Abstract
Rationale
Due to lack of vaccine or cure, the COVID-19 pandemic presents a threat to all human beings, undermining people's basic sense of safety and increasing distress symptoms.
Objective
To investigate the extent to which individual resilience, well-being and demographic characteristics may predict two indicators of Coronavirus pandemic: distress symptoms and perceived danger.
Method
Two independent samples were employed: 1) 605 respondents recruited through an internet panel company; 2) 741 respondents recruited through social media, using snowball sampling. Both samples filled a structured online questionnaire. Correlations between psychological/demographic variables and distress and perceived danger were examined. Path analysis was conducted to identify predictive indicators of distress and perceived danger.
Results
Significant negative correlations were found between individual/community resilience and sense of danger (−0.220 and −0.255 respectively; p < .001) and distress symptoms (- 0.398 and −0.544 respectively; p < .001). Significant positive correlations were found between gender, community size, economic difficulties and sense of danger (0.192, 0.117 and 0.244 respectively; p < .001). Gender and economic difficulties also positively correlated with distress symptoms (0.130 and 0.214 respectively; p < .001). Path analysis revealed that all paths were significant (p < .008 to .001) except between family income and distress symptoms (p = .12). The seven predictors explained 20% of sense of danger variance and 34% the distress symptoms variance. The most highly predictive indicators were the two psychological characteristics, individual resilience, and well-being. Age, gender, community size, and economic difficulties due to COVID-19 further add to predicting distress, while community and national resilience do not. .
Conclusions
Individual resilience and well-being have been found as the first and foremost predictors of COVID-19 anxiety. Though both predictors are complex and may be influenced by many factors, given the potential return of COVID-19 threat and other future health pandemic threats to our world, we must rethink and develop ways to reinforce them.
Highlights
-
•
Current study was conducted during a peak in the COVID-19 pandemic, 1st wave.
-
•
Two pandemic effects, distress symptoms and perceived danger, were examined.
-
•
Best pandemic effect psychological predictors: individual resilience well-being.
-
•
Best pandemic effect’ demographic predictors: age, gender, economic difficulties.
-
•
Community and national resilience did not significantly add to predictions.
1. Introduction
The Coronavirus disease (COVID-19), which erupted in China in 2019, is an infectious disease caused by a newly discovered strain of Coronavirus. This pandemic has rapidly spread worldwide, with constantly growing numbers of morbidity and mortality (Wang et al., 2020a, b). As a result, a large part of the international community has had to cope with the impact of the crisis on almost all aspects of life, including increased morbidity and mortality (Anderson et al., 2020). It is still unclear how long the epidemic will last and what long-term effects it will cause. Yet, it is already clear that the epidemic involves, among other things, the creation of distress among people beyond geographical locations and cultural and social systems (Wang et al., 2020a, b).
The present study, conducted in Israel, examined the extent to which measurements of resilience and demographic characteristics predict two indicators of the COVID-19 pandemic: distress symptoms and sense of danger (World Health Organization, 2020), after controlling for the effects of each other. These effects have been previously studied in the context of security manmade conflicts, natural disasters, and economic crises (Kimhi et al., 2020; Cutter et al., 2008), but have hardly been studied in the context of a large-scale pandemic crisis.
1.1. Distress symptoms and a sense of danger due to the COVID-19 pandemic
The COVID-19 epidemic is a clear and tangible threat to all humans, as there is no validated vaccine or cure for it. As a result, this threatening and painful pandemic undermines people's basic sense of safety and increases distress symptoms. These symptoms include continuous emotional and behavioral difficulties (Soffer-Dudek, 2016) such as depression, anxiety, and grief (Hadi et al., 2006).
The carriers of the COVID-19 are most frequently unrecognizable in the early stages of the disease, which increases the risk of transmission, and may also cause increased apprehension, due to perceived difficulty in defending against (Anderson et al., 2020). Threats on the individual or community safety and wellbeing, as well as the materialization of disastrous events, are likely to enhance a continuous sense of danger that strongly and negatively influences the reaction to such adversities (Scott et al., 2012). A high sense of danger is positively correlated with distress symptoms (Braun-Lewensohn and Al-Sayed, 2018) and negatively correlated with a sense of coherence (Antonovsky, 1993), as well as with individual resilience (Kimhi and Eshel, 2016). Levels of individual distress symptoms and a sense of danger, in the context of the COVID-19 pandemic, constitute the predicted variables in the current study. The main question raised in this study is, to what extent resilience, wellbeing, and demographic characteristics predict distress symptoms and sense of danger?
1.1.1. Resilience
Masten (2018) defines resilience as “the potential of the manifested capacity of a dynamic system to adapt successfully to disturbances that threaten the function, survival, or development of the system”, (P. 187), whereas the American Psychological Association defines resilience as a process of bouncing back from difficult experiences and adapting well in the face of adversity, trauma, tragedy, threats or significant sources of stress (//APA.orgAPA.org, 2014). The importance of the concept of resilience is derived from its direct link to the ability to effectively respond to sudden occurences (Turenne et al., 2019). Three types of resilience are studied more often: individual, community, and national resilience.
Individual resilience is defined as a stable trajectory of healthy functioning after a highly adverse event (Bonanno, 2004). Hjemdal et al. (2011) report that individual resilience (IR) contributes significantly and negatively to the prediction of depression, anxiety, stress, and obsessive-compulsive symptoms. Cacioppo et al. (2011) define it as “the capacity to foster, engage in, and sustain positive relationships and to endure and recover from life stressors and social isolation” (p. 44).
According to Bonanno et al. (2015), community resilience (CR) expresses the interaction between individuals and their community and refers to the success of the community to provide for the needs of its members and the extent to which individuals are helped by their community. A recent literature review claims that CR is associated with increased local capacity, social support, and resources, and with decreased risks, miscommunication, and traumas (Patel et al., 2017).
National resilience (NR) is a broad concept addressing issues of social sustainability and strength in several diverse realms: trust in the integrity of the government, the parliament and other national institutions, belief in social solidarity, and patriotism (Ben-Dor et al., 2002). Examination of the relevant literature indicates that a rather small number of studies have empirically investigated NR and associated it with antecedent variables (e.g., Kimhi and Eshel, 2019). A previous study examined the three levels of resilience and distress due to the COVID-19 pandemic reported that national and community resilience did not add to the prediction of the prediction of distress (Eshel et al., 2020, Kimhi et al., 2020). Based on the above study we will examine similar model of prediction.
To the best of our knowledge, the associations between the three types of resilience, along with relevant demographic variables, as predictors of stress is hardly investigated. The COVID-19 thus presents a unique opportunity in terms of its scope and impact on diverse aspects of life, to study this phenomenon.
1.1.2. Well-being
Well-being is the subjective feeling of health and a positive perception of an individual's quality of life (Hernandez et al., 2018). Earlier studies reported a negative association between distress and well-being (Branson et al., 2019) and a positive association between individual resilience and wellbeing (Eshel and Kimhi, 2016). In the current study, well-being constitutes a predictor of both senses of danger and distress symptoms with the COVID-19 threats. A previous study regarding the community and national resilience, of Israelis living next to the Gaza Strip (an area characterized by an ongoing security threat), has shown that community and national resilience are better predicated by psychological variables than by demographic variables (). Based on these findings, we hypothesized that in the current study the psychological variables, such as individual resilience and well-being, would better predict the sense of danger and the stress symptoms than demographic variables such as family income or age.
1.1.3. Demographic characteristics
Previous studies have found that the demographic characteristics of age, gender, and family income have predicted stress and resilience, primarily in the context of security threats (Eshel and Kimhi, 2016; Marciano et al., 2019). Another study has reported a significant association between the size of the community and community resilience (Kimhi et al., 2013). The current study employed both demographic and psychological variables as predictors of distress in the context of the COVID-19 pandemic. According to the above discussion, we assumed that compared with the psychological factors the demographic characteristics would serve as weaker predictors of sense of danger and distress symptoms (Eshel et al., 2019).
To conclude, based on the above we hypothesized the following: (1) Individual resilience and well-being will negatively significantly predict the levels of sense of danger and distress symptoms. (2) Demographic characteristics (age, gender, community size, and economic difficulties due to the pandemic) will add significantly to this prediction, beyond the effects of resilience and wellbeing. (3) The two psychological characteristics will better predict distress and sense of danger, compared with the four demographic characteristics. In the absence of previous relevant studies in the context of pandemics, we posed a research question: Will community and national resilience significantly add to the prediction of sense of danger and distress symptoms?
2. Method
2.1. Sample and sampling
Two independent samples of Jewish Israelis were employed: (a) An internet sample of 605 respondents derived at random from a large pool of an internet survey company. This sample included similar numbers of males and females (299 females), who agreed to participate in this research (for the reliability and validity of an on-line questionnaire, see Vallejo et al., 2007). (b) The second internet sample included 741 respondents (535 females and 206 males). A snowball sampling was used in which respondents were invited to participate in an online survey and were later asked to invite other potential participants by forwarding the study's online link.
All data was gathered anonymously, following approval of the IRB of the Tel Aviv University. All participants signed an informed consent form before filling out the questionnaires. The aggregation of the participants from both samples constituted the sample analyzed in the present study (N = 1,346, see an explanation for the consolidation of samples at the beginning of the results section). Participants are characterized by a wide range of demographic attributes (Note: Table 1 ).
Table 1.
Distribution of demographic attributes of the present sample (N = 1346).
| Variable | Ranting scale and range | Frequency | Percent (%) | M | SD |
|---|---|---|---|---|---|
| Age groups | 1. 18-30 | 449 | 33 | 42.00 | 16.35 |
| 2. 31-40 | 253 | 19 | |||
| 3. 41-50 | 210 | 16 | |||
| 4. 51-60 | 207 | 15 | |||
| 6. 61-70 | 160 | 12 | |||
| 7. 71+ | 58 | 4 | |||
| Gender | 1. Males | 512 | 38 | 2.82 | 1.23 |
| 2. Female | 834 | 62 | |||
| Level of religiosity | 1. Secular | 798 | 59 | ||
| 2. Traditional | 305 | 23 | |||
| 3. Religious | 186 | 14 | |||
| 4. Vary religious | 57 | 4 | |||
| Family income | Much lower | 258 | 19 | 2.82 | 1.23 |
| Lower | 289 | 21 | |||
| Average | 344 | 26 | |||
| Higher | 352 | 26 | |||
| Much higher | 103 | 8 | |||
| Political attitudes | 1. Extreme left | 57 | 4 | 3.20 | 1.01 |
| 2. Left | 284 | 21 | |||
| 3. Center | 452 | 34 | |||
| 4. Right | 435 | 32 | |||
| 5. Extreme right | 118 | 9 | |||
| Size of community | 1. 0-1000 | 235 | 17 | 3.42 | 1.62 |
| 2. 1000–10,000 | 186 | 14 | |||
| 3. 10,000–20,000 | 251 | 19 | |||
| 4. 20,000 50,000 | 295 | 22 | |||
| 5. 50,000–200,000 | 203 | 15 | |||
| 6. 200,000 and on | 174 | 13 | |||
| Economic difficulties | 1. Not at all | 230 | 17 | 2.79 | 1.27 |
| 2. A little | 393 | 29 | |||
| 3. Medium | 320 | 24 | |||
| 4. Much | 230 | 17 | |||
| 5. Very much | 173 | 13 |
2.2. Instruments
2.2.1. Sense of danger
A seven-item Sense of danger Scale, which was based on Solomon and Prager (1992) scale and referred to as a lingering sense of danger in the context of security threats was employed. However, instead of the term “security”, the threat was modified into the “COVID-19 pandemic threat” in all the relevant questions (e.g., “To what extent are you worried about the increase of the COVID-19 global crisis?”). Furthermore, one item was added to the scale: “To what extent are you worried that we will not be able to overcome the COVID-19 crisis before many citizens in our country will die from this disease”? Responses were rated on a Likert-like scale ranging from 1 (not at all) to 5 (very much). The reliability of this scale in the present study was high (Cronbach's α = 0.79).
2.2.2. Distress symptoms
The level of individual distress symptoms, in the context of the COVID-19 pandemic, was determined by nine items from the Brief Symptom Inventory (BSI, Derogatis and Savitz, 2000) which concern anxiety and depression. This inventory was scored by a Likert scale ranging from 1 (not suffering at all) to 5 (suffering very much). For example, “How much do you suffer from feelings of a sudden fear with no reason?”. Due to ethical considerations, we did not include the item concerning suicidal thoughts. Cronbach's alpha of this scale for the present study was high (α = 0.86).
2.2.3. Individual resilience
Individual resilience was measured by a 10-item Connor-Davidson scale (CD-RISC 10, Campbell-Sills and Stein, 2007) portraying individual feelings of ability and power in the face of difficulties. This scale was rated by a 5-point response scale ranging from 1 = not true at all, to 5 = generally true. Significant positive correlations between this scale and emotional intelligence, life satisfaction, self-esteem, and positive affect as well as negative significant correlation with negative affect have been reported by Alarcón et al. (2020). Reliability of this scale in the investigated sample was high (α = 0.85).
2.2.4. Community resilience
A short version of 10 items of the community resilience scale has been employed (CCRAM10; Leykin et al., 2013). Items pertaining to the ‘security crisis' were modified into the ‘Coronavirus crisis'. This tool encompassed five main issues: social trust, social support, leadership, emergency preparedness, and attachment to place (e.g., ‘‘I trust the decision-makers in my community’‘). Items of this scale were rated by a five-point scale ranging from 1 (does not agree at all) to 5 (totally agree). Reliability of this scale was high (α = 0.92).
2.2.5. National resilience
A short version of the National Resilience Scale was employed (Kimhi and Eshel, 2019). This 13-item tool pertained to trust in national leadership, patriotism, and trust in major national institutions. (e.g., “I love Israel and am proud of it”). In this study, we added three items regarding the COVID-19 pandemic (e.g., “I have full faith in the ability of my country's health system to care for the population in the current coronavirus crisis”). The six-point response scale ranged from 1 (very strongly disagree) to 6 (very strongly agree). Reliability in the present sample was high (α = 0.92).
2.2.6. Well-being
The present measure of well-being was based on the Recovery from War Scale (Kimhi and Shamai, 2004; Kimhi and Eshel, 2009). This nine-item self-report scale described perceived individual strengths in the domains of work, health, recreation, wider social contacts, achievements, family relations, daily functioning, relations with friends, and general assessment of one's life. The six-point response scale ranged from 1 = not good at all to 6 = very good. Reliability of this scale in the present study was high (α = 0.82).
2.2.7. Demographic variables
Seven demographic attributes were examined: (a) age; (b) gender; (c) religiosity: This variable was assessed by one item with a four-point scale ranging from 1 = secular to 4 = ultra-orthodox. (d) Family income level: This variable was assessed by 1-item with a 5-point response scale ranging from 1 = much above-average to 5 = much below average. (e) Educational level: This variable was assessed by one item with a five-point scale ranging from 1 = elementary school to 5 = academic (master's degree and beyond). (f) Size of community: Respondents marked the name of their community and we added the size of the community according to the Israeli Central Bureau of Statistics: 1 = up to 1000, 2 = 1001–10,000, 3 = 10,001–20,000, 4 = 20,001–50,000, 5 = 50,001–200,000, 6 = 200,001 and more. And (g), economic difficulties: This variable was assessed by one item “Are you or your family experiencing financial difficulties due to the COVID-19 pandemic (such as unemployment, downsizing business operations and so on)". The scale ranges from 1 = not at all to 5 = very much.
2.2.8. Data analysis
We examined our first hypothesis according to which individual resilience and well-being will significantly predict levels of sense of danger and distress symptoms, and our second hypothesis, according to which demographic characteristics will add significantly to this prediction, using path analysis/Amos Structural Equation Modeling (IBM, SPSS, https://www.ibm.com/il-en/marketplace/structural-equation-modeling-sem; Arbuckle, 2011). We used Maximum likelihood estimates and examined a saturated model, as we did not find any studies that supported an alternative model. It is important to note that in a saturated model, there is no need to examine a model fit as the default and the saturated model are the same (Arbuckle and Wothke, 2004). The saturated model (all paths are examined), contained two psychological predictors (individual resilience and well-being, controlling for each other) and seven demographic characteristics which predicted two of the COVID-19 effects (sense of danger and distress symptoms, controlling for each other). In the first step, the model was examined separately for each of the two samples using group analysis (Amos option for analysis, which makes it possible to compare two groups belonging to the same sample). Results indicated very similar path analyses with a single difference between them, regarding the path between family income and a sense of danger which was significant for the first model (p = .005) but only nearly significant for the second model (p = .06). Based on these very close results, we decided to combine the two samples into a single mutual sample. Furthermore, to overcome the different measurements’ scales and the use of different types of measurements, (e.g., community size is an ordinal variable while gender is a categorical one), we used standardized scores in the path analysis.
3. Results
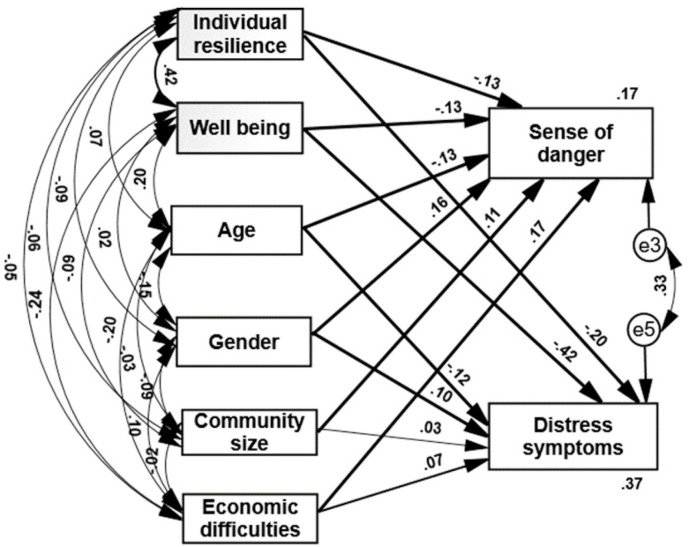
The path analysis of the combined sample indicated the following (see Fig. 1 ): (a) All paths were significant (p < .008 to .001) except for the path between family income and distress symptoms (p = .12). The seven predictors explained 20% of sense of danger variance and 34% the distress symptoms variance. (b) As expected, higher levels of individual resilience and well-being predicted lower reported sense of danger and distress symptoms. These results, regarding the psychological predictors, fully support our first hypothesis. (b) Older age predicted lower levels of sense of danger and distress symptoms. (c) Gender predicted the dependent variables as well: women reported a higher level of sense of danger and distress symptoms, compared to men. (d) Larger sizes of the community predicted higher levels of sense of danger and distress symptoms. (e) Greater economic difficulty due to the COVID-19 pandemic predicted higher levels of sense of danger and distress symptoms. (f) Lower family income, relative to the average family income in Israel, predicted higher levels of sense of danger, but did not significantly predict distress symptoms. These results, regarding the demographic characteristics, almost fully supported our second hypothesis, according to which the demographic characteristics will add significantly to the prediction of sense of danger and distress symptoms. (g) To examine our third hypothesis, we ran separately the two psychological characteristics (individual resilience and well-being) and the four-demographic characteristics. The psychological variables explained 8% of the sense of danger variability and 33% of the distress symptoms variability. The four-demographic variable explained 13% of the sense of danger variability and 10% of the distress symptoms variability. These results supported our hypothesis regarding the distress symptoms but not regarding the sense of danger.
Fig. 1.
Path analysis of psychological and demographic variables predicting sense of danger and distress symptoms. Note. Only one path is not statistically significant: community size to distress symptoms; all other paths (bold and thick) are significant (p < 001).
To examine our research question regarding the contribution of community and national resilience as predictors of sense of danger and distress symptoms, these variables were added to the described model. The results of this path analysis indicated the following: Community and national resilience did not add significantly to the explained variance of both the sense of danger and distress symptoms, compared with the model in which they were not included: The eight predictors explained almost the same percentage of variance: 18% of the sense of danger variance and 37% of the distress symptoms variance.
Finally, and to better understand the associations among all nine variables examined in this study, we have calculated the correlations among the nine predictors and the two predicted variables were calculated (Note: Table 2 ). Results indicated the following: (a) Individual, community and well-being significantly and negatively correlated with sense of danger and distress symptom: The higher the resilience, the lower level of distress. National resilience significantly and negatively correlated with distress symptoms, but not with sense of danger. (b) Age and family income significantly and negatively correlated with sense of danger and distress symptoms: The older the age and the higher the family income, the lower level of distress. And (c), gender and economic difficulties due the COVID-19 pandemic significantly and positively correlated with distress: Being a woman and having more economic difficulties, correlated with higher levels of distress symptoms and sense of danger.
Table 2.
Correlations of psychological and demographic characteristics with a sense of danger and distress symptoms (N = 1346).
| Variable | Sense of danger | Distress symptom |
|---|---|---|
| 1. Individual resilience | -.220*** | -.398*** |
| 2. Well-being | -.255*** | -.5544*** |
| 3. Community resilience | -.117*** | -.176*** |
| 4. National resilience | .018 | -.130*** |
| 5. Age | -.227*** | -.248*** |
| 6. Gender | .192*** | .130*** |
| 7. Community size | .117*** | .069** |
| 8. Economic difficulties | .244*** | .214*** |
| 9. Family income | -.158*** | -.110*** |
**p < .01, ***p < .001.
4. Discussion
The present study aimed to examine the extent to which individual resilience, well-being, and demographic characteristics predict outcomes of the COVID-19 pandemic: a sense of danger and distress symptoms. Based on earlier studies regarding security threats (e.g., Kimhi et al., 2020), we hypothesized that the two individual psychological characteristics will predict these indicators of anxiety and better than several demographic characteristics. However, since none of the previous studies examined resilience due to the health pandemic, this assumption had to be empirically tested.
Our current findings showed similarities to resilience research due to security threats (Eshel et al., 2020) and/or natural disasters (Cutter et al., 2008). However, these findings also specify differences form former research, indicating a possible uniqueness of resilience due to health crises, such as the COVID-19. For example, individual resilience and well-being are much better predictors of coping with the threat in the current study, compared with national and community resilience, which were more predictive in former studies. Most importantly, community and national resilience did not add to the prediction of a sense of danger and distress symptoms in the current study. A possible explanation for this finding may be that the threat of the COVID-19 is first and foremost a health threat to the individual, and as such, dealing with it is more personal and much less social or national. Support for this account can be found in the fact that both community and national resilience were found to be negatively correlated with the predictor variables, but when added to the path analysis equation (along with individual resilience and well-being) they hardly changed their prediction. This explanation needs further research support.
The results of this study are consistent with previous studies that indicate the validity of resilience measures in dealing with threats and crises of various types (Cutter et al., 2008; Suedfeld, 2015). In other words, types of resilience serve as good indicators of people's ability to deal with crises and threats of various kinds. The results of this study also support previous research that examined coping with the threat of corona (e.g., Nair, et al., 2020) and indicated the importance of individual resilience and well-being as predictors of successful coping with the COVID-19 pandemic (Shanahan et al., 2020).
The findings of this study are also consistent with previous studies that examined demographic characteristics as predictors of resilience and stress: age (Masten, 2002), gender (Kimhi and Eshel, 2016), community size (Koziara et al., 2019), and economic status (Martini, 2020). In this respect, it seems that the demographic predictors of different threats are similar beyond the specific type of threat.
4.1. Limitations
Two main limitations deserve mentioning: First, this study is a correlational study that does not allow causality inferences. We thus must be cautious in the interpretation of the findings. Second, our study is based on an internet sample, and there is no guarantee that it is a representative sample, even though the sample is large and includes a wide distribution of demographic variables. We recommend that a similar study be conducted among a representative sample of the population utilizing alternate methodologies, and subsequently, the findings will be compared to ensure validity. Furthermore, we recommend that a similar study be carried out in additional societies, so that a multi-cultural comparison be made.
5. Conclusions
This study focused on the investigation of factors that may predict distress symptoms and sense of danger, including resilience, wellbeing and demographic characteristics. The main conclusion of this study is that the first and foremost predictors of COVID-19 anxiety are individual resilience and well-being. Community and national resilience were not found to be significant predictors of both a sense of danger or distress symptoms. Though both predictors that were found are complex and may be influenced by many factors, given the potential return of COVID-19 threat and other future health pandemic threats to our world, we must rethink and develop ways to reinforce them.
Author statement
All four researchers (Shaul Kimhi, Hadas Marciano, Yohanan Eshel, and Bruria Adini) have contributed equally to this article
References
- Alarcón R., Cerezo M.V., Hevilla S., Blanca M.J. Psychometric properties of the Connor-Davidson Resilience Scale in women with breast cancer. Int. J. Clin. Health Psychol. 2020;20(1):81–89. doi: 10.1016/j.ijchp.2019.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonovsky A. The structure and properties of the sense of coherence scale. Soc. Sci. Med. 1993;36(6):725–733. doi: 10.1016/0277-9536(93)90033-z. [DOI] [PubMed] [Google Scholar]
- APA.org . 2014. The Road to Resilience.http://www.apa.org/helpcenter/road-resilience.aspx [Google Scholar]
- Arbuckle J.L. SPSS Inc; Chicago, IL: 2011. Amos 20 User's Guide. [Google Scholar]
- Arbuckle J, Wothke W. Structural equation modeling using AMOS: An Introduction. Small Waters; Chicago: 2004. [Google Scholar]
- Ben-Dor G., Pedahzur A., Canetti-Nisim D., Zaidise E. The role of public opinion in Israel's national security. Am. Jewish Congress: Congr. Mon. 2002;69(5):13–15. [Google Scholar]
- Bonanno G.A. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am. Psychol. 2004;59(1):20. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- Bonanno G.A., Romero S.S., Klein S.I. The temporal elements of psychological resilience: an integrative framework for the study of individuals, families, and communities. Psychol. Inq. 2015;26(2):139–169. [Google Scholar]
- Branson V., Palmer E., Dry M.J., Turnbull D. A holistic understanding of the effect of stress on adolescent well‐being: a conditional process analysis. Stress Health. 2019;35(5):626–641. doi: 10.1002/smi.2896. [DOI] [PubMed] [Google Scholar]
- Braun-Lewensohn O., Al-Sayed K. Syrian adolescent refugees: how do they cope during their stay in refugee camps? Front. Psychol. 2018;9:1258. doi: 10.3389/fpsyg.2018.01258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J.T., Reis H.T., Zautra A.J. Social resilience. Am. Psychol. 2011;66:43–51. doi: 10.1037/a0021419. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L., Stein M.B. Psychometric analysis and refinement of the connor–davidson resilience scale (CD-RISC): validation of a 10-item measure of resilience. J. Trauma Stress. 2007;20(6):1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- Cutter S.L., Barnes L., Berry M., Burton C., Evans E., Tate E., Webb J. A place-based model for understanding community resilience to natural disasters. Global Environ. Change. 2008;18(4):598–606. [Google Scholar]
- Derogatis L.R., Savitz K.L. The SCL-90-R and Brief symptom inventory (BSI) in primary care. In: Maruish M.E., editor. Handbook of Psychological Assessment in Primary Care Settings. Lawrence Erlbaum Associates; Mahwah, NJ: 2000. pp. 297–334. [Google Scholar]
- Eshel Y., Kimhi S. Determinants of individual resilience following missile attacks: a new perspective. Pers. Indiv. Differ. 2016;95:190–195. [Google Scholar]
- Eshel Y., Kimhi S., Marciano H. Proximal and distal determinants of community resilience under threats of terror. J. Community Psychol. 2019;47(8):1952–1960. doi: 10.1002/jcop.22245. [DOI] [PubMed] [Google Scholar]
- Eshel Yohanan, Kimhi Shaul, Marciano Hadas. Predictors of national and community resilience of Israeli border inhabitants threatened by war and terror. Community Ment. Health J. 2020:1–9. doi: 10.1007/s10597-020-00592-w. [DOI] [PubMed] [Google Scholar]
- Hadi F., Llabre M.M., Spitzer S. Gulf War-related trauma and psychological distress of Kuwaiti children and their mothers. J. Trauma Stress. 2006;19:653–662. doi: 10.1002/jts.20153. [DOI] [PubMed] [Google Scholar]
- Hernandez R, Bassett SM, Boughton SW, Schuette SA, Shiu EW, Moskowitz JT. Psychological well-being and physical health: Associations, mechanisms, and future directions. Emotion Rev. 2018;10(1):18–29. doi: 10.1177/1754073917697824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjemdal O., Vogel P.A., Solem S., Hagen K., Stiles T.C. The relationship between resilience and levels of anxiety, depression, and obsessive– compulsive symptoms in adolescents. Clin. Psychol. Psychother. 2011;18:314–321. doi: 10.1002/cpp.719. [DOI] [PubMed] [Google Scholar]
- Kimhi S., Eshel Y. Demographic characteristics and sense of danger predicting a new measure of individual resilience following a war. J. Community Med. Health Educ. 2016;6(5):472–480. [Google Scholar]
- Kimhi S., Shamai M. Community resilience and the impact of stress: adult response to Israel's withdrawal from Lebanon. J. Community Psychol. 2004;32:439–451. [Google Scholar]
- Kimhi S., Eshel Y. Individual and public resilience and coping with long term outcomes of war. J. Appl. Biobehav. Res. 2009;14:70–89. [Google Scholar]
- Kimhi S, Eshel Y. Measuring national resilience: A new short version of the scale. J. Commun. Resilience. 2019;47(3):517–528. doi: 10.1002/jcop.22135. [DOI] [PubMed] [Google Scholar]
- Kimhi S., Goroshit M., Eshel Y. Demographic variables as antecedents of Israeli community and national resilience. J. Community Psychol. 2013;41(5):631–643. doi: 10.1002/jcop.21561. [DOI] [Google Scholar]
- Kimhi S., Marciano H., Eshel Y., Adini B. Community and national resilience and their predictors in face of terror. Int. J. Disaster Risk Reduct. 2020:101746. [Google Scholar]
- Koziara K., Mijas M., Wycisk J., Pliczko M. vol. 31. Taylor & Francis LTD; : 2019. Perceived exposure to minority stress and health in transgender people–the mediating role of resilience. (International Journal of Sexual Health). A508-A508. [Google Scholar]
- Leykin D., Lahad M., Cohen O., Goldberg A., Aharonson-Daniel L. Conjoint community resiliency assessment measure-28/10 items (CCRAM28 & CCRAM10): a self-report tool for assessing community resilience. Am. J. Community Psychol. 2013;52:313–323. doi: 10.1007/s10464-013-9596-0. [DOI] [PubMed] [Google Scholar]
- Marciano H., Eshel Y., Kimhi S. Predictors of individual, community, and national resiliencies of Israeli jews and arabs. Int. J. Psychol. 2019 doi: 10.1002/ijop.12636. [DOI] [PubMed] [Google Scholar]
- Martini B. Resilience and economic structure. Are they related? Struct. Change Econ. Dynam. 2020 doi: 10.13140/RG.2.2.36530.76484. [DOI] [Google Scholar]
- Masten A.S. Resilience comes of age. Resili. Develop. 2002:281–296. (Springer, Boston, MA). [Google Scholar]
- Masten A.S. Resilience theory and research on children and families: past, present, and promise. J. Family Theory Rev. 2018;10:12–31. [Google Scholar]
- Nair N., Taylor Z.E., Evich C.D., Jones B.L. Relations of positive parenting, effortful control, and resilience in rural Midwestern Latinx early adolescents. Child. Youth Serv. Rev. 2020:105003. [Google Scholar]
- Patel S.S., Rogers M.B., Amlôt R., Rubin G.J. What do we mean by 'community resilience'? A systematic literature review of how it is defined in the literature. PLoS Curr. 2017;9:1–48. doi: 10.1371/currents.dis.db775aff25efc5ac4f0660ad9c9f7db2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott S.B., Poulin M.J., Cohen-Silver R. A lifespan perspective on terrorism: age differences in trajectories of response to 9/11. Dev. Psychol. 2012;49(5):986–998. doi: 10.1037/a0028916. [DOI] [PubMed] [Google Scholar]
- Shanahan L., Steinhoff A., Bechtiger L., Murray A.L., Nivette A., Hepp U. Emotional distress in young adults during the COVID-19 pandemic: evidence of risk and resilience from a longitudinal cohort study. Psychol. Med. 2020:1–10. doi: 10.1017/S003329172000241X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soffer-Dudek N. Sleep-related experiences longitudinally predict elevation in psychopathological distress in young adult Israelis exposed to terrorism. Pers. Indiv. Differ. 2016;100:131–139. [Google Scholar]
- Solomon Z., Prager E. Elderly Israeli holocaust survivors during the Persian Gulf War: a study of psychological distress. Am. J. Psychiatr. 1992;149:1707–1710. doi: 10.1176/ajp.149.12.1707. [DOI] [PubMed] [Google Scholar]
- Suedfeld P. Indomitability, resilience, and posttraumatic growth. In: Ajdukovic D., Kimhi S., Lahad M., editors. Resiliency: Enhancing Coping with Crisis and Terrorism. IOS Press. The NATO Science for Peace and Security Programme; Amsterdam: 2015. pp. 1–18. [Google Scholar]
- Turenne C.P., Gautier L., Degroote S., Guillard E., Chabrol F., Ridde V. Conceptual analysis of health systems resilience: a scoping review. Soc. Sci. Med. 2019;232:168–180. doi: 10.1016/j.socscimed.2019.04.020. [DOI] [PubMed] [Google Scholar]
- Vallejo M.A., Jordán C.M., Díaz M.I., Comeche M.I., Ortega J. Psychological assessment via the internet: a reliability and validity study of online (vs paper-and-pencil) versions of the General Health Questionnaire-28 (GHQ-28) and the Symptoms Check-List-90-Revised (SCL-90-R) J. Med. Internet Res. 2007;9(1):e2. doi: 10.2196/jmir.9.1.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. Jama. 2020;323(14):1341–1342. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; : 2020. Mental Health and Psychosocial Considerations during the COVID-19 Outbreak; p. 18. March 2020 (No. WHO/2019-nCoV/MentalHealth/2020.1) [Google Scholar]