INTRODUCTION
Ophthalmia neonatorum or neonatal conjunctivitis refers to conjunctival inflammation with associated discharge. Onset is within the first 28 days of life and transmission is by delivery via an infected birth canal. The majority of cases are bacterial, the most common bacterial agent being chlamydia; however, it is crucial to consider a viral cause.1 An often underestimated and potentially blinding cause is the herpes simplex virus (HSV), which although common in adults is rare in infants.2 Despite its rare occurrence, GPs must have a high suspicion of HSV conjunctivitis on initial presentation because misdiagnosis in a newborn with an immature immune system has sight-threatening consequences.1,2 Figures 1–3 show a case example of the consequences of late diagnosis.
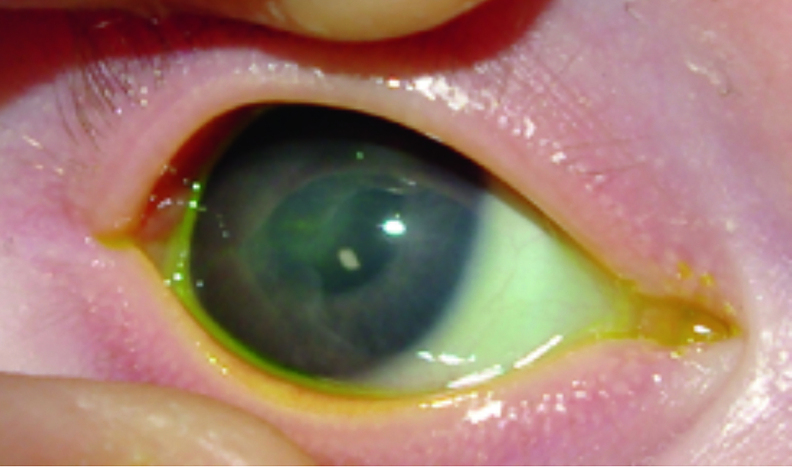
Figure 1.
Mother experienced herpetic genital lesions 2 days after vaginal delivery. Onset of neonate’s symptoms on day 5, treated as bacterial infection. Late diagnosis of HSV-1 at week 3 (fluorescein staining).
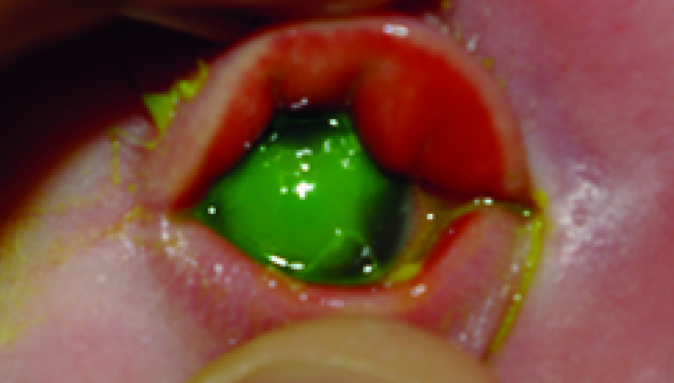
Figure 2.
One week after admission.
Figure 3.
Follow-up 10 months after initial review. Final diagnosis: right-eye herpetic disease (permanent scarring) with secondary glaucoma eventually requiring tube shunt surgery.
HERPES SIMPLEX VIRUS
HSV infections are not always apparent clinically and are common worldwide, with humans being the natural reservoirs. A key feature of HSV-1 and HSV-2 infections is their latency in neural ganglia, a lifelong burden. During its many short reproductive cycles of activation, the virus destroys the host cell while undergoing replication.3,4
HSV-1 and HSV-2 are both causes of eye infections, more commonly HSV-1 in neonates. A large majority of women who pass on the HSV infection to their child have no documented history of genital herpes, partly owing to the subtlety of their clinical symptoms and subsequent misdiagnosis.4 Neonatal HSV infections may be uncommon but the global prevalence is thought to be around 10 per 100 000 live births.3
Transmission is more likely with vaginal delivery and C-sections have been recommended by the Royal College of Obstetricians and Gynaecologists under specific circumstances. Cutaneous damage to the fetal scalp and prolonged duration of rupture of the membranes also carry a higher risk of transmission.3,4
Maternal infections may be:
CLASSIFICATION
PRESENTATION
On presentation, which can be in the first to the fourth week, HSV infections of the eye can be associated with a systemic herpes infection or local skin lesions. Not all cases have a vesicular rash and/or corneal epithelial involvement.3,5
The following localised signs of ocular infection may be unilateral or bilateral:
vesicles on the skin or lid margins;
eyelid oedema;
conjunctival injection (moderate);
conjunctival membrane;
discharge; and
A history of maternal genital herpes is a red-flag symptom. Up to 50% of neonates born via vaginal delivery to mothers with primary genital infections develop an infection themselves.5 Differentiation from blocked nasolacrimal ducts is based on the presence of conjunctival hyperaemia, eyelid swelling, and the relatively early presentation in ophthalmia neonatorum. In particular, cases with presence of corneal haze should be treated as a matter of urgency.
Neonatal ocular HSV is diagnosed by polymerase chain reaction (PCR) of conjunctival swabs. Blood and cerebrospinal fluid (CSF) may also be taken for analysis to exclude CNS and disseminated disease.3–5
MANAGEMENT
Clinically there is an overlap between the HSV disease types and other aetiologies of conjunctival disease (such as gonococcal or chlamydia), which presents a challenge for the primary care physician when deciding on management. An ophthalmic referral should be sought urgently when HSV or any other keratitis is suspected in a neonate.5 Immediate management involves empiric treatment with parenteral aciclovir, ideally in the hospital setting. The recommended treatment is 20 mg/kg three times daily for 14 days (21 days if there is progression to disseminated or CNS disease).2–5
Recurrence in SEM and CNS disease is common. Post-recovery, children should be routinely followed up by ophthalmology and paediatric teams. Many infants require continued suppressive therapy with a lower dose of aciclovir (300 mg/m2/dose three times daily) for 6 months to reduce the frequency of recurrence. Adverse effects of prolonged treatment with aciclovir include neutropaenia, thrombocytopaenia, or elevated creatinine levels. It is wise to check neutrophil counts twice a week while on high-dose aciclovir. This should continue but less frequently while on suppressive therapy along with periodic assessment of kidney and liver function tests.2,3,5
PROGNOSIS
Neonates with HSV infections have varying prognoses determined by the extent of involvement of the disease. Infants with SEM disease have a good prognosis with antiviral therapy. One study reported that 98% of successfully treated neonates had no developmental issues at 12 months of age.3,5
CONCLUSION
There are many aspects of clinical examination and patient history that could cast doubt on the validity of an infection being caused by HSV rather than the more common bacterial causes. For instance, there may be no maternal history of symptoms of genital herpes, no vesicles being visible on initial or even on late presentation of the neonate, or a possible delayed onset of up to 4 weeks after birth.
However, a raised level of awareness should be maintained and an early referral sought, especially if there are any of the above-mentioned warning signs, for example, positive maternal history, corneal haze, conjunctival hyperaemia, or lid swelling associated with ocular discharge. In the hospital the diagnosis is established by obtaining the appropriate cultures for investigation with immediate commencement of empirical treatment, that is, IV aciclovir and subsequent suppressive therapy. Care should be under an ophthalmology team for routine reviews of the disease progress as an inpatient and appropriate follow-up on discharge to monitor for signs of any recurrence.
The most important and commonly reiterated learning point would be vigilance and a high index of suspicion of HSV on the very first presentation, however infrequently these infections may occur in the developed world. Neonates have immature immune systems and should be treated in the same vein as immunocompromised patients. There is a clear trend between the progression to disseminated disease and higher morbidity and mortality, and untimely treatment can lead to lifelong devastating effects for the child that are entirely preventable.
Funding
None.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Patient consent
The patient gave consent for publication of this article and its images.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Palafox SKV, Jasper S, Tauber J, et al. Ophthalmia neonatorum. J Clinic Experiment Ophthalmol. 2011;2:119. [Google Scholar]
- 2.Matos RJC, Peres JMS, Cortesão D. Management of neonatal herpes simplex infection: a rare case of blepharoconjunctivitis and concurrent epithelial and stromal keratitis. Ocul Immunol Inflamm. 2016;26(4):625–627. doi: 10.1080/09273948.2016.1242017. [DOI] [PubMed] [Google Scholar]
- 3.Pinninti SG, Kimberlin DW. Neonatal herpes simplex virus infections. Paediatr Clin North Am. 2013;60(2):351–365. doi: 10.1016/j.pcl.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 4.Scott HJ, Kimberlin DW. Neonatal herpes simplex virus infection: epidemiology and treatment. Clin Perinato. 2015;42(1):47–59. doi: 10.1016/j.clp.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Waggoner-Fountain LA, Grossman LB. herpes simplex virus. Pediatr Rev. 2004;25(3):86–93. doi: 10.1542/pir.25-3-86. [DOI] [PubMed] [Google Scholar]