Abstract
Objective
To review the evidence of the association between performance in eight indicators of diabetes care and a patient's race/ethnicity and socioeconomic characteristics.
Data Source
Studies of adult patients with type 2 diabetes in MEDLINE published between January 1, 2000, and December 31, 2018.
Study Design
Systematic review and meta‐analysis of regression‐based studies including race/ethnicity and income or education as explanatory variables. Meta‐analysis was used to quantify differences in performance associated with patient race/ethnicity or socioeconomic characteristics. The systematic review was used to identify potential mechanisms of disparities.
Data Collection
Two coauthors separately conducted abstract screening, study exclusions, data extraction, and scoring of retained studies. Estimates in retained studies were extracted and, where applicable, were standardized and converted to odds ratios and standard errors.
Principal Findings
Performance in intermediate outcomes and process measures frequently exhibited differences by race/ethnicity even after adjustment for socioeconomic, lifestyle, and health factors. Meta‐analyses showed black patients had lower odds of HbA1c and blood pressure (BP) control (OR range: 0.67‐0.68, P < .05) but higher odds of receiving eye or foot examination (OR range: 1.22‐1.47, P < .05) relative to white patients. A high school degree or more was associated with higher odds of HbA1c control and receipt of eye examinations compared to patients without a degree. Meta‐analyses of income included a handful of studies and were inconsistently associated with diabetes care performance. Differences in diabetes performance appear to be related to access‐related factors such as uninsurance or lacking a usual source of care; food insecurity and trade‐offs at very low incomes; and lower adherence among younger and healthier diabetes patients.
Conclusions
Patient race/ethnicity and education were associated with differences in diabetes quality measures. Depending on the approach used to rate providers, not adjusting for these patient characteristics may penalize or reward providers based on the populations they serve.
Keywords: chronic disease, determinants of health, payment systems, quality of care/patient safety (measurement), racial/ethnic differences in health and health care, social determinants of health, systematic reviews/meta‐analyses
What this Study Adds.
Some studies of diabetes quality measures commonly used for public reporting or reimbursement have found differences in performance associated with patient race/ethnicity or socioeconomic characteristics.
This systematic review and meta‐analysis reviewed studies with regression adjustment for race/ethnicity, and income or education and quantified the magnitude of differences associated with these variables. Reviewed studies were also used to identify likely mechanisms underlying differences in diabetes quality associated with patient race/ethnicity, education, or income.
Racial/ethnic minorities tended to exhibit lower odds of HbA1c, blood pressure, or LDL control relative to white patients, but higher odds of receipt for process measures. Patients with a high school degree or more were more likely to have controlled HbA1c and have received eye examinations. Few studies measured income consistently, which was inconsistently associated with diabetes care performance.
Differences in diabetes care performance appear to be related to access‐related factors such as uninsurance or a usual source of care; food insecurity and trade‐offs at low incomes; and patient behavior associated with age and health status with younger and healthier patients being less likely to adhere to recommended care.
1. INTRODUCTION
Clinical diabetes measures such as those used in the Health Effectiveness Data and Information Set are widely used for quality reporting and reimbursement to align provider incentives with value in both the public and private sectors. 1 , 2 , 3 , 4 Ideally, measures of provider quality reflect differences in effectiveness, safety, and timeliness of health services between providers, and minimize the influence of patient behavioral factors, illness severity, or socioeconomic characteristics. However, studies have consistently found lower performance in quality measures for some minorities and patients in vulnerable socioeconomic strata. 5 , 6 , 7 , 8 , 9 , 10 This suggests payment arrangements relying on quality reporting may punish providers delivering care for larger numbers of vulnerable patients, who may be disproportionately more likely to have diabetes and other chronic conditions. 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18
While there is growing recognition that sociodemographic factors are related to quality differences, the size of these effects is less certain because methods for measuring and analyzing sociodemographic factors vary across studies and metrics used to measure quality may differ in their sensitivity to patient sociodemographics. 14 Diabetes process measures reflect care delivered directly by providers to patients, whereas intermediate outcomes such as hemoglobin A1c control may be more sensitive to patient behavior and sociodemographic differences. The association between sociodemographic factors and observed quality may vary by quality measure, the context in which care is delivered, assay method used for intermediate outcomes, data collection, and sampling approaches, as well as methods used to analyze data. A recent Report to Congress called for greater inquiry into factors mediating associations between quality measures and patient sociodemographic characteristics to inform methods for patient case mix adjustment. 14
We conducted a systematic review and meta‐analysis to assess the evidence underlying the magnitude of differences in diabetes care related to patient race/ethnicity, education, and income. We studied diabetes process and intermediate outcomes to understand the sensitivity of both types of measures to differences in sociodemographic patient mix. Socioeconomic status (SES) differences were operationalized as patient educational attainment and income level controlling for insurance status, since these variables are correlated with socioeconomic advancement. The study aimed to answer the following research questions: (a) What does the literature suggest about the mechanisms underlying differences in diabetes quality by race/ethnicity, and education or income? and (b) What is the magnitude of differences in diabetes care associated with race/ethnicity, and education or income?
2. METHODS
2.1. Systematic review design and study selection
Eight diabetes measures used by major regulatory or accrediting bodies such as the National Committee for Quality Assurance or the Centers for Medicare & Medicaid Services (CMS) were selected because of the well‐established connection between these quality measures and patient outcomes. Five are process measures (dilated eye examination rate, foot examination testing rate, low‐density lipoprotein (LDL) cholesterol testing rate, hemoglobin A1c (HbA1c) testing rate, nephropathy screening rate), and three are intermediate outcomes (HbA1c control, blood pressure (BP) control, LDL cholesterol control).
Searches of the MEDLINE database were used to identify peer‐reviewed studies with one or more of the selected diabetes measures as study outcomes and that examined the role of race/ethnicity with income or education on diabetes care. The review also included regression‐based studies examining mechanisms of disparities in diabetes care related to patient race/ethnicity, income, or education. English language articles published between January 1, 2000, and December 31, 2018, that met these criteria were retained. Search terms used to query the MEDLINE database are listed in Appendix S1. Results from MEDLINE searches were supplemented with studies mined from references.
All retained articles were required to be original research focusing on type 2 adult diabetic populations conducted in an Organization for Economic Co‐Operation and Development (OECD) country. Studies were retained if they examined the relationship between patient sociodemographics and diabetes quality using a multiple regression model with diabetes quality as an outcome and explanatory variables for race/ethnicity, with income or education. Studies were considered as including a measure of income if their analyses included income as dollar‐denominated variables, income‐to‐federal poverty threshold ratio, Townsend score, deprivation index, social class index, income quantiles, food stamp receipt, or dual eligibility status. Studies were also required to account for a patient's health insurance status. Studies including insured and uninsured patients in their samples were retained if they included insurance status as a regression covariate. Studies not including insurance status as a covariate were retained if the sample was entirely composed of insured individuals.
Our review targeted studies examining the relationship between sociodemographics and quality among type 2 diabetes patients using regression modeling as well as studies elucidating mechanisms related to disparities. Studies with samples not primarily composed of patients with type 2 diabetes or that analyzed data using simple bivariate approaches were excluded. Also, studies examining the level of intermediate outcomes without an explicit aim and design to investigate mechanisms or variables mediating the relationship between diabetes quality and the selected patient sociodemographic variables were excluded. We also excluded studies of interventions to improve patient self‐management of diabetes, health literacy, or care management interventions which could attenuate differences in receipt of care or control related to educational or health literacy differences among patients.
2.2. Scoring, data extraction, and standardization
Studies retained in the review were scored to assess strength of study design and measurement approach. The New Castle Ottawa scale was adapted to rate internal and external validity of design and the data used to measure patient race/ethnicity and SES‐related factors (Appendix S2). Two coauthors independently scored each study for risk of bias, and the study's score was taken as the average of both coauthors’ scores. Scores ranged from 0 to 6 with a score of 6 indicating both reviewers rated the study as meeting all assessment criteria for strength of study design.
Data extracted from each retained study included study reference, target population and exclusion criteria, study design, quality measures, sample size, results, and where applicable, regression estimate, and standard error. Extracted elements underwent dual review to confirm accuracy. Studies varied in the type of estimate (eg, odds ratio or fitted percentage) used to quantify disparities in quality, how diabetes outcome measures were coded, and the reference categories used for race/ethnicity, income, and education.
Because of these differences, several steps were taken to standardize extracted elements to improve comparability across studies. First, wherever possible, estimates reported in studies were used to calculate odds ratios and standard errors (SEs). Results reported as fitted percentages were converted to odds ratios. If a study did not report any SE data (eg, by only reporting p‐values for example), we used patient counts and the bivariate logistic formula to calculate SEs for extracted odds ratios. To assess whether this approach might over‐ or understate odds ratio SEs, we compared 95% confidence intervals (Cis) from logistic regression against 95% CIs using the bivariate formula using simulated data and examined results across 500‐10,000 iterations (see Appendix S6). SEs calculated using the bivariate logistic formula were smaller than SEs from logistic regression by approximately 9.5 to 10 percent. Therefore, we inflated SEs by 10 percent wherever patient counts were used and reported the inflated odds ratio SEs in our results.
Second, outcomes were sometimes modeled as gaps in diabetes care for process measures or poor control for intermediate outcomes. Where this occurred, the inverse of the odds ratio was taken to obtain the odds ratio reflecting controlled outcomes or receipt of care. Third, where derived odds ratios were calculated from predicted percentages, we calculated the odds ratio using a consistent reference category where possible to maximize the number of studies included in the meta‐analysis. For race/ethnicity, white diabetes patients were used as the reference. For education, individuals with less than a high school (HS) education (<HS) were used as the reference. For income, diabetes patients with incomes below the federal poverty level (FPL) were used as the reference category.
2.3. Systematic review and meta‐analysis
For the systematic review, the results and findings of each study were reviewed and summarized to identify key themes or patterns in the association between our sociodemographic variables and diabetes care. Key themes from the systematic review were summarized and reviewed to identify potentially important variables mediating sociodemographic disparities in diabetes care. Studies varied in the extent to which covariates for patient demographics, health status, case severity, comorbid conditions, access differences, and lifestyle were used. These included variables such as availability of a usual source of care; diet, exercise, and lifestyle behaviors; obesity or body mass index (BMI); adjustment for related conditions; and diabetes duration and treatment type. We summarize variables used in studies retained in the review in our discussion of the literature and, where possible, examined differences in effects for some covariates compared with race/ethnicity, income, or education.
DerSimonian‐Laird random effect (RE) meta‐analyses were used to combine extracted odds ratios from studies with usable estimates for race/ethnicity and SES characteristics. This approach assumes each study's estimate is drawn from a different distribution. 19 We viewed this as a more tenable assumption since estimates may vary because of sampling approach, empirical model, covariates, context, and other factors.
Although there is no consensus in the literature for how studies should be selected, we used the following approach when including studies in meta‐analyses. 20 First, odds ratios for a sociodemographic variable such as black or ≥HS education were only combined when both the variable and its reference group were consistently measured across estimates. Second, we sought to use estimates from samples that are more likely to reflect the general population of a country. This approach was chosen so that odds ratios would be more likely to reflect differences in the general population rather than differences that might prevail in a specific segment of the population (eg, income differences in diabetes care among low‐income Asians). We consequently excluded studies using samples predominantly composed of specific population subgroups such as elderly/near‐elderly patients or low‐income Hispanics. STATA version 16 was used to estimate meta‐analytic estimates.
We examined estimates of studies retained for meta‐analysis and conducted checks of the robustness of our meta‐analysis results. 20 Studies differed by whether uninsured patients were included in samples. We investigated whether this difference was related to differences in odds ratios by comparing estimates of studies containing only insured patients against results from studies including insured and uninsured patients. To examine whether our results were potentially influenced by publication bias, we used the trim‐and‐fill procedure to assess the robustness of our meta‐analysis results (Figure 1). 21
Figure 1.
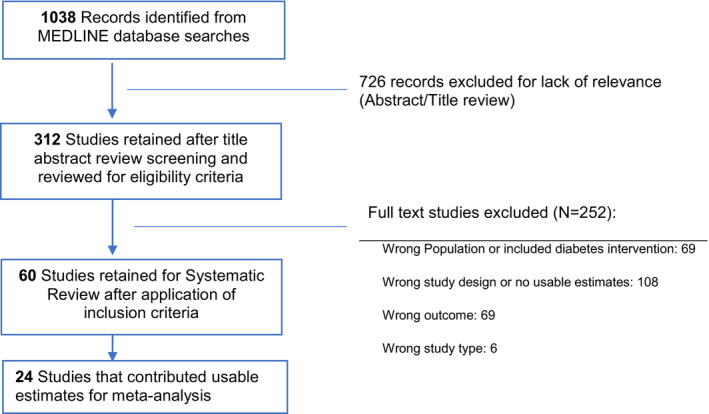
PRISMA flowchart of articles identified and retained for the systematic review and meta‐analysis [Colour figure can be viewed at wileyonlinelibrary.com]
3. RESULTS
3.1. General characteristics of studies for the systematic review
Table 1 presents characteristics of each of the 60 articles retained in the systematic review by extracted characteristics and the assigned article quality score. Regression models of diabetes measures varied in the types of covariates used to adjust for patient characteristics such as clinical conditions, access to care, behavioral conditions, and health status differences as well as characteristics of the area where a patient resides. Among the 60 studies, about half (N = 29) controlled for type of diabetes treatment (insulin, diet and exercise only, diabetes medications), 34 adjusted for self‐reported health status or comorbidity, and 19 included a measure reflecting regular access, usual source of care, or utilization. Studies also varied in whether they controlled for length of time an individual had diabetes (N = 27), body mass index (BMI) (N = 23), and diet, exercise, and self‐management behaviors (N = 18). Among articles retained for the systematic review, 12 used samples composed predominantly of a specific subpopulation such as low‐income Hispanic patients (N = 5), elderly or near‐elderly (N = 5), or low‐income black patients (N = 1) and were excluded from meta‐analyses.
Table 1.
Systematic review of articles examining diabetes care indicators against patient race and socioeconomic status (Complete references for the list of studies in Table 1 can be found in references 5, 7, 8, 9, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80)
| No. | Study | Target population (study sample size) | Diabetes indicators a with estimates reported in paper | Care setting, Location (data source) | Study covariates | Summary of results | Score |
|---|---|---|---|---|---|---|---|
| 1 | Al Sayah et al (2015) | Patients in the sample were from 2 primary care clinics in South Carolina if aged 18+ y with a DX of type 2 diabetes in their medical record, a clinic appointment between June and Aug 2010, and consented to participate in the study. Patients were excluded if they did not speak English or if research assistants determined they were too ill or cognitively impaired to participate (N = 343) | HbA1c < 7%; systolic BP < 130 | Two primary care clinics in South Carolina (survey and clinic records 2010) | Logistic regressions were used to explain control in intermediate outcomes. Model adjusted for age, sex, race/ethnicity, years of education, annual income, diabetes self‐efficacy, diabetes self‐management, employment, insurance status, health literacy, and depressive symptoms | Study examined the association between health literacy and intermediate outcomes in a low‐income predominantly African American patient population. Health literacy is not consistently related to HbA1c control or systolic blood pressure control. The authors concluded inadequate health literacy was modestly associated with being less informed about self‐management of diabetes, weakly associated with lower self‐efficacy, and weakly associated with worse depressive symptoms | 3/6 |
| 2 | Ali et al (2012) | Nonpregnant diabetes patients aged ≥ 18 self‐reporting a diabetes DX (N = 1350) | HbA1c > 9% | Ambulatory care setting using a national survey (NHANES 2007‐2010) | Race; education; income; demographic variables; ins status; ambulatory utilization; usual source of care; diabetes treatment type; and clinical comorbidities | This study examined the demographic, SES, clinical, and access‐related patient characteristics associated with poor HbA1c control. Compared to white patients, black patients had significantly higher adjusted odds of poor HbA1c control (7.9%, P < .05), but rates for Hispanic patients did not differ from white patients. Poor HbA1c control did not differ significantly by education level or income level. Rates of poor HbA1c control were lower among adults aged ≥ 65 y relative to young/middle‐aged adults (18‐64); among married vs. nonmarried individuals; among patients not using medications compared with patients on insulin therapy only or insulin with other oral glucose‐lowering medications. Poor control was higher among uninsured patients compared with non‐Medicare public insurance, Medicare, and private insurance | 5/6 |
| 3 | Azam et al (2015) | Patients with diabetes, 18‐75 y, diagnosed before May 2012 from 96 primary care practices in London boroughs (Lambest, Southwark, and Lewisham). Patients were excluded if temporary residents; type 1 diabetes; severe mental illness (dementia, bipolar disorder, substance dependence, and personality disorder); severe advanced diabetes complications (registered blind, dialysis, above knee amputation); and not fluent in English (N = 1488) | Not applicable | Ambulatory care setting, 96 primary care practices in London boroughs of Lambest, Southwark, and Lewisham (clinical records and standardized interview data) | Descriptive cross‐sectional analysis: age, gender, and self‐reported ethnicity, date of diabetes diagnosis, HbA1c at diagnosis, macrovascular complications (myocardial infarction (MI), stroke/cerebrovascular accident (CVA)), BMI, BP, foot examination, sensory neuropathy, retinopathy status, lipid profile, microalbuminuria, and medication status (oral hypoglycemic, insulin, both) Logistic regression relating patient characteristics against HbA1c < 6.5% or ≥ 6.5%: age at diagnosis, ethnicity, gender, DX BMI, BP, and lipid profile | Study objective was to compare patient status 1 y after T2D diagnosis between patients diagnosed using solely HbA1c ≥ 6.5% against those with HbA1c < 6.5%. Logistic regressions showed race (black, South Asian/other), age at DX, and triglyceride levels at DX significantly predicted diabetes DX with HbA1c < 6.5% or ≥ 6.5%. At 1‐y follow‐up after DX, patients with HbA1c < 6.5% had significantly lower (in %s) use of hypoglycemic medications, lower microalbuminuria, higher smoking, and higher MIs. Using the HbA1c ≥ 6.5% threshold solely to diagnose diabetes would have resulted in nearly a quarter of the sample being categorized as not having diabetes | 4/6 |
| 4 | Badedi et al (2016) | Random sample using stratified clustering at the health center level among patients with type 2 diabetes registered in primary care center registries (N = 288) | HbA1c control (<7%) | Jazan city, Saudi Arabia (survey with structured interview) | Models were estimated for clusters of variables such as physical health, depression, and stressful life events | Factors associated with poor glycemic control included a lack of education, polypharmacy, duration of diabetes ≥ 7 y, patients who were smokers or divorced, patients reporting depression or stress, and patients who did not comply with diet or take their medications as prescribed. The study found lower HbA1c levels among patients who received family support or had close relationship with their physicians, patients who were knowledgeable about diabetes, or those with greater confidence in ability to manage self‐care behaviors | 3.5/6 |
| 5 | Betancourt et al (2013) | Surveyed patients in UPENN health system EMR aged 18+ y with 1 + code for diabetes type 2 HbA1c test result who responded to survey during January 2011 to December 2011. Patients without a telephone number, not self‐identifying with diabetes mellitus, not speaking English, hospitalized, or in long‐term institutionalization were excluded (N = 332) | HbA1c < 8% | Ambulatory setting in urban university health system (UPENN health system EMR and survey 2011) | Study models included age; gender; education(<HS, some college, college,>college); insurance (private, Medicare, dual, Medicaid); income ($0‐$9 K, 10 K‐19 K, 20 K‐69 K, >70 K); employment (working, retired, unemployed, disabled); years w diabetes (0‐5, 6‐10, 11‐15,>15); # comorbidities (0‐1, 2‐3, ≥4); race (black, white, other); medications (diet/oral hypoglycemic, insulin, both); JCS coping (confrontive, emotive, evasive); diet temptations (social and internal, high caloric, negative emotional); trust in physicians; self‐reported medication adherence | This study examined self‐care behaviors, psychosocial stressors, and a patient's relationship with their physician in poor glucose control. Racial disparities in poor glucose control were hypothesized to be partially mediated by these and related psychosocial factors. Results showed that both dietary temptation and confrontive coping style were related to glucose control more generally, and these psychosocial factors did not explain racial disparities. Black‐white differences in glucose control (black race was associated with 2.43 OR for poor control) remained largely unchanged after adjusting for demographics, diabetes disease, dietary social temptations, confrontive coping style, and medication adherence. Models included an interaction term between black race and confrontive coping style. Patient‐reported relationship with physician was not related to glucose control | 4.5 |
| 6 | Brown et al (2005) | Diabetes patients aged 18+ and enrolled in 1 of 11 managed care plans for ≥ 18 mo with 1+ claims. Nursing home residents, pregnant women, and patients unable to provide informed consent or missing race/SES data were excluded (N = 7456) | HbA1c test; lipid profile; nephropathy test; dilated eye examination; foot examination; BP ≥ 140/90; LDL cholesterol ≥ 130 mg/dL; HbA1c ≥ 8% | Managed care ambulatory care clinics, CA, HI, MI, NJ, PA, TX (multi‐state TRIAD survey across 11 managed care plans collected between 7/2000 and 8/2001) | Cross‐sectional hierarchical regression models adjusted for age; gender; education; income; health status; mental health status; type of treatment; comorbid conditions; and duration of diabetes | Objective of the study was to examine racial/ethnic and sociodemographic variation in diabetes care in managed care settings. Compared to white diabetes patients, black patients had 5%‐10% lower rates of HbA1c testing, lipid testing, and influenza vaccination, but similar rates for other measures. No meaningful differences in rates of adherence to recommended care or thresholds were found for Hispanic or Asian diabetes patients. Patients with < HS education were associated with lower eye examinations and higher %s of poor LDL control, but otherwise no differences by education were found. Attempts to manage BP, glucose, and LDL levels were more aggressive among lower income and less educated patients | 3/6 |
| 7 | Chatterji et al (2012) | Adults aged ≥ 20 with self‐reported diabetes DX with complete data for blood glucose, BP, lipids, and current smoking and sociodemographic variables (N = 2937) | HbA1c levels ≥ 7%; diastolic BP ≥ 130 or systolic ≥ 80; lipids ≥ 200 mg/dL in total cholesterol | Ambulatory care setting using a national survey (NHANES 1988‐1994, 1999‐2008) | Study accounted for age; gender; marital status; diabetes duration; obesity; BMI; access to routine care; health insurance type; survey year; comorbidities; education; and health insurance | Study examined racial/ethnic and education‐related disparities in improvement in cardiovascular risk factors for diabetes patients. For the 1999‐2008 period, black (OR = 1.52, P < .05) and Hispanic (OR = 1.53, P < .05) patients were significantly more likely to have poor HbA1c control than white patients, but did not differ in BP control. Patients with > HS education were significantly less likely to have poor HbA1c control (OR = 0.65, P < .05), poor BP control (OR = 0.65, P < .05), and less likely to smoke (OR = 0.63, P < .05) compared to patients with less than a HS education | 4.5/6 |
| 8 | Chen et al (2014) | Patients with type 2 diabetes in the outpatient clinic of the metabolism department providing written consent to participate were included. Patients with poor vision unable to see the questionnaire, cognitive problems, disabled due to cerebrovascular accident, or in poor physical condition were excluded. Recruitment occurred during August 2012 to December 2012 (N = 467) | HbA1c < 7% | Ambulatory setting at Chung Shan Medical University Hospital in Taiwan (clinic records 2012) | Logistic regression was used to model variables associated with adequacy of health literacy. Generalized estimating equations (GEE) were used to model HbA1c level. GEE models included age, gender, education, income, duration of diabetes, family history of diabetes, regiments for glycemic control, original and most recently measured HbA1c, BMI, diabetes‐related complications (peripheral neuropathy, retinopathy, renal failure, and macroangiopathy) and comorbidities (cardiovascular disease, hypertension and hyperlipidemia, cancers, stroke, others) | Study authors noted that patients with both adequate and marginal health literacy were able to demonstrate good HbA1c control. The analysis found that when demographic, clinical, and socioeconomic variables were added to model differences in HbA1c levels were no longer significant and suggest health literacy and socioeconomic characteristics may over adjust models. The authors noted the importance of instructional materials, health education, and care support from health care providers in assisting patients to achieve glycemic control, especially those with marginal or inadequate health literacy | 3/6 |
| 9 | Chen et al (2015) | Multicenter study in mainland China of T2DM patients in 26 outpatient medical centers between August 2010 and April 2012. Inclusion criteria were confirmed T2DM, aged ≥ 18 y, body mass index (BMI) over 18, and written informed consent. Patients with gestational diabetes mellitus, secondary diabetes (steroid‐induced, cystic fibrosis, hemochromatosis, and chronic pancreatitis), or type 1 diabetes were excluded (N = 9065) | HbA1c control (<7%) | Multicenter study including tertiary and community health centers (Health Records 2010‐2012) | Modeled poor HbA1c control using logistic regression with adjustment for age, gender, duration of diabetes, education, smoking, drinking, waist circumference, BMI, and hypertension | This study investigated the relationship between patient characteristics and HbA1c control in a Chinese mainland population with an emphasis on obesity as a growing problem among diabetes patients. The results show that higher educational attainment, higher age, and smaller waist circumference are associated with greater odds of HbA1c < 7%. Longer duration of diabetes was associated with lower odds of HbA1c control | 2/6 |
| 10 | Chew et al (2008) | Adults aged ≥ 18 with 2+ amb. Visits with DM dx during 24 mo period; or 1 or more inpatient stays/ED visit with DM dx. Excluded patients with only gestational diabetes dx or abnormal glucose tolerance (N = 14,822) | HbA1c level < 7%; HbA1c level > 9.5%; LDL cholesterol level < 100 mg/dL; LDL cholesterol level > 160 mg/dL | Grady Health System, Harborview Medical Center, Cambridge Health Alliance, Cook County Bureau of Health Services, LA State University Medical Center, Community Health Network (EMR system for hospitals in safety‐net hospital consortium) | Study adjusts receipt of appropriate care for age; gender; cohort year; and whether the patient was never; intermittently; or continually insured; race. Patient sample is drawn from a consortium of safety‐net hospitals | This study examines racial and SES disparities among diabetes patients treated in a safety‐net hospital consortium. The study's model found black (OR = 1.62, P < .05) and Hispanic patients (OR = 1.58, P < .05) were more likely to have poor HbA1c control. Models also found black (OR = 1.09, P < .05) and Asian patients (Or = 1.18, P < .05) were more likely to have poor LDL control defined as LDL levels > 160 mg/dL. Compared to patients without coverage, diabetes patients with continuous coverage had a reduced chance of poor HbA1c control (OR = 0.74, P < .05) and a lower chance of poor LDL control (OR = 0.83, P < .05). The omission of a usual source of care may have distorted results | 3/6 |
| 11 | Choi et al (2011) | Asian, Latino, and white adults aged ≥ 18 with type II diabetes (N = 3531) | HbA1c test; foot examination in last 12 mo; eye examination in last 12 mo | All settings, representative survey of CA state residents (2007 CHIS) | The study's models included controls for race; language proficiency (English proficient; limited English proficiency); age; sex; marital status; length of time in the United States; income; health insurance status; perceived health; comorbid conditions (high BP; heart disease; congestive heart failure); and diabetes treatment | This study examined disparities in diabetes care and management by ethnicity and English language proficiency. English proficient Latinos in the study had 10% fewer HbA1c checks per year compared with white patients (P < .05) but did not differ in terms of monthly glucose checks, feet examinations, or eye examinations. Latinos with limited English proficiency had 24% fewer HbA1c checks per year (P < .01), and 39% fewer glucose checks per month (P < .001) and no other differences. English proficient Asians did not differ from white patients in any of the four outcomes, but Asians with limited English proficiency had 54% fewer glucose checks per month and 40% fewer feet examinations per year than white patients | 2.5/6 |
| 12 | Crowley et al (2014) | Multisite randomized trial. All patients had type 2 diabetes and poor blood pressure control. Patients with impaired decision making (eg, dementia), pregnancy, and aged < 18 y or > 100 were excluded. Kaiser patients were also excluded if treated in hospital, nursing facility, hospice, or home care or had < 12 mo of an active drug benefit in prior year (N = 963) | HbA1c control (persistent poorly controlled defined as an uninterrupted HbA1c > 8% for 1 y) | Adherence and Intensification of Medications Trial made up of 16 primary care teams at 3 Veterans Affairs and 2 Kaiser Permanente medical centers | Age, sex, race/ethnicity (non‐white), education level (some college or more), marital status (divorced), age at DX, diabetes duration, income, insulin use, HbA1c level, BP level, LDL level, BP medication use, statin use, and self‐reported health, self‐reported medication adherence, refill gaps for BP and oral diabetes medications, patient activation, self‐efficacy, PACIC scale, health care satisfaction, number of HbA1c values, PCP visits, ER visits, and diabetes endocrinology visits | The study's objective was to explore factors related to persistent poorly controlled diabetes. Patients with persistently poorly controlled diabetes were younger, had been diagnosed with diabetes earlier, higher LDL, had insulin use, higher antihypertensive burden, and lower statin use relative to patients with well‐controlled diabetes | 3.5/6 |
| 13 | Davila et al (2011) | Adults aged 20+ with self‐reported diabetes with usable HbA1c data. Excluded pregnant patients and patients diagnosed before age 30 (N = 369) | HbA1c level ≥ 7% | Ambulatory care setting using a national survey (NHANES 1999‐2004) | Study adjusted for age; # of hours worked; education; insurance status; race; insulin use; employment; occupation type; BMI category; diabetes treatment types; duration; hypertension DX; history of cardiovascular disease; smoking status; alcohol use; physical activity | Working 41+ h per week was associated with higher risk of suboptimal HbA1c control (>7%) but no difference for poor control (>9%). Black patients had elevated risk of poor (OR = 3.08, 95% CI: 1.51‐7.81) and suboptimal (OR = 3.43, 95% CI: 1.51‐7.81) control compared with white patients. ORs for Hispanic (OR = 1.83, 95% CI: 0.61‐5.54) and Other race (OR = 1.52, 95% CI: 0.44‐5.25) patients were elevated but not significant. Compared to patients with less than a HS education, neither high school grads (OR = 0.98) nor patients with more than a HS education (OR = 0.65) were significantly different. However, patients with insurance were significantly less likely to have HbA1c > 9% (OR = 0.37, P < .05) than uninsured | 4/6 |
| 14 | DeVoe et al (2009) | Diabetic adults aged ≥ 18 with full data on insurance status (N = 6562) | A1C screening; LDL screening; BP check; foot check; eye check | Ambulatory care setting using a national survey (MEPS 2002‐2005) | Retrospective overlapping panel design using MEPS for 2002‐2005. Statistical analysis includes age; gender; race; employed; geographic region; MSA/non‐MSA; income; education; insurance status/USC; health status | The study's research aim was to examine the effects of health insurance and a usual source of care on diabetes care for adults with diabetes. The results find no significant differences for Hispanics or other races relative to white patients for HbA1c testing, LDL testing, and foot examinations. Non‐Hispanic and non‐white patients were more likely to receive eye examinations (OR = 1.24, P < .05). Patients with a HS education or more were less likely to receive a HbA1c test (OR = 0.76, P < .05), but otherwise no differences were found relative to patients with less than a HS education. Results for income indicated patients at or near the federal poverty level are significantly less likely to receive HbA1c test, LDL tests, and foot examinations (significant ORs ranged from 0.52 to 0.81) | 3.5/6 |
| 15 | Díaz‐Apodaca et al (2010) | Hispanic adults aged ≥ 18 living in the US‐Mexico border region during April 2001 to November 2002 (N = 424) | HbA1c level < 7.0%; foot examinations; eye examinations; self‐monitored glucose testing | Ambulatory care setting, the US‐Mexico border (cross‐sectional survey of residents near US‐Mexico border stratified by ethnicity and geographic location) | Models included sex; age; systolic BP; diastolic BP; BMI; whether foot examination done; whether eye examination done; diabetes treatment (oral hypoglycemic, insulin); self‐monitoring of blood glucose; # of visits to the doctor; insurance coverage status; and SES status (high, medium, low) | The study's objective was to assess quality of diabetes care provided to Hispanic diabetes patients living in the border region between the United States and Mexico. Descriptive data showed that compared with US Hispanic diabetes patients, patients residing on the Mexican side of the border exhibited significantly lower adherence to eye examinations (24.8% vs. 55.0%, P < .01), foot examinations (27% vs. 57%, P < .01), and self‐monitored blood glucose (17.8% vs. 56.3%, P < .01). Logistic regression model results suggest the odds of appropriate receipt of care and control of HbA1c are higher for Hispanics on the US side of border OR = 1.18 (95% CI: 0.72‐1.94), although the difference is not statistically significant | 3.5/6 |
| 16 | Gary et al (2008) | Adult diabetes patients aged 18+ in 1 of 11 health plans for 18+ mo, with 1+ claim, Spanish/ English‐speaking, receiving majority of diabetes care through plan. Excluded pregnant or institutionalized patients (N = 7830) | HbA1c < 7%; LDL < 100; BP < 130/80 | Ambulatory setting. Patients in managed care plans (TRIAD study data 7/2000‐8/2001) | Used cross‐sectional analysis with age; sex; race; education; income; Charlson index; duration of diabetes; smoking; physical activity; self‐monitored blood glucose; foot care; SF12 physical health score; SF12 mental health score; % in census tract living in poverty | This study's objective was to examine whether residential environment may influence health behaviors and outcomes in diabetes patients. In regression models of intermediate outcomes and select health behaviors, diabetes patients in the tertile that perceived the fewest neighborhood problems showed statistically significant increases in the probability of engaging in weekly physical activity, having controlled BP, and averaged slightly higher mental and physical health scores on the SF‐12. There were no statistically significant differences between diabetes patients by HbA1c control < 7%, LDL control < 100 mg/dL, or in terms of the average levels of these intermediate outcomes | 2.5/6 |
| 17 | Gregg et al (2010) | Continuously enrolled adults for at least 3 y, aged ≥ 18 in 1 of 11 managed care plans. Excluded patients who are pregnant or with probably type I diabetes (N = 8392) | HbA1c testing; lipid profile; urinary albumin; dilated eye examination; and foot examination | Managed care ambulatory care clinics, CA, HI, MI, NJ, PA, TX (TRIAD data at two time points: 7/2000 to 10/2001 and follow‐up from 4/2002 to 3/2003) | Generalized estimating equations with multiple imputation for patients missing medical chart data were used to predict gaps in care with age; sex; race/ethnicity; marital status; income; education; smoker; duration of diabetes; diabetes medication type; self‐rated health status; nonfinancial barriers to access; presence of CHD; and Charlson comorbidity index | This study examined the persistence of gaps in the delivery of standard diabetes care over a 3‐y period (2000‐2003). The results found that younger and healthier patients (aged 18‐44 with fewer comorbid conditions, shorter length of diabetes) were more likely to have gaps in care as were patients with lower income, smokers (vs. nonsmokers), and employed persons (vs. nonemployed or retired). Racial differences varied by measure with blacks being 15% more likely to miss lipid tests, black (10%) and Asian (11%) patients more likely to miss proteinuria tests, and whites (11%) more likely to miss eye examinations | 3.5/6 |
| 18 | Harris (2001b) | White, black, or Hispanic diabetic adults aged ≥ 25. Women with diabetes DX during pregnancy; subjects with type 1 diabetes mellitus (defined: <30 y old, with continuous insulin use) were excluded (N = 1480) | HbA1c level; urine albumin; BP; LDL cholesterol levels | Ambulatory care setting using a national survey (NHANES III 1988‐1994) | Models included variables controlling for household income; education; age; duration of diabetes; BMI; self‐management of diabetes; diabetes treatment types; race; insurance status; prior DX of hypertension or dyslipidemia; current treatment of hypertension or dyslipidemia if present | Study objective was to examine disparities in health care access, utilization, health status, and outcomes among diabetes patients by race and ethnicity and to examine whether outcomes are influenced by access and utilization. The authors conclude no association exists between SES and diabetes‐related outcomes (blood glucose control, hypertension control, lipid control, or albuminuria) in whites, blacks, or Mexicans, respectively. Mexicans with a high school education or more were twice as likely (OR = 2.1, 95% CI: 1.1‐4.1) to have normal albuminuria levels compared to patients with less than a high school education | 4/6 |
| 19 | Heisler et al (2003) | Observational study of Adult diabetes patients that had 2 or more ambulatory visits and 1 hospitalization who completed the Diabetes Quality Improvement Project survey from 21 VA facilities (ICD‐9). Randomly sampled 80 eligible patients in each facility (N = 916) | HbA1c test; dilated eye examination; foot examination; nephropathy screen in past 2 y; HbA1c level (≤9.5%); LDL level (<130 mg/dL); and BP (<140/90) | 21 Veterans Affairs facilities (Diabetes Quality Improvement Project Survey 1999‐2000) | Regression models included race; annual income; education; diabetes duration; medication/insulin use; diabetes comorbidities; total illness burden index; treatment type for diabetes; patient self‐management of diet; exercise; medications; glucose monitoring and foot care; percent of facility patients with 2+ outpatient visits in past year; percent of patients with 80%+ of care at VA facility; and facility‐level patient race mix | This study's objective was to assess racial disparities in quality of diabetes process and intermediate outcomes and treatment intensity. Study found no white‐black differences in receipt of HbA1c test or foot examinations, although blacks were less likely to receive LDL screens. Sensitivity analyses indicated lower eye examination rates for blacks were associated with their use of facilities with lower overall eye examination rates. Blacks were more likely to have poor LDL control (≥ 130 mg/dL) and poor BP control (BP ≥ 140/90 mmHg), although treatment intensity did not differ between blacks and whites | 4/6 |
| 20 | Heltberg et al (2017) | Random sample of Danish citizens aged 30 or over was sampled for a health survey. Subjects were recruited during January 2010 to October 2013. This study examined a subset of the surveyed population with type 2 diabetes (N = 907) | LDL > 2.5 mmol/L; HbA1c > 7.5% | Ambulatory care setting in Naestved municipality in Denmark (survey database) | Logistic regressions were used to identify factors associated with poor LDL control and poor HbA1c control. Covariates included gender; age; education (basic, vocational training, short academic, long academic); income; occupation type (working, welfare, retired); and marital status (married/cohabiting, living single) | This study investigated multiple outcomes to examine the role of socioeconomic factors and health in persons with diabetes. The authors conclude that middle age (46‐60 y), low education (basic schooling), and low income (<21.4 K Euros) are associated with nonattainment of diabetes management objectives such as controlled intermediate outcomes, physical activity, and smoking cessation. Education and income were not associated with significant differences in LDL > 100 mg/dL or HbA1c > 6.5% | 4/6 |
| 21 | Ibanez et al (2018) | All patients over 20 y of age registered in Atenea (Spain) with a diagnosis of type 2 diabetes on May 15, 2014, were included in this study. Patients less than 20 y, not found in the population register, or missing the educational variable were excluded (N = 32,638) | HbA1c level > 7%; blood pressure > 140/90 mmHg; LDL cholesterol level > 100 mg/dl | Ambulatory care setting (Primary Care EMR for Regional Health Service of Navarre & 2013 Population Register) | The authors used mixed‐effect logistic regressions to examine the relationship between educational level and control of intermediate outcomes. Models included age, sex, education, income, sex*education, sex*income, and basic health zone as a random effect | This study examined the relationship between education level and controlled intermediate outcomes in disproportionately low‐income diabetic population. Persons that are less educated were between 12% and 34% more likely to have uncontrolled HbA1c than university‐educated patients. Persons with income below 18 K Euros were 19% more likely to have HbA1c > 7% but were 10% less likely to have uncontrolled HbA1c than persons with income at or above 18 K Euros (P < .01). Persons with income below 18 K Euros composed 69% of the sample | 3.5/6 |
| 22 | James et al (2012) | Open cohort design with adult type 2 diabetes patients aged 35 to 74 y prescribed at least 1 one or more prescriptions for diabetes during the period. Patients were drawn from area of high social deprivation (N = 24,111) | Mean HbA1c level; binary outcome = 1 if HbA1c ≤ 7.5% | All practices in primary care trusts of Tower Hamlets and |
Multilevel model with separate levels for year, patient, practice, and primary care trust. Covariates: patient age; patient gender; self‐reported ethnicity; Townsend score; BMI; smoking status; diabetes meds: metformin only; diabetes meds: combined oral; year indicator variables; ethnicity year interaction terms Newham in inner London (EMIS Web System Data 2004‐2009) |
Study objective was to examine whether type 2 diabetes patient ethnicity differences in HbA1c control changed over a five‐year period. This study found declines in the disparities between white, Black, and South Asian patients in mean HbA1c level over time and probability of HbA1c below 7.5%. SES was measured using the Townsend score, which was significantly associated with a 2% increase in HbA1c level for each unit increase in the Townsend. The interaction between ethnicity and Townsend score was not significant indicating declines in social deprivation were associated with similar effects across ethnic groups | 3.5/6 |
| 23 | Kim et al 2017 | Patients older than 19 who were diagnosed with diabetes or revealed to have diabetes by examination of the data were included (N = 1168 males and N = 1248 females) | HbA1c control (<7%) | 2007‐2014 Korea National Health and Nutrition Survey | Age, second‐hand smoke exposure, health insurance, date of diabetes diagnosis, medication therapy, tobacco use, days strength training, health status | Exposure to second‐hand smoke at home was revealed as a risk factor for poor glycemic control. Analysis showed a negative association of diabetes management with second‐hand smoke in both sexes, regardless of income status or healthy/unhealthy behaviors | 4/6 |
| 24 | Kirk et al (2011) | Adult diabetics at Winston‐Salem, NC, academic medicine clinic, only black/white (N = 669) | HbA1c < 7%; LDL cholesterol level; BP | Academic family medicine clinic, Winston‐Salem, NC (2006 Patient survey linked to medical chart) | Type 2 diabetes patients in academic family medicine clinic in Winston Salem, NC. Cross‐sectional logistic regression, with age; gender; income; education; insurance status; race; # of clinician visits; BMI; tobacco use; living alone or with others; weekly exercise level; diabetes education | This study's objective was to examine the relationship between patient characteristics and glycemic control among type 2 diabetes patients in an academic family medicine practice. Analysis of data for this academic family medicine clinic found that female patients (OR = 1.61, P < .05) and Medicare patients (OR = 2.16, P < .05) had a significantly higher odds of HbA1c control. No other variables were significantly associated with improved HbA1c control | 4/6 |
| 25 | Kollannoor‐Samuel et al (2011) | Low‐income Latino adults with type 2 diabetes, HbA1c ≥ 7%, age ≥ 21, with no medical conditions limiting physical mobility (N = 211) | HbA1c > 9.2% | Ambulatory care setting, Hartford county, CT (DIALBEST database December 2006‐February 2009) | Cross‐sectional design without a comparison group. Logistic regression controlled for age; gender; income; insurance status; education; and Latino ethnic groups, but no controls for case severity were included | This study's objective was to examine demographic, SES, cultural, and lifestyle characteristics associated with fasting blood glucose levels, and HbA1c control among type 2 diabetes patients in a clinical trial. Odds of HbA1c ≥ 9.2% were significantly higher for patients with incomes of $300/month or less compared to patients with>$500/month (OR = 10.4, P < .05), in age group 21‐44 relative to elderly (OR = 2.24, P < .05). Having medical insurance (OR = 0.31, P < .05) and daytime breaks for 30‐60 min (OR = 0.07, P < .05) were significantly associated with a lower odds of HbA1c ≥ 9.2% | 1/6 |
| 26 | Lopez et al (2016) | Residents of three Boston inner‐city areas, aged 30‐79 y (surveyed during March 2002‐June 2005). BACH is a multistage 1:1:1 stratified random sample of participants by gender and self‐identified race/ethnicity (black, Latino, white), and age. Overall sample includes both diabetic and nondiabetic patients, but a subanalysis examined acculturation on HbA1c < 7% among Latino patients with diabetes (N = 148) | HbA1c > 7% | Urban ambulatory care setting, Boston, MA (survey database) | Logistic regressions were used to examine how acculturation and health literacy were associated with HbA1c control among Latino patients with diabetes. Models included age, gender, education, health literacy, BMI, cholesterol level, presence of coronary disease, use of antihyperglycemic medication | This study sought to examine the role of acculturation of Latino patients with diabetes and HbA1c control. Sixty percent of the sample had low acculturation (measured using Bidimensional Acculturation Scale for Latinos), high illiteracy rates, and poor diabetes knowledge. Results showed acculturation was associated with low HbA1c control, possibly reflecting the high rates of illiteracy in the sample | 5/6 |
| 27 | Lynch et al (2014) | Patients with T2D attending 3 primary care clinics in southeastern United States, aged 18 or over, with a type 2 diabetes DX, willing to complete a survey and receiving care at one of the three clinics. Patients were ineligible if they did not speak English, were cognitively impaired, or too ill to participate during interactions with research assistants. Patients with type 1 diabetes or gestational diabetes were excluded. Recruitment occurred during May to August 2011 (N = 661) | HbA1c < 7%; BP < 130/80 mmHg; LDL cholesterol < 100 mg/dL | Primary care settings of Veterans Administration medical center in southeast United States (Clinic EMR and survey data May 2011‐Aug 2011) | Logistic regression was used to compare differences between Blacks and white patients with diabetes. Models included age, sex, education, employment, insurance, income, health status, and site | Study objective was to examine whether racial/ethnic differences in intermediate outcomes exist in large primary care clinic in the southeastern United States. The results show that non‐Hispanic blacks have lower odds of BP < 130/80 than non‐Hispanic white patients, but otherwise no difference exists for HbA1c or LDL control. Composite control for non‐Hispanic blacks was also notably lower than non‐Hispanic whites | 2.5/6 |
| 28 | Mainous et al (2007) | Adult diabetes patients aged ≥ 18 of Hispanic or non‐Hispanic white ethnicity from 42 of the 50 states (surveys were not collected in MA, RI, IL, MI, KS, NE, ND, OR, Guam, Puerto Rico, and Virgin Islands) (N = 20,588) | HbA1c test in past year; foot examination in past year; dilated eye examination in past year | Ambulatory care setting using a national survey (BRFSS 2004) | A cross‐sectional study design using logistic regression with sex; age; race; high school education; annual household income; language of interview; health insurance status; usual provider; whether a patient skipped doctor visits in prior 12 mo because of cost of care; and number of visits for diabetes in past 12 mo | This study's objective was to examine disparities in the quality of diabetes care provided to Hispanic and non‐Hispanic white diabetes patients. Even after adjusting for sociodemographic factors, language, utilization, and usual source of care, non‐Hispanic whites remained more likely to receive HbA1c tests, foot examinations, and perform tests of peripheral neuropathy. Insurance status and usual source of care may have a confounding influence on self‐monitoring of blood glucose. Using insulin, lower income, fewer physician visits, and Spanish language were associated with higher risk of not receiving a HbA1c test, lack of self‐monitoring blood glucose | 3/6 |
| 29 | Mainous III et al (2004) | Non‐Hispanic white and black adults aged 20+ y that participated in the adult examination and laboratory data file with either diabetes or hypertension (N = 20,588) | HbA1c level; HbA1c level < 8% (binary); systolic and diastolic BP; BP < 140/90 (binary) | Ambulatory care setting using a national survey (NHANES 1988‐1994) | Logistic regression controlled for age; sex; level of income; insurance coverage; level of education; self‐reported health; length of time with diabetes; BMI; usual source of care; number of times seen by a physician | This study's objective was to examine differences in control and management of diabetes patients among black and white diabetes patients residing in rural and urban areas. After adjusting for patient characteristics, blacks had a significantly higher risk of elevated hypertension irrespective of urban/rural location compared with white patients. Urban blacks did not differ from urban or rural whites in HbA1c control. Rural blacks had elevated diastolic and systolic BP relative to rural/urban whites, but BP control did not differ between rural and urban blacks. Differences in hypertension control between urban and rural residents were driven by significantly lower patient compliance to physician directions among rural black diabetes patients. Including patient SES variables in the model did not change disparities in HbA1c and BP control | 4/6 |
| 30 | Maneze et al (2016) | Patients 18+ y diagnosed with T2DM and HbA1c test present in last 2 y in clinical file, attending diabetes outpatient clinics at two centers in southwestern Sydney Australia recruited between May and December 2015 consenting to participate in study (N = 224) | Not applicable | Ambulatory care clinics in urban metropolitan setting (Clinic records 2015) | Logistic regression to identify correlates of diabetes self‐management and health literacy. Models included age, gender, education level, marital status, country of birth, self‐rated health stats, HbA1c > 7%, depression, confidence, knowledge, health literacy duration of diabetes diagnosis, BMI, medical comorbidities, and DSMQ‐16 scores | The aim of the study was to examine relationships between sociodemographic, clinical, and psychological factors and health literacy and its relationship with diabetes self‐management within a diverse population with T2D. A health literacy score of 10 or less was categorized as low. Patients with up to primary schooling were 212% (OR = 3.12) more likely to have low literacy, and patients with more than secondary schooling were 65% less likely (OR = 0.35) to have low literacy. Patients born overseas, experiencing depression symptoms, and HbA1c > 7% were more likely to have low literacy. Patients younger than age 60, with more than secondary schooling education, diabetes knowledge score < 7, or with depression symptoms were more likely to score low in diabetes self‐management. Higher health literacy alone was less important than diabetes‐specific knowledge for self‐management of diabetes | 2.5/6 |
| 31 | Mayer et al 2015 | Urban medical center EMR system was used to identify eligible patients aged 30 to 80 with at least one DX code for type 2 diabetes in the past year with a laboratory result for HbA1c in the prior 7 days. Selected patients were Medicaid or uninsured in a ZIP code with > 30% of population is below FPL. Excluded non‐English‐speaking patients (N = 407) | HbA1c control (>8%) | EMR records were used to survey participants of the UPenn Health System surveyed from June to December 2013 | Logistic regression for poor HbA1c control used age, sex, race/ethnicity, percentage of FPL, education level, food insecure, cost‐related medication nonadherence, foregone medical care; used emergency food programs, received SNAP, diet, employment status, number of occupants in household, insurance type, insulin use, BMI, and years with diabetes. (Select models included interactions between SNAP receipt and food insecurity.) | Food insecurity was associated with poor glucose control. Receipt of food assistance via the Supplemental Nutrition Assistance Program (SNAP) among food‐insecure individuals was associated with better diabetes control. Results showed greater intake of fruits and vegetables was associated with lower risk of poor HbA1c control. The authors note that the effect of fruit and vegetable intake on glucose control did not appear to differ between food secure and food‐insecure persons and suggest the lack of difference may reflect unmeasured differences or measurement error in their data | 2.5/6 |
| 32 | McCall et al (2004) | Diabetes patients aged 65‐74 residing in CO (N = 9,453) | Annual A1c; biennial ophthalmologic examinations and biennial lipid tests | Hospital and ambulatory setting in state of Colorado (Medicare claims in 1997‐1998 for CO residents) | Adjusted ORs were estimated via models including patient age; sex; race/ethnicity; rural/urban residence; Johns Hopkins ACG risk adjustment; # outpatient physician visits; # of endocrinologist visits; ED visits; number of hospitalizations; LOS; time from diabetes DX; and DE status | This study's objective was to compare the quality of diabetes care provided to dually eligible (DE) diabetes patients against care provided to non‐DE diabetes patients. Compared to non‐DE diabetes patients, urban and rural DE patients had a lower odds of receiving eye examinations and lipid tests. Rural DE patients had a lower odds of receiving HbA1c tests. Black race was associated with a lower odds of receiving an annual A1c test, lipid testing, and (all three measures together) relative to white patients. Compared to white patients, all minorities had a lower odds of receiving all three tests. The results indicate important differences in DE patients by urban/rural residence and use of endocrinologist visits | 4/6 |
| 33 | McElduff et al (2005) | South Asian (mostly Pakistani or Indian) and European adults aged 25‐74 in Blackburn, NW, UK (N = 9,453) | BP; total cholesterol; retinal screening; foot examination | Ambulatory setting, Blackburn, UK (Blackburn Diabetes Information System 1995‐2001) | The analysis used generalized linear models adjusted for age; sex; Townsend score; and ethnicity | This study's objective was to examine whether there are variations in intermediate outcomes by ethnicity after adjusting for SES characteristics. The authors found that adherence for process and intermediate outcomes of care were improving across all ethnicities between 1995 and 2001, although the level of control was lower for South Asian patients. White patients were more likely to be older, male, and to receive treatment for diabetes by diet alone. Adjustment for patient SES using the Townsend score or location where care was delivered produced minor changes in estimates of the association between ethnicity and outcomes, so the authors concluded that SES adjustment did not function as a confounding influence | 2/6 |
| 34 | McWilliams et al (2006) | White/Hispanic/ black diabetic adults aged 40‐85 with diabetes, hypertension, or coronary artery disease. Excluded Hispanics born outside United States. (diabetes N = 1733; hypertension N = 4521; coronary artery disease, diabetes, or stroke N = 2928) | BP < 140/90; HbA1c < 7%; total cholesterol < 200 mg/dL | Ambulatory care setting using a national survey (NHANES 1999‐2006) | The study used a repeated cross‐sectional data analysis, adjusting for age; sex; race; education; income; BMI; smoking status; and insurance status | This study's objective was to assess trends in control of BP, HbA1c, cholesterol level by race/ethnicity, education, and changes in the trend for patients aged 65 and above. Results found SES differences were generally smaller among adults < aged 65 compared with adults over age 65. The exception was BP differences between white and black patients with hypertension aged 40‐64 which were higher than differences for older adults. Higher education was associated with slightly lower but statistically significant BP differences for adults under and over age 65 | 4/6 |
| 35 | Moreno et al (2015) | Latino adults with diabetes 1) self‐identified as Latino; (2) speaking English or Spanish; (3) with current diagnosis of diabetes type 2; (4) 18 y of age or greater; and (5) with 1 primary care visit to the health center in the last 12 mo. Patients consenting to the study were retained. Conducted in a large migrant health care system providing safety‐net care in 2 rural CA counties (N = 250) | hemoglobin A1C <=8.0%; LDL cholesterol <=100 mg/dL; blood pressure <=140/90 mm Hg; eye examination; foot examination, HbA1c test, LDL C test, composite intermediate outcome measure; composite process measure | Safety‐net health system in rural, high agricultural area with high poverty (survey collected July 2009‐January 2010 linked to medical chart data) | Regression models for each outcome included age, sex, yearly household income for 2008, education, insurance coverage, general health status, body mass index, number of doctor visits in last 12 mo, insulin use, and years with diabetes | The aim of the study was to study the relationship between food insecurity, healthcare services, and diabetes care among Latinos with diabetes in a rural agricultural region. The results show that food insecurity is related to significantly lower control of diabetes intermediate outcomes (HbA1c < 8%, BP < 140/90, LDL < 100 mg/dL) and significantly lower receipt of many diabetes process care (eye examinations, foot examinations) as well as a substantially higher odds of foregoing recommended medications due to costs. The reference group used in the study were Latinos that were food secure | 3/6 |
| 36 | Nelson et al (2005) | Adult diabetes patients aged ≥ 18 with usable BRFSS data (N = 11,647) | Dilated eye examination in past year; foot examination in the past year; receipt of HbA1c test in past year | Ambulatory setting, national (BRFSS 2000) | Multivariate logistic regression controlling for race/ethnicity; annual income; gender; education; insulin use; and age | The study examined the association between type of health insurance coverage and quality of care for US diabetes patients. Uninsured patients were less likely to receive eye examinations (OR = 0.4, P < .05), foot examinations (OR = 0.5, P < .05), HbA1c tests (OR = 0.4, P < .05), and daily blood sugar checks (OR = 0.6, P < .05). Blacks were more likely to receive foot examinations (OR = 1.9, P < .05), HbA1c tests (OR = 2.0, P < .05), and diabetes education (OR = 1.5, P < .05). Hispanics were more likely to receive HbA1c tests (OR = 2.0, P < .05) but less likely to perform daily blood sugar checks (OR = 0.3, P < .05). Having less than a high school education was associated with being less likely to perform daily blood sugar checks (OR = 0.6, P < .05) and receive diabetes education (OR = 0.6, P < .05). Insulin users were more likely to receive all types of care | 1/6 |
| 37 | Nicholas et al (2011) | HRS diabetic respondents, age ≥ 50 (glycemic control N = 588) | A1C < 7%; A1C < 9% | Ambulatory care setting using a national survey (HRS 2003 Diabetes Survey, HRS 2006 in Person Diabetes Interview) | Food stamp recipients were compared against 1) never users and 2) persons that began or ceased food stamp use. Logistic regressions of HbA1c control included food stamp receipt; exercise; smoking status; HbA1c screening; cholesterol screening; retinopathy screening; Medicaid coverage, excellent/good self‐rated health; race; household income‐to‐poverty ratio; education status; marital status; gender | This study's research aim was to examine the relationship between participation in the US department of agriculture's food stamp program and Medicare costs, utilization, and glycemic control. The results do not find effects of the food stamp program on Medicare costs although food stamp receipt was associated with a 7 percentage point increase in inpatient hospitalizations and exercise was associated with 1.6 to 2 fewer physician visits. Differences were not found for outpatient utilization or ESRD status. Food stamp receipt was not associated with a significant or consistent pattern for HbA1c control either at the 7% or 9% threshold | 1/6 |
| 38 | Nowlin et al (2018) | Adults with and without type 2 diabetes aged 20+ at time of interview; self‐identifying as NHW, African American, Hispanic Mexican American, or another Hispanic group; with complete dietary data. Persons pregnant, with incomplete or unreliable 24 h data, or considered to have type 1 diabetes (T1D) (n = 32) were excluded. Subjects missing data on any covariate or main outcome were also excluded (n = 7850, 6562 with diabetes, 1288 without diabetes) | HbA1c level | Ambulatory care setting using national survey (NHANES 2007‐2010). | Used structural equation model (SEM) to examine the outcomes HbA1c level, C reactive protein (CRP), BMI, and Healthy Eating Index (HEI). HbA1c level is mediated by CRP, BMI, and HEI, and race/ethnicity has direct effects on HbA1c level and effects mediated via BMI, HEI, and CRP. Models were estimated separately for diabetes and nondiabetes patients. Covariates included age, gender, physical activity, education, income poverty ratio, smoking status, time in the United States | Used SEM to test whether disparities in HbA1c control occurring by race/ethnicity are mediated by nutrition and inflammation‐related differences measured by body mass, diet quality, and inflammation. The results did not find significant direct effects of race/ethnicity differences on HbA1c level among persons with diabetes over and above effects that may prevail via differences in BMI, diet quality, and CRP. Although the analysis suggests differences in HbA1c level occurring by race/ethnicity, may prevail for black, Hispanic diabetes patients relative to non‐Hispanic white patients | 4.5/6 |
| 39 | Nwasuruba et al (2009) | Adult diabetes patients aged ≥ 18 with self‐reported diabetes (N = 1,720) | A1C test in past year; foot examination in past year; dilated eye examination in past year | Ambulatory care setting (Texas BRFSS 2002‐2004). | Logistic regression including age; sex; race; marital status; employment status; education; income; diabetes education; insurance status; self‐rated health status; # of doctor visits; BMI; and insulin use | This study's objective was to examine racial/ethnic differences in self‐management and quality of care for diabetes patients in Texas during 2002‐2004. Only race results are reported. Non‐Hispanic black and Hispanic patients were more likely to receive foot examinations (non‐Hispanic black OR = 1.83, P < .05; Hispanic OR = 1.61, P < .05) but less likely to receive pneumonia shots (non‐Hispanic black OR = 0.58, P < .05; Hispanic OR = 0.54, P < .05) | 2.5/6 |
| 40 | Oladele et al (2006) | Patients with diabetes confirmed by a physician, age ≥ 35, of black, white, or Hispanic ethnicity. Excluded patients with unusable data for foot examinations, eye examinations, smoking cessation, and women with gestational diabetes (N = 23,434) | Eye examination; foot examination | Ambulatory care setting. National (BRFSS 1998‐2001) | Observational study of BRFSS 1998‐2001 using logistic regression including age; gender; race; insurance status, social class; duration of diabetes; and insulin use | The purpose of this study was to examine racial/ethnic differences in diabetes preventive practices after accounting for sociodemographic differences including social class. Black and Hispanic diabetes patients were associated with a lower odds of missing foot examinations and missing smoking cessation, respectively. Younger patients were significantly more likely to smoke and miss annual eye examinations, while lacking health insurance was associated with significantly higher odds of missing care and smoking (OR ranged from 1.3 to 2.1, all P < .05). Test of interacting race and social class variables was not significant | 2/6 |
| 41 | Ortiz et al (2015) | Data from the 2005, 2007, 2009, and 2011/2012 CHIS public use files were used to identify Mexican adults diagnosed with diabetes aged 35 y and above. The study's aim was to examine whether a Mexican adult's generational status is significantly related to receipt of diabetes process care (N = 3072) | Eye examination, foot examination, HbA1c test in the past year | Ambulatory care setting, sample representative of diabetes patients in the state of CA (CHIS 2005, 2007, 2009, 2011/2012) | Logistic regression was used to model diabetes processes and included generational status (first generation, second generation, 2.5 generation, third generation); age; sex; educational attainment; federal poverty income ratio; marital status; residence in rural area; employment status; English language proficiency; health insurance type, smoking; self‐perceived health status | The study's aim was to test whether generational status among Mexican Americans is associated with variations in diabetes processes of care. The results found that Mexican diabetes born of second or more generations following the first generation were less likely to receive eye examinations, foot examinations, and HbA1c tests. A significantly smaller proportion of first‐generation patients had a college degree or more and had higher poverty rates than other generations. First‐generation patients also tended to report worse health status than other generations | 4/6 |
| 42 | Paz et al (2006) | Noninstitutionalized, self‐identifying adult Latino or Mexican type 2 diabetes patients living near La Puente, CA, aged ≥ 40. Excluded patients diagnosed before age 30 (N = 821) | Eye examination, foot examination | Ambulatory care. (Participants in Los Angeles Latino Eye Study (LALES) 2004) | Cross‐sectional design, stepwise logistic regression with age; education < HS; income < $20 k; smoking status; health insurance; vision insurance; time since last physical ≥ 1 yr; self‐glucose test; ≥ 2 comorbidities; no usual clinical provider; diabetic nephropathy; glaucoma; hypertension; any visual impairment | The study's aim was to examine patient characteristics associated with noncompliance to American Diabetes Association (ADA) guidelines for vision care in an adult Latinos population with type 2 diabetes. The odds of not receiving an annual eye examination were higher for diabetes patients with less than a high school education (OR = 1.5, P < .05), without health insurance (OR = 2.5, P < .01), without a physical examination in the last 12 mo (OR = 1.8, P < .01), and with HbA1c 9% (OR = 1.7, P < .01) | 2.5/6 |
| 43 | Rawshani et al (2015) | Patients newly diagnosed with T2DM with 1+ entries in the Swedish National Diabetes Register (NDR) from 1/1/2002 to 12/31/2011 with T2DM DX reported at least 12 mo from date of DX were retained. Patients that did not meet this definition were retained if aged 40+ at DX and treated with diet only; diet with oral hypoglycemic agents (OHAs); or combo of OHAs and insulin (N = 131,935) | HbA1c < 7% during the second year after DX | Ambulatory care setting in Sweden (National Diabetes Register January 2002 to December 2011) | Mixed‐effects logistic regression was used to accommodate repeated observations in the data and estimate associations between HbA1c control and patient characteristics. Covariates included sex, race/ethnicity, smoker, education attainment, income quintiles, BMI, physical activity level, and glucose‐lowering treatment (diet, OHA, insulin, insulin + OHA) | This study examined ethnic disparities in glycemic control in Sweden during 2002‐2011. Results show ethnicity is associated with significant differences in HbA1c control and levels that are comparable in size with daily physical exercise | 3.5/6 |
| 44 | Saaddine et al (2002) | Retained adults aged 18‐75 with prior DX of diabetes from a physician and excluded women with gestational diabetes (BRFSS N = 3059, NHANES N = 1026) | Dilated eye examination; lipid test; foot examination; HbA1c > 9.5%; BP < 140/90; LDL < 130 mg/dL | Ambulatory care setting using a national survey (NHANES III 1988‐1994, BRFSS 1995) | Study design is cross‐sectional. Estimated logistic regressions with sex; age; race; education; annual household income; health insurance; insulin use; duration of diabetes | This study's objective was to document the quality of diabetes care provided in the United States during 1988‐1995. Results from logistic regressions found patients aged 65‐75 were more likely than patients aged 18‐44 to receive lipid testing, eye examinations, and controlled BP. Black patients were more likely to have elevated HbA1c and BP compared with white patients | 4/6 |
| 45 | Saaddine et al (2006) | Adults with diabetes aged 18‐75. Excluded women with gestational diabetes (NHANES 1988‐1994 N = 1024; NHANES 1999‐2002 N = 750; BRFSS 1995 N = 3065; BRFSS 2002 N = 13,078) | HbA1c > 9%, LDL cholesterol < 130 mg/dL, BP < 140/90, nephropathy test, dilated eye examination, foot examination, aspirin therapy | Ambulatory care setting. National (NHANES, 1988‐1994 and 1999‐2002; BRFSS 1995 and 2002) | Pooled cross‐sectional study design. Logistic regression with age, gender, poverty income ratio, education, race, health insurance status, insulin use, binary variable for time | This study sought to examine changes in the quality of diabetes care provided in the United States between 1998 and 2002. Over the period studied, lipid test, eye examinations, and LDL control showed the most improvement over time. Patients with ≥ HS showed a 9.8 percentage point improvement in lipid testing. Whites (+24%), <HS (+34%), and insured (+21%) showed improvements in LDL control over baseline levels | 4/6 |
| 46 | Saydah et al (2007) | Adults aged ≥ 20 with prior diabetes DX by clinician. Excluded pregnant women at time of interview, participants missing information on A1c levels (N = 843) | HbA1c level < 7% | Ambulatory care setting, National (NHANES 1999‐2002) | Pooled cross‐sectional analysis with logistic regression including age, gender, poverty income ratio, education, race, health insurance status, waist circumference, time since last BP reading, and diabetes treatment (insulin only, oral med, combination, neither) | This study's objective was to examine racial/ethnic differences in good glycemic control after controlling for SES factors such as education and income. In multiple regression results, Mexican Americans were less likely to have HbA1c < 7% OR = 0.43, P < .05), but blacks did not differ from white patients. Interactions between SES status measures and race were not significant. Patients using either insulin or oral medication or a combination were significantly less likely to have HbA1c < 7% (OR ranged from 0.06 to 0.24) | 5/6 |
| 47 | Selby et al (2007) | Adult diabetes patients aged ≥ 18, continuously enrolled for 18 mo, who received 5 of 7 care processes without missing data for HbA1c, LDL, and BP control (N = 3,533) | HbA1c > 8% | Managed care ambulatory care clinics, CA, HI, MI, NJ, PA, TX (TRIAD survey 2000‐2004) | Logistic regression included age; gender; education; race; BMI; prior history of CHD, and diabetes treatment (oral only, insulin only, insulin + oral); moderate/severe depression; depression scale based on PHQ8; perceived neighborhood crime; glucose strip copay; cost burden a problem; getting needed care; trust in physician score; smoking; physical activity ≥ 3 times/ week | This study examined a patient population receiving 5 of 7 diabetes care processes (A1c test, lipid test, albumin screen, eye examination, foot examination, taking aspirin, influenza vaccination) and examined patient characteristics associated with poor control of one or more of three diabetes intermediate outcomes (A1c control, LDL control, BP control) using patients with good control in all three intermediate outcomes as their reference group. Regressions found odds of poor control were associated with certain minority races (black, Asian, other race), lower education, younger age, higher BMI, smoking, reporting cost as a barrier to care, and use of oral agents. In contrast, a prior history of CHD, vigorous physical exercise, and trust in one's physician were associated with good control | 5/6 |
| 48 | Shani et al (2010) | All diabetes Israeli patients treated by same physician 2+ y, aged ≥ 18 (N = 170 PCPs, N = 18,316 diabetes patients) | Percentage of patients with HbA1c level < 7%; percentage of patients with BP < 130/80; percentage of patients with LDL cholesterol < 100 mg/dL | Primary care clinics. Israel. 2005 (Clalit Health Services Primary HMO Database 2004‐2005) | Longitudinal design using 2004 patient characteristics with follow‐up and measurement in 2005. Linear regression models at the physician level with sex, age, SES status, BMI, new immigrant status. b | Study aim was to examine the relationship between the proportion of a physician's patients with controlled diabetes intermediate outcomes and patient characteristics. Regression results showed that physicians with higher proportions of low SES patients and higher mean BMI had lower percentages of diabetes patients with HbA1c < 7%. Higher proportions of immigrants were associated with higher percentages of diabetes patients with HbA1c < 7%. None of these characteristics were related to BP control | 3/6 |
| 49 | Sloan et al (2004) | Patients aged 65+ in 1991 with a diabetes DX code on two or more nonhospital Medicare claims or 1 or more claims for hospital, hospice, and skilled nursing services (N = 4906 diabetes patients) | Eye examination | Institutional and noninstitutional settings, National (National Long‐Term Care Survey (NTLCS) with matched Medicare claims 1991‐1999) | Longitudinal cohort design with logistic regression and binary variables for reading; diabetes DX; point of diabetes DX; diabetic retinopathy; glaucoma; age‐related macular degeneration; cataract; not diagnosed; diabetes complications; time point of death; dementia; years of education; income; ADLs; married; children at home; children in 1 hr drive; in nursing home; months on Medicaid; months on HMO; eye doctors per 10,000 pop; dxCG score; male; black; Hispanic; other races | This study's objective was to identify the factors associated with compliance with guidelines for recommended care for annual eye examinations for patients diagnosed with diabetes or age‐related macular degeneration (ARMD). Receipt of eye examinations was higher for patients with a DX of DR (OR range: 1.53‐1.67, P < .05), glaucoma (OR range: 1.24‐3.86, P < .05), ARMD (1.76‐1.83, P < .5), and cataract (OR = 2.9, P < .05). Patients with dementia were less likely to receive eye examinations (OR = 0.71, P < .05), as were patients of black descent (OR = 0.68, P < .05), Hispanic, and Other races were not significantly different from whites. Patients in nursing homes were more likely to receive eye examinations (OR = 1.96, P < .05), as were patients with spouses or children at home (OR range: 1.10‐1.20, P < .05). Each additional year of education was associated with a 37% increase odds of an eye examination (P < .05). While these factors were related to the probability of receipt, 80% of the variation in probability of receipt (pseudo R 2 ) remained unexplained | 5.5/6 |
| 50 | Sundquist et al (2011) | Patients aged 35‐74 in Stockholm, Sweden, with type 2 diabetes mellitus using primary health care centers (PHCCs) during 2005. Excluded patients with type 1 diabetes (N = 5048) | HbA1c testing; HbA1c < 6%; lipid profile; LDL < 130 | Primary care clinics Stockholm County, Sweden (2005 Patient Electronic medical records from 25 Primary Health Care Clinics of Stockholm County Sweden linked to national Migmed database) | Longitudinal cohort design. Obtained electronic health records for patients visiting PHCCs in 2005. Logistic regression included sex; age; country of birth; education level; family income quartiles | Study examined association between patient sociodemographics and HbA1c, and lipid control for type 2 diabetes patients. Women were more likely to reach HbA1c < 6%, while men were more likely to controlled LDL/HDL/HbA1c. Older patients were more likely to have controlled HbA1c, total cholesterol, triglycerides, and HDL cholesterol. Immigrants from Middle Eastern and other countries had lower odds of HbA1c < 6% compared with Swedish patients. Patients with the lowest family income levels were less likely to have controlled HbA1c, triglycerides, HDL, or the composite rate | 3/6 |
| 51 | Tabaei et al (2017) | Adults (18 ≥ y old) with diabetes in New York City (NYC) (N = 182,756) | HbA1c control (<7%; sensitivity analysis examined < 8%) | NYC Department of Health & Mental Hygiene HbA1c Registry from 2007 to 2013 | Study adjusts for individual‐level age; sex; frequency of HbA1c testing; duration of follow‐up; average time between HbA1c testing; ZIP code % of white pop; ZIP code % of black population; ZIP code % of Latino population; ZIP code % population with income < FPL; ZIP code % population college grad; ZIP code % population HS grad; ZIP code % population < HS; ZIP code total population; ZIP code residential advantage composite quintiles (Q1 is least advantaged, Q5 is most advantaged) | These results show that residential areas with greater resources to support healthy food and residential walkability are associated with improved glycemic control in persons with diabetes | 2/6 |
| 52 | Tao et al (2016) | Patients aged 18 y or older, diagnosed with type 2 diabetes with a duration of at least 6 mo at enrollment, willing to sign consent, and able to complete the questionnaires were included. Patients with type 1 diabetes and/or gestational diabetes were excluded from the study (N = 25,454) | HbA1c < 7%; BP < 140/80 mmHg | Outpatient hospital setting of 104 hospitals across all major regions of China (3B STUDY database, August 2010 and March 2011) | Models adjusted for age, gender, BMI, smoking, alcohol consumption, exercise, and diabetes duration | This study's objective was to examine SES and metabolic control and diabetes complications in Chinese patients with diabetes. Results showed patients with a college education or above had 38% higher odds of HbA1c < 7% (relative to patients that are illiterate). No differences in BP < 140/80 were found for college‐educated patients. Control of all three intermediate outcomes (HbA1c, BP, and total cholesterol) was also 30% higher for college‐educated patients. Illiterate patients showed 10% and 19% higher risk of cardiovascular disease and cerebrovascular disease. Higher income was not consistently related to improved control in intermediate outcomes | 2/6 |
| 53 | Toivakka et al (2018) | Included all patients diagnosed with type 2 diabetes (ICD‐10 code E11) by the end of 2012 in region of North Karelia (N = 10,204) | HbA1c < 7% | Ambulatory care setting (Regional Electronic Patient Database 2012, Statistics Finland Database 2011) | Models included age, gender, patient‐level income, patient‐level education, patient unemployment, area income, area education, area unemployment and random effects terms for municipality, and postal code are | This study examined the use of patient‐level SES measures against postal code area‐level measures of SES in explaining variation in HbA1c control. Results showed that patient education level and income were associated with lower HbA1c level. Area‐level measures of education (eg, education level of people residing around the patient) had similar effects on HbA1c level as did patient‐level education | 1.5/6 |
| 54 | Traylor et al (2010) | Kaiser adult diabetes patients aged ≥ 18 DX before 1/1/2005 with active drug benefit continuously throughout 2005. Excluded Asian patients (N = 108,555) | HbA1c level; LDL cholesterol level; systolic BP | Managed care ambulatory care, Northern CA (2005 Kaiser Permanente database) | Longitudinal cohort design with physician random effect probit and logit models with patient age; sex; preferred language; No. of comorbidities; No. of primary care visits in 2005; Medicare status; No. of meds; geocoded education and income; physician age; sex; race/ethnicity; language; panel size; No. of diabetic patients | This study examined the relationship between patient‐physician concordance in race/ethnicity and cardiovascular disease‐related intermediate outcomes for diabetes care in a large cohort of diabetes patients enrolled in a private insurer. The study also examined whether concordance is related to appropriate modification of treatment in response to risk factor levels. In models adjusting for patients and physician characteristics, black and Hispanic race remained significant factors explaining variation in HbA1c control, LDL control, and BP control. Race was also related to treatment intensification. Patient‐physician race concordance did not explain differences in intermediate outcomes or the intensification of outcomes | 3/6 |
| 55 | Trivedi et al (2005) | Medicare advantage beneficiaries aged ≥ 65, who are black/white (N = 1,803,451) | Eye examination; HbA1c testing; HbA1c < 9.5%; lipid profile; LDL < 130 | Managed care setting, nationwide (patient‐level Medicare managed care HEDIS data, 1997‐2003) | Repeated cross‐sectional data. Fit multiple multivariate linear regression models. Adjusted for age; sex; rurality; health plan; Medicaid eligibility; ZIP code % of persons age 65 and older with some college or more; ZIP code % of persons age 65 and older with income below FPL | Used nine HEDIS measures to examine White‐black disparities for Medicare Advantage plan patients during 1997‐2003. Regression adjustment with certain covariates reduced black‐white disparities: Medicaid coverage; enrollee residence in high poverty/low education areas; and rural residence. Age and gender adjustment did not affect the size of disparities | 3/6 |
| 56 | Wilf‐Miron et al (2010) | Maccabi Healthcare Service (MHS) enrolled Israeli diabetes patients aged 18‐80 who visited GP at least once every 2 y captured in the computerized diabetes registry (N = 74,953) | HbA1c testing; LDL cholesterol testing; complete follow‐up of HbA1c testing, LDL testing, and nephropathy screen; HbA1c > 9%; LDL < 100 | Israeli health care setting (MHS electronic medical record. December 2007 to November 2008) | Logistic regressions included age; gender; immigrant status; SES rank (SER) 1‐10; supplementary voluntary health insurance (SVHI). | Examined disparities in delivery of care, management, and control of diabetes in large Israeli HMO. Process diabetes outcomes showed higher adherence among older patients, females, SVHI holders, immigrants from former Soviet Union, Arabs, and patients of lower SER (1‐10). A similar pattern was observed for HbA1c control and LDL control, except relationship with gender favored males and SVHI was not significant for LDL control | 3/6 |
| 57 | Williams et al (2013) | Patients eligible for sample were aged 65+ by 1/1/2005 with drug costs> $2250 by 10/1/2006, and continuously enrolled in a MAPD plan from 1/1/2005 to 12/31/2006, or newly enrolled in PDP during 11/15/2005 and 3/1/2006 and continuously enrolled until 12/31/2006. Medicare beneficiaries with low‐income subsidy (LIS), full prescription drug coverage in the gap, and not providing informed consent were excluded (N = 1264) | Not applicable | Ambulatory care setting (TRIAD survey 2006) | Regression modeled cost‐related nonadherence (CRN) for a given patient‐medication dyad to examine characteristics associated with CRN. Variables included indicators for type of medication (diabetes, hypertension, cholesterol‐lowering, symptom relief, and other); comorbidity count, OOP costs in Q1 of 2006; age; gender; race/ethnicity (white non‐Hispanic, Hispanic, African American, Asian, Other); educational attainment (<HS, HS, some college, college grad+); annual income (<$25 K, $25 K‐$40 K,>$40 K); plan type; presence of any coverage for medications in the gap | The study's analysis included examination of the rate and correlates of self‐reported CRN among a population of older persons with diabetes. Results showed diabetic patients in the sample were more likely to forego cholesterol or other medications (as opposed to diabetes or hypertension medications) due to cost (OR = 1.54, 1.40). Patients aged 75+ in the sample were significantly less likely to have CRN. Patients with only a high school degree were significantly more likely to have CRN (relative to patients with a college degree or higher) as were patients with incomes below $25 K (relative to patients with incomes of at least $40 K) | 2/6 |
| 58 | Wong et al (2012) | Adult, noninsulin using, type 2 diabetes patients visiting general outpatient clinics (GOPCs) in Tseung Kwan O and Sai Kung districts (N = 1970) | HbA1c testing; nephropathy screening; eye examination; smoking status; BMI; cholesterol measurement; HbA1c < 7%; BP < 130/80 mmHg; LDL < 2.6 mmol/L | Ambulatory, government primary care clinics (patient medical records from 3 GOPCs in Tseung Kwan O and Sai Kung districts from July to October 2009) | Retrospective cross‐sectional data. Conducted logistic regression with age; sex; insurance payment status (proxy measure of SES); clinic; duration of diabetes; and BMI | This study's objective was to examine patient characteristics related to disparities in diabetes quality for type 2 diabetes patients in Hong Kong. Process measures showed lower compliance among patients aged 75+ (compared with patients aged < 55), women, and fee waiver patients (patients not required to pay for health insurance). Control of intermediate outcomes showed differences between clinics and by patient age groups. Compared with patients aged < 55, patients aged 55+ were more likely to have HbA1c < 7% | 3.5/6 |
| 59 | Yoo et al (2017) | Randomly selected sample of patients with diabetes from 8 metro cities and 9 provinces in Korea (N = 43,283) | HbA1c testing | Korean National Health Insurance Research Database (covers 97% of Korean population) 2012‐2013 | Age, sex, income level, duration of diabetes, medical institution visited most frequently for diabetes care, and regional factors captured by % farmer population | The frequency of HbA1c monitoring in Korea is suboptimal, especially in rural areas, and this study found significant regional variation | 4.5/6 |
| 60 | Zeng et al (2018) | Community residents in Xiamen, China, in 2016 with type 2 diabetes (N = 798) | HbA1c control (<7%) | Community setting in Xiamen, China (survey linked to patient medical records 2016) | Adjusted for sex, age, education (illiterate and primary school, secondary, tertiary), type of medication(none, pills only, insulin only, pills, and insulin), self‐monitoring of blood glucose, BMI, smoking status, alcohol consumption, duration of diabetes, monthly income, and number of comorbidities (none, 1‐2, 3+) | Sex‐specific educational disparities exist in the association between self‐monitoring and glycemic control | 2.5/6 |
Abbreviations: 3B STUDY, blood glucose blood pressure blood lipid in Chinese patients with type 2 diabetes; BMI, body mass index; BP, blood pressure; CHD, coronary heart disease; DX, diagnosis; ESRD, end‐stage renal disease; FPL, federal poverty level; HbA1c, hemoglobin A1c; HEDIS, Health Effectiveness Data and Information Set; HMO, health maintenance organization; LDL, low‐density lipoprotein; MAPD, medicare advantage prescription drug; OR, odds ratio; PDP, prescription drug plan; SER, socioeconomic rank; SES, socioeconomic status; SVHI, supplemental voluntary health insurance; T2DM, type 2 diabetes mellitus; USC, usual source of care.
Adapted New Castle Ottawa Score
Low SES in Shani et al (2010) is defined by the National Insurance Institute of Israel using the patient's income.
3.2. Meta‐analysis of diabetes quality measures by race/ethnicity
Table 2 presents results across all diabetes care measures for race/ethnicity and education. Appendices S4 and S5 present forest plots for all diabetes measures for each race/ethnicity and education. Across 15 studies controlling for race/ethnicity, income, or education, blacks with diabetes tended to have lower control in intermediate outcomes compared to whites with diabetes, but had a higher likelihood of tests in several process measures. Blacks with diabetes had lower odds for controlled HbA1c (OR = 0. 67, 95% CI: 0.55‐0.83) and blood pressure (OR = 0.68, 95% CI: 0.58‐0.80). Among process measures, blacks had higher odds for dilated eye examinations, foot examinations, and nephropathy screening (OR range: 1.22‐1.49, P < .05) but a lower odds of lipid testing (OR: 0.72, CI: 0.59‐0.88) compared with whites. Studies examining diabetes measures varied in heterogeneity with HbA1c control, LDL control, HbA1c testing, and lipid testing exhibiting high heterogeneity (I 2 range: 83‐98 percent), while heterogeneity among other measures was lower (I 2 range: 43‐59 percent; Figure 2).
Table 2.
Meta‐analysis results for diabetes care measures by patient race/ethnicity and education
| Race/Ethnicity b | Education c | ||||
|---|---|---|---|---|---|
| Black | Hispanic | Asian | ≥HS | ||
| Intermediate outcomes | |||||
| HbA1c control | Effect size: | 0.672 a | 0.682 a | 1.515 | 1.242 a |
| 95% CI: | 0.546, 0.828 | 0.607, 0.767 | 1.318, 1.742 | 1.130, 1.364 | |
| No. of studies (I 2 statistic): | 10 (98%) | 9 (91%) | 1 (NA) | 12 (85%) | |
| BP control | Effect size: | 0.680 | 1.141 | 1.124 | 1.109 |
| 95% CI: | 0.580, 0.796 | 0.977, 1.333 | 0.983, 1.279 | 0.953, 1.291 | |
| No of studies (I 2 statistic) | 7 (86%) | 5 (87%) | 1 (NA) | 5 (92%) | |
| LDL control | Effect size: | 0.959 | 1.148 | 0.756 | 1.078 |
| 95% CI: | 0.718, 1.280 | 0.913, 1.443 | 0.599, 0.952 | 0.840, 1.383 | |
| No of studies (I 2 statistic) | 6 (94%) | 5 (97%) | 2 (84%) | 4 (92%) | |
| Process measures | |||||
| HbA1c test | Effect size: | 0.935 | 1.146 | 1.303 | 0.96 |
| 95% CI: | 0.654, 1.336 | 0.841, 1.562 | 1.012, 1.677 | 0.839, 1.098 | |
| No of studies (I 2 statistic): | 4 (83%) | 5 (79%) | 2 (51%) | 2 (55%) | |
| Eye examination | Effect size: | 1.218 a | 1.138 | 1.376 a | 1.277 a |
| 95% CI: | 1.114, 1.331 | 0.973, 1.330 | 1.133, 1.670 | 1.170, 1.393 | |
| No of studies (I 2 statistic) | 7 (43%) | 9 (80%) | 3 (39%) | 4 (83%) | |
| Foot examination | Effect size: | 1.493 a | 1.088 | 1.275 a | 1.065 |
| 95% CI: | 1.307, 1.786 | 0.928, 1.275 | 1.103, 1.473 | 0.951, 1.193 | |
| No of studies (I 2 statistic): | 6 (59%) | 8 (80%) | 2 (0%) | 4 (90%) | |
| Lipid test | Effect size: | 0.722 a | 1.014 | 1.221 a | 1.191 |
| 95% CI: | 0.593, 0.880 | 0.956, 1.076 | 1.088, 1.370 | 0.895, 1.583 | |
| No of studies (I 2 statistic): | 4 (86%) | 4 (0%) | 2 (0%) | 4 (99%) | |
| Nephropathy screening | Effect size: | 1.27 | 1.11 | 1.08 | 0.94 |
| 95% CI: | 1.08, 1.49 | 0.94, 1.32 | 0.92, 1.27 | 0.84, 1.05 | |
| No of studies (I 2 statistic): | 1 (NA) | 1 (NA) | 1 (NA) | 1 (NA) | |
Estimates in bold are significant at the 5% level or higher.
Abbreviations: BP, blood pressure; CI, confidence intervalHbA1c, hemoglobin A1c; ≥HS, high school degree or more; LDL, low‐density lipoprotein.
Estimate and 95% CI are comparable to results after trim‐and‐fill imputation with no substantive difference. Difference in OR point estimate minus trim‐and‐fill OR ranged from −0.111 to +0.123. There was 50% or greater overlap between estimate's 95% CI and 95% CI from trim‐and‐fill procedure.
Race/ethnicity estimates use white patients with diabetes as the reference group.
Education results use patients with less than high school degree as the reference group.
Figure 2.
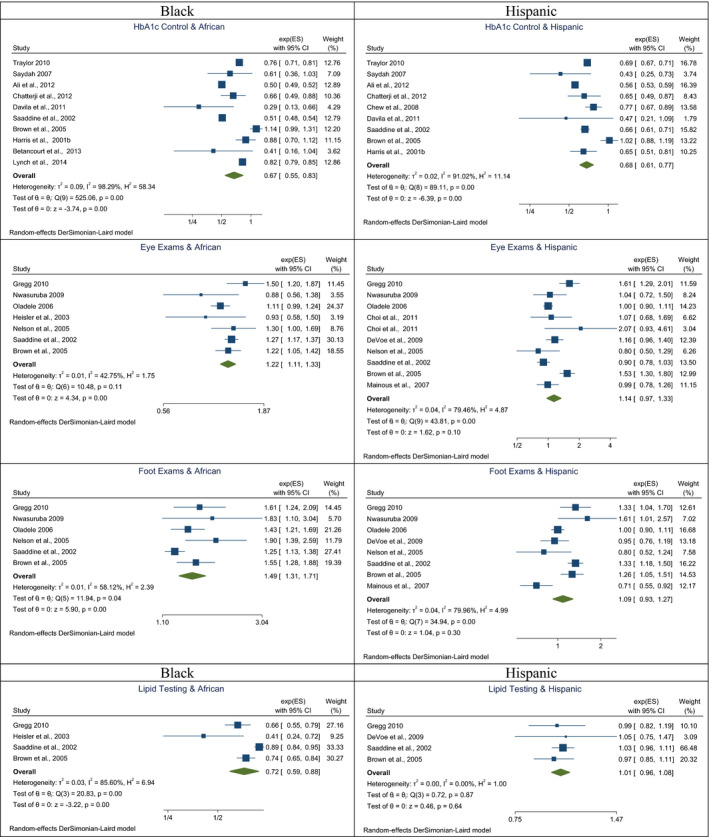
Forest plots for meta‐analyses of select diabetes care measures for Hispanic and black diabetes patients[Colour figure can be viewed at wileyonlinelibrary.com]
Results for Hispanics with diabetes across 16 studies suggest Hispanic ethnicity was not associated with differences in process measures relative to white patients although Hispanic patients had lower odds of HbA1c control (OR = 0.68, 95% CI: 0.61‐0.77) but no difference among other intermediate outcomes. Unlike studies examining diabetes care for blacks, estimates for Hispanics showed high levels of heterogeneity across studies for all measures (I 2 range: 79‐97 percent) except lipid testing.
Asians (N = 4 studies) exhibited higher control or receipt of care (OR range: 1.22‐1.52, all P < .05) for HbA1c control, HbA1c testing, dilated eye examinations, foot examinations, and lipid tests but lower control for LDL cholesterol (OR: 0.76, 95% CI: 0.60‐0.95) than whites. Studies contributing estimates for four measures showed I 2 ranging from 0 to 51 percent. This suggests sampling variability may have played more of a role than differences in study design in variability across study estimates. The two studies for LDL cholesterol control showed higher heterogeneity than other measures (I 2 = 84 percent) for Asians, suggesting differences between the estimates may reflect study design features.
Overall, blacks and Hispanics exhibited lower control in intermediate outcomes with greater odds of care or no difference in process measures compared with white patients. Asian patients with diabetes tended to have higher control or no difference across all measures except LDL control. Studies for blacks and Hispanics exhibited high heterogeneity for important intermediate outcomes such as HbA1c and LDL control, suggesting differences in study design, patient sampling, covariate choice, and context underlie variation across studies. Results for blacks and Hispanics did not differ markedly between studies using only insured populations versus those that also included uninsured patients. Results in Table 2 were consistent with results following the trim‐and‐fill procedure for race/ethnicity in the HbA1c control, dilated eye examinations, foot examinations, and lipid testing measures.
3.3. Meta‐analysis of diabetes quality measures by education
Meta‐analyses of 13 studies examining the relationship between education level and diabetes quality found that having a high school education or more was associated with higher HbA1c control (OR = 1.24, 95% CI: 1.13‐1.36) or receipt of dilated eye examinations (OR = 1.28, 95% CI: 1.17‐1.39). For other diabetes measures, lacking a high school degree was not associated with significant differences in odds of control or receipt of care, although odds ratio estimates for high school or more were larger than one for all measures except nephropathy screening (P > .05). Study estimates for education indicated significant heterogeneity across all measures except HbA1c control (I 2 = 55 percent) and nephropathy screening, with I 2 statistics ranging from 83 to 99 percent. As with meta‐analyses for race, comparisons of studies that were wholly based on insured populations did not exhibit notable differences from studies that included uninsured diabetes patients. Results for education were consistent with estimates from the trim‐and‐fill procedure for HbA1c control and dilated eye examinations.
3.4. Differences in diabetes quality measures by income
Forty‐two studies in the systematic review used a measure of income, but variables used to measure income varied substantially across studies. Approaches included percentile indicators (eg, quartiles) of varying dollar thresholds, thresholds based on other currencies, deprivation indices, Townsend score, social class rankings, food stamp receipt, and percentage of the federal poverty level. Among the three studies that could be combined, meta‐analyses indicated inconsistent associations between higher income and improved control in intermediate outcomes or receipt of process care (results not shown).
3.5. Possible mechanisms explaining differences in diabetes care quality associated with patient socioeconomics
The systematic review identified several variables that may influence or mediate socioeconomic‐related disparities in diabetes care. We categorized these variables broadly into three groups: access‐related factors such as presence of a usual source of care and local health system resources; factors related to food insecurity and trade‐offs at lower incomes; and patient age group and health status.
Variables indicating barriers in accessing care such as the lack of insurance, lack of a usual source of care, dual eligibility for Medicare and Medicaid, or rurality appear to be interrelated with important sociodemographic differences in diabetes quality. 8 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 Similar measures that may adjust for differences in access included the number of generalist physician visits, endocrinologist visits, or other metrics of ambulatory care utilization. 8 , 23 , 25 Quartile or similar indicators of primary care visit thresholds might proxy for access in the absence of reliable data on insurance or a usual source of care. Out of nine studies that reported usable estimates for insurance, and race, the estimate for lack of insurance was always larger than race/ethnicity for every outcome examined in 4 of the studies. 8 , 22 , 23 , 26 Among the ten studies with usable estimates for insurance and education/income, lack of insurance was always larger than education or income across outcomes in 7 of the studies. 8 , 22 , 23 , 24 , 26 , 27 , 28 Depending on the sample, access‐related measures may have mediating effects on race/ethnicity or other characteristics related to diabetes care. 25
Across studies, younger and healthier patients were associated with lower performance in diabetes care possibly reflecting a tendency to forego testing or self‐management because of nonadherence or resource constraints. Among fifteen studies that reported estimates for patient age, 11 included results showing older patients or patients in poorer health status having a greater likelihood of complying with diabetes care guidelines. 8 , 23 , 25 , 26 , 27 , 31 , 32 , 33 , 34 , 35 Odds ratios in studies examining intermediate outcomes similarly tended to show greater control for patients over age 65 for HbA1c control and LDL control. 8 , 30 , 31 , 32
The literature noted a variety of challenges that compound difficulties in managing diabetes among very low‐income populations. Food insecurity was associated with significantly lower HbA1c control and receipt of care for diabetes, strongly suggesting a significantly increased risk of foregoing needed medications to pay for food relative to food secure patients. 36 , 37 While reduced performance among patients probably reflects resource trade‐offs, other studies suggest that neighborhood characteristics such as crime, walkability, and the availability of fresh fruits and vegetables may also ease or impede management of diabetes. 38 , 39
4. DISCUSSION
Which quality measures should be adjusted for patient sociodemographic differences to make provider comparisons more equitable and how that adjustment should be conducted remain important and controversial issues for health care policy makers. 14 The use of quality measures to inform consumers and incentivize improved value in the delivery of care remain key features in transitioning incentives toward value. However, if measures are unduly sensitive to patient characteristics their use could punish providers who disproportionately care for larger numbers of more complex and vulnerable patients. Along this vein, the National Quality Forum recommends adjusting quality measures for SES and race/ethnicity, but cautions that the adjustment approach is chosen carefully to avoid introducing perverse provider incentives into the delivery of care. 40
Although this study found differences in the odds of diabetes care performance associated with race/ethnicity and education, the effects of these relationships on quality reporting and payment will depend on the rules used to determine provider payment or to assign ratings to providers. Depending on the rules are chosen to determine ratings, the sociodemographic differences found in this study could influence some provider ratings more and others less. Differences in diabetes performance appear to be specific to individual race/ethnic groups. These differences were persistent even after regression adjustment for age, sex, clinical condition, health status, income, education, psychological coping, or lifestyle. Relative to whites, black and Hispanic patients had lower performance in intermediate outcomes but higher performance in many process measures. Recent studies suggest some of the differences between race/ethnic groups in intermediate outcomes may be attributable to biologic differences such as higher risk of hypertension among black patients. 41 Performance across both intermediate outcomes and process measures tended to rise with education although meta‐analyses found only two of the eight measures were statistically significant. Although the direction of association varied, the magnitude of effects did not differ substantially between process and intermediate outcome measures (Table 2).
This systematic review highlighted potential factors that may mediate performance in diabetes measures such as access to care, patient age, and health status. It was difficult to determine which variables were most influential in driving differences. Difficulties in access, such as lacking insurance coverage or a usual source of care, were associated with diminished care for six of the eight diabetes measures in this study. Lower odds of control or receipt of care among younger patients with diabetes could reflect tendencies to delay regular testing, or reluctance to lifestyle changes needed to slow disease progression because of the lack of immediate negative health effects. Among sixteen studies that reported estimates, ten found that younger and potentially healthier patients were more likely to have lower odds of control or receipt of care. The systematic review found other variables influencing the relationship between socioeconomics and diabetes care quality. These included language proficiency, patient sociocultural background, food insecurity, neighborhood effects, second‐hand smoke, and number of hours worked on a weekly basis. Among these variables, access differences may have the most substantial mediating influence on sociodemographic differences in diabetes quality.
Studies included in this review were largely observational, and real‐world application of these concepts may require modifications to make adjustments feasible. Measuring income or education in administrative data has limitations. 42 Findings from this review suggest that relative to associations with race/ethnicity and education, factors influencing an individual's ability to regularly access health services may play a more prominent role in influencing performance in diabetes care measures. Although the accuracy of race/ethnicity in administrative data may sometimes be limited, this measure may be more readily available as opposed to measures of income, education, and more direct measures of the potential drivers of these health disparities.
Our study includes several limitations. Many patient characteristic‐quality measure cells remain populated by a small number of studies and should be interpreted with caution. Only one study contributed usable results for the nephropathy screening measure. Estimates across all diabetes measures for Asian race/ethnicity except dilated eye examinations included fewer than 3 studies. Analyses relating patient income with diabetes quality also included only 3 studies. Second, studies retained in the meta‐analysis were published manuscripts and may be subject to publication bias. We used the trim‐and‐fill procedure to test the sensitivity of our results and found consistency in 10 of the 15 significant relationships after imputation. Third, studies in this review apply the average measurement of an intermediate outcome at a point in time to individuals when in reality metrics such as HbA1c or blood pressure levels vary continuously. 43
Case mix adjustment of quality measures for the purpose of comparing provider quality should carefully consider the clinical and nonclinical makeup of patients constituting the analytic sample. Our findings suggest patient race/ethnicity and educational level should be considered when case mix adjusting diabetes quality measures for patient sociodemographic differences. Differences related to patient income were not consistent across the income levels studied; therefore, we are not able to rule out this variable as a socioeconomic confounder for diabetes care. Other findings suggest markers such as food insecurity or food assistance may be important in case mix adjustment for comparisons that include low‐income populations. Because data for patient race/ethnicity, education, access, and health status are not always available, future studies should investigate the implications for adjustment when one or more of these types of variables are omitted.
Supporting information
Appendix S1‐S6
Author Matrix
ACKNOWLEDGMENT
Joint Acknowledgment/Disclosure Statement: The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the US Department of Health and Human Services or any of its agencies.
Lee W, Lloyd JT, Giuriceo K, Day T, Shrank W, Rajkumar R. Systematic review and meta‐analysis of patient race/ethnicity, socioeconomics, and quality for adult type 2 diabetes. Health Serv Res. 2020;55:741–772. 10.1111/1475-6773.13326
REFERENCES
- 1. Rosenthal MB, Landon BE, Normand ST, et al. Pay for Performance in Commercial HMOs. N Engl J Med. 2006;355(18):1895‐1902. [DOI] [PubMed] [Google Scholar]
- 2. Song Z, Safran DG, Landon BE, et al. The alternative quality contract based on a global budget lowered medical spending and improved quality. Health Aff. 2011;31(8):1885‐1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McWilliams JM, Hatfield LA, Chernew ME, et al. Early performance of accountable care organizations in Medicare. N Engl J Med. 2016;374(24):2357‐2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McWilliams JM, Gilstrap LG, Stevenson DG, et al. Changes in postacute care in the Medicare shared savings program. JAMA Intern Med. 2017;177(4):518‐526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brown AF, Gregg EW, Stevens MR, et al. Race, ethnicity, socioeconomic position, and quality of care for adults with diabetes enrolled in managed care. Diabetes Care. 2005;28(12):2864‐2870. [DOI] [PubMed] [Google Scholar]
- 6. Zaslavsky AM, Epstein AM. How patients’ sociodemographic characteristics affect comparisons of competing health plans in California on HEDIS quality measures. Int J Qual Health Care. 2005;17(1):67‐74. [DOI] [PubMed] [Google Scholar]
- 7. McWilliams JM, Meara E, Zaslavsky AM, et al. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of Medicare coverage. Ann Intern Med. 2009;150(8):505‐515. [DOI] [PubMed] [Google Scholar]
- 8. Ali MK, Cullard KM, Imperatore G, Barker L, Gregg EW. Division of diabetes translation. characteristics associated with poor glycemic control among adults with self‐reported diagnosed diabetes – National Health and Nutrition Examination Survey, United States 2007–2010. Morb Mortal Wkly Rep. 2012;Suppl:32‐37. [PubMed] [Google Scholar]
- 9. Chatterji P, Joo H, Lahiri K. Racial/ethnic and education related disparities in the control of risk factors for cardiovascular disease among individuals with diabetes. Diabetes Care. 2012;35:305‐312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Joynt KE, Jha AK. A path forward on Medicare readmissions. N Engl J Med. 2013;368(13):1175‐1177. [DOI] [PubMed] [Google Scholar]
- 11. Lysy Z, Booth GL, Shah BR, et al. The impact of income on the incidence of diabetes: a population‐based study. Diabetes Res Clin Pract. 2013;99:372‐379. [DOI] [PubMed] [Google Scholar]
- 12. Maty SC, Everson‐Rose SA, Haan MN, et al. Education, income, occupation, and the 34‐year incidence (1965–99) of Type 2 diabetes in the Alameda County Study. Int J Epidemiol. 2005;34:1274‐1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Connolly V, Unwin N, Sherriff P, et al. Diabetes prevalence and socioeconomic status: populated based study showing increased prevalence of type 2 diabetes mellitus in deprived areas. J Epidemiol Commun Health. 2000;54:173‐177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Office of the Assistant Secretary for Planning and Evaluation . Report to Congress: Social Risk Factors and Performance Under Medicare’s Value‐Based Purchasing Programs. Washington, D. C.: U. S. Department of Health and Human Services; 2016. [Google Scholar]
- 15. Fiscella K, Burstin H, Nerenz DR. Quality measures and sociodemographic risk factors, to adjust or not to adjust. J Am Med Assoc. 2014;312(24):2615‐2616. [DOI] [PubMed] [Google Scholar]
- 16. Jha AK, Zaslavsky AM. Quality reporting that addresses disparities in health care. J Am Med Assoc. 2014;312(3):225‐226. [DOI] [PubMed] [Google Scholar]
- 17. Werner RM, Asch DA. The unintended consequences of publicly reporting quality information. J Am Med Assoc. 2005;293(10):1239‐1244. [DOI] [PubMed] [Google Scholar]
- 18. Werner RM, Goldman LE, Adams DR. Comparison of change in quality of care between safety‐net and non‐safety‐net hospitals. J Am Med Assoc. 2008;299(18):2180‐2187. [DOI] [PubMed] [Google Scholar]
- 19. DerSimonian R, Laird N. Meta‐analysis in clinical trials. Control Clin Trials. 1986;7:177‐198. [DOI] [PubMed] [Google Scholar]
- 20. Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 10: Analysing data and undertaking meta‐analyses In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, eds. Cochrane Handbook for Systematic Reviews of Interventions version 6.0. Chichester (UK): John Wiley & Sons; (updated July 2019). 2019: [Google Scholar]
- 21. Duvall S, Tweedie R. Trim and fill: a simple funnel‐plot based method of testing and adjusting for publication bias in meta‐analysis. Biometrics. 2000;56(2):455‐463. [DOI] [PubMed] [Google Scholar]
- 22. Nelson KM, Chapko MK, Reiber G, et al. The association between health insurance coverage and diabetes care; data from the 2000 behavioral risk factor surveillance system. Health Serv Res. 2005;40(2):361‐372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Oladele CRW, Barnett E. Racial/Ethnic and social class differences in preventive care practices among persons with diabetes. BMC Public Health. 2006;6:259‐267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Paz SH, Varma R, Klein R, et al. Noncompliance with vision care guidelines in lationos with type 2 diabetes mellitus. Ophthalmology. 2006;113(8):1372‐1377. [DOI] [PubMed] [Google Scholar]
- 25. Mainous AG, Diaz VA, Koopman RJ, et al. Quality of care for hispanic adults with diabetes. Fam Med. 2007;39(5):351‐356. [PubMed] [Google Scholar]
- 26. DeVoe JE, Tillotson CJ, Wallace LS. Usual source of care as a health insurance substitute for U. S. adults with diabetes? Diabetes Care. 2009;32(6):983‐989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kirk JK, Davis SW, Hildebrandt CA, Strachan EN, Peechara ML, Lord R. Characteristics associated with glycemic control among family medicine patients with type 2 diabetes. N C Med J. 2011;72(5):345‐350. [PubMed] [Google Scholar]
- 28. Chew LD, Schillinger D, Maynard C, Lessler DS. Glycemic and lipid control among patients with diabetes at six U.S. public hospitals. J Health Care Poor Underserved. 2009;19(4):1060‐1075. [DOI] [PubMed] [Google Scholar]
- 29. Kollannoor‐Samuel G, Chhabra J, Fernandez ML, et al. Determinants of fasting plasma glucose and glycosylated hemoglobin among low income latinos with poorly controlled type 2 diabetes. J Immigr Minor Health. 2011;13:809‐817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Saaddine JB, Engelgau MM, Beckles GL, Gregg EW, Thompson TJ, Narayan KMV. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med. 1990s;136(8):565‐574. [DOI] [PubMed] [Google Scholar]
- 31. Saaddine JB, Cadwell B, Gregg EW, et al. Improvements in diabetes processes of care and intermediate outcomes: United States, 1988–2002. Ann Intern Med. 2006;144(7):465‐474. [DOI] [PubMed] [Google Scholar]
- 32. Davila EP, Florez H, Trepka MJ, et al. Long work hours is associated with suboptimal glycemic control among US Workers with diabetes. Am J Ind Med. 2011;54:375‐383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sundquist K, Chaikiat A, Leon VR, Johansson S, Sundquist J. Country of birth, socioeconomic factors, and risk factor control in patients with type 2 diabetes: a Swedish study from 25 primary health care centres. Diabetes Metab Res Rev. 2010;27:244‐254. [DOI] [PubMed] [Google Scholar]
- 34. Wilf‐Miron R, Peled R, Yaari E, et al. Disparities in Diabetes Care: role of the patient’s socio‐demographic characteristics. BMC Public Health. 2010;10:729‐737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gregg EW, Karter AJ, Gerzoff RB, et al. Characteristics of insured patients with persistent gaps in diabetes care services. Med Care. 2010;48(1):31‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mayer VL, McDonough K, Seligman H, Mitra N, Long JA. Food insecurity, coping strategies and glucose control in low income patients with diabetes. Public Health Nutr. 2015;19(6):1103‐1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Moreno G, Morales LS, Isiordia M, et al. Latinos with Diabetes and Food Insecurity in an Agricultural Community. Med Care. 2015;53(5):423‐429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gary TL, Karter AJ, Safford MM, et al. Perception of neighborhood problems, health behaviors, and diabetes outcomes among adults with diabetes in managed care. Diabetes Care. 2008;31(2):273‐278. [DOI] [PubMed] [Google Scholar]
- 39. Tabaei BP, Rundle AG, Wu WY, et al. Associations of residential socioeconomic, food, and built environments with glycemic control in persons with diabetes in New York City from 2007–2013. Am J Epidemiol. 2017;187(4):736‐745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Risk adjustment for socioeconomic status or other sociodemographic factors. National Quality Forum. http://www.qualityforum.org/Publications/2014/08/Risk_Adjustment_for_Socioeconomic_Status_or_Other_Sociodemographic_Factors.aspx. Accessed December 4, 2014
- 41. Ford CN, Leet RW, Kipling LM, et al. Racial differences in performance of HbA1c for the classification of diabetes and prediabetes among US adults of non‐Hispanic black and white race. Diabet Med. 2019;36:1234‐1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Samson LW, Finegold K, Ahmed A, Jensen M, Filice CE, Joynt KE. Examining measures of income and poverty in Medicare administrative data. Med Care. 2017;55(12):e158‐e163. [DOI] [PubMed] [Google Scholar]
- 43. Beck RW, Connor CG, Mullen DM, Wesley DM, Bergenstal RM. The fallacy of average: how using HbA1c alone to assess glycemic control can be misleading. Diabetes Care. 2017;40(8):994‐999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Nicholas LH. Can food stamps help to reduce Medicare spending on diabetes? Economic and Human Biology. 2011;9:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Al Sayah F, Majumdar SR, Egede LE, Johnson JA. Associations between health literacy and health outcomes in a predominantly low income African American population with type 2 diabetes. Journal of Health Communication: International Perspectives. 2015;40:1‐8. [DOI] [PubMed] [Google Scholar]
- 46. Azam M, Marwood L, Ismail K, et al. Diabetes complications at presentation and one year by glycated haemoglobin at diagnosis in a multiethnic and diverse socioeconomic population: results from the south London Diabetes Study. Journal of Diabetes Research. 2015;2015:587673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Badedi M, Solan Y, Darraj H, et al. Factors Associated with long term control of type 2 diabetes mellitus. Journal of Diabetes Research. 2016;2016:2109542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Betancourt RM, Degnan KO, Long JA. Racial differences in glucose control among patients with type 2 diabetes: A survey on dietary temptations, coping, and trust in physicians. Ethn Dis. 2015;23(4):409‐414. [PubMed] [Google Scholar]
- 49. Chen GD, Huang CN, Yang YS, Lew‐Ting CY. Patient perception of understanding health education and instructions has moderating effect on glycemic control. BMC Public Health. 2014;14:683‐691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chen R, Ji L, Chen L, et al. Glycemic control rate of T2DM outpatients in China: a multi‐center survey. Med Sci Monit. 2015;21:1440‐1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Choi S, Lee J, Rush E. Ethnic and language disparities in diabetes care among California residents. Ethn Dis. 2011;21(2):183‐189. [PubMed] [Google Scholar]
- 52. Crowley MJ, Holleman R, Klamerus ML, Bosworth HB, Edelman D, Heisler M. Factors associated with persistent poorly controlled diabetes mellitus: Clues to improving management in patients with resistant poor control. Chronic Illness. 2014;10(4):291‐302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Diaz‐Apodaca BA, Cosio FG, Canela‐Soler J, Ruiz‐Holguin R, Cerqueira MT. Quality of diabetes care: a cross‐sectional study of adults of Hispanic origin across and along with United States‐Mexico Border. Rev Panam Salud Publica. 2010;28(3):207‐2013. [DOI] [PubMed] [Google Scholar]
- 54. Harris MI. Racial and ethnic differences in health care access and health outcomes for adults with type 2 diabetes. Diabetes Care. 2001;24(3):454‐459. [DOI] [PubMed] [Google Scholar]
- 55. Heisler M, Smith DM, Hayward RA, Krein SL, Kerr EA. Racial disparities in diabetes care processes, outcomes, and treatment intensity. Med Care. 2003;41(11):1221‐1232. [DOI] [PubMed] [Google Scholar]
- 56. Heltberg A, Andersen JS, Kragstrup J, Siersma V, Sandholdt H, Ellervik C. Social disparities in diabetes care: a general population study in Denmark. Scand J Prim Health Care. 2017;35(1):54‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ibanez B, Galbete A, Goni MJ, et al. Socioeconomic inequalities in cardiometabolic control in patients with type 2 diabetes. BMC Public Health. 2018;18:408. 9 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. James GD, Baker P, Bardrick E, Mathur R, Hull S, Robson J. Ethnic and social disparity in glycaemic control in type 2 diabetes; cohort study in general practice 2004–2009. J R Soc Med. 2012;105:300‐308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Kim D, Choy YS, Park EC. Association between secondhand smoke and glycemic control in adult diabetes patients. Prev Med. 2017;94:48‐54. [DOI] [PubMed] [Google Scholar]
- 60. Lopez L, Grant RW, Marceau L, Piccolo R, McKinlay JB, Meigs JB. Association of acculturation and health literacy with prevalent dysglycemia and diabetes control among Latinos in the Boston Area Community Health (BACH) Survey. J Immigr Minor Health. 2016;18(6):1266‐1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Lynch CP, Williams JLS, Reid J, Joseph R, Keith B, Egede LE. Racial/ethnic differences in multiple diabetes outcomes in patients with type 2 diabetes in the Southeastern United States. Ethn Dis. 2014;24(2):189‐194. [PubMed] [Google Scholar]
- 62. Mainous AG, King DE, Garr DR, Pearson WS. Race, rural residence, and control of diabetes and hypertension. Ann Fam Med. 2004;2(6):563‐568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. McCall DT, Reusch JE, Sauaia A, Barton P, Hamman RF. Are low‐income elderly patients at risk for poor diabetes care? Diabetes Care. 2004;27(5):1060‐1065. [DOI] [PubMed] [Google Scholar]
- 64. McElduff P, Edwards R, Burns JA, et al. Comparison of processes and intermediate outcomes between South Asian and European patients with diabetes in Blackburn, north‐west England. Diabet Med. 2005;22:1226‐1233. [DOI] [PubMed] [Google Scholar]
- 65. Nowlin S, Cleland CM, Parekh N, Hagan H, Melkus G. Racial and ethnic disparities in predictors of glycemia: a moderated mediation analysis of inflammation related predictors of diabetes in the NHANES 2007–2010. Nut Diabetes. 2018;8:56. 12 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Nwasuruba C, Osuagwu C, Bae S, Singh KP, Egede LE. Racial differences in diabetes self‐management and quality of care in Texas. J Diabetes Complications. 2009;23:112‐118. [DOI] [PubMed] [Google Scholar]
- 67. Ortiz SE, Perez DJ, Ponce NA. The quality of diabetes management among Mexican adults in California. Med Care. 2015;53(9):792‐799. [DOI] [PubMed] [Google Scholar]
- 68. Rawshani A, Svensson A‐M, Rosengren A, Zethelius B, Eliasson B, Gudbjornsdottir S. Impact of ethnicity on progress of glycaemic control in 131 935 newly diagnosed patients with type 2 diabetes: a nationwide observational study from the Swedish National Diabetes Register. BMJ. 2015;5:e007599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Saydah S, Cowie C, Eberhardt MS, Rekeneire ND, Narayan KMV. Race and ethnic differences in glycemic control among adults with diagnosed diabetes in the United States. Ethn Dis. 2007;17: 529‐535. [PubMed] [Google Scholar]
- 70. Selby JV, Swain BE, Gerzoff RB, et al. Understanding the gap between good processes of diabetes care and poor intermediate outcomes. Med Care. 2007;45(12):1144‐1153. [DOI] [PubMed] [Google Scholar]
- 71. Shani M, Nakar S, Lustman A, Baievsky T, Rosenberg R, Vinker S. Patient characteristics correlated with quality indicator outcomes in diabetes care. Br J Gen Pract. 2010;60:655‐659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Sloan FA, Brown DS, Carlisle ES, Picone GA, , Lee PP. Monitoring visual status: why patients do or do not comply with practice guidelines. Health Serv Res. 2004;39(5): 1429‐1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Tao X, Li J, Zhu X, et al. Association between socioeconomic status and metabolic control and diabetes complications: a cross sectional nationwide study in Chinese adults with type 2 diabetes mellitus. Cardiovasc Diabetol. 2016;15:61. 10 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Toivakka M, Pihlapuro A, Tkkylainen M, Mehtatalo L, Laatikainen T. The usefulness of small area based socioeconomic characteristics in assessing the treatment outcomes of type 2 diabetes patients: a register based mixed effect study. BMC Public Health. 2018;18:1258:7 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Traylor AH, Mangione CM, Subramanian U, Selby JV, Uratsu CS, Schmittdiel JA. Patient race/ethnicity and patient‐physician race/ethnicity concordance in the management of cardiovascular disease risk factors for patients with diabetes. Diabetes Care. 2010;33(3):520‐525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Trevedi AN, Azslavsky AM, Schneider EC, Ayanian JZ. Trends in the quality of care and racial disparities in Medicare managed care. N Engl J Med. 2003;353(7):692‐700. [DOI] [PubMed] [Google Scholar]
- 77. Williams J, Steers WN, Ettner SL, Mangione CM, Duru OK. Cost related nonadherence by medication type among Medicare part D beneficiaries with diabetes. Med Care. 2013;51(2):193‐198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Wong KW, Ho SY, Chao DVK. Quality of diabetes care in public primary care clinics in Hong Kong. Fam Pract. 2012;29:196‐202. [DOI] [PubMed] [Google Scholar]
- 79. Yoo KH, Shin DW, Cho MH, Kim SH, Bahk HJ, Kim SH, Jeong SM, Yun JM, Park JH, Kim H, Cho B. Regional variations in frequency of glycosylated hemoglobin (HbA1c) monitoring in Korea: A multilevel analysis of nationwide data.. Diabetes Research and Clinical Practice. 2017;131:61‐69. [DOI] [PubMed] [Google Scholar]
- 80. Zeng Y, Wu J, Han Y, et al. Educational disparities in the associations between self monitoring of blood glucose and glycemic control in type 2 diabetes patients in Xiamen, China. Journal of Diabetes. 2018;10:715‐723. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1‐S6
Author Matrix


