delivery (eg, placenta accreta and other morbid placentation in future pregnancies) are not considered using individual births as the unit of analysis. 66
The geographic scope of our study limits generalizability of these findings to other states, regions, and health systems. These results must be interpreted in the specific context of Minnesota's childbearing population, particularly black women, who experienced a notable increase in cesarean use in the period before policy implementation. The extent of racial disparity in many health outcomes (eg, cardiovascular disease) exhibits marked regional variability, with frequently higher disparities in the US Southeast. 67 The Minnesota population differed from that of other states in other ways (eg, higher frequency of dual Medicare/Medicaid enrollees, suggesting more people with disabilities among the childbearing population); we controlled for such variables that were available in our data source. Baseline morbidity rates in Minnesota were higher than in control states; this may owe to efforts to improve the accuracy of birth data collection in Minnesota, or to higher rates of disability among pregnant Medicaid beneficiaries. 19 One must also consider the role of chance in explaining our findings; our sensitivity analyses of 2 control states as a hypothetical “policy state” revealed 2 significant differences. Notably, these changes both related to differences in cesarean birth among white women. This finding is expected, given that trends in cesarean use were changing dynamically during the study period. 68
These results also apply most directly to people who are enrolled in Medicaid fee‐for‐service coverage; results of similar policies may differ when implemented by different payers and in different populations. Further, we were limited by the data elements available on Medicaid claims which does not include potentially important covariates such as maternal education, maternal nativity, and maternal BMI. We chose to focus on the black/white racial disparity in cesarean use and maternal morbidity, but policies may affect outcomes and disparities for other racial/ethnic groups (eg, among Asian Americans, Latinx people, American Indians/Alaska Natives, and multiracial people).
5. CONCLUSION
One Medicaid program's blended payment policy for uncomplicated childbirth resulted in decreases in cesarean use that differed by maternal race. Specifically, the overall decrease in cesarean use that followed this policy was larger among black women, who experienced a decrease in cesarean rate than was more than twice as large as the decrease observed among white Medicaid beneficiaries. This study suggests that policies limiting cesarean use may have the added benefit of narrowing racial disparities in these outcomes. Future research will need to continue assessing the effects of maternal policies on disparities—even when those policies target the entire population. There is also a need to understand underlying racial inequities in maternal health, including identifying explanatory factors for the greater use of nonmedically indicated cesarean birth among black people. Finally, attention to unintended consequences, including distinguishing these effects by race, is needed. This study's finding that postpartum hemorrhage increased in Minnesota after policy implementation highlights the need to weigh complications of labor and birth against the goal of cesarean reduction and to examine the racial equity implications of both policy effects and unintended consequences.
Policy implementation and evaluation are complex, and rigorous consideration of how policies effect health equity and other (nontargeted) outcomes is perhaps especially complex. Nonetheless, such research is essential to ensure that health policies do not result in unintended complications, worsening health equity, or both.
CONFLICT OF INTEREST
None.
Supporting information
Appendix S1
Author Matrix
ACKNOWLEDGMENT
Joint Acknowledgment/Disclosure Statement: This research was completed with support from the Medicaid and CHIP Payment and Access Commission (MACPAC) under contract MACP17417T1, and from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant R00 HD079658‐03 to JMS). Data access for this analysis was supported by the Health Equity Research Data Access Program through the Office of Minority Health at the Centers for Medicare & Medicaid Services. The findings, statements, and views expressed are those of the authors and do not necessarily represent those of any funding agency.
Snowden JM, Osmundson SS, Kaufman M, Blauer Peterson C, Kozhimannil KB. Cesarean birth and maternal morbidity among Black women and White women after implementation of a blended payment policy. Health Serv Res. 2020;55:729–740. 10.1111/1475-6773.13319
REFERENCES
- 1. Caughey AB, Cahill AG, Guise JM, Rouse DJ. Obstetric care consensus no. 1: safe prevention of the primary cesarean delivery. Obstet Gynecol. 2014;123(3):693‐711. [DOI] [PubMed] [Google Scholar]
- 2. King TL. Reducing the cesarean rate: our time is now. J Midwifery Womens Health. 2014;59(3):231‐232. [DOI] [PubMed] [Google Scholar]
- 3. Geller EJ, Wu JM, Jannelli ML, Nguyen TV, Visco AG. Neonatal outcomes associated with planned vaginal versus planned primary cesarean delivery. J Perinatol. 2010;30(4):258‐264. [DOI] [PubMed] [Google Scholar]
- 4. Gerten KA, Coonrod DV, Bay RC, Chambliss LR. Cesarean delivery and respiratory distress syndrome: does labor make a difference? Am J Obstet Gynecol. 2005;193(3 Pt 2):1061‐1064. [DOI] [PubMed] [Google Scholar]
- 5. Blondon M, Casini A, Hoppe KK, Boehlen F, Righini M, Smith NL. Risks of venous thromboembolism after cesarean sections: a meta‐analysis. Chest. 2016;150(3):572‐596. [DOI] [PubMed] [Google Scholar]
- 6. Curtin SC, Gregory KD, Korst LM, Uddin SF. Maternal morbidity for vaginal and cesarean deliveries, according to previous cesarean history: new data from the birth certificate, 2013. Natl Vital Stat Rep. 2015;64(4):1‐13. [PubMed] [Google Scholar]
- 7. Gregory KD, Jackson S, Korst L, Fridman M. Cesarean versus vaginal delivery: whose risks? Whose benefits? Am J Perinatol. 2012;29(1):7‐18. [DOI] [PubMed] [Google Scholar]
- 8. Bryant AS, Worjoloh A, Caughey AB, Washington AE. Racial/ethnic disparities in obstetric outcomes and care: prevalence and determinants. Am J Obstet Gynecol. 2010;202(4):335‐343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Getahun D, Strickland D, Lawrence JM, Fassett MJ, Koebnick C, Jacobsen SJ. Racial and ethnic disparities in the trends in primary cesarean delivery based on indications. Am J Obstet Gynecol. 2009;201(4):422. e421‐427. [DOI] [PubMed] [Google Scholar]
- 10. Kozhimannil KB, Muoto I, Darney BG, Caughey AB, Snowden JM. Early elective delivery disparities between non‐Hispanic Black and White women after state wide policy implementation. Womens Health Issues. 2018;28(3):224‐231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Huesch M, Doctor JN. Factors associated with increased cesarean risk among African American women: evidence from California, 2010. Am J Public Health. 2015;105(5):956‐962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Howell EA, Brown H, Brumley J, et al. Reduction of peripartum racial and ethnic disparities: a conceptual framework and maternal safety consensus bundle. Obstet Gynecol. 2018;131(5):770‐782. [DOI] [PubMed] [Google Scholar]
- 13. Mann S, Hollier LM, McKay K, Brown H. What we can do about maternal mortality – and how to do it quickly. N Engl J Med. 2018;379(18):1689‐1691. [DOI] [PubMed] [Google Scholar]
- 14. Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2017. Natl Vital Stat Rep. 2018;67(8):1‐50. [PubMed] [Google Scholar]
- 15. Oshiro BT, Henry E, Wilson J, Branch DW, Varner MW. Decreasing elective deliveries before 39 weeks of gestation in an integrated health care system. Obstet Gynecol. 2009;113(4):804‐811. [DOI] [PubMed] [Google Scholar]
- 16. Snowden JM, Muoto I, Darney BG, et al. Oregon's hard‐stop policy limiting elective early‐term deliveries: association with obstetric procedure use and health outcomes. Obstet Gynecol. 2016;128(6):1389‐1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hutcheon JA, Strumpf EC, Harper S, Giesbrecht E. Maternal and neonatal outcomes after implementation of a hospital policy to limit low‐risk planned caesarean deliveries before 39 weeks of gestation: an interrupted time‐series analysis. BJOG. 2015;122(9):1200‐1206. [DOI] [PubMed] [Google Scholar]
- 18. Donovan EF, Lannon C, Bailit J, Rose B, Iams JD, Byczkowski T. A statewide initiative to reduce inappropriate scheduled births at 36(0/7)‐38(6/7) weeks' gestation. Am J Obstet Gynecol. 2010;202(3):243 e241‐248. [DOI] [PubMed] [Google Scholar]
- 19. Kozhimannil KB, Graves AJ, Ecklund AM, Shah N, Aggarwal R, Snowden JM. Cesarean delivery rates and costs of childbirth in a state Medicaid program after implementation of a blended payment policy. Med Care. 2018;56(8):658‐664. [DOI] [PubMed] [Google Scholar]
- 20. Johnson EM, Rehavi MM. Physicians treating physicians: information and incentives in childbirth. Am Econ J Econ Policy. 2016;8(1):115‐141. [Google Scholar]
- 21. Minnesota Session Laws . An act relating to state government; making technical health and human services changes; making health care program policy changes; changing health care eligibility provisions; authorizing rule making; requiring reports; changing appropriations; appropriating money. In. Chapter 1732009.
- 22. Frohlich KL, Potvin L. Transcending the known in public health practice: the inequality paradox: the population approach and vulnerable populations. Am J Public Health. 2008;98(2):216‐221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sarkar U, Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc. 2011;18(3):318‐321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Snowden JM, Chen YH, McFarland W, Raymond HF. Prevalence and characteristics of users of pre‐exposure prophylaxis (PrEP) among men who have sex with men, San Francisco, 2014 in a cross‐sectional survey: implications for disparities. Sex Transm Infect. 2017;93(1):52‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chen J, Vargas‐Bustamante A, Mortensen K, Ortega AN. Racial and ethnic disparities in health care access and utilization under the affordable care act. Med Care. 2016;54(2):140‐146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Rep. 2003;118(4):358‐365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hardeman RR, Murphy KA, Karbeah J, Kozhimannil KB. Naming institutionalized racism in the public health literature: a systematic literature review. Public Health Rep. 2018;133(3):240‐249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Thomas S, Fayter D, Misso K, et al. Population tobacco control interventions and their effects on social inequalities in smoking: systematic review. Tob Control. 2008;17(4):230‐237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sehgal AR. Impact of quality improvement efforts on race and sex disparities in hemodialysis. JAMA. 2003;289(8):996‐1000. [DOI] [PubMed] [Google Scholar]
- 30. Kozhimannil KB, Karaca‐Mandic P, Blauer‐Peterson CJ, Shah NT, Snowden JM. Uptake and utilization of practice guidelines in hospitals in the United States: the case of routine episiotomy. Jt Comm J Qual Patient Saf. 2017;43(1):41‐48. [DOI] [PubMed] [Google Scholar]
- 31. Muoto I, Darney BG, Lau B, et al. Shifting patterns in cesarean delivery scheduling and timing in Oregon before and after a statewide hard stop policy. Health Serv Res. 2018;53:2839‐2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Eichelberger KY, Doll K, Ekpo GE, Zerden ML. Black lives matter: claiming a space for evidence‐based outrage in obstetrics and gynecology. Am J Public Health. 2016;106(10):1771‐1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kuklina EV, Whiteman MK, Hillis SD, et al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J. 2008;12(4):469‐477. [DOI] [PubMed] [Google Scholar]
- 34. Tangel V, White RS, Nachamie AS, Pick JS. Racial and ethnic disparities in maternal outcomes and the disadvantage of peripartum Black women: a multistate analysis, 2007‐2014. Am J Perinatol. 2019;36(8):835‐848. [DOI] [PubMed] [Google Scholar]
- 35. Ford CL, Airhihenbuwa CO. The public health critical race methodology: praxis for antiracism research. Soc Sci Med. 2010;71(8):1390‐1398. [DOI] [PubMed] [Google Scholar]
- 36. Korst LM, Fridman M, Lu MC, et al. Monitoring childbirth morbidity using hospital discharge data: further development and application of a composite measure. Am J Obstet Gynecol. 2014;211(3):268 e261‐268 e216. [DOI] [PubMed] [Google Scholar]
- 37. Looft E, Simic M, Ahlberg M, Snowden JM, Cheng YW, Stephansson O. Duration of second stage of labour at term and pushing time: risk factors for postpartum haemorrhage. Paediatr Perinat Epidemiol. 2017;31(2):126‐133. [DOI] [PubMed] [Google Scholar]
- 38. Tita AT, Andrews WW. Diagnosis and management of clinical chorioamnionitis. Clin Perinatol. 2010;37(2):339‐354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. St. Clair T, Cook TD, Hallberg K. Examining the internal validity and statistical precision of the comparative interrupted time series design by comparison with a randomized experiment. Am J Eval. 2014;35(3):311‐327. [Google Scholar]
- 40. Janevic T, Egorova NN, Zeitlin J, Balbierz A, Hebert PL, Howell EA. Examining trends in obstetric quality measures for monitoring health care disparities. Med Care. 2018;56(6):470‐476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. McLemore MR, Altman MR, Cooper N, Williams S, Rand L, Franck L. Health care experiences of pregnant, birthing and postnatal women of color at risk for preterm birth. Soc Sci Med. 2018;201:127‐135. [DOI] [PubMed] [Google Scholar]
- 42. Roberts D. Killing the Black Body: Race, Reproduction, and the Meaning of Liberty. New York, NY: Pantheon; 1998. [Google Scholar]
- 43. Slaughter‐Acey JC, Caldwell CH, Misra DP. The influence of personal and group racism on entry into prenatal care among African American women. Womens Health Issues. 2013;23(6):e381‐e387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Slaughter‐Acey JC, Sealy‐Jefferson S, Helmkamp L, et al. Racism in the form of micro aggressions and the risk of preterm birth among black women. Ann Epidemiol. 2016;26(1):7‐13 e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404‐416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mendez DD, Hogan VK, Culhane JF. Institutional racism, neighborhood factors, stress, and preterm birth. Ethn Health. 2014;19(5):479‐499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Feagin J, Bennefield Z. Systemic racism and U.S. health care. Soc Sci Med. 2014;103:7‐14. [DOI] [PubMed] [Google Scholar]
- 48. Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453‐1463. [DOI] [PubMed] [Google Scholar]
- 49. Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci USA. 2016;113(16):4296‐4301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Dehon E, Weiss N, Jones J, Faulconer W, Hinton E, Sterling S. A systematic review of the impact of physician implicit racial bias on clinical decision making. Acad Emerg Med. 2017;24(8):895‐904. [DOI] [PubMed] [Google Scholar]
- 51. Petersen EE, Davis NL, Goodman D, et al. Vital signs: pregnancy‐related deaths, United States, 2011‐2015, and strategies for prevention, 13 states, 2013‐2017. MMWR Morb Mortal Wkly Rep. 2019;68(18):423‐429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Admon LK, Winkelman TNA, Zivin K, Terplan M, Mhyre JM, Dalton VK. Racial and ethnic disparities in the incidence of severe maternal morbidity in the United States, 2012‐2015. Obstet Gynecol. 2018;132(5):1158‐1166. [DOI] [PubMed] [Google Scholar]
- 53. Vedam S, Stoll K, Taiwo TK, et al. The Giving Voice to Mothers study: inequity and mistreatment during pregnancy and childbirth in the United States. Reprod Health. 2019;16(1):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Muse S, BMMA (Black Mamas Matter Alliance) . Setting the standard for holistic care of and for Black women In: Black Paper. 2018. [Google Scholar]
- 55. Warne D, Frizzell LB. American Indian health policy: historical trends and contemporary issues. Am J Public Health. 2014;104(Suppl 3):S263‐S267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Clancy CM, Glied SA, Lurie N. From research to health policy impact. Health Serv Res. 2012;47(1 Pt 2):337‐343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. IOM (Institute of Medicine) . Unintended Consequences of Health Policy Programs and Policies: Workshop Summary. Washington, DC: The National Academies Press; 2001. [PubMed] [Google Scholar]
- 58. Einerson BD, Miller ES, Grobman WA. Does a postpartum hemorrhage patient safety program result in sustained changes in management and outcomes? Am J Obstet Gynecol. 2015;212(2):140‐144 e141. [DOI] [PubMed] [Google Scholar]
- 59. Skupski DW, Brady D, Lowenwirt IP, et al. Improvement in outcomes of major obstetric hemorrhage through systematic change. Obstet Gynecol. 2017;130(4):770‐777. [DOI] [PubMed] [Google Scholar]
- 60. Berg CJ, Harper MA, Atkinson SM, et al. Preventability of pregnancy‐related deaths: results of a state‐wide review. Obstet Gynecol. 2005;106(6):1228‐1234. [DOI] [PubMed] [Google Scholar]
- 61. Ford JB, Roberts CL, Simpson JM, Vaughan J, Cameron CA. Increased postpartum hemorrhage rates in Australia. Int J Gynaecol Obstet. 2007;98(3):237‐243. [DOI] [PubMed] [Google Scholar]
- 62. Bateman BT, Berman MF, Riley LE, Leffert LR. The epidemiology of postpartum hemorrhage in a large, nationwide sample of deliveries. Anest Analg. 2010;110(5):1368‐1373. [DOI] [PubMed] [Google Scholar]
- 63. ACOG (American College of Obstetricians & Gynecologists) . Practice bulletin no. 183: postpartum hemorrhage. Obstet Gynecol. 2017;130(4):e168‐e186. [DOI] [PubMed] [Google Scholar]
- 64. Grobman WA, Bailit JL, Rice MM, et al. Racial and ethnic disparities in maternal morbidity and obstetric care. Obstet Gynecol. 2015;125(6):1460‐1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Gyamfi‐Bannerman C, Srinivas SK, Wright JD, et al. Postpartum hemorrhage outcomes and race. Am J Obstet Gynecol. 2018;219(2):185 e181‐185 e110. [DOI] [PubMed] [Google Scholar]
- 66. Silver RM. Abnormal placentation: placenta previa, vasa previa, and placenta accreta. Obstet Gynecol. 2015;126(3):654‐668. [DOI] [PubMed] [Google Scholar]
- 67. Carnethon MR, Pu J, Howard G, et al. Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136(21):e393‐e423. [DOI] [PubMed] [Google Scholar]
- 68. Martin JA, Hamilton BE, Osterman MJK, Curtin SC, Mathews TJ. Births: final data for 2012 In: NVS Reports, Vol. 62 Hyattsville, MD: National Center for Health Statistics; 2013. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Author Matrix


