Abstract
Objective
To examine whether low‐income children's use of preventive dental services is linked to variation in state Medicaid policies that affect parents' access to dental care in Medicaid.
Data Sources
Medical Expenditure Panel Survey (2011‐2016), Area Health Resources File, and Medicaid adult dental coverage policies.
Study Design
We conducted a quasi‐experimental analysis using linked parent‐child dyads in low‐income families (≤125 percent of the Federal Poverty Level). We assessed whether expansions of Medicaid to low‐income adults under the Affordable Care Act were associated with increases in the use of preventive dental services among low‐income children when state Medicaid programs did vs did not cover these services for adults.
Principal Findings
Over the study period, 37.8 percent of low‐income children received at least one annual preventive dental visit. We found no change in children's receipt of preventive dental care associated with Medicaid expansions in states that covered (1.26 percentage points; 95% CI: −3.74 to 6.27) vs did not cover preventive dental services for adults (3.03 percentage points; 95% CI: −2.76 to 8.81). (differential change: −1.76 percentage points; 95% CI: −8.09, 4.56). However, our estimates are imprecise, with wide confidential intervals that are unable to rule out sizable effects in either direction.
Conclusion
We did not find an association between Medicaid expansions with concurrent coverage of preventive dental services for adults and children's use of these services. Factors other than parental access to dental benefits through Medicaid may be more salient determinants of preventive dental care use among low‐income children.
Keywords: dentistry, Medicaid, state health policies
What This Study Adds.
Previous studies found that Medicaid coverage for adults has “spillover effects” on low‐income children's receipt of care.
No research has examined the relationship between policies that affect parental access to dental services in Medicaid—specifically, Medicaid expansions and dental coverage for adults—and low‐income children's likelihood of receiving preventive dental care.
This study did not find changes in children's use of preventive dental services associated with Medicaid expansions in states that did vs did not cover adult dental benefits in Medicaid, suggesting that other factors other than Medicaid eligibility and dental coverage policies for adults may be more salient determinants of preventive dental care use among low‐income children.
1. INTRODUCTION
Medicaid expansions for children and the introduction of the Children's Health Insurance Program (CHIP) in the 1990s have reduced disparities in dental care use by race and income. 1 , 2 Despite improvements in oral health over the last two decades, dental caries remain the most common chronic disease of childhood, affecting an estimated 46 percent of US children ages 2‐19, with disproportionate prevalence in low‐income families and among racial and ethnic minorities. 3 Poor oral health can lead to problems eating, speaking, and learning 4 , 5 whose ramifications can persist into adulthood, 6 affecting long‐term health 7 , 8 and economic outcomes. 9
Preventive dental care has been shown to reduce the incidence of dental caries and associated health care costs, 10 , 11 but the use of preventive dental services among children varies widely. Children who are black, Hispanic, or in low‐income families are 40‐50 percent less likely to receive preventive dental care than children who are white or of higher socioeconomic status. 12 Although preventive dental services are covered for all children in Medicaid and CHIP, research has found substantial variation across states in the level of access to dental services, due in part to state‐level differences in Medicaid payment rates to providers and geographic variation in the supply of dentists. 13
In addition to these factors, one study identified a parent's receipt of dental care as a salient determinant of their child's dental care use. 14 Although this study's observational design limited the extent to which its authors could control for other determinants of parents' and children's dental care use, its findings are consistent with a larger literature that finds “spillover” effects of parental access to care on their children's receipt of care. For example, Medicaid expansions for low‐income parents have been shown to increase the likelihood that their children received an annual well‐child visit. 15 , 16 , 17 , 18 However, no research has examined the relationship between policies that affect parental access to dental services in Medicaid and children's likelihood of receiving preventive dental care.
Two sources of state policy variation can affect low‐income parents' access to preventive dental care in Medicaid. First, state Medicaid programs vary considerably in the level of dental benefits provided to adults, with some covering preventive dental care and others covering emergency services only. 19 This stands in contrast to children, for whom states have consistently provided preventive dental services in Medicaid and CHIP under the Early Periodic Screening Diagnosis and Treatment benefit (made mandatory in 2009). 20 Second, states differ in their implementation of the Affordable Care Act's (ACA) Medicaid expansion, which increased Medicaid eligibility for nondisabled and nonpregnant adults. Although the ACA did not explicitly change dental coverage policy for adults in Medicaid (it remains an optional benefit), many low‐income adults gained dental coverage in states that expanded Medicaid and covered preventive dental services for adults through their Medicaid programs. 21 Recent research has linked Medicaid expansions with concurrent dental coverage to increases in oral health care use and to reductions in dental‐related emergency department visits among adults. 22 , 23 , 24
In this study, we analyzed linked parent‐child dyads from nationally representative survey data to investigate whether state policies that affect adults' access to dental care in Medicaid have spillover effects on low‐income children's receipt of preventive dental care. We employed a quasi‐experimental design that compared changes in children's receipt of three preventive dental services (cleanings, fluoride treatment, and sealant applications) associated with Medicaid expansions in states where Medicaid did vs did not cover preventive dental services for adults.
2. METHODS
2.1. Data
We analyzed data from the Medical Expenditure Panel Survey‐Household Component (MEPS) for the years 2011‐2016. The MEPS includes detailed information about individuals' health care use (including visits to a dentist), health insurance status, socioeconomic status, and family characteristics. When weighted, the MEPS is representative of the noninstitutionalized US population. 25 , 26
We linked the MEPS to annual state‐level data on the status of Medicaid expansions 27 and to state Medicaid programs' coverage of dental benefits for adults for the period 2011‐2016. We constructed this dental coverage dataset by consolidating policy information from the Medicaid and CHIP Payment and Advisory Commission, 28 the Center for Health Care Strategies, 29 the Kaiser Family Foundation, 30 Medicaid state plan amendments filed with CMS, 31 and the peer‐reviewed literature 32 (Appendix S1).
We incorporated information from two other data sources. First, we used the Area Health Resources File (AHRF) to obtain annual county‐level measures of dental provider supply, poverty, and urbanicity. Second, we obtained annual state‐level data on fee‐for‐service Medicaid reimbursement rates for child dental prophylaxis (Dental Procedures and Nomenclature [CDT] code 1120) from the American Academy of Pediatrics' Medicaid reimbursement reports. 33 One of the authors (TK) checked and supplemented these payment data via personal communication with the American Dental Association's Health Policy Institute.
2.2. Study population
Our study sample consisted of dyads of children and parents in families with incomes ≤125 percent of the FPL (≤$32 750 in income for a family of four in 2020). 34 We limited our sample to children ages 6 to 18 years living with a nonelderly, nondisabled adult (parent or guardian) ages 21‐64. (For brevity, we refer to the adults in these dyads as parents.) We selected children age 6 and older because these children have either begun to, or have developed, permanent teeth. Consistent with prior research examining within‐family spillover effects of Medicaid policy, 18 we selected the mother or female guardian for the parent‐child dyad in two‐parent families, such that each child appeared in our study sample once and was linked to the characteristics of one parent. Children of women who were pregnant at any point during the calendar year and who did not have a father in the household were excluded because pregnant women gain dental coverage through Medicaid in many states during pregnancy. 35 , 36 Additional details of our inclusion criteria are reported in the Appendix S1.
2.3. Dependent variable
In our main analysis, we examined whether a child received any preventive dental service in the calendar year using the MEPS dental visit files. Preventive dental services were defined as dental prophylaxis (cleaning), fluoride treatment, 37 or sealant application 38 by a dental professional (Appendix S1). Healthy People 2020 identifies the use of these preventive dental services as important for improving children's oral health. 39 In subanalyses, we separately assessed children's receipt of a dental prophylaxis only vs fluoride treatment or sealants combined. We combined fluoride treatment and sealants as these methods have strong supporting evidence in preventing dental caries. 40 , 41
2.4. Independent variable
We analyzed two independent variables. First, we assessed whether states had implemented the ACA's Medicaid expansion by each year of our study period (through 2016). We considered a state to have expanded Medicaid by a given year if its expansion was effective on or before September 1 of that year. Second, we assessed states' coverage of dental benefits for adults in each study year. We considered states to have provided adult dental benefits if their Medicaid programs covered more than emergency services for adult Medicaid recipients. 22 , 32
2.5. Covariates
We included the following covariates in our analyses. First, we controlled for the following parental characteristics: age, sex, race/ethnicity, language, education, employment, and smoking status. Second, we adjusted for family income as a categorical variable (relative to the Federal Poverty Level), family size, and parental structure (a two‐parent household vs a single‐parent household). Third, we controlled for child age and sex. Fourth, at the county level, we controlled for the number of dentists per 1000 residents, the poverty rate, and an indicator for whether the family lived in an urban area (defined as a metropolitan statistical area). Finally, given the well‐documented relationship between Medicaid payment rates to providers and provider participation in Medicaid, 32 , 42 , 43 we adjusted for Medicaid reimbursement rates to dentists for a common preventive dental procedure (child prophylaxis, CDT code 1120), which we assessed at the state‐year level.
2.6. Statistical analyses
We assessed whether states' implementation of the ACA's Medicaid expansion was associated with increases in the probability that low‐income children received preventive dental care in states whose Medicaid programs did vs did not cover dental services for adults. Using the parent‐child dyad (indexed by i) as the unit of analysis, we estimated linear probability models of the form:
In this model, is a binary indicator that a child received at least one preventive dental service in year t, is a binary variable equal to one if a state Medicaid program covered dental services for adults in year t, and indicates whether state s had implemented the ACA's Medicaid expansion by year t. We adjusted for child, parent, and county‐level characteristics (), Medicaid fee‐for‐service payment rates for dental prophylaxis (), state fixed effects ( to control for time‐invariant state characteristics, and year fixed effects () to control for time trends common to all states. We adjusted for family survey weights in the MEPS and clustered standard errors at the state level for inference.
We report three estimates from this model:
, which represents the change in children's preventive dental care use associated with state Medicaid programs' coverage of preventive dental services for adults. Because our model includes state fixed effects, is estimated from within‐state changes in adult dental coverage policies.
, which is the change in children's preventive dental care use associated with Medicaid expansions in states that did not concurrently cover preventive dental services for adults.
, the differential change in children's preventive dental care use associated with Medicaid expansions in states that did vs did not concurrently cover preventive dental services for adults. This is our primary estimate of interest.
2.7. Supplementary analyses
We conducted four supplementary analyses. First, we examined whether Medicaid expansions were associated with increases over time in children's receipt of preventive dental services when states consistently covered these services for adults. To do so, we estimated event‐study models to assess time‐varying treatment effects of Medicaid expansions, separately in 24 states that covered dental services for adults in each year of our study period and in 19 states that did not cover these services in any study year (Table 2). We plotted unadjusted estimates from these event‐study models and report corresponding estimates of adjusted time‐varying effects in the Appendix S1.
TABLE 2.
States categorized by Medicaid expansion status and dental coverage policies for adults
| Medicaid coverage of preventive dental services for adults | Medicaid expansion status by 2016 | |
|---|---|---|
| Expanded (32 states) | Did not expand (19 states) | |
| All study years (2011‐2016; 24 states) | 19 states: AR, AK, CT, DC, IN, IA, KY, MA, MI, MN, NJ, NM, NY, ND, OH, OR, PA, RI, VT | 5 states: NE, NC, SD, WI, WY |
| Some study years (8 states) | 5 states: CA, CO, IL, MT, WA | 3 states: MO, SC, UT |
| No study years (19 states) | 8 states: AZ, DE, HI, LA, MD, NV, NH, WV | 11 states: AL, FL, GA, ID, KS, ME, MS, OK, TN, TX, VA |
Based on Kaiser Family Foundation data on the status of state Medicaid expansions and Medicaid dental coverage policies reported by the Medicaid and CHIP Payment and Advisory Commission, the Center for Health Care Strategies, the Kaiser Family Foundation, Medicaid state plan amendments filed with CMS, and the peer‐reviewed literature.
Second, to check whether we could isolate changes associated with Medicaid expansions from secular state trends, we used these event‐study models to examine whether pre‐expansion trends in children's preventive dental service use differed between expansion and nonexpansion states categorized according to their adult dental coverage policies.
Third, we examined whether Medicaid expansions with vs without concurrent adult dental coverage were associated with differential changes in the likelihood that low‐income children were enrolled in Medicaid or CHIP. We performed this analysis to examine whether Medicaid policy changes for adults might affect children's use of preventive dental care via take‐up of Medicaid or CHIP.
Fourth, we re‐estimated our main empirical model using logistic regression to test whether our estimates were sensitive to functional form.
3. RESULTS
Our analytic sample consisted of 7798 annual parent‐child dyads with incomes ≤125 percent FPL, representing 39 028 587 weighted pairs in our 6‐year study period (Table 1). The majority (79.4 percent) of children in these dyads were enrolled in CHIP or Medicaid, and 66.4 percent were racial or ethnic minorities. The preponderance of parents in the dyads (89.3 percent) was female, and 42.9 percent were enrolled in Medicaid. Across all study years, 37.8 percent of children received at least one annual preventive dental service, the majority of which were for dental prophylaxis (Figure S2 in Appendix S1). Over time, the proportion of low‐income children who received at least one preventive dental service increased from 36.2 percent in 2011 to 40.1 percent in 2016.
TABLE 1.
Study population characteristics
| Variable | Mean or proportion |
|---|---|
| Child characteristics | |
| Female, % | 50.0 |
| Child age in years, mean (SD) | 10.1 (0.06) |
| Child age, % by age category | |
| 6‐9 | 15.4 |
| 10‐14 | 32.5 |
| 15‐18 | 52.1 |
| Child race and ethnicity, % in category | |
| White non‐Hispanic | 33.7 |
| Black non‐Hispanic | 19.7 |
| Hispanic | 37.7 |
| Other | 9.0 |
| Child enrolled in Medicaid or CHIP, % | 79.4 |
| Parent characteristics | |
| Female, % | 89.3 |
| Parent age in years, mean (SD) | 37.8 (0.12) |
| Parent race and ethnicity, % in category | |
| White non‐Hispanic | 37.4 |
| Black non‐Hispanic | 19.5 |
| Hispanic | 35.7 |
| Other | 7.4 |
| Parent enrolled in Medicaid, % a | 42.9 |
| Parent comfortable with English language, % | 70.5 |
| Parent smoker, % | 25.5 |
| Parent education, % in category | |
| Less than high school | 30.4 |
| Completed high school | 35.6 |
| Any college | 33.2 |
| Not specified | 0.80 |
| Unemployed, % | 48.5 |
| Family characteristics | |
| Family size, % in category | |
| 2 or less | 13.3 |
| 3 | 20.6 |
| 4 | 26.9 |
| 5 | 21.5 |
| 6 | 10.8 |
| 7 or more | 6.8 |
| Family income as a percent of the Federal Poverty Level in category, % | |
| Less than 100% | 76.7 |
| 100% to less than 125% | 23.3 |
| Single‐parent family, % | 49.5 |
| Lives in urban area, % | 77.0 |
Analysis of N = 39 028 587 weighted dyads (7798 unweighted dyads) in families with income at or below 125 percent FPL who surveyed in the 2011‐2016 MEPS. Estimates were adjusted for family survey weights.
We did not adjust for parental enrollment in Medicaid in our regression analyses as this is an outcome of Medicaid expansions.
States vary considerably in their dental coverage policies for adults (Table 2). By the conclusion of our study period in 2016, 19 of the 32 states that expanded Medicaid covered dental services for adults in each year from 2011 to 2016. Of the 19 states that had not expanded Medicaid by 2016, five consistently covered dental services for adults from 2011 to 2016. Only eight states changed adult dental coverage policies during our study period. Because most of the variation in dental coverage is between (rather than within) states, we primarily focus on differences in the association of Medicaid expansions with children's dental care use between states with and without Medicaid dental coverage for adults.
Table 3 displays the adjusted associations between Medicaid expansions, Medicaid dental coverage for adults, and children's receipt of preventive dental care, as estimated from main empirical model (full regression estimates are shown in Table S2 of the Appendix S1). In states that covered preventive dental services for adults in Medicaid, implementation of the ACA's Medicaid expansion was not associated with a change in the probability that low‐income children received least one annual preventive dental service (1.26 percentage points; 95% CI: −3.74 to 6.27). (This corresponds to from our model.) In states that did not cover preventive dental services for adults in Medicaid, expansion was not associated with a statistically significant change in the probability that low‐income children received preventive dental care (3.03 percentage points; 95% CI: −2.76 to 8.81). The difference in these estimates, which corresponds to our regression estimate , was not statistically significant (−1.76 percentage points; 95% CI: −8.09 to 4.56) and small relative to mean preventive dental service utilization among children in our study population (approximately 36.2 percent of children in 2011 received at least one annual preventive dental service in 2011, and 40.1 percent did in 2016). We did not find any statistically significant associations between these Medicaid policies for adults and specific categories of preventive service use among children (dental prophylaxis vs fluoride treatment or sealant application).
TABLE 3.
Adjusted associations between Medicaid dental coverage for adults, Medicaid expansions, and children's receipt of preventive dental services
| Any preventive service | Dental prophylaxis | Fluoride treatment or sealant application | ||||
|---|---|---|---|---|---|---|
| Percent of children in families ≤ 125% of FPL receiving services (probability of any annual use) |
2011 36.2 |
2016 40.1 |
2011 35.5 |
2016 39.6 |
2011 11.8 |
2016 17.7 |
| Changes in children's preventive dental care use associated with: | ||||||
| Medicaid dental coverage for adults † |
−4.17 [−8.17, 0.27] |
−5.16* [−10.27, −0.05] |
1.91 [−2.55, 6.37] |
|||
| Medicaid expansions without concurrent dental coverage for adults ‡ |
3.03 [−2.76, 8.81] |
3.69 [−1.76, 9.15] |
−0.02 [−6.10, 6.07] |
|||
| Medicaid expansions in states with vs without Medicaid concurrent dental coverage for adults § |
−1.76 [−8.09, 4.56] |
−1.88 [−8.20, 4.44] |
−2.34 [−9.10, 4.40] |
|||
Estimates are from a multivariable linear regression model predicting child's receipt of preventive dental services as a function of Medicaid dental coverage for adults, Medicaid expansion, and an interaction between Medicaid expansion status and Medicaid dental coverage for adults, controlling for child, parent, and family‐level characteristics and state and year fixed effects. Estimates were adjusted for family survey weights. 95% confidence intervals [in brackets] were constructed using standard errors clustered at the state level. Any preventive service was defined as any dental cleaning, fluoride treatment, or sealant application visit. Analysis of N = 39 028 587 weighted dyads (7798 unweighted dyads) in families with income at or below 125 percent FPL surveyed in the 2011‐2016 MEPS. Estimates are reported in percentage points.
P < .05.
Corresponds to from the regression model.
Corresponds to from the regression model.
Corresponds to coefficient from the regression model.
In sensitivity analyses, we examined potential sources of bias in our study design and assessed the robustness of our estimates to the functional form of our regression models. First, we separately examined time‐varying changes in children's use of preventive dental services associated with Medicaid expansions in states that continuously covered Medicaid dental benefits for adults and in states that did not cover dental benefits for adults in any year of our study period (Figure 1; estimates reported in Table S3 in the Appendix S1). We found no evidence of gains in children's preventive dental care use in the postexpansion period or evidence of effects that began to emerge more prominently several years after expansion.
FIGURE 1.
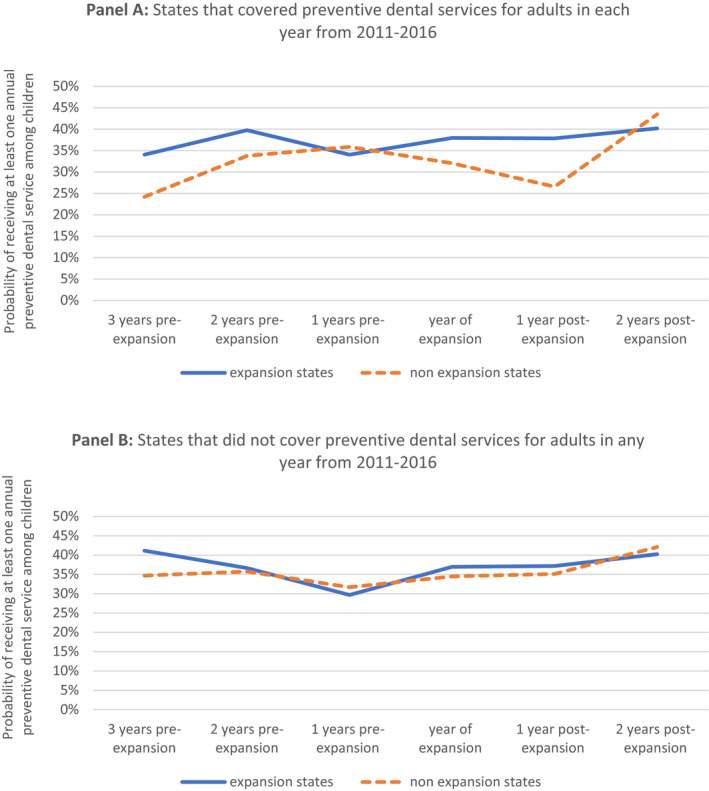
Trends in children's use of preventive dental services in states categorized by Medicaid expansion status and coverage of preventive dental services for adults in Medicaid [Colour figure can be viewed at wileyonlinelibrary.com].
Note: States were categorized by their Medicaid expansion status and coverage of preventive dental services for adults (see Table 2 for details). We report unadjusted probabilities of receiving at least one annual preventive dental service use among low‐income children in each year relative to Medicaid expansion (in states that expanded Medicaid by 2016) or relative to 2014 (for states that had not expanded by 2016). Estimates are reported separately for 24 states whose Medicaid programs covered preventive dental services for adults in each year from 2011 to 2016 (Panel A) and 19 states whose Medicaid programs did not cover preventive dental services for adults in any study year (Panel B) [Colour figure can be viewed at wileyonlinelibrary.com]
Second, we examined whether our estimates of changes in children's preventive dental service use before and after ACA's Medicaid expansion could have been biased by differential trends preceding this expansion (or prior to 2014 for nonexpansion states). In states that continuously covered dental benefits for adults during our study period, we found a modest, but not statistically significant, increase in children's preventive dental service use prior to 2014 in nonexpansion states compared to pretrends in expansion states. In states that did not cover dental benefits for adults in any year of our study period, we did not detect an appreciable difference in pretrends between expansion and nonexpansion states. Thus, while secular trends are unlikely to substantially affect our estimates, any bias they introduce would likely make our estimates slightly conservative given the secular increases in children's dental care use in nonexpansion (rather than expansion) states that provided dental benefits for adults.
Third, we did not find that Medicaid expansions were associated with differential increases in Medicaid or CHIP take‐up among low‐income children in states that did vs did not concurrently cover dental benefits for adults (Table S4 in the Appendix S1).
Finally, we explored whether our estimates were sensitive to the functional form of the regression models we ran. Table S5 of the Appendix S1 displays the results of logit model, for which our estimates were qualitatively similar to those of the linear model presented in our main analyses.
4. DISCUSSION
In this study, we used nationally representative data from the Medical Expenditure Panel Survey to examine the use of preventive dental services among low‐income children and to assess whether changes in state Medicaid policies that affect low‐income adults' access to dental care are linked to changes in children's use of preventive dental services. On average from 2011 to 2016, we found that 37.8 percent of low‐income children received at least one annual preventive dental service—considerably lower than has been reported in higher‐income populations 44 —which is consistent with prior evidence that low‐income children face persistent barriers to dental care. 45 , 46 Given evidence that parental access to care through Medicaid may have “spillover” effects on children's health care use, 15 , 16 , 17 , 18 we studied whether expansions of Medicaid with concurrent dental coverage for adults were linked to increases in children's use of preventive dental care. We did not find statistically significant changes in children's use of preventive dental care associated with expansions in states that did vs did not cover preventive dental care for adults in Medicaid. However, our estimates are imprecise, with wide confidential intervals that are unable to rule out sizable effects in either direction.
These results stand in contrast to other studies that found positive “spillover” effects of adult Medicaid coverage on low‐income children's use of physical health care. 15 , 16 , 17 , 18 Our findings may reflect differences in health services systems for medical and dental care or persistent barriers to dental care use among children. For example, dental care has historically operated separately from medical care and has focused on tertiary treatment rather than prevention. 47 In addition, inadequate referral systems between physicians and dentists 48 , 49 and the limited availability of dentists accepting Medicaid patients 50 , 51 present continued barriers to dental care access among low‐income children and might limit extent to which children benefit when their parents receive dental coverage through Medicaid.
A growing body of research demonstrates that implementation of the ACA's Medicaid expansion has had favorable effects on adult dental service use and oral health outcomes when states cover dental services for adults in Medicaid, although these effects may vary by population or local variation in the supply of dental providers. 22 , 23 , 24 , 52 This evidence led us to hypothesize a possible “spillover” effect of Medicaid expansions and dental coverage for adults on low‐income children's use of preventive dental care. However, we did not find evidence of such a spillover effect, suggesting that policies other than adult dental coverage through Medicaid may play a more prominent role in children's receipt of preventive dental services.
Policies that directly expand access to dental care for children may have more direct impacts on children's dental care use. For example, school‐based oral sealant programs have been found to be effective in increasing sealant use and in preventing dental caries among low‐income children. 53 , 54 In addition, all state Medicaid programs now reimburse primary care providers for fluoride varnish treatment following a 2014 US Preventive Services Task Force (USPTF) recommendation. 55 This has led to increased fluoride varnish use and improved oral health outcomes among low‐income children. 56 , 57
Although we did not find evidence that expansions of Medicaid with dental coverage for adults affected children's use of preventive dental care, our findings should not be construed as evidence that Medicaid policies are unrelated to oral health care access or outcomes in low‐income populations. First, low‐income adults have substantial oral health needs 58 , 59 , 60 and a large literature demonstrates that adults derive direct benefits when Medicaid facilitates greater access to preventive dental care. For example, providing comprehensive dental coverage for adults in Medicaid is associated with an increase in dental visits, preventive and restorative service use, and improved oral health outcomes. 32 , 61 , 62 Conversely, losing Medicaid dental coverage has been linked to increased ED use for nontraumatic dental conditions. 63 Second, our findings do not necessarily imply that policies restricting dental benefits for adults in Medicaid would not harm children's access to preventive dental services.
Limitations of our study design could have biased us away from finding a beneficial effect of increases in parental dental coverage in Medicaid on children's use of dental care. First, our estimates could have been biased by unobserved changes in the characteristics of Medicaid enrollees or factors linked to children's receipt of dental care. For example, we did not control for variation in dental provider networks established by Medicaid Managed Care Organizations (MCOs), payment rates negotiated between Medicaid MCOs and dental providers (which may differ from those in fee‐for‐service Medicaid), or whether states “carved‐out” dental benefits from physical health benefits in Medicaid. Second, secular increases (though small) in children's use of preventive dental services in states that did not expand Medicaid but did cover preventive dental services for adults may have biased us away from finding a beneficial effect of Medicaid expansions in dental coverage states. Finally, we acknowledge that Medicaid expansions may take time to yield detectable gains in children's use of preventive dental services. However, we did not find any significant gains among children by the third year of expansion in states whose Medicaid programs consistently covered dental benefits for adults.
5. CONCLUSION
Although prior research found that expanded Medicaid coverage for parents has “spillover” effects on children's use of medical services, we did not find evidence of a similar relationship between Medicaid expansions with concurrent adult dental coverage and low‐income children's use of preventive dental services. Factors other than Medicaid eligibility and dental coverage policies for adults may be more salient determinants of preventive dental care use among low‐income children.
Supporting information
Author Matrix
Appendix S1
ACKNOWLEDGMENT
Joint Acknowledgment/Disclosure Statement: Dr Roberts was supported by a research scientist development award from the Agency for Healthcare Research and Quality (grant number K01HS026727). This content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. Dr Donohue receives salary support from Pennsylvania Department of Human Services. No Other Disclosures.
Khouja T, Burgette JM, Donohue JM, Roberts ET. Association between Medicaid expansion, dental coverage policies for adults, and children's receipt of preventive dental services. Health Serv Res. 2020;55:642–650. 10.1111/1475-6773.13324
REFERENCES
- 1. Vujicic M, Nasseh K. A decade in dental care utilization among adults and children (2001‐2010). Health Serv Res. 2014;49(2):460‐480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nasseh K, Vujicic M. Dental Care Utilization Steady among Working‐Age Adults and Children, Up Slightly among the Elderly. Chicago: Health Policy Institute Research Brief. American Dental Association; 2016. [Google Scholar]
- 3. Fleming E, Afful J. Prevalence of total and untreated dental caries among youth: United States, 2015‐2016. NCHS Data Brief. 2018;307:1‐8. [PubMed] [Google Scholar]
- 4. Jackson SL, Vann WF Jr, Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children's school attendance and performance. Am J Public Health. 2011;101(10):1900‐1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Seirawan H, Faust S, Mulligan R. The impact of oral health on the academic performance of disadvantaged children. Am J Public Health. 2012;102(9):1729‐1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Li KY, Okunseri CE, McGrath C, Wong MC. Trends in self‐reported oral health of US adults: National Health and Nutrition Examination Survey 1999–2014. Commun Dent Oral Epidemiol. 2018;46(2):203‐211. [DOI] [PubMed] [Google Scholar]
- 7. Department of Health & Human Services . Oral Health in America: A Report of the Surgeon General. Washington, D.C.: NIH Publication; 2000;155‐188. [Google Scholar]
- 8. Otomo‐Corgel J, Pucher JJ, Rethman MP, Reynolds MA. State of the science: chronic periodontitis and systemic health. J Evid Based Dent Pract. 2012;12(3 Suppl):20‐28. [DOI] [PubMed] [Google Scholar]
- 9. Glied S, Neidell M. The economic value of teeth. J Hum Resour. 2010;45(2):468‐496. [Google Scholar]
- 10. Lee I, Monahan S, Serban N, Griffin PM, Tomar SL. Estimating the cost savings of preventive dental services delivered to Medicaid‐enrolled children in six southeastern states. Health Serv Res. 2018;53(5):3592‐3616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sen B, Blackburn J, Morrisey MA, et al. Effectiveness of preventive dental visits in reducing nonpreventive dental visits and expenditures. Pediatrics. 2013;131(6):1107‐1113. [DOI] [PubMed] [Google Scholar]
- 12. Edelstein BL, Chinn CH. Update on disparities in oral health and access to dental care for America's children. Acad Pediatr. 2009;9(6):415‐419. [DOI] [PubMed] [Google Scholar]
- 13. Fisher‐Owens SA, Soobader MJ, Gansky SA, et al. Geography matters: state‐level variation in children's oral health care access and oral health status. Public Health. 2016;134:54‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Isong IA, Zuckerman KE, Rao SR, Kuhlthau KA, Winickoff JP, Perrin JMJP. Association between parents' and children's use of oral health services. Pediatrics. 2010;125:502‐508. [DOI] [PubMed] [Google Scholar]
- 15. Dubay L, Kenney G. Expanding public health insurance to parents: effects on children's coverage under Medicaid. Health Serv Res. 2003;38(5):1283‐1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. DeVoe JE, Marino M, Angier H, et al. Effect of expanding Medicaid for parents on children's health insurance coverage: lessons from the Oregon experiment. JAMA Pediatr. 2015;169(1):e143145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hudson JL, Moriya AS. Medicaid expansion for adults had measurable 'welcome mat' effects on their children. Health Aff (Millwood). 2017;36(9):1643‐1651. [DOI] [PubMed] [Google Scholar]
- 18. Venkataramani M, Pollack CE, Roberts ET. Spillover effects of adult medicaid expansions on children's use of preventive services. Pediatrics. 2017;140(6):e20170953. [DOI] [PubMed] [Google Scholar]
- 19. Medicaid.Gov . Dental care. https://www.medicaid.gov/medicaid/benefits/dental/index.html. Accessed September 9, 2018
- 20. Edelstein BL. Pediatric oral health policy: its genesis, domains, and impacts. Pediatr Clin North Am. 2018;65(5):1085‐1096. [DOI] [PubMed] [Google Scholar]
- 21. Center for Health Care Strategies . Medicaid adult dental benefits: an overview. January 2018.
- 22. Singhal A, Damiano P, Sabik L. Medicaid adult dental benefits increase use of dental care, but impact of expansion on dental services use was mixed. Health Aff (Millwood). 2017;36(4):723‐732. [DOI] [PubMed] [Google Scholar]
- 23. Elani HW, Kawachi I, Sommers BD. Changes in emergency department dental visits after Medicaid expansion. Health Serv Res. 2020;55(3):367‐374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wehby GL, Lyu W, Shane DM. The impact of the ACA Medicaid expansions on dental visits by dental coverage generosity and dentist supply. Med Care. 2019;57(10):781‐787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cohen S. Sample design of the 1996 medical expenditure panel survey household component MEPS methodology report No. 2. AHCPR Pub. 1997(97‐0027).
- 26. Agency for Healthcare Research and Quality . Medical expenditure panel surevy‐survey background. 2009; https://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp. Accessed December 5, 2018
- 27. Kaiser Family Foundation . Status of state Medicaid expansion decisions. https://www.kff.org/medicaid/issue‐brief/status‐of‐state‐medicaid‐expansion‐decisions‐interactive‐map/. Accessed September 2019
- 28. MACPAC . TMaCPaAC. Chapter 2: Medicaid coverage of dental benefits for adults. 2015.
- 29. Center for Health Care Strategies Inc . Medicaid Adult Dental Benefits: An Overview. February 2015.
- 30. Kaiser Family Foundation . Medicaid benefits: dental services. https://www.kff.org/medicaid/state‐indicator/dental‐services. Accessed September 9, 2018
- 31. Centers for Medicare & Medicaid Services . Medicaid state plan amendments. https://www.medicaid.gov. Accessed September 9, 2018
- 32. Decker SL, Lipton BJ. Do Medicaid benefit expansions have teeth? The effect of Medicaid adult dental coverage on the use of dental services and oral health. J Health Econ. 2015;44:212‐225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Academy American of Pediatrics . Medicaid reimbursement reports. https://www.aap.org/en‐us/professional‐resources/Research/research‐resources/Pages/Medicaid‐Reimbursement‐Reports.aspx. Accessed September 4, 2019
- 34. U.S. Department of Health & Human Services . Poverty guidelines. 2019; https://aspe.hhs.gov/2019‐poverty‐guidelines. Accessed December 5, 2019
- 35. Kloetzel MK, Huebner CE, Milgrom P. Referrals for dental care during pregnancy. J Midwifery Womens Health. 2011;56(2):110‐117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Children's Dental Health Project . Oral health during pregnancy: oral health's unanswered questions. September 2018.
- 37. Marinho VC, Worthington HV, Walsh T, Clarkson JE. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2013;7:Cd002279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wright JT, Crall JJ, Fontana M, et al. Evidence‐based clinical practice guideline for the use of pit‐and‐fissure sealants: a report of the American Dental Association and the American Academy of Pediatric Dentistry. J Am Dent Assoc. 2016;147(8):672‐682 e612. [DOI] [PubMed] [Google Scholar]
- 39. U.S. Department of Health & Human Services . Healthy People 2020 topics and objectives: oral health. 2011.
- 40. Azarpazhooh A, Main PA. Efficacy of dental prophylaxis (rubber cup) for the prevention of caries and gingivitis: a systematic review of literature. Br Dent J. 2009;207(7):E14; discussion 328‐329. [DOI] [PubMed] [Google Scholar]
- 41. Wei L, Griffin SO, Robison VA. Disparities in receipt of preventive dental services in children from low‐income families. Am J Prev Med. 2018;55(3):e53‐e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Buchmueller TC, Orzol S, Shore‐Sheppard LD. The effect of Medicaid payment rates on access to dental care among children. American Journal of Health Economics. 2015;1(2):194‐223. [Google Scholar]
- 43. Decker SL. Changes in Medicaid physician fees and patterns of ambulatory care. Inquiry. 2009;46(3):291‐304. [DOI] [PubMed] [Google Scholar]
- 44. Berdahl T, Hudson J, Simpson L, McCormick MC. Annual report on children's health care: dental and orthodontic utilization and expenditures for children, 2010‐2012. Acad Pediatr. 2016;16(4):314‐326. [DOI] [PubMed] [Google Scholar]
- 45. Dye BA, Tan S, Smith V, et al. Trends in oral health status; United States, 1988‐1994 and 1999‐2004. 2007. [PubMed]
- 46. Li C‐H, Albuquerque MS, Gooch BF. Use of dental care and effective preventive services in preventing tooth decay among US children and adolescents—Medical Expenditure Panel Survey, United States, 2003–2009 and National Health and Nutrition Examination Survey, United States, 2005–2010. MMWR Suppl. 2014;63(2):54. [PubMed] [Google Scholar]
- 47. Watt RG, Daly B, Allison P, et al. Ending the neglect of global oral health: time for radical action. Lancet. 2019;394(10194):261‐272. [DOI] [PubMed] [Google Scholar]
- 48. Kranz AM, Rozier RG, Preisser JS, Stearns SC, Weinberger M, Lee JY. Examining continuity of care for Medicaid‐enrolled children receiving oral health services in medical offices. Matern Child Health J. 2015;19(1):196‐203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Harnagea H, Couturier Y, Shrivastava R, et al. Barriers and facilitators in the integration of oral health into primary care: a scoping review. BMJ Open. 2017;7(9):e016078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Seale NS, Casamassimo PS. Access to dental care for children in the United States. J Am Dent Assoc. 2003;134(12):1630‐1640. [DOI] [PubMed] [Google Scholar]
- 51. Smith RG, Lewis CW. Availability of dental appointments for young children in King County, Washington: implications for access to care. Pediatr Dent. 2005;27(3):207‐211. [PubMed] [Google Scholar]
- 52. Nasseh K, Vujicic M. The impact of the affordable care act's Medicaid expansion on dental care use through 2016. J Public Health Dent. 2017;77(4):290‐294. [DOI] [PubMed] [Google Scholar]
- 53. Griffin S, Naavaal S, Scherrer C, Griffin PM, Harris K, Chattopadhyay S. School‐based dental sealant programs prevent cavities and are cost‐effective. Health Aff (Millwood). 2016;35(12):2233‐2240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Griffin SO, Naavaal S, Scherrer C, Patel M, Chattopadhyay S, Community Preventive Services Task Force . Evaluation of school‐based dental sealant programs: an updated community guide systematic economic review. Am J Prev Med. 2017;52(3):407‐415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. U.S. Preventive Services Task Force . Final update summary: dental caries in children from birth through age 5 years: screening. 2014; https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/dental‐caries‐in‐children‐from‐birth‐through‐age‐5‐years‐screening. Accessed September 9, 2018
- 56. Kranz AM, Duffy E, Dick AW, Sorbero M, Rozier RG, Stein BD. Impact of Medicaid policy on the oral health of publicly insured children. Matern Child Health J. 2019;23(1):100‐108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Kranz AM, Preisser JS, Rozier RG. Effects of physician‐based preventive oral health services on dental caries. Pediatrics. 2015;136(1):107‐114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Li KY, Okunseri CE, McGrath C, Wong MCM. Trends in self‐reported oral health of US adults: National Health and Nutrition Examination Survey 1999‐2014. Community Dent Oral Epidemiol. 2018;46(2):203‐211. [DOI] [PubMed] [Google Scholar]
- 59. Moeller J, Starkel R, Quinonez C, Vujicic M. Income inequality in the United States and its potential effect on oral health. J Am Dent Assoc. 2017;148(6):361‐368. [DOI] [PubMed] [Google Scholar]
- 60. Hom JK, Wong C, Stillson C, et al. New Medicaid enrollees see health and social benefits in Pennsylvania's expansion. Inquiry. 2016;53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Choi MK. The impact of Medicaid insurance coverage on dental service use. J Health Econ. 2011;30(5):1020‐1031. [DOI] [PubMed] [Google Scholar]
- 62. Abdus S, Decker SL. Association between Medicaid adult nonemergency dental benefits and dental services use and expenditures. J Am Dent Assoc. 2019;150(1):24‐33. [DOI] [PubMed] [Google Scholar]
- 63. Singhal A, Caplan DJ, Jones MP, et al. Eliminating Medicaid adult dental coverage in California led to increased dental emergency visits and associated costs. Health Aff (Millwood). 2015;34(5):749‐756. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author Matrix
Appendix S1


