Abstract
Background
Practitioners expected the Affordable Care Act (ACA) to increase availability of health services and access to treatment for Americans with substance use disorders (SUDs). Yet research has not examined the associations among ACA enrollment mechanisms, deductibles, and the use of SUD treatment and other healthcare services. Understanding these relationships can inform future healthcare policy.
Methods
We conducted a longitudinal analysis of patients with SUDs newly enrolled in the Kaiser Permanente Northern California health system in 2014 (N=6,957). Analyses examined the likelihood of service utilization (primary care, specialty SUD treatment, psychiatry, inpatient, and emergency department [ED]) over three years after SUD diagnosis, and associations with enrollment mechanisms (ACA Exchange vs. other), deductibles (none, $1–$999 [low] and ≥$1,000 [high]), membership duration, psychiatric comorbidity, and demographic characteristics. We also evaluated whether the enrollment mechanism moderated the associations between deductible limits and utilization likelihood.
Results
Service utilization was highest in the 6 months after SUD diagnosis, decreased in the following 6 months, and remained stable in years 2–3. Relative to patients with no deductible, those with a high deductible had lower odds of using all health services except SUD treatment; associations with primary care and psychiatry were strongly negative among Exchange enrollees. Among non-Exchange enrollees, patients with deductibles were more likely than those without deductibles to receive SUD treatment. Exchange enrollment compared to other mechanisms was associated with less ED use. Psychiatric comorbidity was associated with greater use of all services. Nonwhite patients were less likely to initiate SUD and psychiatry treatment.
Conclusions
Higher deductibles generally were associated with use of fewer health services, especially in combination with enrollment through the Exchange. The role of insurance factors, psychiatric comorbidity and race/ethnicity in health services for people with SUDs are important to consider as health policy evolves.
Keywords: Affordable Care Act, Substance use disorder, Mental health, Race/ethnic disparities, Health insurance, Deductible
1. Introduction
Health care reform in the United States has had major implications for people with substance use disorders (SUDs) (Buck, 2011; Druss & Mauer, 2010; Molfenter, Capoccia, Boyle, & Sherbeck, 2012), including greater opportunities to enroll in private insurance coverage, increased access to services, and changes in health care costs (Feder et al., 2017; Saloner, Bandara, Bachhuber, & Barry, 2017). The Affordable Care Act (ACA) (U.S. Congress, 2010) established state insurance exchanges to promote and offer health coverage, and mandated SUD and psychiatric disorder treatment as essential benefits. Practitioners expected these ACA mandates, implemented in 2014, to increase access to care (Humphreys & Frank, 2014; Tai & Volkow, 2013).
Following ACA implementation in 2014, the overall number of individuals living without insurance dropped (Maclean & Saloner, 2019; Thomas, Shartzer, Kurth, & Hall, 2018). Evidence suggests a positive impact of the ACA on both SUD and psychiatry coverage (Cowell, Prakash, Jones, Barnosky, & Wedehase, 2018; Novak, Anderson, & Chen, 2018; Shover, Abraham, D’Aunno, Friedmann, & Humphreys, 2019), including an increase in insurance choices (Abraham et al., 2017; Andrews et al., 2018; Feder et al., 2017). The number of individuals with identified SUDs enrolled in health plans increased (Campbell, Parthasarathy, Altschuler, Young-Wolff, & Satre, 2018). But access to services remains a major concern (Feder et al., 2017; Saloner et al., 2017), and much is still unknown regarding how ACA-associated enrollment through insurance exchanges and cost-sharing structures (especially deductibles) are associated with access to and use of SUD treatment and other health services in this complex patient population.
SUD treatment initiation and retention are key clinical goals for SUD patients (Mertens & Weisner, 2000; Satre, Campbell, Gordon, & Weisner, 2010; Satre, Mertens, Arean, & Weisner, 2004). Specific characteristics of the ACA, such as enrollment via new state insurance exchanges and increased patient cost sharing via higher deductibles, may influence treatment differentially for people with SUDs who may be new enrollees (with or without prior coverage). Patient cost sharing (e.g., high deductibles) may adversely impact both initiation and retention. If SUD treatment and psychiatry services are viewed as discretionary and less essential than primary care, they may be especially vulnerable to cost-sharing mechanisms (Lo Sasso & Lyons, 2002, 2004; Stein, Orlando, & Sturm, 2000). A previous evaluation of SUD patients enrolled in the same California healthcare system found that compared to a pre-ACA enrollment cohort with SUDs, post-ACA SUD patients had more psychiatric and medical conditions and greater enrollment in high-deductible plans. Although this prior work did not examine patterns of health service utilization, the findings suggest that newly enrolled patients post-ACA may have greater clinical needs as well as increased financial obstacles to accessing services (Campbell et al., 2018). It is important to not only evaluate SUD treatment initiation and retention over time following implementation of the ACA, but also to evaluate how factors related to the ACA may influence utilization of other health services.
The current study aimed to extend what is currently known about the consequences of healthcare reform by examining the potential relationship of ACA exchange enrollment and high deductible health plans to trends in health service utilization in a cohort of individuals who were newly enrolled in a healthcare system and had a documented SUD. We examined factors associated with utilization as conceptualized by the Andersen model of healthcare utilization (Andersen, 1995; Weisner, Matzger, Tam, & Schmidt, 2002), which proposes that utilization is determined by predisposing (e.g., race/ethnicity and other demographic factors) need (e.g., diagnoses) (Andersen, 1995) and enabling factors (e.g., benefit plan, Exchange enrollment) (Dhingra, Zack, Strine, Pearson, & Balluz, 2010). We hypothesized that psychiatric comorbidity would be associated with greater use of health services, and that members with higher deductibles would be less likely to initiate SUD and psychiatry treatment but would have higher emergency department (ED) and inpatient utilization than those without deductibles. As with earlier studies (Holder, 1998; Parthasarathy, Weisner, Hu, & Moore, 2001), which indicate that SUD diagnosis is often precipitated by a critical event such as an ED visit, we expected that postdiagnosis utilization would be highest in the period immediately following diagnosis but would likely decrease over time, although trajectories would vary by type of utilization. Knowing how these factors are associated with use of healthcare can be highly informative to future healthcare reform and behavioral health services research.
2. Methods
2.1. Study setting
Kaiser Permanente Northern California (KPNC) is an integrated healthcare system serving approximately 4 million members (45% of the commercially insured population in the region) (Terhune, 2013). The membership is racially and socioeconomically diverse and representative of the demographic of the geographic area (Gordon, 2015; Selby et al., 2005). SUD treatment is provided in specialty clinics within KPNC, which patients can access directly without a referral. The group-based treatment model (with individual counseling and medications as needed) is similar to outpatient treatment programs nationwide. Treatment sessions take place daily or four times a week, depending on severity, for nine weeks (Satre et al., 2004). Treatment in psychiatry includes assessment, individual and group psychotherapy, and medication management (Lake & Turner, 2017). KPNC is not contracted to provide SUD care or intensive psychiatry treatment for Medicaid patients and those patients are referred to county providers. The University of California, San Francisco and Kaiser Permanente Northern California Institutional Review Boards approved the study and approved a waiver of informed consent.
2.2. Data source and cohort
We extracted all data from electronic health records (EHRs). The study cohort included adults aged 18–64 years who were newly enrolled in KPNC between 1/1/2014 and 12/31/2014, had an SUD diagnosis documented in the EHR within one year of enrollment, and were still enrolled in the six months following their SUD diagnosis (n=6,957). We focused on new enrollees based on the premise that ACA-related influence would be more apparent among first-time enrollees than in the overall SUD-diagnosed membership. We included individuals with Medicaid (17%) but excluded individuals aged 65 and older because the ACA has less directly impacted Medicare enrollees. We used International Classification of Diseases, Version 9, (ICD-9) codes of 291, 292, 303–305 (excluding 305.1 of tobacco dependence) and ICD-10 codes of F10–F19 to identify SUDs; we excluded those with tobacco use disorder only.
2.3. Measures
We extracted patient demographic, clinical, and service utilization data for the 36 months following the first SUD diagnosis date (the index date), giving each individual up to 36 months of follow-up except in the case of death or disenrollment. We aggregated longitudinal data into 6-month intervals, yielding a maximum of 6 repeated measures for every individual.
2.3.1. Demographics
We linked sex, age at index date, and race/ethnicity using unique identifiers.
2.3.2. Type of SUD
We identified the type of SUD (e.g., alcohol, cannabis, amphetamines, cocaine, opioids, hallucinogens, and sedatives), and comorbid tobacco use disorder.
2.3.3. Membership duration before SUD diagnosis
We calculated the duration of time between enrollment at KPNC and patients’ index date (e.g. first SUD diagnosis), and categorized patients based on whether they were members for <6 months or ≥6 months before their index date.
2.3.4. Chronic medical comorbidities
We identified common chronic medical conditions (Ornstein, Nietert, Jenkins, & Litvin, 2013), many of which are known to be associated with SUDs (Mertens, Lu, Parthasarathy, Moore, & Weisner, 2003) using ICD-9/10 codes recorded within the first year after initial enrollment. Conditions included asthma, atherosclerosis, atrial fibrillation, chronic kidney disease, chronic liver disease, chronic obstructive pulmonary disease, coronary disease, diabetes mellitus, dementia, epilepsy, gastroesophageal reflux, heart failure, hyperlipidemia, hypertension, migraine, osteoarthritis, osteoporosis and osteopenia, Parkinson’s disease or syndrome, peptic ulcer, and rheumatoid arthritis. Patients with chronic medical conditions utilize more health services than patients without such conditions (Gulley, Rasch, & Chan, 2011), which may influence their decision to choose a plan with a lower (or no) deductible if given an option (Gulley et al., 2011), so we included this covariate to control for confounding.
2.3.5. Psychiatric disorder comorbidities
Using ICD-9/10 codes recorded within the first year of initial enrollment at KPNC, we identified psychiatric disorders regulated by California mental health parity law (i.e., bipolar disorder, depressive disorders, developmental disorders, eating disorders, obsessive compulsive and panic disorders, and schizophrenia) (Disability Rights California, 2014), plus anxiety disorders.
2.3.6. Individual deductible limits and ACA exchange mechanisms
Deductibles are features across different benefit plans, including commercial plans, but are more common in ACA benefit plans. The individual deductible limit is the amount the individual must pay out-of-pocket for health expenses before eligibility for health plan benefits. At KPNC, there are many types of benefit plans that include deductibles. Patients with deductible plans that do not include SUD as a covered benefit are responsible for bearing the cost of those services until their deductible is reached, and/or the accumulating cost of copays for multiple visits as part of the SUD care model. We did not include type of insurance (beyond deductible limits) as a covariate due to its collinearity with deductible limits and enrollment via the ACA exchange (Medicaid patients did not have a deductible and enrolled through another mechanism).
We categorized deductible limits into three levels (none, 1–$999 and ≥$1,000), as in prior research (Parthasarathy & Campbell, 2016) and based on the definition of high deductibles (Galbraith et al., 2011) and benefit plans available at KPNC during this period. Since deductible limits may change over time, we used the minimum level over each 6-month time window during follow-up. We imputed missing deductible levels during a given 6-month window (n=231) with the last known value during the follow-up period, and we dropped patients with no known deductible limit during the entire 36 months of follow-up from the analysis (n=25).
Coverage mechanism included enrollment via the California Exchange vs. other mechanisms (e.g., employer-based large group purchasers or individual plans not purchased on the Exchange).
2.3.7. Service utilization
We examined outpatient visits in primary care, specialty SUD treatment and psychiatry, and inpatient hospitalization and ED use. We aggregated utilization in each 6-month time interval as total counts and dichotomous measures (any utilization vs. none).
2.4. Analyses
We summarized utilization data into 6-month intervals, and we examined trends in health service utilization over 36 months after patients received an SUD diagnosis with Chi-squared tests using 6-month intervals. Using multivariable logistic regression, we examined associations between deductible limits, enrollment via the California ACA Exchange, membership duration, and psychiatric comorbidity; and the likelihood of utilizing health services (dichotomous—any use versus none) in the 36-month follow-up period, controlling for patient demographic characteristics (i.e., gender, age, and race/ethnicity) and chronic medical comorbidity. We also evaluated whether enrollment via the California ACA exchange moderated the associations between deductible limits and the likelihood of utilization by adding interaction terms to the multivariable models. We estimated the associations with deductible limits for each enrollment mechanism by constructing hypothesis tests and confidence intervals on linear combinations of the regression coefficients from these models. To account for correlation between repeated measures, we used the generalized estimating equations methodology (Liang & Zeger, 1986). We censored patients at a given 6-month interval if they were not a member of KPNC during that time.
We conducted a sensitivity analysis to determine whether high utilizers leaving the health system influenced the observed pattern of decreased utilization from the 0–6 month to the 6–12 month follow-up periods. Using Chi-squared tests, we compared utilization during the 0–6 month period between patients who remained in the cohort (noncensored group) and patients who disenrolled from KPNC (censored group) at 6–12 months. We hypothesized that if the censored group had greater utilization than the noncensored group, then there would be evidence of high utilizers leaving the health system. We also conducted Chi-squared tests to determine whether censorship was associated with deductible limits and enrollment mechanisms.
We conducted all analyses using SAS v9.4. We assessed significance at a p-value < 0.05.
3. Results
3.1. Cohort characteristics and bivariate associations
The final study cohort consisted of 6,957 patients, who were 62% male and 58% white (Table 1), with a mean age of 39 years (SD=12; data not shown). About 17% enrolled via the California ACA Exchange, among whom a larger proportion enrolled in plans with high (≥$1,000) and low ($1–$999) deductibles (28% and 37%, respectively), compared to patients who enrolled via other mechanisms (17% and 7%, respectively). The average duration of KPNC membership before receiving an SUD diagnosis was 146 days (SD=106), with 64% of the cohort having <6 months of membership. Alcohol (58%) and cannabis use disorder (30%) were the most commonly diagnosed SUDs. More than half of the cohort had a psychiatric disorder (58%); anxiety (37%) and depressive disorders (36%) were the most prevalent. Approximately 61% of the cohort had a chronic medical comorbidity. Patient characteristics by deductible limit (Table S1) and type of SUD diagnosis (Table S2) are presented in the Supplementary Material.
Table 1.
Baseline a patient demographic, clinical characteristics, and insurance coverage of newly enrolled Kaiser Permanente Northern California members with substance use disorders (SUDs) post-ACA in 2014 by enrollment mechanism.
|
n (%b) |
||||
|---|---|---|---|---|
| Characteristic | Overall | ACA Exchange | Other | p-value c |
| Overall | 6,957 (100) | 1,209 (17.4) | 5,748 (82.6) | |
| Gender | 0.020 | |||
| Male | 4,281 (61.5) | 779 (64.4) | 3,502 (60.9) | |
| Female | 2,676 (38.5) | 430 (35.6) | 2,246 (39.1) | |
| Age group | <.001 | |||
| 18–34 | 3,092 (44.4) | 410 (33.9) | 2,682 (46.7) | |
| 35–49 | 2,153 (30.9) | 342 (28.3) | 1,811 (31.5) | |
| 50–64 | 1,712 (24.7) | 457 (37.8) | 1,255 (21.8) | |
| Race/ethnicity | <.001 | |||
| White | 4,048 (58.2) | 809 (66.9) | 3,239 (56.4) | |
| Black | 904 (13.0) | 67 (5.5) | 837 (14.6) | |
| Asian, Native Hawaiian, or Pacific Islander | 458 (6.6) | 109 (9.0) | 349 (6.1) | |
| Latino/Hispanic | 1,158 (16.6) | 166 (13.7) | 992 (17.3) | |
| Other/Unknown | 389 (5.6) | 58 (4.8) | 331 (5.8) | |
| Deductible limit at baseline | <.001 | |||
| None | 4,801 (69.0) | 421 (34.8) | 4,380 (76.2) | |
| Low ($1 to $999) | 723 (10.4) | 337 (27.9) | 386 (6.7) | |
| High (≥$1,000) | 1,433 (20.6) | 451 (37.3) | 982 (17.1) | |
| Membership duration before SUD diagnosis | 0.110 | |||
| <6 months | 4,477 (64.4) | 802 (66.3) | 3,675 (63.9) | |
| ≥6 months | 2,480 (35.6) | 407 (33.7) | 2,073 (36.1) | |
| Type of SUD | ||||
| Alcohol | 4,065 (58.4) | 790 (65.3) | 3,275 (57.0) | <.001 |
| Cannabis | 2,049 (29.5) | 320 (26.5) | 1,729 (30.1) | 0.010 |
| Multi-drug | 248 (3.6) | 36 (3.0) | 212 (3.7) | 0.230 |
| Opioids | 1,067 (15.3) | 156 (12.9) | 911 (15.8) | 0.010 |
| Other drugs d | 1,388 (20.0) | 193 (16.0) | 1,195 (20.8) | <.001 |
| Stimulants e | 1,102 (15.8) | 146 (12.1) | 956 (16.6) | <.001 |
| Tobacco-related use disorder f | 2,638 (37.9) | 433 (35.8) | 2,205 (38.4) | 0.100 |
| Chronic medical comorbidity | 4,262 (61.3) | 796 (65.8) | 3,466 (60.3) | <.001 |
| Psychiatric comorbidity | 4,053 (58.3) | 696 (57.6) | 3,357 (58.4) | 0.590 |
| Anxiety disorders | 2,559 (36.8) | 436 (36.1) | 2,123 (36.9) | 0.570 |
| Bipolar spectrum | 944 (13.6) | 144 (11.9) | 800 (13.9) | 0.060 |
| Depressive disorders | 2,492 (35.8) | 451 (37.3) | 2,041 (35.5) | 0.240 |
| Schizophrenia or schizoaffective disorder | 180 (2.6) | 18 (1.5) | 162 (2.8) | 0.008 |
Abbreviations: ACA, Affordable Care Act.
Baseline is date of SUD diagnosis. We identified all diagnoses within the year after initial enrollment in 2014.
Percentages may not add up to 100% due to rounding error.
We assessed bivariate associations between patient characteristics and enrollment mechanisms with Chi-squared tests.
Other drugs include hallucinogens, inhalants, sedatives, hypnotics, anxiolytics, and unspecified.
Stimulants include amphetamines, methamphetamines, cocaine, and other psychostimulants.
We did not include tobacco-related use disorder in the inclusion criteria but could be comorbid.
3.2. Unadjusted trends in likelihood of utilization
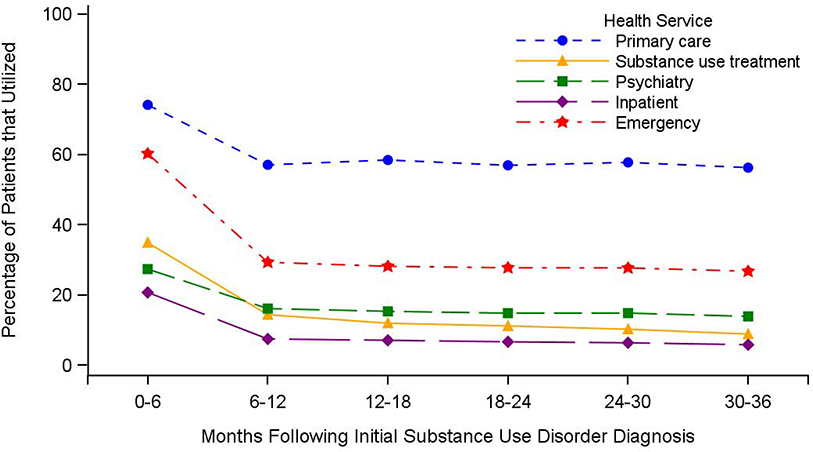
Utilization of any primary care, specialty SUD treatment, psychiatry, inpatient hospitalizations, and ED was highest in the 0–6 months after index and decreased in the subsequent (6–12 months) time window; utilization remained stable thereafter (Figure 1, Table S3). These trends did not vary by deductible limit (Figure S1) or type of SUD diagnosis (Figure S2).
Figure 1.
Unadjusted post-ACA trends in health service utilization over 36 months among newly enrolled Kaiser Permanente Northern California members with substance use disorders in 2014, (n=6,957).
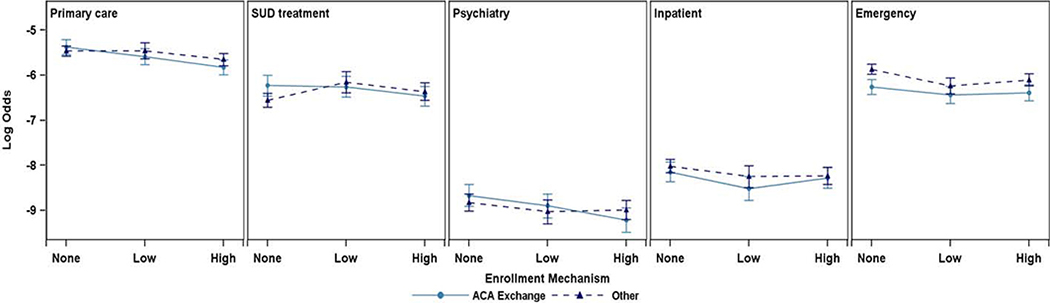
3.3. Adjusted relative likelihood of utilizing health services
Controlling for demographic characteristics, chronic medical conditions, and psychiatric comorbidities, there was evidence that the enrollment mechanism moderated the associations between deductible limits and the likelihood of utilizing primary care and psychiatry treatment from the multivariable models (Table 2; Figure 2). Among patients who enrolled via the ACA exchange, those with high deductibles were less likely than those without deductibles to utilize primary care (odds ratio [OR]=0.64, 95% confidence interval [CI]=0.54–0.77) and psychiatry treatment (OR=0.58, 95% CI=0.45–0.74). The corresponding ORs among patients who enrolled via other non-ACA mechanisms were 0.83 (95% CI=0.74–0.92) for primary care and 0.85 (95% CI=0.73–0.98) for psychiatry; these represent a significantly lower difference of 22% (ratio of odds ratios [ORR]=0.78, 95% CI=0.63–0.96) and 32% (ORR=0.68, 95% CI=0.51–0.91), respectively.
Table 2.
Multivariable analyses of utilization of outpatient health services in primary care, specialty SUD treatment, and psychiatry over 36 months among newly enrolled KPNC members with SUD.
| Primary care | Specialty SUD treatment | Psychiatry | ||||
|---|---|---|---|---|---|---|
| Characteristic | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value |
| Time window (reference: 0–6 months) | ||||||
| 6–12 months | 0.39 (0.35, 0.42) | <.001 | 0.29 (0.27, 0.32) | <.001 | 0.44 (0.41, 0.48) | <.001 |
| 12–18 months | 0.40 (0.36, 0.43) | <.001 | 0.23 (0.21, 0.26) | <.001 | 0.40 (0.37, 0.45) | <.001 |
| 18–24 months | 0.35 (0.32, 0.38) | <.001 | 0.21 (0.19, 0.23) | <.001 | 0.38 (0.34, 0.42) | <.001 |
| 24–30 months | 0.36 (0.32, 0.39) | <.001 | 0.19 (0.17, 0.22) | <.001 | 0.38 (0.34, 0.42) | <.001 |
| 30–36 months | 0.33 (0.29, 0.36) | <.001 | 0.16 (0.14, 0.18) | <.001 | 0.35 (0.31, 0.39) | <.001 |
| Gender (reference: Male) | 2.10 (1.94, 2.27) | <.001 | 0.75 (0.67, 0.84) | <.001 | 1.44 (1.30, 1.59) | <.001 |
| Age group at baseline (reference: 18–34 years) | ||||||
| 35–49 years | 1.13 (1.03, 1.23) | 0.009 | 1.40 (1.23, 1.60) | <.001 | 1.01 (0.90, 1.14) | 0.827 |
| 50–64 years | 1.42 (1.28, 1.58) | <.001 | 1.09 (0.94, 1.28) | 0.258 | 0.76 (0.66, 0.87) | <.001 |
| Race/ethnicity (reference: White) | ||||||
| Asian, Native Hawaiian, or Pacific Islander | 1.14 (1.01, 1.29) | 0.040 | 0.54 (0.45, 0.65) | <.001 | 0.73 (0.62, 0.85) | <.001 |
| Black | 1.07 (0.93, 1.24) | 0.324 | 0.51 (0.41, 0.64) | <.001 | 0.78 (0.62, 0.97) | 0.026 |
| Hispanic | 1.07 (0.97, 1.18) | 0.197 | 0.66 (0.56, 0.78) | <.001 | 0.82 (0.70, 0.96) | 0.015 |
| Other or Unknown | 0.62 (0.52, 0.73) | <.001 | 0.81 (0.63, 1.04) | 0.102 | 1.03 (0.81, 1.30) | 0.833 |
| ACA exchange (reference: other mechanism) | 1.09 (0.95, 1.25) | 0.238 | 1.39 (1.15, 1.68) | <.001 | 1.17 (0.98, 1.39) | 0.082 |
| Deductible limit (reference: none) | ||||||
| Low ($1 to $999) | 1.00 (0.86, 1.17) | 0.974 | 1.50 (1.22, 1.85) | <.001 | 0.81 (0.66, 1.00) | 0.052 |
| High (≥$1,000) | 0.83 (0.74, 0.92) | <.001 | 1.22 (1.04, 1.42) | 0.014 | 0.85 (0.73, 0.98) | 0.023 |
| Membership duration before SUD diagnosis (reference: <6 months) | 0.89 (0.83, 0.96) | 0.002 | 0.78 (0.69, 0.87) | <.001 | 1.00 (0.90, 1.11) | 0.949 |
| Comorbid chronic medical condition (reference: none) | 2.21 (2.04, 2.40) | <.001 | 0.62 (0.55, 0.70) | <.001 | 1.12 (1.00, 1.26) | 0.043 |
| Comorbid psychiatric disorder (reference: none) | 1.44 (1.34, 1.56) | <.001 | 2.13 (1.89, 2.40) | <.001 | 13.80 (11.70, 16.27) | <.001 |
| ACA exchange * Low deductible, ORR | 0.81 (0.63, 1.04) | 0.093 | 0.65 (0.47, 0.89) | 0.007 | 0.98 (0.71, 1.34) | 0.888 |
| Low vs no deductible, ACA exchange | 0.81 (0.67, 0.98) | 0.034 | 0.97 (0.77, 1.23) | 0.827 | 0.79 (0.62, 1.01) | 0.058 |
| Low vs no deductible, other mechanism | 1.00 (0.86, 1.17) | 0.974 | 1.50 (1.22, 1.85) | <.001 | 0.81 (0.66, 1.00) | 0.052 |
| ACA exchange * High deductible, ORR | 0.78 (0.63, 0.96) | 0.021 | 0.65 (0.49, 0.86) | 0.003 | 0.68 (0.51, 0.91) | 0.010 |
| High vs no deductible, ACA exchange | 0.64 (0.54, 0.77) | <.001 | 0.79 (0.62, 1.00) | 0.051 | 0.58 (0.45, 0.74) | <.001 |
| High vs no deductible, other mechanism | 0.83 (0.74, 0.92) | <.001 | 1.22 (1.04, 1.42) | 0.014 | 0.85 (0.73, 0.98) | 0.023 |
Abbreviations: ACA, Affordable Care Act; CI, confidence interval; KPNC, Kaiser Permanente Northern California; OR, odds ratio; ORR, ratio of odds ratios; SUD, substance use disorder.
Figure 2.
Log odds of utilizing health care services by deductible limit and enrollment mechanism, adjusted for demographic characteristics, chronic medical conditions and psychiatric comorbidities.
There was also evidence that the enrollment mechanism moderated the associations between deductibles and the likelihood of utilizing specialty SUD treatment after adjusting for all other patient characteristics in the multivariable models. Among patients who enrolled via the ACA exchange, there were no significant differences in the likelihood of utilizing specialty SUD treatment between patients with deductibles and those without; however, among patients who enrolled via other mechanisms, patients with high (OR=1.22, 95% CI=1.04–1.42) or low deductibles (OR=1.50, 95% CI=1.22–1.85) were more likely than those without deductibles to utilize specialty SUD treatment.
Compared to patients without a deductible, patients with high (OR=0.80, 95% CI=0.69–0.94) and low (OR=0.79, 95% CI=0.64–0.99) deductibles had lower odds of having a hospitalization (Table 3; Figure 2). Similarly, high and low deductibles were associated with lower odds of ED utilization. Patients enrolled via the ACA Exchange had significantly lower odds of visiting the ED (OR=0.67, 95% CI=0.59–0.77), but had similar odds of using inpatient services as patients who enrolled through other mechanisms (OR=0.88, 95% CI=0.73–1.06). The enrollment mechanism did not moderate the associations between deductible limits and the likelihood of having an inpatient hospitalization or ED visit, controlling for demographics and comorbidities.
Table 3.
Multivariable analyses of utilization of inpatient and emergency department health services over 36 months among newly enrolled KPNC members with SUD.
| Inpatient | Emergency department | |||
|---|---|---|---|---|
| Characteristic | OR (95% CI) | p-value | OR (95% CI) | p-value |
| Time window (reference: 0–6 months) | ||||
| 6–12 months | 0.29 (0.26, 0.33) | <.001 | 0.24 (0.22, 0.26) | <.001 |
| 12–18 months | 0.27 (0.24, 0.30) | <.001 | 0.22 (0.20, 0.24) | <.001 |
| 18–24 months | 0.25 (0.22, 0.28) | <.001 | 0.21 (0.20, 0.23) | <.001 |
| 24–30 months | 0.24 (0.21, 0.27) | <.001 | 0.22 (0.20, 0.24) | <.001 |
| 30–26 months | 0.22 (0.19, 0.25) | <.001 | 0.20 (0.19, 0.22) | <.001 |
| Gender (reference: Male) | 1.06 (0.96, 1.18) | 0.265 | 1.15 (1.06, 1.24) | <.001 |
| Age group at baseline (reference: 18–34 years) | ||||
| 35–49 years | 0.88 (0.78, 0.99) | 0.032 | 0.82 (0.75, 0.90) | <.001 |
| 50–64 years | 1.22 (1.08, 1.38) | 0.002 | 0.77 (0.69, 0.85) | <.001 |
| Race/ethnicity (reference: White) | ||||
| Asian, Native Hawaiian, or Pacific Islander | 1.26 (1.08, 1.46) | 0.002 | 1.88 (1.67, 2.11) | <.001 |
| Black | 1.10 (0.89, 1.36) | 0.369 | 0.84 (0.73, 0.98) | 0.030 |
| Hispanic | 1.04 (0.90, 1.19) | 0.615 | 1.18 (1.06, 1.31) | 0.002 |
| Other or Unknown | 0.84 (0.66, 1.07) | 0.160 | 1.07 (0.89, 1.28) | 0.459 |
| ACA exchange (reference: other mechanism) | 0.88 (0.73, 1.06) | 0.182 | 0.67 (0.59, 0.77) | <.001 |
| Deductible limit (reference: none) | ||||
| Low ($1 to $999) | 0.79 (0.64, 0.99) | 0.038 | 0.69 (0.59, 0.80) | <.001 |
| High (≥$1,000) | 0.80 (0.69, 0.94) | 0.006 | 0.79 (0.71, 0.88) | <.001 |
| Membership duration before SUD diagnosis (reference: <6 months) | 0.91 (0.82, 1.01) | 0.086 | 1.00 (0.93, 1.08) | 0.956 |
| Comorbid chronic medical condition (reference: none) | 2.26 (2.00, 2.54) | <.001 | 1.97 (1.81, 2.15) | <.001 |
| Comorbid psychiatric disorder (reference: none) | 1.60 (1.43, 1.78) | <.001 | 1.40 (1.29, 1.52) | <.001 |
| ACA exchange * Low deductible, ORR | 0.87 (0.61, 1.24) | 0.438 | 1.21 (0.95, 1.55) | 0.123 |
| Low vs no deductible, ACA exchange | 0.69 (0.52, 0.91) | 0.009 | 0.84 (0.69, 1.02) | 0.078 |
| Low vs no deductible, other mechanism | 0.79 (0.64, 0.99) | 0.038 | 0.69 (0.59, 0.80) | <.001 |
| ACA exchange * High deductible, ORR | 1.09 (0.81, 1.47) | 0.555 | 1.12 (0.90, 1.40) | 0.315 |
| High vs no deductible, ACA exchange | 0.88 (0.68, 1.13) | 0.312 | 0.89 (0.73, 1.07) | 0.214 |
| High vs no deductible, other mechanism | 0.80 (0.69, 0.94) | 0.001 | 0.79 (0.71, 0.88) | <.001 |
Abbreviations: ACA, Affordable Care Act; CI, confidence interval; KPNC, Kaiser Permanente Northern California; OR, odds ratio; ORR, ratio of odds ratios; SUD, substance use disorder.
Patients with a longer membership duration before receiving an SUD diagnosis (≥6 months) were less likely to utilize primary care (OR=0.89, 95% CI=0.83–0.96) and specialty SUD treatment (OR=0.78, 95% CI=0.69–0.87) than those with a shorter duration (<6 months); there were no differences for psychiatry treatment, inpatient hospitalizations, or ED visits (Tables 2–3).
Patients with a comorbid psychiatric disorder had significantly higher odds of using all health services studied, controlling for all other characteristics. Specifically, they had 1.4 to 2.1 times the odds of using primary care, specialty SUD, inpatient, and ED services; and 14 times the odds of using psychiatry treatment (Tables 2–3). Patients with a chronic medical comorbidity had significantly higher odds of utilizing all health services, except for specialty SUD treatment, which they were less likely to utilize (Tables 2–3).
Controlling for all other characteristics, nonwhite patients had lower odds of initiating specialty SUD and psychiatry treatment (Table 2). Asian, Native Hawaiian, or Pacific Islander patients had higher odds of utilizing inpatient and ED services compared to white patients (Table 3). Hispanic patients were also more likely to utilize ED services, but Black patients were less likely, compared to white patients. Compared to younger patients (18–34 years), older patients (50–64 years) had higher odds of utilizing primary care and inpatient services, but lower odds of utilizing psychiatry and ED services (Tables 2–3). Patients aged 35–49 years had higher odds of utilizing primary care and specialty SUD services, but lower odds of utilizing inpatient and ED services, compared to patients aged 18–34 years (Tables 2–3).
3.5. Sensitivity analysis
Since the most noticeable change in utilization occurred in the 6–12 month period, we conducted sensitivity analyses comparing patients who remained in the cohort at 6–12 months (noncensored, n=5,976), to patients who were censored due to disenrollment during that time (n=981). The censored group used less primary care (59% vs. 77%, p<.001) and psychiatry services (20% vs. 29%, p<.001) in the first 6 months but were slightly more likely to visit the ED (64% vs. 60%, p=0.009; Table S6). There was no difference between the censored and the noncensored group in specialty SUD and inpatient utilization. The censored group had a larger proportion of patients with high deductibles (28% vs. 19%, p<.001) and a smaller proportion of patients who enrolled via the ACA exchange (13% vs 18%, p<.001) compared to the noncensored group (Table S6).
4. Discussion
This study examined longitudinal patterns of healthcare utilization among SUD patients and their relationships to key aspects of ACA benefit plans, including enrollment mechanisms and deductible levels. We anticipated that the increase in coverage opportunities that the ACA provided would bring high-utilizing patients into health systems, driving up overall use of healthcare. Consistent with prior studies of SUD treatment samples that have found elevated levels of healthcare utilization either immediately before or after starting SUD treatment (Holder, 1998; Parthasarathy et al., 2001; Wickizer, Krupski, Stark, Mancuso, & Campbell, 2006), results of our longitudinal analysis showed that utilization among people with SUDs was highest immediately after initial SUD diagnosis at KPNC, and declined to a stable level in subsequent years. This suggests that the initial high utilization may be temporary. Our sensitivity analysis suggested that this result was not due to high utilizers leaving the KPNC healthcare system. This overall trend in utilization is a welcome finding, and consistent with the intent of the ACA to increase access to care; however, the subsequent decrease in utilization could also signify that patients are disengaging from treatment.
Although we cannot specifically attribute the initial levels of utilization to lack of prior insurance coverage, as we did not have data on prior coverage, we found that individuals with fewer than 6 months of membership before receiving an SUD diagnosis were more likely to utilize primary care and specialty SUD treatment than those who had 6–12 months of membership. This suggests that future healthcare reforms that expand insurance coverage for people with SUDs might also lead to short-term increases in utilization for a range of health services.
Deductibles are a key area of health policy interest given the growing number of people enrolling in deductible plans post-ACA. As anticipated, higher deductibles had a generally negative association with utilizing healthcare in this population. We found that patients with high deductibles (≥$1,000) had lower odds of using primary care, psychiatry, inpatient, and ED services than those without deductibles. Additionally, we found the associations between high deductibles and likelihood of utilizing primary care and psychiatry were strongly negative among ACA Exchange enrollees. Although it is somewhat difficult to gauge the clinical significance of these specific results, the strength of the odds ratios for primary care and psychiatry access gives some indication of the potential impact. The associations of high deductibles with primary care and psychiatry access is worrying given the extent of medical and psychiatric comorbidities among people with SUDs (Mertens, Flisher, Satre, & Weisner, 2008). Although we found more consistent associations for higher deductibles and less healthcare initiation, it is possible that even a modest deductible could deter patients from seeking treatment (Brot-Goldberg, Chandra, Handel, & Kolstad, 2017; Reed et al., 2009). From a public policy and health system perspective, the possibility that deductibles could prevent people with SUDs from accessing any needed medical care is a cause for concern.
Consistent with prior findings (Agarwal, Mazurenko, & Menachemi, 2017), our results suggest that high deductibles have the potential to dissuade SUD patients from accessing needed health services, and that those who enroll via the ACA exchange may be more sensitive to them. This could be attributable to greater awareness of coverage terms due to the mandate that exchange websites offer clear, plain-language explanations to compare insurance options (HealthCare.gov, 2020). In contrast, high deductibles were associated with a greater relative likelihood of SUD treatment utilization. However, this association existed only among patients who enrolled via mechanisms other than the ACA Exchange. It is possible that individuals with emerging or unrecognized substance use problems may have selected higher deductible plans at enrollment due to either not anticipating use of SUD treatment, which is often more price-sensitive relative to other medical care (Hodgkin, Horgan, Garnick, & Merrick, 2003; Parthasarathy & Campbell, 2016; Swartz, 2010), or not being aware of the implications of deductibles. However, once engaged in treatment, individuals with high deductibles may have been motivated to remain there. A contributing factor could also be that such patients were required to remain in treatment either by employer or court mandates, which are common and are associated with retention (Weisner et al., 2009). The varying associations between deductibles and different types of health service utilization by enrollment mechanisms highlight the need for future research in this area.
Insurance exchanges provide access to tax credits, a broader range of coverage levels, and information to assist in healthcare planning that might be less easily accessible through other sources of coverage, e.g., through employers (HealthCare.gov, 2019). In our sample, Exchange enrollment was associated with greater likelihood of remaining a member of KPNC, did not demonstrate an adverse association with routine care, and was associated with lower ED use. However, primary care and psychiatric services use were similar across enrollment types, even within low and high deductible limits. Prior studies have found that health plans offered through the ACA Exchange are more likely to have narrow behavioral health networks compared to other non-Exchange plans (Stewart et al., 2018) and primary care networks (Zhu, Zhang, & Polsky, 2017), which raises concerns about treatment access. For this health system, that concern appears unfounded.
Psychiatric comorbidity was associated with greater service use of all types. Several prior studies have also found that patients with psychiatric comorbidity use more health services than those with SUD alone (Curran et al., 2008; Graham et al., 2017; Painter et al., 2018). Similar to our results, a recent study based in California found that after controlling for patient-level characteristics, the strongest predictors of frequent ED use post-ACA included having a diagnosis of a psychiatric disorder or an SUD (McConville, Raven, Sabbagh, & Hsia, 2018). While the ACA was not expected to alter this general pattern, the inclusion of mental health treatment as an essential benefit was intended to improve availability of care and to contribute to efforts to reduce unnecessary service utilization. Our investigation confirms the ongoing importance post-ACA of psychiatric comorbidity and suggests that future efforts in behavioral health reform must anticipate high demand for healthcare in this vulnerable clinical population.
It is also worth noting that nonwhite patients were less likely to initiate SUD and psychiatry treatment. Race/ethnic disparities in access to care are a longstanding concern in the addiction field (U.S. Department of Health and Human Services & Office of the Surgeon General, 2016). Some expected these disparities to be mitigated post-ACA (Guerrero et al., 2017). Findings on race/ethnic differences are similar to what has been observed in other health systems (McGuire & Miranda, 2008; Saloner & Le Cook, 2013); although, few studies have examined associations post-ACA. One prior study among young adults with SUD and psychiatric conditions post-ACA found modest ethnic disparities in lack of coverage (5–19% differences in coverage) between whites and other ethnic groups (Novak, Williams-Parry, & Chen, 2017); although, another study of young people more broadly found larger gains in coverage among Hispanics and Blacks relative to whites (Lipton, Decker, & Sommers, 2019). The race/ethnic disparities in SUD and psychiatry treatment initiation in this cohort, in which overall insurance coverage was not a barrier but specific mechanisms could be, highlight the importance of addressing this complicated challenge to health equity.
4.1. Study strengths and limitations
This study used a large SUD patient cohort enrolled in health coverage post-ACA and included comprehensive data on diagnoses, insurance coverage, and use of care over three years. KPNC data are well-suited to examine ACA-related changes in health service utilization given the size and diversity of its membership. KPNC’s integrated model is becoming more common as other health plans and federally qualified health centers move toward providing integrated SUD treatment services and using EHRs (Pourat et al., 2012). However, we should note that is an observational study based on EHR data. As such, we cannot attribute causal relationships to our findings. However, we have conducted sensitivity analyses to examine the robustness of our findings in the absence of a randomized clinical trial. These analyses supported our initial findings; e.g., indicating that service use decrease over time was not due to high utilizers leaving KPNC. Medicaid expansion has the potential to improve access to SUD treatment (Andrews et al., 2019), but we were also not able to examine its relationship to services in the current analysis due to collinearity with deductible limits (Medicaid patients in our cohort did not have a deductible). Our study was set in a single nonprofit healthcare delivery system in Northern California, which enabled us to characterize post-ACA patterns of service utilization in depth but did not allow us to compare populations or implementation across systems (e.g., public vs. private). Nevertheless, our findings can inform future work on health reform and policy efforts to improve access to healthcare for similar clinically complex patients in other health systems.
4.2. Conclusion
The ACA provided a critical opportunity to expand access to SUD treatment as well as other important health services for people with SUDs, yet research as rarely examined implementation and subsequent use of care. This study found that in newly enrolled patients with SUDs, health service utilization peaked in the 6 months following an SUD diagnosis and then decreased to a stable level in years 2–3. Among patients with SUDs, deductible limits were generally associated with less health service utilization, which was more pronounced among Exchange enrollees, while psychiatric comorbidity was associated with more use of services. As modifications to the ACA are considered, it is critical to continue investigating the consequences of health reform policies for people with SUDs, including race/ethnic minorities and those with psychiatric comorbidity.
Supplementary Material
Highlights.
Utilization was highest in the first 6 months, then decreased and remained stable.
Higher deductibles were generally associated with use of fewer health services, especially in combination with enrollment through the Exchange.
Psychiatric comorbidity was associated with greater use of all services.
Non-whites were less likely to access substance use treatment and psychiatry.
Acknowledgements
We thank Alison Truman for assistance in project management and Agatha Hinman for assistance in preparing the manuscript.
Sources of Support
The National Institute on Drug Abuse (R21/R33 DA035645) and the Tobacco-Related Disease Research Program (24XT-0008) supported this study. Dr. Satre was also supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (K24 AA025703).
Footnotes
Author statement:
The authors declare no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abraham AJ, Andrews CM, Grogan CM, D’Aunno T, Humphreys KN, Pollack HA, et al. (2017). The Affordable Care Act transformation of substance use disorder treatment. American Journal of Public Health, 107(1), 31–32. 10.2105/ajph.2016.303558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agarwal R, Mazurenko O, & Menachemi N (2017). High-deductible health plans reduce health care cost and utilization, including use of needed preventive services. Health Affairs (Millwood), 36(10), 1762–1768. 10.1377/hlthaff.2017.0610. [DOI] [PubMed] [Google Scholar]
- Andersen RM (1995). Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior, 36(1), 1–10. 10.2307/2137284 [DOI] [PubMed] [Google Scholar]
- Andrews CM, Abraham AJ, Grogan CM, Westlake MA, Pollack HA, & Friedmann PD (2019). Impact of Medicaid restrictions on availability of buprenorphine in addiction treatment programs. American Journal of Public Health, 109(3), 434–436. 10.2105/AJPH.2018.304856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews CM, Grogan CM, Smith BT, Abraham AJ, Pollack HA, Humphreys K, et al. (2018). Medicaid benefits for addiction treatment expanded after implementation of the Affordable Care Act. Health Affairs (Millwood), 37(8), 1216–1222. 10.1377/hlthaff.2018.0272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brot-Goldberg ZC, Chandra A, Handel BR, & Kolstad JT (2017). What does a deductible do? The impact of cost-sharing on health care prices, quantities, and spending dynamics The Quarterly Journal of Economics, 132(3), 1261–1318. 10.1093/qje/qjx013. [DOI] [Google Scholar]
- Buck JA (2011). The looming expansion and transformation of public substance abuse treatment under the Affordable Care Act. Health Affairs (Millwood), 30(8), 1402–1410. 10.1377/hlthaff.2011.0480. [DOI] [PubMed] [Google Scholar]
- Campbell CI, Parthasarathy S, Altschuler A, Young-Wolff KC, & Satre DD (2018). Characteristics of patients with substance use disorder before and after the Affordable Care Act. Drug and Alcohol Dependence, 193, 124–130. 10.1016/j.drugalcdep.2018.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowell AJ, Prakash S, Jones E, Barnosky A, & Wedehase B (2018). Behavioral health coverage in the individual market increased after ACA parity requirements. Health Affairs (Millwood), 37(7), 1153–1159. 10.1377/hlthaff.2017.1517. [DOI] [PubMed] [Google Scholar]
- Curran GM, Sullivan G, Williams K, Han X, Allee E, & Kotrla KJ (2008). The association of psychiatric comorbidity and use of the emergency department among persons with substance use disorders: an observational cohort study. BMC Emergency Medicine, 8, 17 10.1186/1471-227X-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhingra SS, Zack M, Strine T, Pearson WS, & Balluz L (2010). Determining prevalence and correlates of psychiatric treatment with Andersen’s behavioral model of health services use. Psychiatric Services, 61(5), 524–528. 10.1176/appi.ps.61.5.524. [DOI] [PubMed] [Google Scholar]
- Disability Rights California. (2014). What is mental health parity? California Mental Health Service Authority. https://sd15.senate.ca.gov/sites/sd15.senate.ca.gov/files/DRA%20%20mental%20health%20parity%20-%20final.pdf Accessed December 11, 2019. [Google Scholar]
- Druss BG, & Mauer BJ (2010). Health care reform and care at the behavioral health--primary care interface. Psychiatric Services, 61(11), 1087–1092. 10.1176/ps.2010.61.11.1087. [DOI] [PubMed] [Google Scholar]
- Feder KA, Mojtabai R, Krawczyk N, Young AS, Kealhofer M, Tormohlen KN, et al. (2017). Trends in insurance coverage and treatment among persons with opioid use disorders following the Affordable Care Act. Drug and Alcohol Dependence, 179, 271–274. 10.1016/j.drugalcdep.2017.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galbraith AA, Ross-Degnan D, Soumerai SB, Rosenthal MB, Gay C, & Lieu TA (2011). Nearly half of families in high-deductible health plans whose members have chronic conditions face substantial financial burden. Health Affairs (Millwood), 30(2), 322–331. 10.1377/hlthaff.2010.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon NP (2015). Similarity of the adult Kaiser Permanente membership in Northern California to the insured and general population in Northern California: statistics from the 2011–2012 California Health Interview Survey Kaiser Permanente Division of Research, Oakland CA: https://divisionofresearch.kaiserpermanente.org/projects/memberhealthsurvey/SiteCollectionDocuments/chis_non_kp_2011.pdf Accessed March 24, 2020. [Google Scholar]
- Graham K, Cheng J, Bernards S, Wells S, Rehm J, & Kurdyak P (2017). How much do mental health and substance use/addiction affect use of general medical services? Extent of use, reason for use, and associated costs. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 62(1), 48–56. 10.1177/0706743716664884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero EG, Garner BR, Cook B, Kong Y, Vega WA, & Gelberg L (2017). Identifying and reducing disparities in successful addiction treatment completion: Testing the role of Medicaid payment acceptance. Substance Abuse and Treatment, Prevention, Policy, 12(1), 27 10.1186/s13011-017-0113-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulley SP, Rasch EK, & Chan L (2011). The complex web of health: relationships among chronic conditions, disability, and health services. Public Health Reports, 126(4), 495–507. 10.1177/003335491112600406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HealthCare.gov (2019). What marketplace health insurance plans cover. Centers for Medicare and Medicaid Services. https://www.healthcare.gov/coverage/what-marketplace-plans-cover/ Accessed April 23, 2020.
- HealthCare.gov (2020). Mental health & substance abuse coverage. U.S. Centers for Medicare & Medicaid Services. https://www.healthcare.gov/coverage/mental-health-substance-abuse-coverage/ Accessed April 23, 2020.
- Hodgkin D, Horgan CM, Garnick DW, & Merrick EL (2003). Cost sharing for substance abuse and mental health services in managed care plans. Medical Care Research and Review, 60(1), 101–116. 10.1177/1077558702250248. [DOI] [PubMed] [Google Scholar]
- Holder HD (1998). Cost benefits of substance abuse treatment: an overview of results from alcohol and drug abuse. Journal of Mental Health Policy and Economics, 1(1), 23–29. . [DOI] [PubMed] [Google Scholar]
- Humphreys K, & Frank RG (2014). The Affordable Care Act will revolutionize care for substance use disorders in the United States. Addiction, 109(12), 1957–1958. 10.1111/add.12606. [DOI] [PubMed] [Google Scholar]
- Lake J, & Turner MS (2017). Urgent need for improved mental health care and a more collaborative model of care. Permanente Journal, 21(7), 492–493. 10.7812/TPP/17-024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang K-Y, & Zeger SL (1986). Longitudinal data analysis using generalized linear models. Biometrika, 73(1), 13–22. 10.1093/biomet/73.1.13. [DOI] [Google Scholar]
- Lipton BJ, Decker SL, & Sommers BD (2019). The Affordable Care Act appears to have narrowed racial and ethnic disparities in insurance coverage and access to care among young adults. Medical Care Research and Review, 76(1), 32–55. 10.1177/1077558717706575. [DOI] [PubMed] [Google Scholar]
- Lo Sasso AT, & Lyons JS (2002). The effects of copayments on substance abuse treatment expenditures and treatment reoccurrence. Psychiatric Services, 53(12), 1605–1611. 10.1176/appi.ps.53.12.1605. [DOI] [PubMed] [Google Scholar]
- Lo Sasso AT, & Lyons JS (2004). The sensitivity of substance abuse treatment intensity to co-payment levels. Journal of Behavioral Health Services and Research, 31(1), 50–65. 10.1007/BF02287338. [DOI] [PubMed] [Google Scholar]
- Maclean JC, & Saloner B (2019). The effect of public insurance expansions on substance use disorder treatment: Evidence from the Affordable Care Act. Journal of Policy Analysis and Management, 38(2), 366–393. 10.1002/pam.22112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConville S, Raven MC, Sabbagh SH, & Hsia RY (2018). Frequent Emergency Department users: A statewide comparison before and after Affordable Care Act implementation. Health Affairs (Millwood), 37(6), 881–889. 10.1377/hlthaff.2017.0784. [DOI] [PubMed] [Google Scholar]
- McGuire TG, & Miranda J (2008). New evidence regarding racial and ethnic disparities in mental health: policy implications. Health Affairs (Millwood), 27(2), 393–403. 10.1377/hlthaff.27.2.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens JR, Flisher AJ, Satre DD, & Weisner CM (2008). The role of medical conditions and primary care services in 5-year substance use outcomes among chemical dependency treatment patients. Drug and Alcohol Dependence, 98(1–2), 45–53. 10.1016/j.drugalcdep.2008.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens JR, Lu YW, Parthasarathy S, Moore C, & Weisner CM (2003). Medical and psychiatric conditions of alcohol and drug treatment patients in an HMO: Comparison with matched controls. Archives of Internal Medicine, 163(20), 2511–2517. 10.1001/archinte.163.20.2511. [DOI] [PubMed] [Google Scholar]
- Mertens JR, & Weisner CM (2000). Predictors of substance abuse treatment retention among women and men in an HMO. Alcoholism: Clinical and Experimental Research, 24(10), 1525–1533. 10.1111/j.1530-0277.2000.tb04571.x. [DOI] [PubMed] [Google Scholar]
- Molfenter T, Capoccia VA, Boyle MG, & Sherbeck CK (2012). The readiness of addiction treatment agencies for health care reform. Substance Abuse and Treatment, Prevention, Policy, 7(1), 16 10.1186/1747-597X-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak P, Anderson AC, & Chen J (2018). Changes in health insurance coverage and barriers to health care access among individuals with serious psychological distress following the Affordable Care Act. Administration and Policy in Mental Health, 45(6), 924–932. 10.1007/s10488-018-0875-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak P, Williams-Parry KF, & Chen J (2017). Racial and ethnic disparities among the remaining uninsured young adults with behavioral health disorders after the ACA expansion of dependent coverage. Journal of Racial and Ethnic Health Disparities, 4(4), 607–614. 10.1007/s40615-016-0264-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornstein SM, Nietert PJ, Jenkins RG, & Litvin CB (2013). The prevalence of chronic diseases and multimorbidity in primary care practice: a PPRNet report. Journal of the American Board of Family Medicine, 26(5), 518–524. 10.3122/jabfm.2013.05.130012. [DOI] [PubMed] [Google Scholar]
- Painter JM, Malte CA, Rubinsky AD, Campellone TR, Gilmore AK, Baer JS, et al. (2018). High inpatient utilization among Veterans Health Administration patients with substance-use disorders and co-occurring mental health conditions. American Journal of Drug and Alcohol Abuse, 44(3), 386–394. 10.1080/00952990.2017.1381701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parthasarathy S, & Campbell CI (2016). High-deductible health plans: Implications for substance use treatment. Health Services Research, 51(5), 1939–1959. 10.1111/1475-6773.12456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parthasarathy S, Weisner C, Hu TW, & Moore C (2001). Association of outpatient alcohol and drug treatment with health care utilization and cost: Revisiting the offset hypothesis. Journal of Studies on Alcohol, 62(1), 89–97. 10.15288/jsa.2001.62.89. [DOI] [PubMed] [Google Scholar]
- Pourat N, Davis AC, Salce E, Hilberman D, Roby DH, & Kominski GF (2012). In ten California counties, notable progress in system integration within the safety net, although challenges remain. Health Affairs (Millwood), 31(8), 1717–1727. 10.1377/hlthaff.2012.0545. [DOI] [PubMed] [Google Scholar]
- Reed M, Fung V, Price M, Brand R, Benedetti N, Derose SF, et al. (2009). High-deductible health insurance plans: Efforts to sharpen a blunt instrument. Health Affairs (Millwood), 28(4), 1145–1154. 10.1377/hlthaff.28.4.1145. [DOI] [PubMed] [Google Scholar]
- Saloner B, Bandara S, Bachhuber M, & Barry CL (2017). Insurance coverage and treatment use under the Affordable Care Act among adults with mental and substance use disorders. Psychiatric Services, 68(6), 542–548. 10.1176/appi.ps.201600182. [DOI] [PubMed] [Google Scholar]
- Saloner B, & Le Cook B (2013). Blacks and Hispanics are less likely than whites to complete addiction treatment, largely due to socioeconomic factors. Health Affairs (Millwood), 32(1), 135–145. 10.1377/hlthaff.2011.0983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre DD, Campbell CI, Gordon NS, & Weisner C (2010). Ethnic disparities in accessing treatment for depression and substance use disorders in an integrated health plan. International Journal of Psychiatry in Medicine, 40(1), 57–76. 10.2190/PM.40.1.e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre DD, Mertens JR, Arean PA, & Weisner C (2004). Five-year alcohol and drug treatment outcomes of older adults versus middle-aged and younger adults in a managed care program. Addiction, 99(10), 1286–1297. 10.1111/j.1360-0443.2004.00831.x. [DOI] [PubMed] [Google Scholar]
- Selby JV, Smith DH, Johnson ES, Raebel MA, Friedman GD, & McFarland BH (2005). Kaiser Permanente Medical Care Program In Strom BL (Ed.), Pharmacoepidemiology (pp. 241–259). New York: Wiley [Google Scholar]
- Shover CL, Abraham A, D’Aunno T, Friedmann PD, & Humphreys K (2019). The relationship of Medicaid expansion to psychiatric comorbidity care within substance use disorder treatment programs. Journal of Substance Abuse Treatment, 105, 44–50. 10.1016/j.jsat.2019.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein B, Orlando M, & Sturm R (2000). The effect of copayments on drug and alcohol treatment following inpatient detoxification under managed care. Psychiatric Services, 51(2), 195–198. 10.1176/appi.ps.51.2.195. [DOI] [PubMed] [Google Scholar]
- Stewart MT, Horgan CM, Hodgkin D, Creedon TB, Quinn A, Garito L, et al. (2018). Behavioral health coverage under the Affordable Care Act: What can we learn from marketplace products? Psychiatric Services, 69(3), 315–321. 10.1176/appi.ps.201700098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz K (2010). Cost-sharing: effects on spending and outcomes. The Synthesis project. Research synthesis report (20), 71583. [PubMed] [Google Scholar]
- Tai B, & Volkow ND (2013). Treatment for substance use disorder: opportunities and challenges under the affordable care act. Social Work in Public Health, 28(3–4), 165–174. 10.1080/19371918.2013.758975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terhune C (2013). Report: Kaiser tops state health insurance market with 40% share. Los Angeles Times. http://articles.latimes.com/2013/jan/29/business/la-fi-mo-health-insure-market-20130129 Accessed June 9, 2020. [Google Scholar]
- Thomas KC, Shartzer A, Kurth NK, & Hall JP (2018). Impact of ACA health reforms for people with mental health conditions. Psychiatric Services, 69(2), 231–234. 10.1176/appi.ps.201700044. [DOI] [PubMed] [Google Scholar]
- U.S. Congress. (2010). Patient Protection and Affordable Care Act, 42 U.S.C. § 18001. Public Law 111–148. https://www.gpo.gov/fdsys/pkg/PLAW-111publ148/html/PLAW-111publ148.htm Accessed April 23, 2020.
- U.S. Department of Health and Human Services, & Office of the Surgeon General. (2016). Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, DC: U.S. Department of Health & Human Services. [PubMed] [Google Scholar]
- Weisner C, Lu Y, Hinman A, Monahan J, Bonnie RJ, Moore CD, et al. (2009). Substance use, symptom, and employment outcomes of persons with a workplace mandate for chemical dependency treatment. Psychiatric Services, 60(5), 646–654. 10.1176/appi.ps.60.5.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisner C, Matzger H, Tam T, & Schmidt L (2002). Who goes to alcohol and drug treatment? Understanding utilization within the context of insurance. Journal of Studies on Alcohol and Drugs, 63(6), 673–682. 040401/djb;rev.081402/djb. [DOI] [PubMed] [Google Scholar]
- Wickizer TM, Krupski A, Stark KD, Mancuso D, & Campbell K (2006). The effect of substance abuse treatment on Medicaid expenditures among general assistance welfare clients in Washington state. Milbank Q, 84(3), 555–576. 10.1111/j.1468-0009.2006.00458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu JM, Zhang Y, & Polsky D (2017). Networks in ACA marketplaces are narrower for mental health care than for primary care. Health Affairs (Millwood), 36(9), 1624–1631. 10.1377/hlthaff.2017.0325. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.