Highlights
-
•
Colonic lipomatosis may present with acute abdominal complications.
-
•
Acute appendicitis is a rare manifestation of colonic lipomatosis.
-
•
Surgery is the preferred treatment approach for acute complications of colonic lipomatosis.
-
•
No patient or author details are included in the figures submitted with the abstract.
Keywords: Colonic, Lipomatosis, Case report, Appendicitis
Abstract
Introduction
Colonic lipomatosis is defined as a poorly circumscribed, non-capsulated fat accumulation in the submucosal layer of the colonic wall. Clinical presentation varies from asymptomatic to acute surgical complications.
Presentation of case
We report the case of a 79-year old male who arrived at the Emergency Department complaining of worsening abdominal pain, fever and nausea. A CT scan revealed a periappendicular abscess extended to the ileocecal valve and also the presence of diffuse intramural fatty tissue of the ascending colon. The patient underwent surgery and a right hemicolectomy was performed. The final histological exam confirmed the diagnosis of gangrenous appendicitis with diffuse abscessualization of the ileocecal valve and the presence of submucosal lipomatosis of the ICV extending to the ascending colon. Patient was discharged at 11th-POD.
Discussion
Acute appendicitis can represent a complication, although rare, of colonic lipomatosis. The underlying mechanism can be explained by the obstruction of the stool discharge from the appendix caused by the thickened colonic wall due to lipomatosis. Despite the lack of established guidelines on the management of colonic lipomatosis, surgery remains the preferred treatment in case of acute complications.
Conclusion
Acute appendicitis is a rare clinical manifestation of colonic lipomatosis. As in the case of other acute complications, such as intussesception, surgery remains the preferred therapeutic approach.
1. Introduction
This case report is in line with the SCARE guidelines for surgical case reports [1].
Colonic lipomatosis is defined as a poorly circumscribed, non-capsulated fat accumulation in the submucosal layer of the colonic wall and represents a rare condition with a reported prevalence of 0.2% [2]. It is generally first discovered between 50 and 65 years of age and has a predominance for women. The most frequently involved localizations are the ileocecal valve (ICV) and the ascending colon [3].
Clinical manifestations of colonic lipomatosis are usually mild and not specific such as abdominal pain, constipation, diarrhea or bleeding, but it may also lead to acute complications including intestinal intussusception or massive bleeding [[4], [5], [6]]. The first diagnosis is often occasional after an endoscopic procedure or CT scan. Currently there are not any established guidelines for the management of colonic lipomatosis, however in case of remittent symptoms or acute complications surgery remains the most accepted approach.
2. Presentation of case
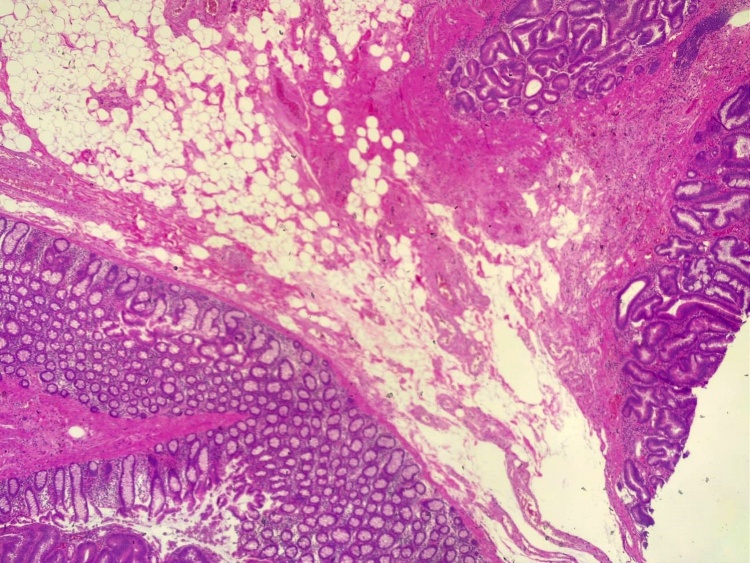
We report the case of a 79-year-old male who came to the Emergency Department of our hospital complaining of worsening abdominal pain in the last 24 h, nausea and fever. His clinical history was positive for arterial hypertension, benign prostatic hypertrophy and an abdominal aortic aneurism (AAA) managed conservatively. At admission he had a blood pressure of 110/55 mm/Hg, heart rate of 94 bpm and 98% oxygen saturation. The clinical examination evidenced a diffuse abdominal pain with relevant parietal tenderness in the lateral quadrants, compatible with acute peritonitis. Laboratory findings showed a WBC of 6.040/mm3 (80% neutrophils) and Reactive C Protein set at 98.2 mg/dL. In consideration of his clinical history an abdominal angio-TC was immediately performed. It excluded an acute complication of the AAA and evidenced an enlarged cecal appendix occupied by dishomogeneous material indicating acute appendicitis. In addition, it also pointed out the presence of amorphous hypodense material of ICV and ascending colon compatible with colonic lipomatosis (Fig. 1). After clinical and radiological examination, the patient was immediately taken to the operating theatre for surgery. A median laparotomy was performed evidencing diffused abdominal peritonitis due to gangrenous perforated appendicitis with relevant involvement of the ICV extended to the ascending colon. Surgery consisted of a right hemicolectomy (Fig. 2) with a side-to-side isoperistaltic ileo-colic hand-sewn anastomosis. The post-operative period was fairly regular, complicated only by an upper respiratory tract infection treated with antibiotics. The patient was discharged in the 11-POD and at the last clinical follow-up performed one month after surgery did not show any surgical complication. The histological examination confirmed the diagnosis of gangrenous appendicitis with diffuse abscessualization of the ileocecal valve and the presence of submucosal lipomatosis of the ICV extending to the ascending colon. In addition, it evidenced the presence of a tubulovillous adenoma with high grade dysplasia of the ascendant colon that was radically excised (Fig. 3).
Fig. 1.
CT scan showing periappendicular abscess.
Fig. 2.
Surgical specimen.
Fig. 3.
Histological image.
3. Discussion
Colonic lipomatosis is a rare condition with a reported prevalence of around 0.2% in a large autopsy series. It is defined as diffuse, non-capsulated fat accumulation in the submucosal layer and must be distinguished from intestinal lipomas, which are encapsulated, and lipohyperplasia, which implies an excess of normal adipose tissue in the submucosa. The etiology of lipomatosis is still unclear. It has been associated with an embryonic displacement of adipose tissue or with chronic irritation of the bowel. In a descending order they are more frequent in the caecum, ascending, sigmoid, transverse, rectum and descending colon.
The clinical manifestations are usually not specific and characterized by abdominal pain, constipation, diarrhea or bleeding. In some cases it may lead to complications such as intestinal intussesception or massive bleeding. We have reported an usual presentation of colonic lipomatosis with acute appendicitis, which has been described in only a few cases in literature [7]. Such association could be explained by the mechanical obstruction of the stool discharge from the appendix caused by the lipomatosis leading to the formation of appendicolite that increase the frequency of appendicitis. In a recent study, Börekci et al. showed a significant association between the thickness of lipomatosis and frequency of acute appendicitis [8].
The diagnosis is usually made after an endoscopic procedure or CT scan. On CT imaging it is often described as intramural hypoattenuating area with attenuation values between -80 and -120 HU [9].
Due to the rarity of the condition, at the moment there are no established guidelines on the management of colonic lipomatosis. Endoscopic approach can be considered in case of lipomas of ICV up to 2–2.5 cm, due the high risk of perforation and haemorrhage [10]. Otherwise, surgery remains the most accepted treatment, with the limited right hemicolectomy being the preferred surgical approach.
4. Conclusion
This is a very rare case of colonic lipomatosis presenting with acute appendicitis. Clinical examination and imaging studies are essential in making the right diagnosis. Surgery is the preferred treatment approach in case of acute abdominal complications of colonic lipomatosis.
Funding
None.
Ethical approval
The study is exempt from ethical approval in our institution.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Gerti Dajti
Alessio Vagliasindi
Simone Bosi
Enrico Guerra
Federico Zanzi
Gian Domenico Raulli
Contribution according to the SCARE report:
Gerti Dajti – 3, 4, 9–11
Alessio Vagliasindi – 4, 11
Simone Bosi – 5–8
Enrico Guerra – 11
Federico Zanzi – 11
Gian Domenico Raulli – 6, 8, 11
Registration of research studies
Not applicable as not a “first-in-man” study.
Guarantor
Dott. Alessio Vagliasindi.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of Competing Interest
The authors report no declarations of interest.
References
- 1.Agha R.A., Borrelli M.R., Farwana R. The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 2.Weinberg T., Feldman M., Sr. Lipomas of the gastrointestinal tract. Am. J. Clin. Pathol. 1955;25(3):272–281. doi: 10.1093/ajcp/25.3.272. [DOI] [PubMed] [Google Scholar]
- 3.Bilgic Y., Altinsoy H.B., Yildirim N., Alatas O., Kanat B.H., Sahin A. Familial abdominal and intestinal lipomatosis presenting with upper GI bleeding. Case Rep. Gastrointest. Med. 2015;2015 doi: 10.1155/2015/123723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pagacz M., Willis I., Alexis J. Massive lipomatosis of the small intestine causing intussusception. Case Rep. Gastrointest. Med. 2019;2019 doi: 10.1155/2019/9701478. Published 2019 Dec 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar K., Noori M.R., Patel K.M., Yuen W., Bello C. Rare diagnosis of intestinal lipomatosis complicated by intussusception in an adult: a case report. Int. J. Surg. Case Rep. 2017;39:339–342. doi: 10.1016/j.ijscr.2017.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamid H.K., Ahmed I., Mohamed A., O’Hanrahan T. Ileocecal lipohyperplasia presenting as a chronic sideropenicanaemia. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2012-008052. bcr-2012-008052. Published 2013 Jul 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith S.R., Fenton L. Lipohyperplasia of the ileo-caecal valve causing appendicitis. Aust. N. Z. J. Surg. 2000;70(1):76–77. doi: 10.1046/j.1440-1622.2000.01752.x. [DOI] [PubMed] [Google Scholar]
- 8.Börekci H., Serin H.İ, Baş H., Börekci E. Relationship between appendicitis and diameter of ileocecal lipomatosis and also ileocecal angle. Surg. Radiol. Anat. 2020;42(4):437–441. doi: 10.1007/s00276-019-02392-8. [DOI] [PubMed] [Google Scholar]
- 9.Ure E., Cingoz M., Kandemirli S.G., Akbas S., Tutar O., Ogut A.G. CT and MR imaging features of diffuse lipomatosis of the abdomen. Diagn. Interv. Imaging. 2016;97(11):1189–1191. doi: 10.1016/j.diii.2016.03.013. [DOI] [PubMed] [Google Scholar]
- 10.Geraci G., Pisello F., Arnone E., Sciuto A., Modica G., Sciumè C. Endoscopic resection of a large colonic lipoma: case report and review of literature. Case Rep. Gastroenterol. 2010;4(1):6–11. doi: 10.1159/000260053. Published 2010 Feb 3. [DOI] [PMC free article] [PubMed] [Google Scholar]