Abstract
Breast cancer (BC) is the most common female cancer and the second cause of death among women worldwide. The 5-year relative survival rate recently improved up to 90% due to increased population coverage and women’s attendance to organised mammography screening as well as to advances in therapies, especially systemic treatments. Screening attendance is associated with a mortality reduction of at least 30% and a 40% lower risk of advanced disease. The stage at diagnosis remains the strongest predictor of recurrences. Systemic treatments evolved dramatically over the last 20 years: aromatase inhibitors improved the treatment of early-stage luminal BC; targeted monoclonal antibodies changed the natural history of anti-human epidermal growth factor receptor 2-positive (HER2) disease; immunotherapy is currently investigated in patients with triple-negative BC; gene expression profiling is now used with the aim of personalising systemic treatments. In the era of precision medicine, it is a challenging task to define the relative contribution of early diagnosis by screening mammography and systemic treatments in determining BC survival. Estimated contributions before 2000 were 46% for screening and 54% for treatment advances and after 2000, 37% and 63%, respectively. A model showed that the 10-year recurrence rate would be 30% and 25% using respectively chemotherapy or novel treatments in the absence of screening, but would drop to 19% and 15% respectively if associated with mammography screening. Early detection per se has not a curative intent and systemic treatment has limited benefit on advanced stages. Both screening mammography and systemic therapies continue to positively contribute to BC prognosis.
Keywords: Breast neoplasms, Mammography, Cancer screening, Prognosis, Precision medicine
Key points
The stage at diagnosis is still crucial in determining survival outcomes for breast cancer.
Screening attendance is associated with a reduction of advanced-stage disease.
Novel endocrine and anti-human epidermal growth factor receptor 2 (HER2)-targeted therapies have substantially improved survival.
Early diagnosis and personalised treatments synergistically contribute to improve prognosis.
We do still need breast cancer screening in the era of precision medicine.
Introduction
Breast cancer is the most common female cancer worldwide, accounting for 30% of all new cancer diagnoses in women [1]. Social and economic trends are associated with a continuous increase in incidence rates by approximately 0.5% per year [1, 2]. Ageing population, maternity delay and low parity, obesity and sedentary lifestyle – along with an escalation in the diffusion of breast cancer mammography screening – contributed to this increase in high-income countries [2].
Traditionally, survival outcomes are influenced by tumour size, nodal involvement, grade, hormone receptor (HR) and human epidermal growth factor receptor 2 (HER2) status. Although breast cancer remains the second leading cause of death among women after lung cancer, the 5-year relative survival rate in the United States has improved from 79% in 1984–1986 to 91% in 2008–2014 [3, 4]. Similar trends have been observed in Europe: in Italy, survival improved from 80% in 1995 to 88% in 2010 [5].
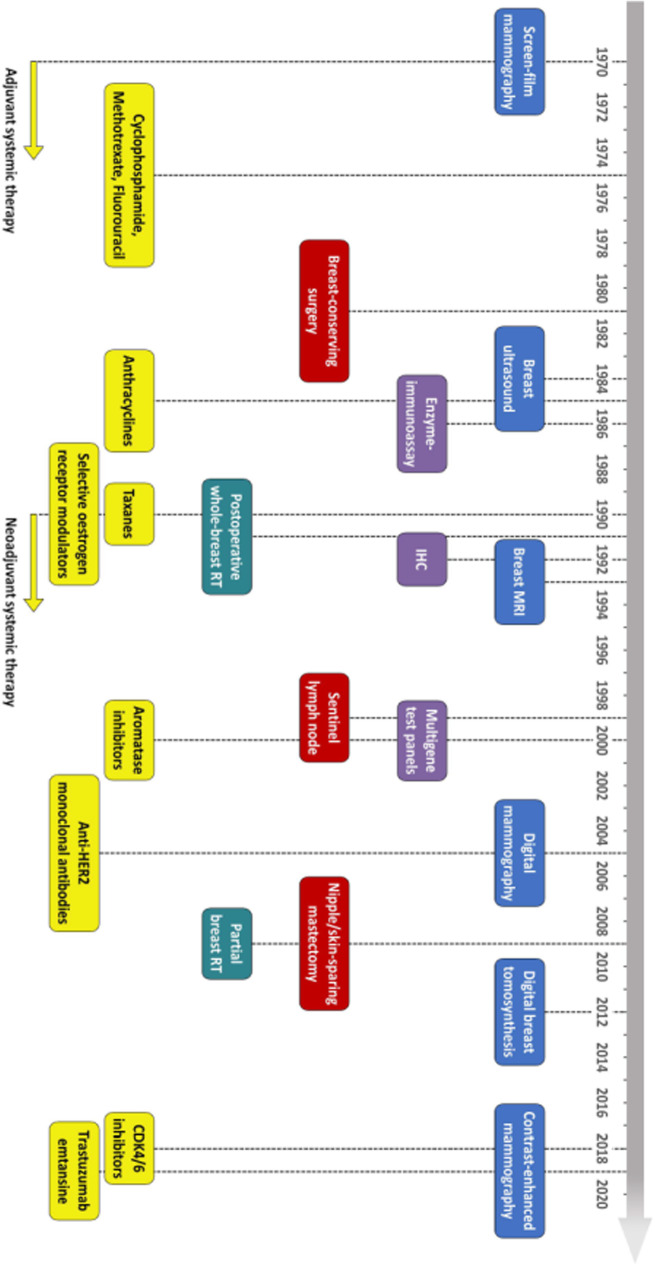
As detailed by the timeline in Fig. 1, breast cancer care has substantially evolved over the past fifty years, with non-negligible changes in screening and diagnostics, histological analysis, surgery, radiation therapy, and systemic treatments. The implementation and diffusion of screening mammography and various improvements in systemic anticancer treatments have been the main drivers of these changes [6]. In Europe, 63.9 million women had access to population-based breast cancer screening in 2016 compared with 54.4 million in 2007, with 88% of the estimated target population completing rollout, compared with 41% in 2007. Nevertheless, a wide geographical variability in invitation coverage still exists [7]. Similarly, in the 2000s, the use of chemotherapy has increased up to 80%, and the use of tamoxifen up to 50% for patients with oestrogen receptor-positive tumours: nowadays, in Italy, about 50% of patients undergoing surgery for stage I–III breast cancer receive systemic treatments that include targeted therapy [8], while in the United States targeted therapy is administered to almost 20% of patients with stage I–II disease and to over 60% of those with stage III disease [9]. Of note, along with traditional prognostic factors, gene expression profiling is now increasingly adopted, aiming to personalise therapeutic approaches and escalate or de-escalate systemic treatments [10]. In this complex framework, an evaluation of the impact of screening and systemic treatments on breast cancer prognosis looks challenging: their relative contribution may substantially differ across countries with different screening attendance rate and access to anticancer treatments.
Fig. 1.
Key advances in the recent history of breast cancer care (the date of introduction of each innovation was based on literature review with reference to first large studies confirming its clinical value). Specific evolutions or improvements are colour-coded. Imaging is in light blue, pathology in violet, surgery in red, radiation therapy in blue-green, systemic treatments in yellow. RT, radiation therapy: IHC, immunohistochemistry; MRI, magnetic resonance imaging; CDK4/6, cyclin-dependent kinase 4/6
Benefits deriving from screening and early diagnosis may become questionable when considering the efficacy of current systemic treatment options. In a theoretical model, a break-even point can be hypothesised when the advantages of early diagnosis by screening are nullified by the efficacy of individualised therapies. Nonetheless, detecting breast cancer before it is no longer curable should still be considered an advantage for the patient, since it remains unlikely that currently available therapies could be so effective without an early diagnosis. Any modification to this balance relies on the potential of systemic treatments to kill cancer cells at any stage, reducing or nullifying the screening benefit.
This critical review highlights the major landmark improvements in mammography screening and systemic treatment, to appraise their impact on breast cancer prognosis and to question the role of breast cancer screening in the era of precision medicine.
Mammography screening
Mammography screening was introduced in 1956 for the “detection of early cancer of the breast” [11]. In the 1970s, several randomised controlled trials confirmed a beneficial improvement of mammography screening on breast cancer mortality [12]. Such benefit pertains to women aged 50 to 74 years and is maximal, about 30%, in those aged 60 to 69 years [13–16]. Mammography screening programs have the general aim of reducing breast cancer-specific mortality both by minimising the risk of diagnosing breast cancer in the advanced stage and by maximising the efficacy and safety of anticancer treatments and their impact on prognosis.
The first x-ray units dedicated to mammography used x-ray film and paired fluorescent screens to capture the image, in the so-called screen-film mammography, which has been gradually replaced since the early 2000s by digital mammography units. In 2005, a landmark study by Pisano et al. [17] compared the diagnostic accuracy of digital and screen-film mammography in 42,760 asymptomatic women. At receiver operating characteristic analysis over the entire population, the areas under the curve (AUCs) of the two methods differed by a non-significant 0.03. However, the digital technique was significantly superior among women over 50 (0.15 AUC difference), among women having heterogeneously or extremely dense breasts (0.11 AUC difference), and among women being in pre- or perimenopause (0.15 AUC difference). Digital mammography allowed also to deliver a lower radiation dose and resulted in easier image storage and subsequent access. Its initially higher costs dwindled quite quickly, its uptake steadily increased [18, 19]. By 2015, 96% of all mammography units in the United States had gone digital [20].
The incidence of advanced-stage tumours in the target population is a specific proxy indicator of screening efficacy, given the absence of confounding effects of treatments at the time of diagnosis. However, studies on this topic have adopted different thresholds in defining the severity of the diseases and are characterised by poor to fair overall quality. Nevertheless, a meta-analysis of trials combined their results – including the most severe disease categories available – and showed a significant reduction in the risk of advanced-stage disease for women aged 50 years or older (relative risk 0.62, 95% confidence interval [CI] 0.46–0.83) randomly assigned to undergo screening: this benefit was however not seen in women aged 39 to 49 years [14].
More recently, a prospective Italian cohort study was conducted on 413,447 women undergoing screening in the 1990s and followed up for 13 years as part of the IMPACT project [21]. Screening attendance was positively associated with: (a) a 39% reduction of the incidence of pT2–T4 lesions (66.3‰ versus 108.6‰, incidence rate ratio 0.61, 95% CI 0.57–0.66), including a 28% reduction of pT2 lesions and a 68% reduction of pT3–T4 lesions; (b) a 28% reduction in the incidence of stage II–IV disease (130.1‰ versus 180.6‰, incidence rate ratio 0.72, 95% CI 0.68–0.76), including a 35% reduction of stage IIB, a 43% reduction of stage III, and a 73% reduction of stage IV. Notably, patients undergoing screening also benefited from a 17% reduction in the incidence of poorly differentiated carcinomas and from a 50% increase of breast-conserving surgery rates. These results were also confirmed following adjustments to exclude self-selection bias, a significant reduction in the use of mastectomy being also observed [22].
Another interesting large population study – including 549,091 women across nine Swedish counties [23] – was conducted to evaluate the impact of screening mammography on breast cancer mortality. The study used an analytic strategy focusing on the incidence of fatal breast cancers within 10 years from the date of diagnosis, whereas other studies had been retroactively considering 10 years from the date of death. Women who attended mammography screening had a significant 41% reduction in their risk of dying of breast cancer within 10 years (relative risk 0.59, 95% CI 0.51–0.68) and a 25% reduction in the rate of advanced breast cancer (relative risk 0.75, 95% CI 0.66–0.84), regardless of the recent improvements in systemic treatments.
In 2019, the American Cancer Society and the National Cancer Institute published cancer treatment and survivorship statistics in the United States. Most patients (44%) were diagnosed with stage I disease, 30% with stage II, 9% with stage III and 5% with stage IV. The 5-year breast cancer relative survival ranged from approximately 100% for stage I disease to 26% for stage IV breast cancer [9]. Interestingly, in 2018 Mariotto et al. [24] provided the first population-based summaries of the risk of breast cancer recurrence in United States women, using cancer registry disease-specific survival: stage remained the strongest predictor of the risk of recurrence, along with age (60–74 years) and HR-negative status. Thus, we can still affirm that tumour stage has a substantial impact on prognosis and on the risk of disease recurrence.
Systemic treatments
Chemotherapy has been used in the adjuvant setting since the early 1970s when landmark studies in the United States and in Italy documented a benefit of regimens such as L-phenylalanine mustard or the combination of cyclophosphamide, methotrexate and 5-fluorouracil (CMF) in patients with node-positive breast cancer [25, 26]. In the 1980s and 1990s, anthracyclines and taxanes proved to be more effective than CMF [27]; in the meantime, tamoxifen was found to substantially improve the survival of women with HR-positive tumours [28], and later on, aromatase inhibitors (AIs) proved to further improve outcomes in postmenopausal patients. During the 2000s, anti-HER2 therapies were developed as one of the first targeted systemic treatment options, changing dramatically the management and prognosis of HER2-positive breast cancer; in the same decade, genome expression profiling was deployed in routine practice, further improving the personalisation of breast cancer treatments [29]. Nonetheless, patient selection remains crucial to maximise efficacy and safety of systemic treatments. The current standard of care for different disease subtypes is summarised below.
Luminal breast cancer
The introduction of AIs has been a key improvement in the management of HR-positive, HER2-negative breast cancer [9, 30]. Nowadays, AIs are standard of care for postmenopausal women, based on several studies that have documented better recurrence-free survival and disease-specific mortality in women treated with AIs compared with tamoxifen [19]. Two large phase III studies (the SOFT and TEXT studies) confirmed the role of AIs also for premenopausal patients and/or with high-risk disease, along with ovarian function suppression justified by a recurrence-free survival benefit [31]. An extended course of adjuvant endocrine therapy may also further improve outcomes, especially following upfront use of tamoxifen [32–39], since late recurrences remain a relevant issue for patients with luminal breast cancer [40]. Cyclin-dependent kinase 4/6 inhibitors are also being investigated in the adjuvant setting in several clinical trials [41–44], which might in due course change the current treatment paradigm in this setting.
HER2-positive breast cancer
Targeted agents are the foundation of precision medicine, which involves the use of drugs interfering with specific molecular alterations that drive tumour growth and spread: for example, targeted anti-HER2 agents have radically changed the natural history and prognosis of HER2-positive disease. The use of the anti-HER2 monoclonal antibody trastuzumab for 1 year, along with chemotherapy, is now standard of care for tumours with a size of 5 mm or greater and for tumours of any size with nodal involvement, based on the substantial disease-free and overall survival benefits that have been reported when compared with the use of chemotherapy alone (disease-free survival, hazard ratio for recurrence 0.60, 95% CI 0.50–0.71; overall survival, hazard ratio for mortality 0.66, 95% CI 0.57–0.77) [45]. Moreover, additional benefits have been documented with adjuvant treatment escalation in higher-risk tumours: adding novel anti-HER2 agents, such as pertuzumab and neratinib, improves disease-free survival in women with node-positive disease [46] and recurrence rates in patients with large and HR-positive, HER2-positive tumours [47]. On the other hand, adjuvant treatment de-escalation has been investigated for patients with a lower risk of breast cancer recurrence in order to minimise the impact of systemic treatment on safety and quality of life [48]. Response to preoperative systemic treatment is a prognostic factor in patients with HER2-positive breast cancer, with better survival outcomes in patients without invasive disease at the surgical specimen, defined as ypT0/Tis ypN0 [49]. Therefore, neoadjuvant systemic treatment remains a very reasonable approach [50] and the addition of pertuzumab to trastuzumab to chemotherapy has become a standard of care, considering the improvements in pathological complete response rates [51, 52].
Triple-negative breast cancer
The systemic treatment of HR-negative and HER2-negative breast cancer is still largely limited to the use of chemotherapy. Adjuvant chemotherapy remains standard of care for patients with triple-negative breast cancers, either of 5 mm or greater or with pathologically involved lymph nodes [53]. In this specific setting, several trials are currently investigating the role of novel agents such as immunotherapy, which aims to boost the immune response against the tumour [54–56]. Neoadjuvant chemotherapy is the preferable approach in patients with locally advanced disease or in those who are not candidates for upfront surgery. Nonetheless, the role of neoadjuvant systemic therapy has also expanded, aiming to improve surgical operability and cosmetic outcomes but also to test the chemosensitivity of breast cancer in vivo, which has relevant prognostic implications [49, 57].
Gene expression profiling
Genomics and the ability to evaluate simultaneously the expression of multiple genes led to the development of gene expression profiles, which have been validated to identify patients with a higher risk of disease recurrence who may benefit from the use of adjuvant chemotherapy. Oncotype Dx has been validated both as a prognostic and a predictive tool, although Mammaprint [58], EndoPredict [59, 60], Breast Cancer Index [61] and Predictor Analysis of Microarray 50 (PAM50) [62, 63] may also be used. Oncotype Dx identifies women with node-negative, HR-positive breast cancer whose prognosis is so favourable that the absolute benefit of chemotherapy is likely to be very low. Patients with HR-positive node-negative cancers derive substantial benefit from chemotherapy when their score is high, typically higher than 25. On the other hand, if their score is low or midrange (lower than 25), adding chemotherapy to endocrine treatment for women over 50 showed no benefit, although younger women may experience some benefit [64, 65]. While the use of Oncotype Dx in patients with node-positive, HR-positive breast cancer is supported by less robust evidence, it has been considered [66] and is currently being investigated [67].
The winning weapon: mammography screening plus systemic treatments
Defining the relative contribution of screening mammography and systemic treatments to improve breast cancer outcomes is a challenging task. The increasing use of screening and the gradual implementation of more effective therapeutic approaches occurred over nearly the same period since the 1970s. In the meantime, breast surgery has also evolved, along with the introduction of sentinel lymph node biopsy and radiation therapy. Overall, each of all these developments substantially contributed to improve patient outcome.
The Cancer Intervention and Surveillance Modelling Network used modelling techniques to provide estimates of the contributions of screening mammography and adjuvant treatment to the reduction of breast cancer mortality in the United States from 1975 to 2000 [68]. Seven independent statistical models were developed and yielded similar qualitative conclusions, namely that “the decline in mortality rate can be explained by a combination of screening and therapy and not by either one alone”. The proportion of the total reduction in the rate of death from breast cancer attributed to screening varied in the seven models from 28% to 65% (median 46%). On the other hand, the contribution of systemic therapy including chemotherapy and tamoxifen varied from 35% to 72% (median 54%): differences in these estimates reflect the mutual interaction between the two interventions [68].
Saadatmand et al. [69] investigated – in a large population-based cohort study – whether tumour stage at diagnosis still influences survival in the context of the current therapeutic approaches. This prospective nationwide population-based study was conducted in the Netherlands and included 173,797 women diagnosed with breast cancer, with two cohorts being identified according to the year of breast cancer diagnosis. A total of 80,228 patients were diagnosed with breast cancer from 1999 to 2005, while 93,569 from 2006 to 2012: in this second period – following national guidelines – systemic therapy was more widely used. At univariate and multivariate analyses, tumour stage and nodal status significantly influenced overall and relative survival in both cohorts. Relative survival rates ranged from almost 100% in both cohorts for in situ tumours to 57% and 59% for T4 tumours in the older and more recent cohort, respectively. At multivariate analysis, breast-conserving treatment (more frequently pursued in the 2006–2012 cohort) resulted in a significant survival benefit compared with mastectomy, whereas lymph node dissection (less frequently pursued) was associated with a significantly worse overall survival. The wider use of chemotherapy in the 2006–2012 cohort conferred a hazard ratio for death of 0.86 (95% CI 0.80–0.92). These large-scale results clearly demonstrate that while the use of chemotherapy may impact on survival, tumour size at diagnosis still matters. Authors concluded that “in the current era of effective systemic therapy, diagnosis of breast cancer at an early stage remains vital” [69]. Moreover, considering United States women diagnosed with breast cancer at age 60–74, summaries of the risk of breast cancer recurrence showed a 5-year recurrence rate of 2.5%, 9.6% and 34.5% for stages I, II and III HR-positive breast cancers, and a 5-year recurrence rate of 6.5%, 20.2% and 48.5% for stages I, II and III HR-negative breast cancers [24].
Another study from the United States [6] also assessed to what extent digital mammography screening and novel systemic therapies contributed to the improvement in breast cancer mortality in different disease subtypes from 2000 to 2012: its results are summarised in Table 1. Complex simulation models from the Cancer Intervention and Surveillance Network projecting breast cancer mortality trends for women aged 30 to 79 years estimated a 12% difference (model range, 10–16%) in the overall disease-specific mortality reduction between 2000 (37%, model range, 27–42%) and 2012 (49%, model range, 39–58%). The relative contribution to the decrease in overall breast cancer mortality in 2012 was 37% (model range, 26–51%) for screening and 63% (model range, 49–74%) for treatment. Of the 37% mortality reduction associated with screening in 2012, 33% (model range, 29–48%) was associated with screening advances before 2000 and 4% (model range, 1–8%) after 2000 (the shift from screen-film to digital mammography was relatively less relevant than previous improvements when considering the conspicuous advancements in therapeutic options). Similarly, of the 63% mortality reduction associated with treatments in 2012, 32% was associated with chemotherapy, 27% with hormone therapy and 4% with trastuzumab. Of the 31% mortality reduction (model range, 23–37%) associated with chemotherapy, 9% (model range, 7–14%) was associated with chemotherapy advances after 2000 (largely taxanes). Of the 27% mortality reduction (model range, 18–36%) associated with hormone therapy, 7% (model range, 2–12%) was associated with advances in hormone therapy after 2000 (largely from AIs) [6].
Table 1.
Association of screening and treatment with breast cancer mortality in US women from 2000 to 2012
| Mortality reduction compared to 1975 (%) | Contribution to the difference in mortality reduction in 2012 versus 2000 (%) | ||||||
|---|---|---|---|---|---|---|---|
| In 2000a | In 2012b | Difference | Screening advances | Chemotherapy advances | Hormone therapy advances | Trastuzumab | |
| Overall | 37 | 49 | 12 | 17 | 38 | 29 | 15 |
| ER+/HER2− | 39 | 51 | 12 | 19 | 39 | 42 | 0 |
| ER+/HER2+ | 39 | 58 | 19 | 12 | 22 | 25 | 41 |
| ER−/HER2+ | 29 | 45 | 16 | 11 | 32 | 0 | 57 |
| ER−/HER2− | 29 | 37 | 8 | 22 | 78 | 0 | 0 |
aRelative to the estimated baseline rate of 64 deaths (model range, 56–73) per 100,000 women in 2000; bRelative to the estimated baseline rate of 63 deaths (model range, 54–73) per 100,000 women in 2012. ER oestrogen receptor, HER2 human epidermal growth factor receptor 2. Source: Plevritis et al. [6]
Subtype analyses also demonstrated significant variations in the relative contribution of screening and treatment to the mortality reduction in different tumour molecular subtypes. The largest benefit of screening (48%, model range, 38–57%) was found in the triple-negative tumour breast cancer cohort, while the largest benefit of treatment (69%, model range, 59–77%) was documented in luminal tumours. According to this model-based analysis, both screening and treatment contributed and still contribute to the improvement in breast cancer mortality, with progressively greater contributions of therapeutic advances in the last decades [6].
The relative contribution associated with mammography screening and advances in systemic therapies to the reduction in the recurrence rate is simulated in Figs. 2 and 3. Here, four scenarios combine variably the contribution of screening mammography and chemotherapy or novel systemic treatments (i.e. AIs and targeted agents). In this simulation, stage distribution was derived from Puliti et al. [21], considering attenders and non-attenders to mammography screening and adjusted for self-selection. A 5% overdiagnosis attributed to population screening has been considered when it was included in the scenario. Ten-year disease-specific survival for HR-positive and HR-negative cancers was retrieved from Mariotto et al. [24], based on women aged 60–74 years treated in the 1992–1999 period or in the 2000–2013 period, when more advanced therapies were available. This simulation shows how combining screening mammography and novel systemic agents represent the most favourable scenario with the lowest number of recurrences, also detailing how the recurrence rate at 10 years would be 30% for chemotherapy without screening and 19% for chemotherapy with screening, 25% for novel treatments without screening and 15% for novel treatments with screening.
Fig. 2.
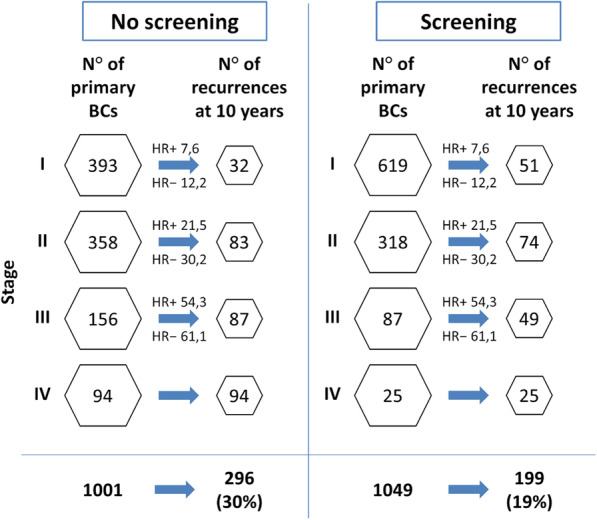
Effect of screening and chemotherapy on breast cancer recurrences among women aged 60 to 74 years, diagnosed with breast cancer between 1992 and 1999. Stage distribution was derived from Puliti et al. [21] considering attenders and non-attenders to screening mammography; 5% overdiagnosis attributed to screening mammography is taken into account. HR+ and HR− recurrences are back-calculated from Mariotto et al. [24]. The worst scenario reflects the absence of mammography screening and the use of chemotherapy alone. BCs, breast cancers; HR+, hormone receptor-positive breast cancers; HR−, hormone receptor-negative breast cancers
Fig. 3.
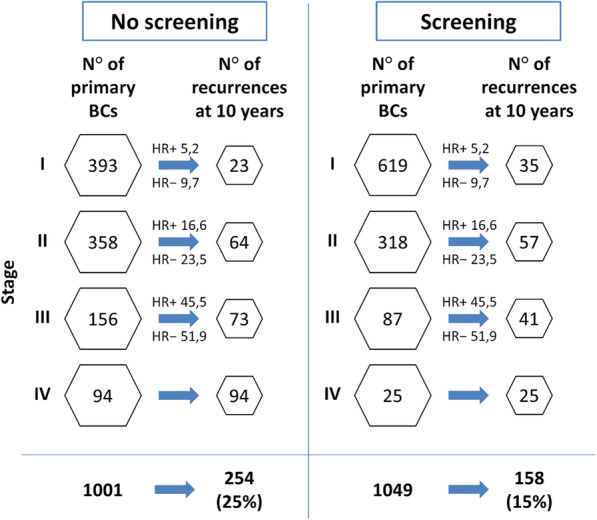
Effect of screening and novel systemic treatments on breast cancer recurrences among women aged 60 to 74 years, diagnosed with breast cancer between 2000 and 2013. Stage distribution was derived from Puliti et al. [21] considering attenders and non-attenders to screening mammography; a 5% overdiagnosis attributed to screening mammography was taken into account. HR+ and HR− recurrences are back-calculated from Mariotto et al. [24]. The most favourable scenario arises from the use of mammography screening associated with novel systemic treatments. BCs, breast cancers; HR+, hormone receptor-positive breast cancers; HR−, hormone receptor-negative breast cancers
Two important aspects should however be considered in the analysis of the evolution of screening and systemic therapies. Despite the widespread use of screening mammography, the introduction of digital techniques represents the most important technical advancement: of note, tomosynthesis has become the technique of choice for symptomatic women and those who are recalled for further assessment after a screening mammogram [13]. Conversely, the evidence in favour of its use as a first-level screening tool is still not sufficient in terms of reduction of interval cancer rate (possibly due to an underlying rate of overdiagnosis [70–73]) and European guidelines [13] have advised against its use for population-based screening programs. On the other hand, increasingly effective novel systemic treatment options are being introduced as a standard of care and gene expression profiling is progressively enabling better decision-making.
This is once again a turning point. In case of further outcome improvements, most of the contribution would then be attributable to better systemic treatments. Nevertheless, MRI [74] and other novel imaging modalities, such as contrast-enhanced mammography [75–77] could come to be considered screening tools in selected populations, their contribution being also promising. Furthermore, a recent survey among members of the European Society of Radiology [78] showed that there are high expectations on the use of artificial intelligence [79, 80]. Dedicated algorithms will focus on personalised risk prediction and prognosis [81] and machine/deep learning software has already shown high performance in interpreting screening mammography. Finally, the availability of molecular analyses on liquid biopsy could represent another promising option [82, 83].
However, further widespread benefits in breast cancer outcomes are expected to become ever slimmer in the context of the efficacy of the current standard treatments: research efforts will therefore need to focus on the role of precision medicine. Once outcomes are maximal in the overall breast cancer patient population, improvements might indeed be sought in selected populations and especially in those with poor prognosis.
Conclusions
The increasing use of screening mammography and improvements in systemic treatments have substantially reduced breast cancer mortality over the last two decades. However, defining their relative contribution to improving outcomes remains a challenging task. Early detection is crucial if followed by effective treatments. Nonetheless, treatments are still less effective in the case of advanced-stage disease. Prevention and early diagnosis contributed to almost half of the reduction in breast cancer mortality, whereas the rest is due to advances in breast cancer treatment, whose role and contribution has become predominant since the early 2000s. In the era of precision medicine, early detection remains crucial and a delay in breast cancer diagnosis, with a tumour detected at an advanced stage, can substantially increase mortality. Screening mammography and systemic anticancer treatment are synergistic in improving breast cancer prognosis.
Abbreviations
- AIs
Aromatase inhibitors
- AUC
Area under the curve
- CI
Confidence interval
- CMF
Cyclophosphamide, methotrexate, and 5-fluorouracil
- HER2
Human epidermal growth factor receptor 2
- HR
Hormone receptor
Authors’ contributions
All authors contributed to the conception and design of this work as well as to the writing and revision phases of the manuscript. All authors read and approved the final manuscript.
Funding
Paolo Giorgi Rossi participated thanks to the Innovative Partnership for Action Against Cancer (iPAAC) EC funded project.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
R. M. Trimboli, P. Giorgi Rossi, N. M. L. Battisti, A. Cozzi, V. Magni, and M. Zanardo all declare that they have no conflicts of interest and nothing to disclose. F. Sardanelli declares to have received grants from or to be a member of the speakers’ bureau/advisory board for Bayer Healthcare, Bracco Imaging, and General Electric.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rubina Manuela Trimboli, Email: trimboli.rm@gmail.com.
Paolo Giorgi Rossi, Email: paolo.giorgirossi@ausl.re.it.
Nicolò Matteo Luca Battisti, Email: nicolo.battisti@rmh.nhs.uk.
Andrea Cozzi, Email: andrea.cozzi1@unimi.it.
Veronica Magni, Email: veronica.magni@studenti.unimi.it.
Moreno Zanardo, Email: moreno.zanardo@unimi.it.
Francesco Sardanelli, Email: francesco.sardanelli@unimi.it.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 2.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. 10.3322/caac.21492 [DOI] [PubMed]
- 3.Hendrick RE, Baker JA, Helvie MA. Breast cancer deaths averted over 3 decades. Cancer. 2019;125:1482–1488. doi: 10.1002/cncr.31954. [DOI] [PubMed] [Google Scholar]
- 4.Howlader N, Noone AM, Krapcho M et al. (eds). SEER Cancer Statistics Review, 1975-2017, National Cancer Institute, Bethesda, MD. https://seer.cancer.gov/csr/1975_2017/. Accessed 31 August 2020
- 5.Coviello V, Buzzoni C, Fusco M, et al. Survival of cancer patients in Italy. Epidemiol Prev. 2017;41:1–244. doi: 10.19191/EP17.2S1.P001.017. [DOI] [PubMed] [Google Scholar]
- 6.Plevritis SK, Munoz D, Kurian AW, et al. Association of screening and treatment with breast cancer mortality by molecular subtype in US women, 2000-2012. JAMA. 2018;319:154–164. doi: 10.1001/jama.2017.19130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Basu P, Ponti A, Anttila A, et al. Status of implementation and organization of cancer screening in the European Union member states-summary results from the second European screening report. Int J Cancer. 2018;142:44–56. doi: 10.1002/ijc.31043. [DOI] [PubMed] [Google Scholar]
- 8.Mangone L, Mancuso P, Tagliabue G, et al. Neoadjuvant therapy for breast cancer. Tumori. 2019;105:488–493. doi: 10.1177/0300891619869505. [DOI] [PubMed] [Google Scholar]
- 9.Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69:363–385. doi: 10.3322/caac.21565. [DOI] [PubMed] [Google Scholar]
- 10.Curigliano G, Burstein HJ, Winer EP, et al. De-escalating and escalating treatments for early-stage breast cancer: the St. Gallen international expert consensus conference on the primary therapy of early breast cancer 2017. Ann Oncol. 2017;28:1700–1712. doi: 10.1093/annonc/mdx308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cohen JG, Ingleby H, Moore L. Can mass x-ray surveys be used in detection of early cancer of the breast? J Am Med Assoc. 1956;161:1069–1071. doi: 10.1001/jama.1956.62970110003010a. [DOI] [PubMed] [Google Scholar]
- 12.Frigerio A, Sardanelli F, Podo F, et al. Radiological screening of breast cancer: evolution. In: Veronesi U, Goldhirsch A, Veronesi P, et al., editors. Breast Cancer. Cham: Springer International Publishing; 2017. pp. 171–203. [Google Scholar]
- 13.Schünemann HJ, Lerda D, Quinn C, et al. Breast cancer screening and diagnosis: a synopsis of the European breast guidelines. Ann Intern Med. 2020;172:46–56. doi: 10.7326/M19-2125. [DOI] [PubMed] [Google Scholar]
- 14.Nelson HD, Pappas M, Cantor A, et al. Harms of breast cancer screening: systematic review to update the 2009 U.S. Preventive Services Task Force recommendation. Ann Intern Med. 2016;164:256–267. doi: 10.7326/M15-0970. [DOI] [PubMed] [Google Scholar]
- 15.Nelson HD, Fu R, Cantor A, et al. Effectiveness of breast cancer screening: systematic review and meta-analysis to update the 2009 U.S. Preventive Services Task Force recommendation. Ann Intern Med. 2016;164:244–255. doi: 10.7326/M15-0969. [DOI] [PubMed] [Google Scholar]
- 16.Klarenbach S, Sims-Jones N, Lewin G, et al. Recommendations on screening for breast cancer in women aged 40–74 years who are not at increased risk for breast cancer. CMAJ. 2018;190:E1441–E1451. doi: 10.1503/cmaj.180463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pisano ED, Gatsonis C, Hendrick E, et al. Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med. 2005;353:1773–1783. doi: 10.1056/NEJMoa052911. [DOI] [PubMed] [Google Scholar]
- 18.Sardanelli F, Fallenberg EM, Clauser P, et al. Mammography: an update of the EUSOBI recommendations on information for women. Insights Imaging. 2017;8:11–18. doi: 10.1007/s13244-016-0531-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sardanelli F, Aase HS, Álvarez M, et al. Position paper on screening for breast cancer by the European Society of Breast Imaging (EUSOBI) and 30 national breast radiology bodies from Austria, Belgium, Bosnia and Herzegovina, Bulgaria, Croatia, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Israel, Lithuania, Moldova, The Netherlands, Norway, Poland, Portugal, Romania, Serbia, Slovakia, Spain, Sweden, Switzerland and Turkey. Eur Radiol. 2017;27:2737–2743. doi: 10.1007/s00330-016-4612-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hendrick RE, Ikeda DM, Miyake KK. Mammography acquisition. In: Ikeda DM, Miyake KK, editors. Breast imaging: the requisites. 3. St. Louis: Elsevier; 2017. pp. 30–75. [Google Scholar]
- 21.Puliti D, Bucchi L, Mancini S, et al. Advanced breast cancer rates in the epoch of service screening: The 400,000 women cohort study from Italy. Eur J Cancer. 2017;75:109–116. doi: 10.1016/j.ejca.2016.12.030. [DOI] [PubMed] [Google Scholar]
- 22.Zorzi M, Puliti D, Vettorazzi M, et al. Mastectomy rates are decreasing in the era of service screening: a population-based study in Italy (1997–2001) Br J Cancer. 2006;95:1265–1268. doi: 10.1038/sj.bjc.6603405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duffy SW, Tabár L, Yen AM, et al. Mammography screening reduces rates of advanced and fatal breast cancers: Results in 549,091 women. Cancer. 2020;126:2971–2979. doi: 10.1002/cncr.32859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mariotto AB, Zou Z, Zhang F, et al. Can we use survival data from cancer registries to learn about disease recurrence? the case of breast cancer. Cancer Epidemiol Biomarkers Prev. 2018;27:1332–1341. doi: 10.1158/1055-9965.EPI-17-1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bonadonna G, Brusamolino E, Valagussa P, et al. Combination chemotherapy as an adjuvant treatment in operable breast cancer. N Engl J Med. 1976;294:405–410. doi: 10.1056/NEJM197602192940801. [DOI] [PubMed] [Google Scholar]
- 26.Fisher B, Carbone P, Economou SG, et al. L-phenylalanine mustard (L-PAM) in the management of primary breast cancer. N Engl J Med. 1975;292:117–122. doi: 10.1056/NEJM197501162920301. [DOI] [PubMed] [Google Scholar]
- 27.Munzone E, Curigliano G, Burstein HJ, et al. CMF revisited in the 21st century. Ann Oncol. 2012;23:305–311. doi: 10.1093/annonc/mdr309. [DOI] [PubMed] [Google Scholar]
- 28.(1998) Tamoxifen for early breast cancer: an overview of the randomised trials. Early Breast Cancer Trialists’ Collaborative Group. Lancet 351:1451–1467. 10.1016/S0140-6736(97)11423-4 [PubMed]
- 29.Andre F, Pusztai L. Molecular classification of breast cancer: implications for selection of adjuvant chemotherapy. Nat Clin Pract Oncol. 2006;3:621–632. doi: 10.1038/ncponc0636. [DOI] [PubMed] [Google Scholar]
- 30.Loibl S, Gianni L. HER2-positive breast cancer. Lancet. 2017;389:2415–2429. doi: 10.1016/S0140-6736(16)32417-5. [DOI] [PubMed] [Google Scholar]
- 31.Francis PA, Pagani O, Fleming GF, et al. Tailoring adjuvant endocrine therapy for premenopausal breast cancer. N Engl J Med. 2018;379:122–137. doi: 10.1056/NEJMoa1803164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Davies C, Pan H, Godwin J, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381:805–816. doi: 10.1016/S0140-6736(12)61963-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gray RG, Rea D, Handley K, et al. ATTom: Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years in 6,953 women with early breast cancer. J Clin Oncol. 2013;31:5–5. doi: 10.1200/jco.2013.31.18_suppl.5. [DOI] [Google Scholar]
- 34.Goss PE, Ingle JN, Martino S, et al. randomised trial of letrozole following tamoxifen as extended adjuvant therapy in receptor-positive breast cancer: updated findings from NCIC CTG MA.17. JNCI J Natl Cancer Inst. 2005;97:1262–1271. doi: 10.1093/jnci/dji250. [DOI] [PubMed] [Google Scholar]
- 35.Mamounas EP, Jeong J-H, Wickerham DL, et al. Benefit from exemestane as extended adjuvant therapy after 5 years of adjuvant tamoxifen: intention-to-treat analysis of the National Surgical Adjuvant Breast and Bowel Project B-33 trial. J Clin Oncol. 2008;26:1965–1971. doi: 10.1200/JCO.2007.14.0228. [DOI] [PubMed] [Google Scholar]
- 36.Goss PE, Ingle JN, Pritchard KI, et al. Extending aromatase-inhibitor adjuvant therapy to 10 years. N Engl J Med. 2016;375:209–219. doi: 10.1056/NEJMoa1604700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tjan-Heijnen VCG, van Hellemond IEG, Peer PGM, et al. Extended adjuvant aromatase inhibition after sequential endocrine therapy (DATA): a randomised, phase 3 trial. Lancet Oncol. 2017;18:1502–1511. doi: 10.1016/S1470-2045(17)30600-9. [DOI] [PubMed] [Google Scholar]
- 38.Blok EJ, Kroep JR, Meershoek-Klein Kranenbarg E, et al. Optimal duration of extended adjuvant endocrine therapy for early breast cancer; results of the IDEAL trial (BOOG 2006-05) JNCI J Natl Cancer Inst. 2018;110:40–48. doi: 10.1093/jnci/djx134. [DOI] [PubMed] [Google Scholar]
- 39.Mamounas EP, Bandos H, Lembersky BC, et al. Use of letrozole after aromatase inhibitor-based therapy in postmenopausal breast cancer (NRG Oncology/NSABP B-42): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20:88–99. doi: 10.1016/S1470-2045(18)30621-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pan H, Gray R, Braybrooke J, et al. 20-year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years. N Engl J Med. 2017;377:1836–1846. doi: 10.1056/NEJMoa1701830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Diéras V, Rugo HS, Schnell P, et al. Long-term pooled safety analysis of palbociclib in combination with endocrine therapy for HR+/HER2- advanced breast cancer. JNCI J Natl Cancer Inst. 2019;111:419–430. doi: 10.1093/jnci/djy109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.A study of palbociclib in addition to standard endocrine treatment in hormone receptor positive HER2 normal patients with residual disease after neoadjuvant chemotherapy and surgery (PENELOPE-B). https://clinicaltrials.gov/ct2/show/study/NCT01864746. Accessed 31 August 2020
- 43.Endocrine therapy with or without abemaciclib (LY2835219) following surgery in participants with breast cancer (monarchE). https://clinicaltrials.gov/show/NCT03155997. Accessed 31 August 2020
- 44.A trial to evaluate efficacy and safety of ribociclib with endocrine therapy as adjuvant treatment in patients With HR+/HER2- early breast cancer (NATALEE). https://clinicaltrials.gov/show/NCT03701334. Accessed 31 August 2020
- 45.Moja L, Tagliabue L, Balduzzi S, et al. Trastuzumab containing regimens for early breast cancer. Cochrane Database Syst Rev. 2012;2012:CD006243. doi: 10.1002/14651858.CD006243.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.von Minckwitz G, Procter M, de Azambuja E, et al. Adjuvant pertuzumab and trastuzumab in early HER2-positive breast cancer. N Engl J Med. 2017;377:122–131. doi: 10.1056/NEJMoa1703643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martin M, Holmes FA, Ejlertsen B, et al. Neratinib after trastuzumab-based adjuvant therapy in HER2-positive breast cancer (ExteNET): 5-year analysis of a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2017;18:1688–1700. doi: 10.1016/S1470-2045(17)30717-9. [DOI] [PubMed] [Google Scholar]
- 48.Tolaney SM, Guo H, Pernas S, et al. Seven-year follow-up analysis of adjuvant paclitaxel and trastuzumab trial for node-negative, human epidermal growth factor receptor 2–positive breast cancer. J Clin Oncol. 2019;37:1868–1875. doi: 10.1200/JCO.19.00066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cortazar P, Zhang L, Untch M, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–172. doi: 10.1016/S0140-6736(13)62422-8. [DOI] [PubMed] [Google Scholar]
- 50.Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) (2018) Long-term outcomes for neoadjuvant versus adjuvant chemotherapy in early breast cancer: meta-analysis of individual patient data from ten randomised trials. Lancet Oncol 19:27–39. 10.1016/S1470-2045(17)30777-5 [DOI] [PMC free article] [PubMed]
- 51.Gianni L, Pienkowski T, Im Y-H, et al. 5-year analysis of neoadjuvant pertuzumab and trastuzumab in patients with locally advanced, inflammatory, or early-stage HER2-positive breast cancer (NeoSphere): a multicentre, open-label, phase 2 randomised trial. Lancet Oncol. 2016;17:791–800. doi: 10.1016/S1470-2045(16)00163-7. [DOI] [PubMed] [Google Scholar]
- 52.Schneeweiss A, Chia S, Hickish T, et al. Pertuzumab plus trastuzumab in combination with standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2-positive early breast cancer: a randomised phase II cardiac safety study (TRYPHAENA) Ann Oncol. 2013;24:2278–2284. doi: 10.1093/annonc/mdt182. [DOI] [PubMed] [Google Scholar]
- 53.Burstein HJ, Curigliano G, Loibl S, et al. Estimating the benefits of therapy for early-stage breast cancer: the St. Gallen international consensus guidelines for the primary therapy of early breast cancer 2019. Ann Oncol. 2019;30:1541–1557. doi: 10.1093/annonc/mdz235. [DOI] [PubMed] [Google Scholar]
- 54.Nanda R, Liu MC, Yau C, et al. Pembrolizumab plus standard neoadjuvant therapy for high-risk breast cancer (BC): Results from I-SPY 2. J Clin Oncol. 2017;35:506–506. doi: 10.1200/JCO.2017.35.15_suppl.506. [DOI] [Google Scholar]
- 55.Schmid P, Cortes J, Pusztai L, et al. Pembrolizumab for early triple-negative breast cancer. N Engl J Med. 2020;382:810–821. doi: 10.1056/NEJMoa1910549. [DOI] [PubMed] [Google Scholar]
- 56.Gianni L, Huang C-S, Egle D et al (2020) Abstract GS3-04: Pathologic complete response (pCR) to neoadjuvant treatment with or without atezolizumab in triple negative, early high-risk and locally advanced breast cancer. NeoTRIPaPDL1 Michelangelo randomised study. In: Proceedings of the 2019 San Antonio Breast Cancer Symposium; 2019 Dec 10–14; San Antonio, TX. Philadelphia (PA): AACR; Cancer Res 2020;80(4 Suppl):Abstract nr GS3-04. http://www.cancerres.aacrjournals.org/content/80/4_Supplement/GS3-04.
- 57.Hennigs A, Riedel F, Marmé F, et al. Changes in chemotherapy usage and outcome of early breast cancer patients in the last decade. Breast Cancer Res Treat. 2016;160:491–499. doi: 10.1007/s10549-016-4016-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cardoso F, van’t Veer LJ, Bogaerts J, et al. 70-gene signature as an aid to treatment decisions in early-stage breast cancer. N Engl J Med. 2016;375:717–729. doi: 10.1056/NEJMoa1602253. [DOI] [PubMed] [Google Scholar]
- 59.Filipits M, Rudas M, Jakesz R, et al. A new molecular predictor of distant recurrence in ER-positive, HER2-negative breast cancer adds independent information to conventional clinical risk factors. Clin Cancer Res. 2011;17:6012–6020. doi: 10.1158/1078-0432.CCR-11-0926. [DOI] [PubMed] [Google Scholar]
- 60.Dubsky P, Brase JC, Jakesz R, et al. The EndoPredict score provides prognostic information on late distant metastases in ER+/HER2− breast cancer patients. Br J Cancer. 2013;109:2959–2964. doi: 10.1038/bjc.2013.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sgroi DC, Carney E, Zarrella E, et al. Prediction of late disease recurrence and extended adjuvant letrozole benefit by the HOXB13/IL17BR biomarker. JNCI J Natl Cancer Inst. 2013;105:1036–1042. doi: 10.1093/jnci/djt146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dowsett M, Sestak I, Lopez-Knowles E, et al. Comparison of PAM50 risk of recurrence score with Oncotype DX and IHC4 for predicting risk of distant recurrence after endocrine therapy. J Clin Oncol. 2013;31:2783–2790. doi: 10.1200/JCO.2012.46.1558. [DOI] [PubMed] [Google Scholar]
- 63.Gnant M, Filipits M, Greil R, et al. Predicting distant recurrence in receptor-positive breast cancer patients with limited clinicopathological risk: using the PAM50 risk of recurrence score in 1478 postmenopausal patients of the ABCSG-8 trial treated with adjuvant endocrine therapy alone. Ann Oncol. 2014;25:339–345. doi: 10.1093/annonc/mdt494. [DOI] [PubMed] [Google Scholar]
- 64.Paik S, Tang G, Shak S, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor–positive breast cancer. J Clin Oncol. 2006;24:3726–3734. doi: 10.1200/JCO.2005.04.7985. [DOI] [PubMed] [Google Scholar]
- 65.Sparano JA, Gray RJ, Makower DF, et al. Adjuvant chemotherapy guided by a 21-gene expression assay in breast cancer. N Engl J Med. 2018;379:111–121. doi: 10.1056/NEJMoa1804710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gluz O, Nitz UA, Christgen M, et al. West German study group phase III planb trial: first prospective outcome data for the 21-gene recurrence score assay and concordance of prognostic markers by central and local pathology assessment. J Clin Oncol. 2016;34:2341–2349. doi: 10.1200/JCO.2015.63.5383. [DOI] [PubMed] [Google Scholar]
- 67.Gonzalez-Angulo AM, Barlow WE, Gralow J, et al. SWOG S1007: A phase III, randomised clinical trial of standard adjuvant endocrine therapy with or without chemotherapy in patients with one to three positive nodes, hormone receptor (HR)-positive, and HER2-negative breast cancer with recurrence score (RS) J Clin Oncol. 2011;29:TPS104–TPS104. doi: 10.1200/jco.2011.29.15_suppl.tps104. [DOI] [Google Scholar]
- 68.Berry DA, Cronin KA, Plevritis SK, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005;353:1784–1792. doi: 10.1056/NEJMoa050518. [DOI] [PubMed] [Google Scholar]
- 69.Saadatmand S, Bretveld R, Siesling S, Tilanus-Linthorst MMA. Influence of tumour stage at breast cancer detection on survival in modern times: population based study in 173 797 patients. BMJ. 2015;351:h4901. doi: 10.1136/bmj.h4901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Alabousi M, Zha N, Salameh J, et al. Digital breast tomosynthesis for breast cancer detection: a diagnostic test accuracy systematic review and meta-analysis. Eur Radiol. 2020;30:2058–2071. doi: 10.1007/s00330-019-06549-2. [DOI] [PubMed] [Google Scholar]
- 71.Hovda T, Holen ÅS, Lång K, et al. Interval and consecutive round breast cancer after digital breast tomosynthesis and synthetic 2D mammography versus standard 2D digital mammography in BreastScreen Norway. Radiology. 2020;294:256–264. doi: 10.1148/radiol.2019191337. [DOI] [PubMed] [Google Scholar]
- 72.Bernardi D, Gentilini MA, De Nisi M, et al. Effect of implementing digital breast tomosynthesis (DBT) instead of mammography on population screening outcomes including interval cancer rates: Results of the Trento DBT pilot evaluation. Breast. 2020;50:135–140. doi: 10.1016/j.breast.2019.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Conant EF, Barlow WE, Herschorn SD, et al. Association of digital breast tomosynthesis vs digital mammography with cancer detection and recall rates by age and breast density. JAMA Oncol. 2019;5:635–642. doi: 10.1001/jamaoncol.2018.7078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bakker MF, de Lange SV, Pijnappel RM, et al. Supplemental MRI screening for women with extremely dense breast tissue. N Engl J Med. 2019;381:2091–2102. doi: 10.1056/NEJMoa1903986. [DOI] [PubMed] [Google Scholar]
- 75.Zanardo M, Cozzi A, Trimboli RM, et al. Technique, protocols and adverse reactions for contrast-enhanced spectral mammography (CESM): a systematic review. Insights Imaging. 2019;10:76. doi: 10.1186/s13244-019-0756-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cozzi A, Schiaffino S, Sardanelli F. The emerging role of contrast-enhanced mammography. Quant Imaging Med Surg. 2019;9:2012–2018. doi: 10.21037/qims.2019.11.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ghaderi KF, Phillips J, Perry H, et al. Contrast-enhanced mammography: current applications and future directions. Radiographics. 2019;39:1907–1920. doi: 10.1148/rg.2019190079. [DOI] [PubMed] [Google Scholar]
- 78.European Society of Radiology (ESR) (2019) Impact of artificial intelligence on radiology: a EuroAIM survey among members of the European Society of Radiology. Insights Imaging 10:105. 10.1186/s13244-019-0798-3 [DOI] [PMC free article] [PubMed]
- 79.McKinney SM, Sieniek M, Godbole V, et al. International evaluation of an AI system for breast cancer screening. Nature. 2020;577:89–94. doi: 10.1038/s41586-019-1799-6. [DOI] [PubMed] [Google Scholar]
- 80.Pisano ED. AI shows promise for breast cancer screening. Nature. 2020;577:35–36. doi: 10.1038/d41586-019-03822-8. [DOI] [PubMed] [Google Scholar]
- 81.Sardanelli F. Trends in radiology and experimental research. Eur Radiol Exp. 2017;1:1. doi: 10.1186/s41747-017-0006-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Neri E, Del Re M, Paiar F, et al. Radiomics and liquid biopsy in oncology: the holons of systems medicine. Insights Imaging. 2018;9:915–924. doi: 10.1007/s13244-018-0657-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Underwood JJ, Quadri RS, Kalva SP, et al. Liquid biopsy for cancer: review and implications for the radiologist. Radiology. 2020;294:5–17. doi: 10.1148/radiol.2019182584. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.