Abstract
Many adolescent smoking prevention programmes target social norms, typically evaluated with self-report, susceptible to social desirability bias. An alternative approach with little application in public health are experimental norms elicitation methods. Using the Mechanisms of Networks and Norms Influence on Smoking in Schools (MECHANISMS) study baseline data, from 12–13 year old school pupils (n = 1656) in Northern Ireland and Bogotá (Colombia), we compare two methods of measuring injunctive and descriptive smoking and vaping norms: (1) incentivized experiments, using monetary payments to elicit norms; (2) self-report scales. Confirmatory factor analysis (CFA) examined whether the methods measured the same construct. Paths from exposures (country, sex, personality) to social norms, and associations of norms with (self-reported and objectively measured) smoking behavior/intentions were inspected in another structural model. Second-order CFA showed that latent variables representing experimental and survey norms measurements were measuring the same underlying construct of anti-smoking/vaping norms (Comparative Fit Index = 0.958, Tucker Lewis Index = 0.951, Root Mean Square Error of Approximation = 0.030, Standardized Root Mean Square Residual = 0.034). Adding covariates into a structural model showed significant paths from country to norms (second-order anti-smoking/vaping norms latent variable: standardized factor loading [β] = 0.30, standard error [SE] = 0.09, p < 0.001), and associations of norms with self-reported anti-smoking behavior (β = 0.40, SE = 0.04, p < 0.001), self-reported anti-smoking intentions (β = 0.42, SE = 0.06, p < 0.001), and objectively measured smoking behavior (β = − 0.20, SE = 0.06, p = 0.001). This paper offers evidence for the construct validity of behavioral economic methods of eliciting adolescent smoking and vaping norms. These methods seem to index the same underlying phenomena as commonly-used self-report scales.
Subject terms: Human behaviour, Psychology, Health care, Medical research
Introduction
Globally, tobacco smoking is still the most important preventable risk factor for chronic disease1. Smokers usually start during adolescence when the influence of social norms on behavior is most apparent2. Early prevention is critical because young smokers can develop serious chronic health problems and are more sensitive to nicotine addiction3. With the introduction of e-cigarettes into the market in the mid-2000s, and as a result of large-scale marketing, e-cigarettes have gained popularity in all age groups, and particularly amongst adolescents4–7. Whilst e-cigarettes are seen as a potential cessation aid amongst adults, for adolescents they are more typically used for experimentation, similar to conventional cigarettes, are associated with willingness to smoke, and may act as a “gateway” to smoking4,8,9. Therefore, the current study examines social norms for smoking and vaping together. Adolescence is a time when young people are susceptible to social influence and many take their cues from the norms of friends, family, and most importantly, peers2. Therefore, many programmes aimed at smoking prevention are anchored in social norms approaches or overtly use peer influencers, with the majority targeting children at the outset of adolescence (around 12–13 years)10–12. The Mechanisms of Networks and Norms Influence on Smoking in Schools (MECHANISMS) study aims to prevent smoking amongst adolescents and to investigate the mechanisms through which social norms for smoking and vaping are established and transmitted through social networks in schools13.
Social norms can be defined in terms of individuals’ beliefs regarding the actions and beliefs of others in a reference group, and an important distinction has been made between injunctive norms (doing what others think one should do) and descriptive norms (doing what others do)14. Survey-based measures of injunctive norms rely on participants’ self-reports regarding what others who are important to them (e.g. parents, friends, peers) think they “should (not)” do. Similarly, survey-based measures of descriptive norms ask respondents how frequently others who are important to them smoke. Such methods have the benefit of simplicity and clarity, but concerns about social desirability bias arise15 because a respondent may perceive that researchers do not approve of smoking, and may not wish to reveal that a parent smokes or would not disapprove of smoking. When considering the issue of social norms measurement for evaluating public health interventions, practical methods which can mitigate the impact of social desirability bias and contribute to understanding mechanisms, are required14.
One potential method for eliciting social norms derives from game theory, a branch of economics that has developed well-defined mathematical models describing cooperation and competition. Using incentivized experimental approaches to elicit social norms has gained some traction in behavioral economics16, but there has been little evidence of transfer into public health. In behavioral economics research, these methods have been applied to explain behaviors such as reciprocity, co-operation, pro-sociality, or honouring agreements in the presence of a verbal promise17,18. The MECHANISMS study applies incentivized experimental approaches to reduce social desirability bias when measuring social norms for adolescent smoking and vaping by asking respondents to guess how peers would answer, and providing them with monetary incentives to ‘match’ their own response to the most common response in their school year group. To measure injunctive norms, respondents are asked to guess how peers would rate the social appropriateness of “a parent smoking in front of young children”, for example. Respondents are told that they will be paid a fixed amount if their response “is the same as the most common response provided in your school year group”. This modal response is elicited as the social norm. Since respondents are asked to think about how others will respond, rather than providing personal opinions, the need for social desirability is mitigated19. The introduction of incentives to guess how most others are guessing, provides further reason to report beliefs truthfully.
Our experiments’ norm elicitation protocol (NEP) provides several additional advantages over a self-report survey. The underlying theoretical model hypothesizes that behavioral heterogeneity within a given setting is related to the degree to which individuals suffer disutility from norm violations or gain from norm adherence (i.e. individuals’ norm-following sensitivities), whilst behavioral heterogeneity between different settings is related to the fact that norms vary between settings17. Our NEP measures both normative beliefs and norm-following sensitivities to account for these effects. We also observe how strong the ‘norms’ are (whether a relatively large or small proportion of respondents provide the modal response), and whether there are multiple actions of comparable social appropriateness. While experimental methods of norms’ elicitation confer all of these advantages, self-report methods have the advantages of simplicity, low cost, and ease of distribution. Furthermore, the two methods focus on slightly different aspects of norms (the experiments inquire about the beliefs of the reference group whilst the self-report methods ask about influences amongst the respondent’s family, friends and peers, who may or may not be representative of a particular reference group). Thus, we propose that the two methods should be viewed as complementary. Identification of latent norms constructs, and an understanding of their relative ability to explain variance in intervention effects, will improve our ability to understand the active mechanisms in such interventions.
Most studies of norms based public health programmes have been conducted in high-income countries while studies in low-middle income countries (LMICs) are limited10. Meanwhile, the tobacco industry has started to strategically target LMICs as its markets are depleted elsewhere20. Our study includes data collected from pupils attending schools throughout Northern Ireland [NI] (a constituent country of the United Kingdom [UK], a high income country21, with approximately 2 million inhabitants22) and Bogotá (the capital city of Colombia, an upper middle income country23, with over 7 million inhabitants24), and aims to compare results between the two settings where the smoking rates, culture, and social norms are different. For example, current cigarette consumption amongst adolescents aged 11–16 years in NI, is 4% compared to 13.1% in Bogotá for adolescents aged 12–18 years25,26. Across the UK, current e-cigarette consumption was 4.9% in 2019 for adolescents aged 11–18 years, similar to rates for conventional cigarettes (5% of adolescents aged 11–15 years)27,28. In Colombia, it is estimated that by 2017 e-cigarette consumption among adolescents will have reached the same prevalence rates as cigarette consumption (9% of adolescents aged 13–15 years)29. In July 2009, Colombia adopted the World Health Organization’s Framework Convention on Tobacco Control30 into legislation, regulating advertising, packaging, sale to the underage population, and smoke-free public places. This was despite tobacco company opposition, reduced state capacity, historical political conditions (e.g. powerful alliances between the tobacco industry and government agricultural agencies, prevalence of tobacco plantations), and efforts to position tobacco as a post-conflict development strategy31,32. Thus, Latin American countries have historically been vulnerable to the effects of the tobacco epidemic, and smoking has been integrated into their culture and customs32. In the UK, the first tobacco harm reduction programme was introduced in 197233, and whilst there has been a long history of anti-tobacco campaigning34, reliance on tobacco industry advice and research previously led to significant delays in introducing more comprehensive tobacco control policies before 199133. Studying the measurement of social norms for adolescent smoking and vaping across such diverse settings will help to better characterize how they spread in schools and impact behavior. Therefore, it is important to understand potential differences in measurement properties of the instruments between the settings.
The current paper aims to compare and contrast the experimental and survey-based social norms measures which were collected as part of the MECHANISMS study.
Specific objectives include to:
Investigate the construct and factorial validity of the norms measures;
Examine whether the experimental and self-reported norms measures are determined by the same underlying latent construct;
Assess cross-country, sex, and personality differences on each latent variable and cross-country differences for individual norms items;
Investigate the relationship between the latent norms variables and self-reported anti-smoking behavior, self-reported anti-smoking intentions, and objectively measured smoking behavior.
Methods
Study design and participants
Fifteen schools (N = 7 in NI, N = 8 in Bogotá; participation = 90.8%, n = 1656/1824 pupils) took part in the MECHANISMS study between September 2018 and November 2019. We aimed to recruit all pupils in a single year group (aged 11–13 years/Year 9 in NI and 11–15 years/Year 7 in Bogotá, target age 12–13 years). During a single school semester, participants received one of two school-based smoking prevention programmes with proven effectiveness11,35. In a pre-post design, pupils participated in incentivized (monetary) norms elicitation experiments, whose design is rooted in the fields of behavioral economics and game theory16,17,36, and completed a self-report survey.
Ethics approval was granted from Queen's University Belfast on September 21, 2018 and from Universidad de los Andes, Bogotá Colombia on July 30, 2018. All participants and parents provided informed consent. The experimental protocol, and all data collection procedures, were carried out in accordance with institutional guidelines for research involving human participants. The baseline assessment consisted of two separate sessions with each class in the school year group in each school, during which participants completed an experiment and self-report survey. Experiments and surveys were delivered via the platform Qualtrics (Qualtrics, Provo, Utah, USA) and completed on iPads. Information on study procedures, the study flow diagram, baseline characteristics of participants, and a glossary of terms are available in supplement 1. Prior to implementation in Bogotá, all study instruments underwent a cultural adaptation process including translation into Spanish language and back translation, using the heuristic framework for cultural adaptation proposed by Barrera & Castro37,38.
Incentivized experiments
The incentivized (game theory) experiments consisted of a series of incentivized tasks based on published designs in behavioral economics16,17,36. There were four parts to the experiment and the current paper uses data from Parts 1–3. Part 1 consisted of a Rule-Following (RF) task measuring each participant's sensitivity to the effects of social norms17,36. The task instructs participants that they have five minutes to allocate 50 balls across two buckets (one blue and one yellow) following an explicitly stated arbitrary rule ("The rule is to put the balls in the blue bucket"). Following the rule imposes explicit monetary costs directly proportional to the degree of rule-following. The central premise is that the more a participant cares intrinsically about rule-following the more willing he/she will be to incur the costs of doing so36. Individuals’ norms sensitivities were elicited as the number of balls allocated to the blue (rule-following) bucket.
Parts 2 and 3 of the experiment consisted of a series of incentivized coordination games which used methods employed by Krupka and Weber16 to elicit injunctive and descriptive social norms around smoking and vaping in the whole school year group. Participants were provided with financial incentives to match their ratings/estimates to other participants' in their school year group as opposed to providing personal opinions. Specifically, participants were informed that they would receive a payment if their response to a randomly selected question matched the most common answer provided in their school year group. Injunctive norms reflect shared beliefs among members of a population about what actions people ought to take16. Injunctive norms were assessed by asking participants to ‘coordinate’ with others in their school year group to rate the social appropriateness of a series of smoking- and vaping-related situations. Descriptive norms reflect shared beliefs among members of a population about what actions people actually do take16. Descriptive norms were assessed by asking participants to ‘coordinate’ with others in their school year group to estimate the proportion of their school year group who would be accepting of a close friend smoking or vaping. For each item, the ‘norm’ is elicited as the modal response in the year group. Table 1 shows the assessed smoking- and vaping-related scenarios and numerical coding of responses. More information on the theoretical underpinning of these methods, and full experimental protocols are provided in supplements 1 and 2.
Table 1.
Smoking/vaping-related injunctive and descriptive social norms elicited in the experiment and self-report survey.
| Variable name | Scenario/Question | Responses/Coding |
|---|---|---|
| Experiment Part 1: Rule-following | ||
| Rule-following (BlueBucket) | Rule-following (individuals’ norms sensitivities): Number of balls allocated to the blue (rule-following) bucket | 1 (least rule-following) to 50 (most rule-following) |
| Experiment Part 2: Injunctive norms (α = 0.77)a | ||
| Part 2 Situation 2 (P2S2) | Parent smoking in their own home in front of children under age of 5 | − 1 = Extremely socially inappropriate; − 0.6 = Very socially inappropriate; − 0.2 = Somewhat socially inappropriate; + 0.2 = Somewhat socially appropriate; + 0.6 = Very socially appropriate; + 1 = Extremely socially appropriate |
| Part 2 Situation 3 (P2S3) | An adult smoking in a car with children under the age of 16 in the car | As per P2S2 |
| Part 2 Situation 4 (P2S4) | Someone selling cigarettes to a teenager who looks younger than 16 without requesting proof of age | As per P2S2 |
| Part 2 Situation 5 (P2S5) | In a recent superhero movie the lead actor is seen smoking in the opening scene | As per P2S2 |
| Part 2 Situation 6 (P2S6) | An older student from school is smoking outside school, for example, at a bus stop | As per P2S2 |
| Part 2 Situation 7 (P2S7) | A pupil from school is using an e-cigarette while walking to school | As per P2S2 |
| Part 2 Situation 8 (P2S8) | A pupil from school shares a photograph of him/herself using an e-cigarette on social media | As per P2S2 |
| Part 2 Situation 9 (P2S9) | A pupil from school is chewing tobacco | As per P2S2 |
| Experiment Part 3: Descriptive norms (α = 0.85)a | ||
| Part 3 Question 1 (P3Q1) | The proportion of my peers who would be accepting of a close friend smoking | − 1 = None of my peers; − 0.6 = Only a few of my peers; − 0.2 = Some of my peers; + 0.2 = A lot of my peers; + 0.6 = Most of my peers; + 1 = All of my peers |
| Part 3 Question 2 (P3Q2) | The proportion of my peers who would be accepting of a close friend vaping | As per P3Q1 |
| Survey: Self-reported injunctive norms (α = 0.74)b,c | ||
| Injunctive Norms 1 (IN1) | Most of the people who are important to me think that I… | − 2 = Definitely should smoke; − 1 = Maybe should smoke; 0 = Don't know/neutral; + 1 = Maybe should not smoke; + 2 = Definitely should not smoke |
| Injunctive Norms 2 (IN2) | My mother thinks that I… | As per IN1. Responses of “I don’t have a mother” were also set to 0 |
| Injunctive Norms 3 (IN3) | My father thinks that I… | As per IN1. Responses of “I don’t have a father” were also set to 0 |
| Injunctive Norms 4 (IN4) | My brother(s) think(s) that I… | As per IN1. Responses of “I don’t have a brother” were also set to 0 |
| Injunctive Norms 5 (IN5) | My sister(s) think(s) that I… | As per IN1. Responses of “I don’t have a sister” were also set to 0 |
| Injunctive Norms 6 (IN6) | My friends think that I… | As per IN1. Responses of “I don’t have a friend” were also set to 0 |
| Injunctive Norms 7 (IN7) | My best friend thinks that I… | As per IN1. Responses of “I don’t have a best friend” were also set to 0 |
| Survey: Self-reported descriptive norms (α = 0.54)b,d | ||
| Descriptive Norms 1 (DN1) | Does your best friend smoke? | 1 = Very often; 2 = Often; 3 = Occasionally; 4 = Rarely; 5 = Never/Don't know. Responses of “I don’t have a best friend” were also set to 5 |
| Descriptive Norms 2 (DN2) | Does your mother smoke? | As per DN1. Responses of “I don’t have a mother” were also set to 5 |
| Descriptive Norms 3 (DN3) | Does your father smoke? | As per DN1. Responses of “I don’t have a father” were also set to 5 |
| Descriptive Norms 4 (DN4) | Do any of your brothers smoke? | As per DN1. Responses of “I don’t have a brother” were also set to 5 |
| Descriptive Norms 5 (DN5) | Do any of your sisters smoke? | As per DN1. Responses of “I don’t have a sister” were also set to 5 |
| Survey: Self-reported smoking behavior and intentionsb | ||
| Past Smoking Behavior (SmokePast) | Now read the following statements carefully and tick the box next to the one which best describes you. (I have never smoked; I have only ever tried smoking once; I used to smoke sometimes but I never smoke a cigarette now; I sometimes smoke cigarettes now but I don’t smoke as many as one a week) | 1 = Sometimes smoke; 2 = Previous smoker; 3 = Smoked once; 4 = Never smoked |
| Intentions (Intent) | If you DON’T currently smoke, do you intend to take up smoking in the next 6 months? | 1 = I am a smoker; 2 = Definitely start smoking; 3 = Probably start smoking; 4 = Don't know; 5 = Probably remain; 6 = Definitely remain a non-smoker |
| Smokerlyzer readings: Objectively measured smoking behavior | ||
| Carbon monoxide reading (COreading) | Objectively measured smoking behavior over the past 24 h captured using hand-held carbon monoxide monitors (PICOAdvantage Smokerlyzer, Bedfont) to measure expelled air carbon monoxide in parts per million (ppm) in a range of 0–150 ppm with an accuracy of 2 ppm/5% (whichever is greater) | Continuous variable (ppm) |
| Survey: Self-reported sex and personality characteristicsb | ||
| Sex | Participant sex | 0 = Boy; 1 = Girl/Prefer not to say |
| Need to Belong (Belong) | Need to Belong Scale | Average of 10 items, each coded 1–5: 1 (lowest need to belong)-5 (greatest need to belong). Not available for two Colombian schools |
| Fear of Negative Evaluation (Negative) | Fear of Negative Evaluation Scale | Average of 12 items, each coded 1–5: 1 (lowest fear of negative evaluation)-5 (greatest fear of negative evaluation). Not available for two Colombian schools |
| Prosocial Behavior (Prosocial) | Prosocial Behavior Scale | Sum of five items, each coded 0–2: 0 (least prosocial)-10 (most prosocial) |
| Big 5 Openness (Big5Open) | Big 5 Personality Questionnaire (Openness subscale) | Average of 10 items, each coded 0–4: 0 (lowest openness)-4 (greatest openness) |
| Big 5 Extraversion (Big5Extra) | Big 5 Personality Questionnaire (Extraversion subscale) | Average of 10 items, each coded 0–4: 0 (least extraverted)-4 (most extraverted) |
| Big 5 Agreeableness (Big5Agree) | Big 5 Personality Questionnaire (Agreeableness subscale) | Average of 10 items, each coded 0–4: 0 (least agreeable)-4 (most agreeable) |
| Big 5 Conscientiousness (Big5Cons) | Big 5 Personality Questionnaire (Conscientiousness subscale) | Average of 10 items, each coded 0–4: 0 (least conscientious)-4 (most conscientious) |
| Big 5 Stability (Big5Stab) | Big 5 Personality Questionnaire (Stability subscale) | Average of 10 items, each coded 0–4: 0 (least stability)-4 (most stability) |
aResponses to experimental items were numerically coded to run between − 1 and + 1 following procedures adopted in Krupka and Weber16.
bAll items on the survey were coded such that higher numerical values represented greater anti-smoking norms, greater anti-smoking behavior or intentions, or higher values of the personality traits (Need to Belong, Fear of Negative Evaluation, Pro-social Behavior, Big 5 Personality Questionnaire).
cResponses to survey injunctive norms items were numerically coded to run between − 2 and + 2 following Cremers et al.92.
dResponses to survey descriptive norms items were numerically coded to run between + 1 and + 5 following Cremers et al.92.
Self-report survey
A survey was used to collect socio-demographic and personal characteristics, social networks data, past and present smoking behavior and intentions, psychosocial constructs and wellbeing. All survey items were previously validated and adopted from studies conducted with children of a similar age13. The current paper uses data collected from seven items measuring injunctive social norms for smoking39, five items measuring descriptive social norms for smoking39, one item measuring past smoking behavior40,41, one item measuring smoking intentions over the next six months42, a ten-item Need to Belong scale43,44, a 12-item Fear of Negative Evaluation Scale44–46, a five-item Pro-social Behavior Scale44,47, and the five subscales of the “Big 5” Personality Questionnaire48,49 (Table 1). Pupils also had their smoking behavior in the last 24 h measured using a hand-held carbon monoxide monitor (PICOAdvantage Smokerlyzer, Bedfont)50. This is an electrochemical sensor which measures expelled air carbon monoxide in parts per million (ppm) in a range of 0–150 ppm with an accuracy of 2 ppm/5% (whichever is greater)50. A pupil was considered to have engaged in smoking behavior if they provided a reading of > 9 ppm in line with previous research35,51. We analysed objective smoking behavior as a continuous variable (expelled air carbon monoxide in ppm)35.
Statistical analysis
The statistical analysis was guided by the following specific objectives:
To conduct confirmatory factor analysis (CFA) to explore the construct and factorial validity of the norms measures;
To investigate whether the experimental and self-reported norms measures are determined by the same underlying latent construct using second-order CFA;
To assess cross-country, sex, and personality differences on each latent variable using multiple indicators multiple causes (MIMIC) modelling52,53, and cross-country differences for individual items using differential item functioning (DIF) analysis;
To investigate the relationship between the DIF-adjusted latent “anti-smoking/vaping norms” variables and self-reported anti-smoking behavior, self-reported anti-smoking intentions, and objectively measured smoking behavior, using structural equation modelling (SEM).
Analyses were conducted using Stata 13 (StataCorp)54 and R version 3.6.155. Means and standard deviations were computed and histograms were graphed to visualize distributions of all variables. Cronbach's alpha coefficients were computed for: (1) experimentally derived injunctive norms; (2) experimentally derived descriptive norms; (3) survey injunctive norms; (4) survey descriptive norms. As a preliminary step, we examined whether individual norms items from the experiments (Part 2 Situations 2–9, Part 3 Questions 1–2) and survey (Injunctive Norms 1–7, Descriptive Norms 1–5) were showing theoretically expected inter-relationships and associations with self-reported anti-smoking behavior, intentions, and objectively measured smoking behavior. Spearman's rank-order correlations were computed, examining the association between individual norms items from the experiments and survey, and associations between self-reported anti-smoking behavior, intentions, and objectively measured smoking behavior. Individual norms items were examined for an association with self-reported anti-smoking behavior, self-reported anti-smoking intentions, and objectively measured smoking behavior, using mixed-effects regressions. Rule-following was compared between NI and Colombia using a cluster-adjusted t-test with number of balls allocated to the blue bucket in the RF task as the outcome and participant school as the cluster variable. This was carried out using Stata’s ‘clttest’ command.
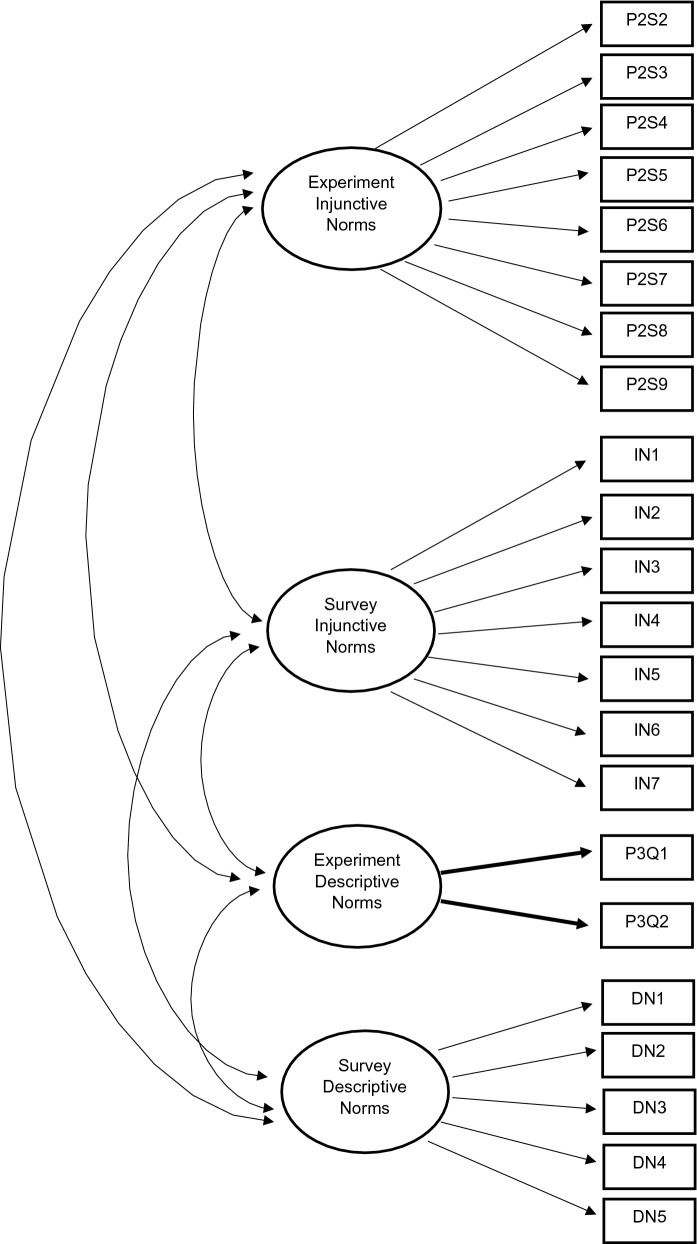
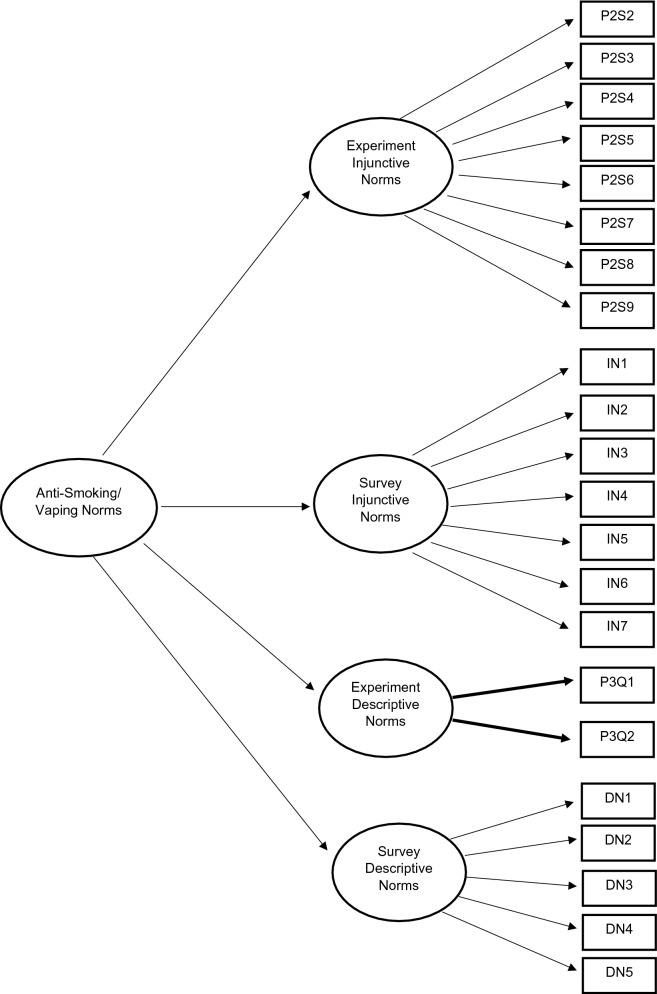
CFA is a statistical technique to determine whether measures of a construct are consistent with a researcher’s understanding of the nature of the construct, or factor, by testing whether the data fits a hypothesized measurement model56. To assess factorial and construct validity, separate CFAs were conducted for: experimental injunctive norms (model 1); survey injunctive norms (model 2); experimental descriptive norms (model 3); survey descriptive norms (model 4; objective 1). To compare the experimental and survey measurements, a CFA model was conducted containing four correlated first-order latent variables (model 5; Fig. 1). A final CFA model was derived, similar to model 5, in which the covariance between the first-order latent variables was described by an overall second-order latent construct labelled “Anti-Smoking/Vaping Norms” (model 6; Fig. 2; objective 2)57. Since our experimentally derived measure of descriptive norms consisted only of two items, convergence was achieved by constraining the loadings of both indicators to be equal58.
Figure 1.
Theoretic first-order measurement model with four correlated latent variables.
Figure 2.
Theoretic second-order measurement model with four first-order latent variables.
CFAs were conducted using the lavaan package in R59. To reduce bias in standard errors which threatens maximum likelihood estimation60–62, robust standard errors were computed (Huber White)63,64. This estimator was favoured over the categorical estimators since all indicators had more than five response categories62,65,66. It also permitted imputation of missing data using full information maximum likelihood. The Little (1988) test was used to determine whether data for individual items were missing completely at random (MCAR) using Stata’s ‘mcartest’ command with 200 iterations in the expectation maximization algorithm67. A p value of < 0.0001 was obtained, indicating that the data were not MCAR, which justified imputing missing data68. All analyses were repeated without imputation of missing data (i.e. complete cases). Percentages of missing data requiring imputation for individual items ranged from 3.7–3.9% (experimentally derived injunctive norms), 4.2–4.5% (survey injunctive norms), 3.7–3.9% (experimentally derived descriptive norms), and 4.16–4.22% (survey descriptive norms). For the most part, missing data occurred if a participant was present in school on one of the days (for the experiment or the survey), but absent on the other day (n = 123/1636 = 7.5% of participants).
Model fit was assessed in relation to several goodness-of-fit indices. The chi-square statistic can be used to assess the absolute fit of the model to the data, assuming correct model specification57,69. A non-significant result (p > 0.05) indicates good model fit. However, it can be overly influenced by sample size, correlations, variance unrelated to the model, and multivariate non-normality69,70. Comparative Fit Index (CFI) values of ≥ 0.96, Tucker-Lewis Index (TLI) values of ≥ 0.95, Root Mean Square Error of Approximation (RMSEA) values of ≤ 0.06, and Standardized Root Mean Square Residual (SRMR) values of ≤ 0.09 indicate good model fit69,71. A number of parsimony based fit indices were also extracted including the Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC) and adjusted BIC. Lower values on these indices indicate a more parsimonious model69. Measurement models were modified to improve factorial validity by reference to modification indices (MIs)72. Modifications were made only where substantively appropriate, and with strong theoretical justification69,73,74. Subsequent analyses were based on the second-order measurement model. Supplement 3 shows syntax for all analyses.
MIMIC models can be used to examine differences on latent variables by regressing them onto an observed grouping variable. Individual items can then be tested for DIF by regressing them onto the grouping variable whilst controlling for differences at the latent variable level52,53,75. These techniques were used to compare the norms measurements, and to assess measurement invariance, between NI and Colombia (objective 3). Baseline MIMIC models included a measurement model and a structural model: (1) the second-order latent variable regressed onto an observed country variable (0 = NI, 1 = Colombia); (2) the four first-order latent variables regressed simultaneously onto the observed country variable. This showed whether mean values on the overall latent constructs differed between the two countries. DIF occurs when an item has different measurement properties for one group versus another, irrespective of mean differences on the overall latent construct76. To determine which indicators showed DIF, direct paths between country and each observed indicator were constrained to 0, whilst controlling for country differences on the four first-order latent constructs. MIs were inspected along with expected parameter changes (EPCs) and DIF was determined to be present for an item if MI > 3.84 and EPC ≥ 0.1077. This novel approach to assessing DIF has been adopted from a recent study78. In the case of low power (< 0.80), if these conditions were not met, the result was determined as inconclusive.
MIMIC models were also used to determine whether mean values on the overall first- and second-order latent constructs (adjusted for country differences on first-order latent variables and DIF) differed according to sex, personality characteristics (Need to Belong, Fear of Negative Evaluation, Pro-social Behavior, Big 5 personality subscales), and rule-following (number of balls allocated to the blue bucket in the RF task). We also examined, and found no evidence for, DIF according to participant sex (results not reported).
The DIF-adjusted second-order measurement model was investigated for associations with observed self-reported anti-smoking behavior, intentions, and objectively measured smoking behavior, using SEM (objective 4). The structural part of these models included either self-reported anti-smoking behavior, self-reported anti-smoking intentions, or objectively measured smoking behavior as the observed outcome variable regressed onto: (1) the second-order latent variable; (2) the four first-order latent variables simultaneously. Path coefficients were inspected (p < 0.05 provided evidence for a significant association).
Ethical statements
This study complies with all relevant ethical regulations.
Results
Descriptive statistics are shown in Table 2 and supplement 4. Mean responses for all experimental items are < 0, indicating there were already anti-smoking norms established at baseline. Details on the methods and results of the correlational analyses and mixed-effects regressions are discussed in supplement 5. Individual items from the experiments and survey showed theoretically expected inter-relationships and associations with self-reported anti-smoking behavior and intentions (e.g. higher anti-smoking/vaping norm responses were associated with greater anti-smoking behavior and intentions). Theoretically expected inter-relationships were observed between self-reported anti-smoking behavior and intentions, and objectively measured smoking behavior. These models also indicate that (1) pupils who were more rule-following in the RF task were more likely to report higher anti-smoking behavior and intentions; (2) Colombian pupils were more likely to report lower anti-smoking behavior or intentions and to show higher levels of expelled air carbon monoxide in their Smokerlyzer readings (which accords with intercountry differences in smoking prevalence among adolescents). A cluster-adjusted t-test showed there were no between-country differences in rule-following (number of balls allocated to the blue bucket in the RF task, p = 0.19).
Table 2.
Baseline summary statistics, means and standard deviations.
| Northern Ireland (N = 7) | Colombia (N = 8) | All schools (N = 15) | |
|---|---|---|---|
| Experiment, n | 696 | 880 | 1576 |
| Survey, n | 701 | 872 | 1573 |
| Experiment Part 1: Balls allocated to blue (rule-following) bucket | 28.8 (19.2) | 31.6 (16.9) | 30.4 (18.0) |
| Experiment Part 2 (injunctive social norms)a | |||
| P2S2 | − 0.8 (0.3) | − 0.9 (0.2) | − 0.9 (0.3) |
| P2S3 | − 0.7 (0.4) | − 0.7 (0.3) | − 0.7 (0.4) |
| P2S4 | − 0.9 (0.3) | − 0.9 (0.3) | − 0.9 (0.3) |
| P2S5 | − 0.3 (0.4) | − 0.5 (0.4) | − 0.4 (0.4) |
| P2S6 | − 0.6 (0.4) | − 0.5 (0.4) | − 0.6 (0.4) |
| P2S7 | − 0.5 (0.4) | − 0.6 (0.4) | − 0.5 (0.4) |
| P2S8 | − 0.5 (0.4) | − 0.5 (0.4) | − 0.5 (0.4) |
| P2S9 | − 0.8 (0.4) | − 0.8 (0.3) | − 0.8 (0.3) |
| Experiment Part 3 (descriptive social norms)b | |||
| P3Q1 | − 0.5 (0.5) | − 0.5 (0.5) | − 0.5 (0.5) |
| P3Q2 | − 0.3 (0.6) | − 0.5 (0.5) | − 0.4 (0.5) |
| Survey: Smoking behaviorc | 3.8 (0.6) | 3.7 (0.7) | 3.8 (0.6) |
| Survey: Smoking intentionsd | 5.7 (0.8) | 5.5 (1.2) | 5.6 (1.1) |
| Survey: Injunctive social normse | |||
| IN1 | 1.7 (0.7) | 1.8 (0.6) | 1.8 (0.7) |
| IN2 | 1.9 (0.3) | 1.9 (0.4) | 1.9 (0.4) |
| IN3 | 1.8 (0.6) | 1.7 (0.7) | 1.7 (0.7) |
| IN4 | 1.4 (0.9) | 1.4 (0.9) | 1.4 (0.9) |
| IN5 | 1.4 (0.9) | 1.4 (0.9) | 1.4 (0.9) |
| IN6 | 1.5 (0.9) | 1.3 (1.0) | 1.4 (0.9) |
| IN7 | 1.7 (0.7) | 1.5 (0.9) | 1.6 (0.8) |
| Survey: Descriptive social normsf | |||
| DN1 | 4.8 (0.8) | 4.8 (0.7) | 4.8 (0.7) |
| DN2 | 4.2 (1.4) | 4.6 (1.0) | 4.4 (1.2) |
| DN3 | 4.2 (1.4) | 4.4 (1.2) | 4.3 (1.3) |
| DN4 | 4.7 (0.9) | 4.7 (0.8) | 4.7 (0.9) |
| DN5 | 4.8 (0.7) | 4.8 (0.7) | 4.8 (0.7) |
| Survey: Sex and psycho-social variables | |||
| Sex, n(%)g | |||
| Boys | 335 (47.8%) | 436 (50.0%) | 771 (49.0%) |
| Girls | 355 (50.6%) | 431 (49.4%) | 786 (50.0%) |
| Prefer not to say | 11 (1.6%) | 5 (0.6%) | 16 (1.0%) |
| Need to Belong Scale (1–5)h | 3.1 (0.6) | 2.8 (0.6) | 3.0 (0.6) |
| Fear of Negative Evaluation (1–5)i | 2.9 (0.7) | 2.6 (0.6) | 2.7 (0.7) |
| Pro-social Behavior (0–10)j | 8.1 (2.1) | 7.3 (2.1) | 7.6 (2.1) |
| Big 5 (Openness; 0–4)k | 2.4 (0.6) | 2.7 (0.7) | 2.6 (0.7) |
| Big 5 (Extraversion; 0–4)k | 2.6 (0.8) | 2.7 (0.7) | 2.6 (0.7) |
| Big 5 (Agreeableness; 0–4)k | 1.9 (0.8) | 2.6 (0.7) | 2.6 (0.7) |
| Big 5 (Conscientiousness; 0–4)k | 2.7 (0.7) | 2.4 (0.6) | 2.4 (0.7) |
| Big 5 (Stability; 0–4)k | 1.9 (0.8) | 2.1 (0.7) | 2.0 (0.7) |
| Smokerlyzer readings: Objective smoking behavior (carbon monoxide, ppm)l | 1.5 (1.4) | 3.4 (1.5) | 2.5 (1.7) |
a− 1 = Extremely socially inappropriate; − 0.6 = Very socially inappropriate; − 0.2 = Somewhat socially inappropriate; 0.2 = Somewhat socially appropriate; 0.6 = Very socially appropriate; 1 = Extremely socially appropriate.
b− 1 = None of my peers; − 0.6 = Only a few of my peers; − 0.2 = Some of my peers; + 0.2 = A lot of my peers; + 0.6 = Most of my peers; + 1 = All of my peers.
c1 = Sometimes smoke; 2 = Previous smoker; 3 = Smoked once; 4 = Never smoked.
d1 = I am a smoker; 2 = Definitely start smoking; 3 = Probably start smoking; 4 = Don't know; 5 = Probably remain; 6 = Definitely remain a non-smoker.
e− 2 = Definitely should smoke; − 1 = Maybe should smoke; 0 = Don't know/neutral; + 1 = Maybe should not smoke; + 2 = Definitely should not smoke. "I don't have…" responses set to 0.
f1 = Very often; 2 = Often; 3 = Occasionally; 4 = Rarely; 5 = Never/Don't know. “I don’t have…” responses set to 5.
gIn all analyses, sex is coded (0 = Boy; 1 = Girl/Prefer not to say).
hAverage of 10 items, coded 1–5. Not available for two Colombian schools (excluded from analysis).
iAverage of 12 items, coded 1–5. Not available for two Colombian schools (excluded from analysis).
jSum of five items, coded 0–2.
kAverage of 10 items, coded 0–4.
lNot available for one Northern Irish school and two Colombian schools (excluded from analysis).
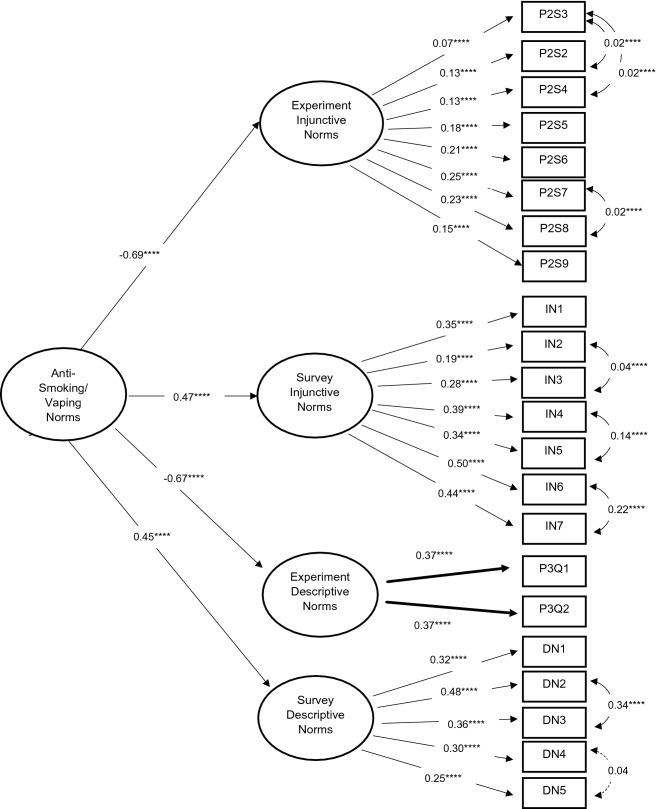
Goodness-of-Fit statistics for our CFA models are shown in supplement 6. Although chi-square tests were significant for almost all of the models (p < 0.05), we did not reject models on this basis as it can be overly influenced by sample size, correlations, variance unrelated to the model, and multivariate non-normality69,70. CFI values ranged from 0.958–1.000 and TLI values ranged from 0.947–1.017. RMSEA values ranged from 0.000–0.059 and SRMR values ranged from 0.000–0.034. Therefore, all models demonstrated a good or satisfactory fit (objective 1). Inspection of model fit indices indicated there was almost an identical fit between the first-order measurement model with four correlated latent variables (model 5; Fig. 1) and the second-order measurement model (model 6; Fig. 2). Subsequent analyses were based on the second-order measurement model. Diagrams showing final model structures and standardized factor loadings are provided in supplement 6 (Fig. 3 shows results for the final second-order measurement model).
Figure 3.
Second-order measurement model with four first-order latent variables, standardized factor loadings, *p < 0.10; **p < 0.05; ***p < 0.01; ****p ≤ 0.001.
The second-order measurement model showed negative standardized factor loadings for the paths connecting the first-order latent constructs representing experimentally derived norms to the underlying second-order latent construct (injunctive norms: standardized factor loading [β] = − 0.69, standard error [SE] = 0.11, p < 0.001; descriptive norms: β = − 0.67, SE = 0.10, p < 0.001), and positive standardized factor loadings for the paths connecting the first-order latent constructs representing survey norms to the underlying second-order latent construct (injunctive norms: β = 0.47, SE = 0.08, p < 0.001; descriptive norms: β = 0.45, SE = 0.10, p < 0.001). This is as expected since the experiment and survey items were coded in the opposite directions intuitively. Thus, higher values on the second-order latent variable represent greater anti-smoking/vaping norms. Therefore, we concluded that our hypothesized measurement models showed good fit to the data, and our four first-order latent variables were measuring the same overall second-order latent variable of “Anti-Smoking/Vaping Norms” (objective 2).
Baseline MIMIC models indicated that there was an association between country and the second-order latent variable measuring anti-smoking/vaping norms (β = 0.30, SE = 0.09, p < 0.001). Therefore, Colombian pupils reported greater anti-smoking norms overall. There were significant intercountry differences for the first-order latent variables measuring experimentally derived injunctive norms (β = − 0.21, SE = 0.08, p = 0.007), survey injunctive norms (β = − 0.21, SE = 0.07, p = 0.004), experimentally derived descriptive norms (β = − 0.31, SE = 0.07, p < 0.001), and survey descriptive norms (β = 0.30, SE = 0.12, p = 0.008) (Table 3). Therefore, Colombian pupils were more likely to give lower social appropriateness ratings in their experiment injunctive norms responses, and to rate that a lower proportion of their school year group would be accepting of a close friend smoking/vaping in their experiment descriptive norms responses. Colombian pupils were also more likely to think that people who are important to them (e.g. parents, siblings) would be more accepting of their own smoking behavior in their survey injunctive norms responses, and more likely to think that people who are important to them smoke less frequently in their survey descriptive norms responses.
Table 3.
Effects of country on first-order norms latent variables, second-order norms latent variables and observed indicators, standardized regression coefficients.
| Latent variable/Observed indicator | Baseline MIMIC model | DIF corrected model | ||
|---|---|---|---|---|
| Β (SE) | p value | Β (SE) | p value | |
| Second-order latent variables | ||||
| Anti-Smoking/Vaping Norms | 0.30 (0.09) | < 0.001 | – | – |
| First-order latent variables | ||||
| Expt. Inj. Norms | − 0.21 (0.08) | 0.007 | − 0.11 (0.07) | 0.15 |
| Sur. Inj. Norms | − 0.21 (0.07) | 0.004 | − 0.35 (0.08) | < 0.001 |
| Expt. Desc. Norms | − 0.31 (0.07) | < 0.001 | − 0.31 (0.07) | < 0.001 |
| Sur. Desc. Norms | 0.30 (0.12) | 0.008 | 0.03 (0.09) | 0.75 |
| Indicatorsa | ||||
| P2S2 | – | – | − 0.10 (0.01) | < 0.001 |
| P2S5 | – | – | − 0.14 (0.02) | < 0.001 |
| IN1 | – | – | 0.15 (0.03) | < 0.001 |
| IN4 | – | – | 0.15 (0.04) | 0.001 |
| DN2 | – | – | 0.38 (0.06) | < 0.001 |
| DN3 | – | – | 0.22 (0.07) | 0.001 |
MIMIC multiple indicators multiple causes, DIF differential item functioning.
aControlling for country differences on the underlying first-order latent variable (0 = Northern Ireland, 1 = Colombia).
Controlling for differences on the latent variables, there was evidence that the following items may be exhibiting DIF: Part 2 Situation 2, Part 2 Situation 5, Part 2 Situation 8, Injunctive Norms 1, Injunctive Norms 3, Injunctive Norms 4, Injunctive Norms 7, Descriptive Norms 2, Descriptive Norms 4, and Descriptive Norms 5. Results were inconclusive for Injunctive Norms 5, Injunctive Norms 6, Descriptive Norms 1, and Descriptive Norms 3 due to low power (supplement 7). There was no further evidence of DIF with the paths from country to the following indicators freely estimated: Part 2 Situation 2, Part 2 Situation 5, Injunctive Norms 1, Injunctive Norms 4, Descriptive Norms 2, and Descriptive Norms 3 (Table 3). After adjusting for DIF, the path from country to the first-order latent variable measuring experimental injunctive norms was no longer statistically significant (p = 0.15) suggesting that between-country differences on this latent variable were due to the items Part 2 Situation 2 and Part 2 Situation 5. After adjusting for DIF, the path from country to the first-order latent variable measuring survey descriptive norms was no longer statistically significant (p = 0.75) suggesting that between-country differences on this latent variable were due to the items Descriptive Norms 2 and Descriptive Norms 3.
Results of MIMIC models examining associations between sex, personality characteristics, and rule-following with latent norms variables are reported in supplement 8. For the second-order latent construct there were significant positive associations with the following variables: Need to Belong (p = 0.003), Pro-Social Behavior (p < 0.001), Openness (p < 0.001), Extraversion (p = 0.03), Agreeableness (p < 0.001), Conscientiousness (p < 0.001), and Stability (p < 0.001). Thus, higher levels on these personality variables were associated with higher anti-smoking/vaping norms. Results are also presented for associations with first-order latent norms constructs (objective 3).
The results of SEM models are shown in Table 4. Higher anti-smoking/vaping norms (on the second-order latent variable) were associated with higher self-reported anti-smoking behavior (β = 0.40, SE = 0.04, p < 0.001), higher self-reported anti-smoking intentions (β = 0.42, SE = 0.06, p < 0.001), and lower objectively measured smoking behavior (β = − 0.20, SE = 0.06, p = 0.001). These models also show a negative association between country and self-reported anti-smoking behavior and intentions suggesting that Colombian pupils were more likely to report higher levels of past/current smoking behavior or greater intentions to take up smoking in the next six months compared to NI pupils. There was also a positive association between country and objective smoking behavior suggesting that Colombian pupils showed higher levels of expelled air carbon monoxide in their Smokerlyzer readings (objective 4).
Table 4.
DIF-adjusted models predicting self-reported anti-smoking behavior, self-reported anti-smoking intentions, and objectively measured smoking behavior.
| Parameter | Outcome variable | |||||
|---|---|---|---|---|---|---|
| Anti-smoking behavior | Anti-smoking intentions | Objective smoking behaviora | ||||
| Β (SE) | p value | Β (SE) | p value | Β (SE) | p value | |
| Second-order latent norm variables as predictor | ||||||
| Outcome variable | ||||||
| Anti-Smoking/Vaping Norms (second-order latent) | 0.40 (0.04) | < 0.001 | 0.42 (0.06) | < 0.001 | − 0.20 (0.06) | 0.001 |
| Country (observed) | − 0.11 (0.03) | 0.001 | − 0.26 (0.05) | < 0.001 | 1.83 (0.08) | < 0.001 |
| First-order latent norms variables as predictors | ||||||
| Outcome variable | ||||||
| Expt. Inj. Norms (first-order latent) | 0.004 (0.02) | 0.83 | − 0.007 (0.03) | 0.81 | 0.02 (0.05) | 0.67 |
| Sur. Inj. Norms (first-order latent) | 0.07 (0.03) | 0.01 | 0.17 (0.04) | < 0.001 | − 0.02 (0.05) | 0.63 |
| Expt. Desc. Norms (first-order latent) | − 0.01 (0.02) | 0.47 | − 0.002 (0.03) | 0.94 | 0.10 (0.04) | 0.02 |
| Sur. Desc. Norms (first-order latent) | 0.31 (0.04) | < 0.001 | 0.28 (0.05) | < 0.001 | − 0.05 (0.06) | 0.44 |
| Country (observed) | − 0.11 (0.03) | 0.001 | − 0.21 (0.05) | < 0.001 | 1.85 (0.08) | < 0.001 |
| Expt. Inj. Norms (first-order latent) | ||||||
| Country (observed) | − 0.11 (0.07) | 0.14 | − 0.11 (0.07) | 0.15 | 0.03 (0.08) | 0.75 |
| Sur. Inj. Norms (first-order latent) | ||||||
| Country (observed) | − 0.35 (0.08) | < 0.001 | − 0.35 (0.08) | < 0.001 | − 0.37 (0.08) | < 0.001 |
| Expt. Desc. Norms (first-order latent) | ||||||
| Country (observed) | − 0.31 (0.07) | < 0.001 | − 0.31 (0.07) | < 0.001 | − 0.21 (0.08) | 0.005 |
| Sur. Desc. Norms (first-order latent) | ||||||
| Country (observed) | 0.06 (0.09) | 0.47 | 0.04 (0.09) | 0.65 | 0.18 (0.10) | 0.09 |
aObjective smoking behavior readings not available for one Northern Irish school and two Colombian schools (excluded from analysis).
Discussion
Using CFA, our results provide evidence supporting the construct and factorial validity of the two different measurement instruments that were used to elicit social norms for adolescent smoking and vaping as part of the MECHANISMS smoking prevention study (incentivized experiments and a self-report survey; objective 1). Second-order measurement models established that experimental and survey measures of injunctive and descriptive norms were measuring the same underlying second-order latent variable (objective 2). SEM models verified that there was a positive association between higher anti-smoking/vaping norms (the second-order latent variable) and higher self-reported anti-smoking behavior and intentions, and lower objectively measured smoking behavior (objective 4). Therefore our experimental and survey norms measures showed comparable explanatory power related to smoking behavior and intentions following cultural adaptation of the instruments. These findings suggest that our experimental measures of social norms capture the same phenomena as the commonly used self-report survey.
Baseline MIMIC models showed that experimentally elicited injunctive norms against smoking/vaping (measured among the school year group), were stronger in Colombia than in NI, but survey responses revealed weaker anti-smoking/vaping injunctive norms in the form of Colombian pupils’ beliefs about their parents, siblings, etc. than among pupils in NI. Colombian pupils also showed weaker descriptive anti-smoking/vaping norms in both the experimental and survey measurements. Controlling for latent variable differences, the DIF analyses revealed which individual items were exhibiting measurement invariance for Colombia versus NI (objective 3). After controlling for differences on individual items, differences in experimentally derived injunctive norms and survey descriptive norms were non-significant at the latent variable level. The analysis indicates that the higher anti-smoking/vaping injunctive norms observed for Colombian pupils in their experimental responses were due entirely to differences in the items Part 2 Situation 2 and Part 2 Situation 5. The higher anti-smoking/vaping descriptive norms observed for Colombian pupils in their survey responses were also due entirely to differences in the items Descriptive Norms 2 and Descriptive Norms 3.
Differences in experimental injunctive norms were due to Colombian pupils providing lower social appropriateness ratings for items Part 2 Situation 2 (a parent smoking in their own home in front of children under the age of 5) and Part 2 Situation 5 (in a recent superhero movie the lead actor is seen smoking in the opening scene). Following the implementation of the tobacco control policy in Colombia, it has been found that smoke-free environments have a high acceptability rate among the Bogotá population (85% acceptance)79. Therefore, our Colombian participants were potentially showing an awareness of a cultural de-normalization of indoor smoking as a result of this smoke-free environment tobacco control policy when answering Part 2 Situation 280. By comparison, in 2016, one in eight young people reported living in a household with an adult who smokes inside the home in NI25. Our NI participants also reported seeing their mothers and fathers smoke more frequently than Colombian pupils, making it more likely that they see adults smoking indoors.
Regarding Part 2 Situation 5, there is considerable literature illustrating how celebrities can impact public health through their influence on knowledge, attitudes and decision-making81, and studies have shown a positive association between exposure to movie smoking and adolescent smoking rates82,83. In Colombia, the tobacco control policy includes a complete ban on tobacco advertisements, sponsorships, and promotions, and has a high level of implementation in television, cinemas and banners79. Moreover, non-paid tobacco product placement in films is not common in Latin America84. By comparison, previous research shows high rates of exposure to smoking in television and movies amongst the UK population85–87. In 2018, over 80% of adolescents (aged 11–18 years) reported seeing smoking in movies, whilst approximately 70% reported seeing smoking on television86.
Colombian pupils provided lower anti-smoking/vaping norms ratings at the latent variable level in their responses to experimental descriptive norms items compared to pupils in NI. Pupils in NI were more likely to estimate that a greater proportion of their school year group would be accepting of a close friend vaping than Colombian pupils (Part 3 Question 2). However, responses to the equivalent smoking item were similar between the two countries. A 2019 report from Public Health England shows that the number of 13–15 year olds who have never smoked but who have tried vaping is increasing in the UK88. Adolescents may be drawn towards e-cigarette use due to perceptions that they are safer and healthier than conventional cigarettes, product features (e.g. different flavourings), and marketing4. The market for e-cigarettes in Colombia is relatively new (since 2015), and they are not clearly regulated79. There is limited evidence regarding the knowledge and access amongst our target population. The UK is one of 20 countries worldwide that classifies certain types of e-cigarettes as medicinal89. Potentially, vaping is regarded as more acceptable in the UK as a result.
For the survey injunctive norms scale, the DIF analysis indicated that ratings for the items Injunctive Norms 1 (most of the people who are important to me think that I,… definitely should smoke,…definitely should not smoke) and Injunctive Norms 4 (my brother(s) think(s) that I,… definitely should smoke,… definitely should not smoke) were higher for Colombian versus NI pupils, in the opposite direction to differences at the latent variable level. Potentially the remaining items of the scale, enquiring individually about parents, sisters and friends, do not fully capture the range of individuals Colombian pupils consider to be "important to me". Future researchers may wish to consider expanding this scale to account for all potential influences and cultural differences regarding the socialization of adolescents. Cross-country differences at the latent variable level for survey descriptive norms items became non-significant when the models were adjusted for DIF on items Descriptive Norms 2 and Descriptive Norms 3. Colombian pupils were more likely to report seeing their mothers and fathers smoke less frequently than pupils in NI. In 2018, 14.7% of the UK population aged 18 years and above smoked cigarettes (15.5% NI)90. In our NI sample, 17.5% of participants reported having mothers who smoked often or very often (19.6% for fathers). Possibly, smoking rates amongst the parents of our NI participants were higher than the NI adult population in general.
Strengths and limitations
Strengths of this paper include the large sample size and use of data from schools in two settings with varying normative, cultural and health behavioral traits following a rigorous cultural adaptation of all study instruments. We also examined measurement invariance across relevant subgroups (i.e. between countries) using MIMIC models and DIF analysis, and examined associations with both self-reported and objective measures of smoking behavior. This paper has several limitations. We did not cross-validate our CFA models on an independent sample. However, due to the complexity of our models, we were reluctant to decrease power for our analysis by reducing the sample size. We examined whether data were MCAR (finding evidence that the data were not MCAR) prior to imputing missing data, and are confident that the approach was appropriate68. Our results also remained unchanged when repeating analyses without imputing missing data. The MECHANISMS study is funded as a proof of concept study involving a relatively small sample of schools in each country. Therefore, we are cautious in generalizing our findings to other schools in NI and Bogotá (Colombia). There was low power for some items in the DIF analysis. One of our first-order latent variables is measured by two items as our study’s assessment of experimentally derived descriptive norms only consisted of two items. Finally, results should be interpreted with caution due to multiple testing.
Implications for future research
This paper shows that incentivized experimental methods from the field of behavioral economics16,17,36 can be used to measure social norms for smoking and vaping behaviors amongst adolescents in two different settings. It has been proposed that such measures are less prone to bias, providing rich information regarding the distribution of acceptable actions (i.e. norms) and individuals’ norm-following sensitivities that can better explain behavioral heterogeneity within and between different settings14,16,36. Our MIMIC models and DIF analyses indicated when items operated differently from the rest of their scale (e.g. item Injunctive Norms 1 and Injunctive Norms 4). Future researchers may wish to consider amending/deleting such items or expanding the scale before conducting research with children from diverse backgrounds. Our MIMIC models also showed positive associations between personality variables (need to belong, pro-social behavior, openness, extraversion, agreeableness, conscientiousness, and emotional stability) and greater perceived anti-smoking/vaping norms. Therefore, when designing interventions attempting to leverage peer influence to promote smoking prevention amongst adolescents (e.g. the ASSIST programme), interventionists may wish to consider whether certain personality types may be more (or less) suited to transmit anti-smoking/vaping norms91. Future research should investigate whether these findings translate to larger, more diverse samples, and different countries.
Conclusions
The MECHANISMS study was conducted with 11–13 year old school pupils in NI (UK) and 11–15 year olds in Bogotá (Colombia) over a single school semester in 15 schools. This paper contributes evidence supporting the construct validity of incentivized experimental and self-report methods of eliciting injunctive and descriptive social norms for adolescent smoking and vaping behaviors. A second-order CFA model confirmed that the experimental and survey norms measures were measuring the same underlying latent construct of anti-smoking/vaping norms. Thus, we propose that the two methods could be used as complementary measures, to provide a richer understanding of the mechanisms through which social norms influence health-related attitudes and behavior. MIMIC modelling and DIF analyses showed that our norms measurements reflected differences between relevant subgroups of participants (i.e. between two settings varying in smoking rates, culture, and norms). Future research should investigate whether these results vary across repeated measurements and whether they apply in different countries.
Supplementary information
Acknowledgements
The authors wish to thank the teachers and pupils in participating schools in each country. We also wish to acknowledge the support from our partners Cancer Focus Northern Ireland and Evidence to Impact. The MECHANISMS study was funded by the Medical Research Council (ref. MR/R011176/1). The authors would also like to acknowledge funding received from the Health and Social Care Research and Development Office (HSC RDO).
Author contributions
J.M.M. is a Research Fellow working on the study, led the statistical analysis and drafted the manuscript. E.O.K. is a study co-Investigator, designed the experiments, advised on the statistical analysis and helped draft the manuscript. E.L.K., A.R. and R.K. are study co-Investigators and designed the experiments. S.S.F. collected the information provided about the legal framework in Colombia and assisted with the interpretation of the results in Colombia. J.M.P. advised on the conduct of the statistical analysis. O.L.S., F.K. and R.F.H. are study Principal Investigators and helped draft the manuscript. All authors reviewed and approved the final manuscript.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Code availability
The code used to generate the results reported in the current study are included in the supplementary files.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors jointly supervised this work: Frank Kee and Ruth F. Hunter.
Contributor Information
Jennifer M. Murray, Email: Jennifer.Murray@qub.ac.uk
Ruth F. Hunter, Email: ruth.hunter@qub.ac.uk
Supplementary information
is available for this paper at 10.1038/s41598-020-72784-z.
References
- 1.World Health Organization. Global Adult Tobacco Survey (GATS). Tobacco Free Initiative (TFI) (2017). Available at: https://www.who.int/tobacco/surveillance/survey/gats/en/. (Accessed: 21st June 2018)
- 2.Vitória PD, Salgueiro MF, Silva SA, de Vries H. Social influence, intention to smoke, and adolescent smoking behaviour longitudinal relations. Br. J. Health Psychol. 2011;16:779–798. doi: 10.1111/j.2044-8287.2010.02014.x. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Office on Smoking and Health. A Report of the Surgeon General: Preventing Tobacco Use Among Youth and Young Adults. Washington DC (2012). https://www.cdc.gov/tobacco/data_statistics/sgr/2012/consumer_booklet/pdfs/consumer.pdf. Accessed 9 Sept 2020. [PubMed]
- 4.Perikleous EP, Steiropoulos P, Paraskakis E, Constantinidis TC, Nena E. E-cigarette use among adolescents: an overview of the literature and future perspectives. Front. Public Health. 2018;6:1. doi: 10.3389/fpubh.2018.00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schneider S, Diehl K. Vaping as a catalyst for smoking? An initial model on the initiation of electronic cigarette use and the transition to tobacco smoking among adolescents. Nicotine Tob. Res. 2016;18:647–653. doi: 10.1093/ntr/ntv193. [DOI] [PubMed] [Google Scholar]
- 6.Wang B, King BA, Corey CG, Arrazola RA, Johnson SE. (2012) Awareness and use of non-conventional tobacco products among U.S. students. Am. J. Prev. Med. 2014;47:S36. doi: 10.1016/j.amepre.2014.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General [Internet]. E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General (Centers for Disease Control and Prevention (US), 2016). [PubMed]
- 8.Wills TA, Sargent JD, Knight R, Pagano I, Gibbons FX. E-cigarette use and willingness to smoke: a sample of adolescent non-smokers. Tob. Control. 2016;25:e52–e59. doi: 10.1136/tobaccocontrol-2015-052349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pepper JK, et al. Adolescent males’ awareness of and willingness to try electronic cigarettes. J. Adolesc. Health. 2013;52:144–150. doi: 10.1016/j.jadohealth.2012.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas RE, McLellan J, Perera R. Effectiveness of school-based smoking prevention curricula: systematic review and meta-analysis. BMJ Open. 2015;5:e006976. doi: 10.1136/bmjopen-2014-006976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Campbell R, et al. An informal school-based peer-led intervention for smoking prevention in adolescence (ASSIST): a cluster randomised trial. Lancet (London, England) 2008;371:1595–1602. doi: 10.1016/S0140-6736(08)60692-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmed SK, Mitchell P, Trevitt J. Social Norms Approach in Secondary Schools: Literature Review. Camberwell: Australian Council for Educational Research Ltd; 2018. [Google Scholar]
- 13.Hunter RF, et al. MECHANISMS Study: using Game Theory to assess the effects of social norms and social networks on adolescent smoking in schools—study protocol. Front. Public Heal. 2020;8:377. doi: 10.3389/fpubh.2020.00377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mackie, G., Moneti, F., Shakya, H. & Denny, E. What Are Social Norms - How Are They Measured? San Diego (2015). https://www.unicef.org/protection/files/4_09_30_Whole_What_are_Social_Norms.pdf. Accessed 9 Sept 2020.
- 15.Efferson C, Vogt S, Elhadi A, El Fadil Ahmed H, Fehr E. Female genital cutting is not a social coordination norm. Science. 2015;349:1446. doi: 10.1126/science.aaa7978. [DOI] [PubMed] [Google Scholar]
- 16.Krupka EL, Weber RA. Identifying social norms using coordination games: why does dictator game sharing vary? J. Eur. Econ. Assoc. 2013;11:495–524. doi: 10.1111/jeea.12006. [DOI] [Google Scholar]
- 17.Kimbrough EO, Vostroknutov A. A portable method of eliciting respect for social norms. Econ. Lett. 2018;168:147–150. doi: 10.1016/j.econlet.2018.04.030. [DOI] [Google Scholar]
- 18.Krupka EL, Leider S, Jiang M. A meeting of the minds: Informal agreements and social norms. Manag. Sci. 2017;63:1708–1729. doi: 10.1287/mnsc.2016.2429. [DOI] [Google Scholar]
- 19.Burks SV, Krupka EL. A multimethod approach to identifying norms and normative expectations within a corporate hierarchy: evidence from the financial services industry. Manag. Sci. 2012;58:203–217. doi: 10.1287/mnsc.1110.1478. [DOI] [Google Scholar]
- 20.Gilmore AB, Fooks G, Drope J, Bialous SA, Jackson RR. Exposing and addressing tobacco industry conduct in low-income and middle-income countries. Lancet. 2015;385:1029–1043. doi: 10.1016/S0140-6736(15)60312-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The World Bank. Data, United Kingdom. (2020). Available at: https://data.worldbank.org/country/united-kingdom?view=chart. (Accessed: 6th June 2020)
- 22.Northern Ireland Statistics and Research Agency. 2018 Mid-year Population Estimates for Northern Ireland. (2019). Available at: https://www.nisra.gov.uk/news/2018-mid-year-population-estimates-northern-ireland. (Accessed: 4th June 2020)
- 23.The World Bank. Data, Colombia. (2020). Available at: https://data.worldbank.org/country/colombia. (Accessed: 6th June 2020)
- 24.National Administrative Department of Statistics. How many are we? Colombia National Census 2018 (2019). Available at: https://sitios.dane.gov.co/cnpv/#!/donde_estamos. (Accessed: 4th June 2020)
- 25.Foster, C., Scarlett, M. & Stewart, B. Young Persons’ Behaviour and Attitude Survey 2016 Health Modules. Belfast (2017). https://www.health-ni.gov.uk/articles/young-persons-behaviour-attitudes-survey. Accessed 30 Mar 2020.
- 26.Ministry of Justice and Law, Ministry of National Education, Ministry of Health and Social Protection. National Study of Psychoactive Substance Use in School Population Colombia. Bogotá (2016). https://www.unodc.org/documents/colombia/2018/Junio/CO03142016_estudio_consumo_escolares_2016.pdf. Accessed 9 Sept 2020.
- 27.Action on Smoking and Health (ASH). Use of E-Cigarettes among Young People in Great Britain. London (2019). http://ash.org.uk/category/information-and-resources/. Accessed 30 July 2020.
- 28.Action on Smoking and Health (ASH). Young People and Smoking. London (2019). http://ash.org.uk/category/information-and-resources/briefings/1. Accessed 30 July 2020.
- 29.Ministry of Health and Social Protection Government of Colombia. Presentation of Results of the National Survey of School Health (ENSE) and the National Survey of Smoking in Youth (ENTJ) 2017 [Presentation]. (2019). Available at: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/ED/GCFI/ense-entj-presentaciones.zip.
- 30.Ministerio de Salud y Protección Social. Ley 1335 de 2009 (Julio 21). (2009). Available at: https://www.alcaldiabogota.gov.co/sisjur/normas/Norma1.jsp?i=36878.
- 31.Uang R, Crosbie E, Glantz SA. Tobacco control law implementation in a middle-income country: Transnational tobacco control network overcoming tobacco industry opposition in Colombia. Global Public Health. 2018;13:1050–1064. doi: 10.1080/17441692.2017.1357188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Müller F, Wehbe L. Smoking and smoking cessation in Latin America: a review of the current situation and available treatments. Int. J. COPD. 2008;3:285–293. doi: 10.2147/COPD.S2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elias J, Ling PM. Origins of tobacco harm reduction in the UK: the ‘Product Modification Programme’ (1972–1991) Tob. Control. 2018;27:e12. doi: 10.1136/tobaccocontrol-2017-054021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Action on Smoking and Health (ASH). Key Dates in the History of Anti-Tobacco Campaigning. London (2017). https://ash.org.uk/information-and-resources/briefings/key-dates-in-the-history-of-anti-tobacco-campaigning/. Accessed 6 June 2020.
- 35.Thurston A, et al. A randomized controlled efficacy trial of a smoking prevention programme with Grade 8 students in high schools. Int. J. Educ. Res. 2019;93:23–32. doi: 10.1016/j.ijer.2018.10.003. [DOI] [Google Scholar]
- 36.Kimbrough EO, Vostroknutov A. Norms Make Preferences Social. J. Eur. Econ. Assoc. 2016;14:608–638. doi: 10.1111/jeea.12152. [DOI] [Google Scholar]
- 37.Barrera M, Castro FG. A heuristic framework for the cultural adaptation of interventions. Clin. Psychol. Sci. Pract. 2006;13:311–316. doi: 10.1111/j.1468-2850.2006.00043.x. [DOI] [Google Scholar]
- 38.Barrera M, Castro F. Cultural Adaptation of Behavioral Health interventions: A Progress Report. J. Consult. Clin. Psychol. 2013;81:196–205. doi: 10.1037/a0027085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cremers H-P, Mercken L, Oenema A, de Vries H. A web-based computer-tailored smoking prevention programme for primary school children: intervention design and study protocol. BMC Public Health. 2012;12:277. doi: 10.1186/1471-2458-12-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fuller E, Hawkins V. Smoking, Drinking and Drug Use Among Young People in England in 2011. London: Health and Social Care Information Centre; 2012. [Google Scholar]
- 41.Dunne L, Thurston A, Gildea A, Kee F, Lazenbatt A. Protocol: A randomised controlled trial evaluation of Cancer Focus NI’s ‘Dead Cool’ smoking prevention programme in post-primary schools. Int. J. Educ. Res. 2016;75:24–30. doi: 10.1016/j.ijer.2015.06.009. [DOI] [Google Scholar]
- 42.Mazanov J, Byrne DG. ‘“Do you intend to smoke?”’: A test of the assumed psychological equivalence in adolescent smoker and nonsmoker intention to change smoking behaviour. Aust. J. Psychol. 2007;59:34–42. doi: 10.1080/00049530600944366. [DOI] [Google Scholar]
- 43.Leary MR, Kelly KM, Cottrell CA, Schreindorfer LS. Construct validity of the Need to Belong Scale: mapping the nomological network. J. Pers. Assess. 2013;95:610–624. doi: 10.1080/00223891.2013.819511. [DOI] [PubMed] [Google Scholar]
- 44.Bevelander KE, et al. Youth’s social network structures and peer influences: study protocol MyMovez project - Phase I. BMC Public Health. 2018;18:504. doi: 10.1186/s12889-018-5353-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leary MR. A brief version of the fear of negative evaluation scale. Personal. Soc. Psychol. Bull. 1983;9:371–375. doi: 10.1177/0146167283093007. [DOI] [Google Scholar]
- 46.Collins KA, Westra HA, Dozois DJA, Stewart SH. The validity of the brief version of the fear of negative evaluation scale. J. Anxiety Disord. 2005;19:345–359. doi: 10.1016/j.janxdis.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 47.Goodman R, Meltzer H, Bailey V. The Strengths and Difficulties Questionnaire: a pilot study on the validity of the self-report version. Int. Rev. psychiatry. 2003;15:173–177. doi: 10.1080/0954026021000046137. [DOI] [PubMed] [Google Scholar]
- 48.Morizot J. Construct validity of adolescents’ self-reported Big Five personality traits. Assessment. 2014;21:580–606. doi: 10.1177/1073191114524015. [DOI] [PubMed] [Google Scholar]
- 49.Ortet G, Martínez T, Mezquita L, Morizot J, Ibáñez MI. Big Five Personality Trait Short Questionnaire: preliminary validation with Spanish adults. Span. J. Psychol. 2017;20:1–11. doi: 10.1017/sjp.2017.8. [DOI] [PubMed] [Google Scholar]
- 50.Bedfont Scientific Ltd. Smokerlyzer Range: User Manual. Kent (2018). https://www.bedfont.com/documents/2910-LAB679 Smokerlyzer Manual - Issue 4.pdf. Accessed 9 Sept 2020.
- 51.Deveci SE, Deveci F, Açik Y, Ozan AT. The measurement of exhaled carbon monoxide in healthy smokers and non-smokers. Respir. Med. 2004;98:551–556. doi: 10.1016/j.rmed.2003.11.018. [DOI] [PubMed] [Google Scholar]
- 52.Joreskog KG, Goldberger AS. Estimation of a model with multiple indicators and multiple causes of a single latent variable. J. Am. Stat. Assoc. 1975;70:631. [Google Scholar]
- 53.Ríos-Bedoya CF, Pomerleau CS, Neuman RJ, Pomerleau OF. Using MIMIC models to examine the relationship between current smoking and early smoking experiences. Nicotine Tob. Res. 2009;11:1035–1041. doi: 10.1093/ntr/ntp093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.StataCorp . Stata Statistical Software: Release 13. College Station: StataCorp LP; 2013. [Google Scholar]
- 55.R Core Team . R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing; 2019. [Google Scholar]
- 56.Myers R. Data Management and Statistical Analysis Techniques. New Delhi: Scientific e-Resources; 2019. [Google Scholar]
- 57.Bollen K. Structural Equations with Latent Variables. New York: Wiley; 1989. [Google Scholar]
- 58.Kenny DA, Kashy D, Bolger N. Data analysis in social psychology. In: Gilbert D, Fiske S, Lindzey G, editors. Handbook of Social Psychology. New York: McGraw-Hill; 1998. pp. 233–265. [Google Scholar]
- 59.Rosseel Y. lavaan: An R package for structural equation modeling. J. Stat. Softw. 2012;48:1–36. doi: 10.18637/jss.v048.i02. [DOI] [Google Scholar]
- 60.Mardia KV. Measures of multivariate skewness and kurtosis with applications. Biometrika. 1970;57:519. doi: 10.1093/biomet/57.3.519. [DOI] [Google Scholar]
- 61.Muthén B, Kaplan D. A comparison of some methodologies for the factor analysis of non-normal Likert variables. Br. J. Math. Stat. Psychol. 1985;38:171–189. doi: 10.1111/j.2044-8317.1985.tb00832.x. [DOI] [Google Scholar]
- 62.Lei P-W, Shiverdecker LK. Performance of estimators for confirmatory factor analysis of ordinal variables with missing data. Struct. Equ. Model. A Multidiscip. J. 2019;6:1–18. [Google Scholar]
- 63.Huber, P. J. The behavior of maximum likelihood estimates under nonstandard conditions. In Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability, vol. 1, 221–233 (University of California Press, 1967).
- 64.White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817. doi: 10.2307/1912934. [DOI] [Google Scholar]
- 65.Raykov T. Scale construction and development using structural equation modeling. In: Hoyle RH, editor. Handbook of Structural Equation Modelling. New York: The Guilford Press; 2012. pp. 472–492. [Google Scholar]
- 66.Rigdon E. Structural equation modeling. In: Marcoulides GA, editor. Modern Methods for Business Research. Mahwah: Erlbaum; 1998. pp. 251–294. [Google Scholar]
- 67.Little RJA. A test of missing completely at random for multivariate data with missing values. J. Am. Stat. Assoc. 1988;83:1198–1202. doi: 10.1080/01621459.1988.10478722. [DOI] [Google Scholar]
- 68.Jakobsen JC, Gluud C, Wetterslev J, Winkel P. When and how should multiple imputation be used for handling missing data in randomised clinical trials—a practical guide with flowcharts. BMC Med. Res. Methodol. 2017;17:162. doi: 10.1186/s12874-017-0442-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hooper D, Coughlan J, Mullen M. Structural equation modelling: guidelines for determining model fit. Electron. J. Bus. Res. Methods. 2008;6:53–60. [Google Scholar]
- 70.Kline RB. Principles and Practice of Structural Equation Modeling. New York: The Guildford Press; 2011. [Google Scholar]
- 71.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 72.Schermelleh-Engel K, Moosbrugger H. Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods Psychol. Res. 2003;8:23–74. [Google Scholar]
- 73.Joreskog K, Long J. Introduction. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. London: Sage; 1993. [Google Scholar]
- 74.Joreskog K. Testing structural equation models. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. London: Sage; 1993. [Google Scholar]
- 75.Woods CM, Oltmanns TF, Turkheimer E. Illustration of MIMIC-model DIF testing with the schedule for nonadaptive and adaptive personality. J. Psychopathol. Behav. Assess. 2009;31:320–330. doi: 10.1007/s10862-008-9118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Woods CM. Evaluation of MIMIC-model methods for DIF testing with comparison to two-group analysis. Multivariate Behav. Res. 2009;44:1–27. doi: 10.1080/00273170802620121. [DOI] [PubMed] [Google Scholar]
- 77.Saris WE, Satorra A, Sorbom D. The detection and correction of specification errors in structural equation models. Sociol. Methodol. 1987;17:105. doi: 10.2307/271030. [DOI] [Google Scholar]
- 78.Fox R, Hyland P, McHugh-Power J, Coogan AN. Posttraumatic stress disorder among older adults: A differential item functioning analysis of PTSD in ICD-11 and DSM-5. Psychol. Trauma Theory Res. Pract. Policy. 2020 doi: 10.1037/tra0000596. [DOI] [PubMed] [Google Scholar]
- 79.Colombia Ombudsman Office. Follow-up report on compliance with the WHO Framework Convention on Tobacco Control in Colombia. (2017).
- 80.Otálvaro-Ramírez S, Rodríguez-Lesmes P, Gallego JM. Tobacco Control Protocol and Household Smoking Behavior: The Case of Bogotá, Colombia. Bogotá: Universidad del Rosario; 2019. [Google Scholar]
- 81.Hoffman SJ, et al. Celebrities’ impact on health-related knowledge, attitudes, behaviors, and status outcomes: protocol for a systematic review, meta-analysis, and meta-regression analysis. Syst. Rev. 2017;6:13. doi: 10.1186/s13643-016-0395-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Morgenstern M, et al. Smoking in movies and adolescent smoking: cross-cultural study in six European countries. Thorax. 2011;66:875–883. doi: 10.1136/thoraxjnl-2011-200489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Thrasher JF, et al. Does film smoking promote youth smoking in middle-income countries? A longitudinal study among Mexican adolescents. Cancer Epidemiol. Biomarkers Prev. 2009;18:3444–3450. doi: 10.1158/1055-9965.EPI-09-0883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Aguinaga Bialous, S. & Shatenstein, S. Profits over People: Tobacco Industry Activities to Market Cigarettes and Undermine Public Health in Latin America and the Caribbean. Washington DC (2002). https://escholarship.org/uc/item/82r4v193. Accessed 9 Sept 2020.
- 85.Anderson SJ, Millett C, Polansky JR, Glantz SA. Exposure to smoking in movies among british adolescents 2001–2006. Tob. Control. 2010;19:197–200. doi: 10.1136/tc.2009.034991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Action on Smoking and Health (ASH). Commons Committee Warned That Smoking on TV and in Films Is Encouraging Child Take-up - Action on Smoking and Health. London (2018). https://ash.org.uk/media-and-news/press-releases-media-and-news/commons-committee-warned-that-smoking-on-tv-and-in-films-is-encouraging-child-take-up/. Accessed 8 June 2020.
- 87.Barker AB, Opazo Breton M, Cranwell J, Britton J, Murray RL. Population exposure to smoking and tobacco branding in the UK reality show ‘Love Island’. Tob. Control. 2018;27:709–711. doi: 10.1136/tobaccocontrol-2017-054125. [DOI] [PubMed] [Google Scholar]
- 88.McNeill, A., Brose, L. S., Calder, R., Bauld, L. & Robson, D. Vaping in England: Evidence Update Summary February 2019. A Report Commissioned by Public Health England. London (2019). https://www.gov.uk/government/publications/vaping-in-england-an-evidence-update-february-2019/vaping-in-england-evidence-update-summary-february-2019. Accessed 19 Feb 2020.
- 89.Kennedy RD, Awopegba A, De León E, Cohen JE. Global approaches to regulating electronic cigarettes. Tob. Control. 2017;26:440–445. doi: 10.1136/tobaccocontrol-2016-053179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Office for National Statistics. Adult smoking habits in the UK. (2018). Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/bulletins/adultsmokinghabitsingreatbritain/2018. (Accessed: 19th February 2020)
- 91.Heine SJ, Buchtel EE. Personality: The universal and the culturally specific. Annu. Rev. Psychol. 2009;60:369–394. doi: 10.1146/annurev.psych.60.110707.163655. [DOI] [PubMed] [Google Scholar]
- 92.Cremers HP, Oenema A, Mercken L, Candel M, De Vries H. Explaining socio-economic differences in intention to smoke among primary school children. BMC Public Health. 2014;14:191. doi: 10.1186/1471-2458-14-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
The code used to generate the results reported in the current study are included in the supplementary files.