Abstract
Spontaneous disappearing breast calcifications is a rarely-reported phenomenon and the relatively small number of studies that have been done mostly associated the resolution of benign-appearing breast calcifications with benign processes. We present a case of a postmenopausal woman who had spontaneously resolving grouped, coarse heterogenous calcifications in the setting a new soft tissue mass which was pathologically proven to be invasive ductal carcinoma. A handful of studies have shown the resolution of indeterminant calcifications to be associated with malignancy, and interestingly, all of these cases also demonstrated a new parenchymal abnormality which is akin to the present case. Overall, the majority of benign-appearing spontaneous resolving microcalcifications likely are related to benign processes; however, radiologists should be aware of the association of disappearing grouped, indeterminant calcifications with the resulting development of malignancy, especially in the presence of a nearby, newly-forming soft tissue mass.
Keywords: Disappearing calcifications; Resolving calcifications; Breast cancer; Malignancy, Mammography
Introduction
Breast calcifications are a common mammographic finding and characteristics of the calcifications help classify them as benign or suspicious [1]. Specifically, the American College of Radiology Breast Imaging Reporting and Data System (ACR BI-RADS) classifies calcifications based on morphology and distribution [2]. Benign morphologies include round, rim, dystrophic, and milk of calcium calcifications; whereas, suspicious morphologies include amorphous, coarse heterogenous, fine pleomorphic, and fine-linear/fine-linear branching calcifications [2].
Spontaneous resolving/disappearing breast calcifications is a rarely-reported occurrence [3]. The relatively small number of prior studies demonstrate that resolution of benign-appearing breast calcifications is nearly always related to benign processes; whereas, the disappearance of indeterminant calcifications can be associated with a contemporaneous malignancy [3].
We present a case of a postmenopausal woman who had spontaneously resolving calcifications contemporaneous with the formation of a soft tissue mass which was pathologically diagnosed as invasive ductal carcinoma. The disappearing calcifications were initially interpreted as benign-appearing; however, on retrospective review they were more consistent with coarse heterogenous calcifications and should have been deemed indeterminate and given a BIRADS 4. This case report adds to the limited number of published studies demonstrating the association between malignancy and the disappearance of an isolated group of indeterminate microcalcifications. The modern radiologist should be aware of this association and be wary of decreasing or disappearing calcifications on follow-up examinations.
Case report
A postmenopausal woman (G5P4A1) over age 65 with a PMHx of hypertension and peripheral vascular disease presented for screening mammography. She was a non-drinker with a 20-pack-year smoking history. Family history of breast cancer included a maternal niece. Her last menstrual period was at age 51. She had never been on hormone replacement therapy nor had evidence of hyperparathyroidism or hypercalcemia.
The patient had a screening mammogram notable for 2 new groups of calcifications in the right breast, group 1 within the upper-outer aspect, posterior depth and group 2 within the lower-inner aspect, middle depth (Fig. 1A and B). Tomosynthesis was performed but did not aid in calcifications characterization nor did it identify an accompanying mass or architectural distortion. Her prior screening mammograms for comparison were notable only for heterogeneously dense breasts with bilateral benign-appearing calcifications. She was called back from screening for a diagnostic mammogram with additional views.
Fig. 1.
Mammographic images of the right breast from the patient's original screening mammogram are shown including the MLO position (A) and CC position (B). This screening mammogram demonstrated new grouped calcifications in the upper-outer aspect posterior depth (group 1; blue circle on MLO and blue arrow on CC). This mammogram also noted new grouped calcifications in the lower-inner aspect of the breast middle depth (group 2; red arrow on both images). Both of these calcifications were considered indeterminant and a diagnostic mammogram with additional views was recommended.
On diagnostic mammography, the new, few faint amorphous calcifications in the right breast lower-inner region (group 2) were only seen on the craniocaudal view. These images were felt to be indeterminant suspicion for malignancy, BIRADS 4: Suspicious Abnormality [2]. A stereotactic biopsy was recommended. On magnification views, the new grouped calcifications in the right breast at upper-outer breast (group 1) were described as grouped, coarse, round, and punctate (Fig. 2). These calcifications were presumed by the interpreting radiology to be probably benign and given a BIRADS 3 category [2]. A 6-month follow-up breast mammogram was recommended.
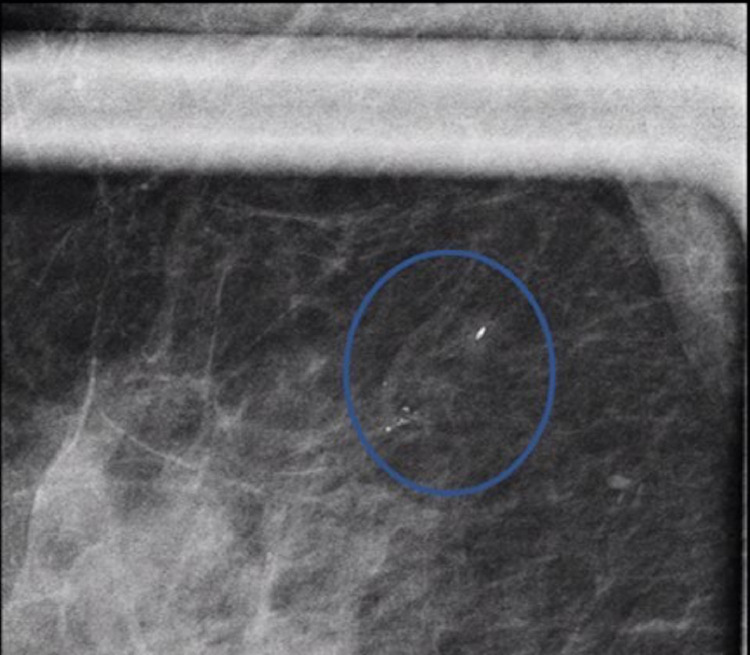
Fig. 2.
Magnification image of the group 1 calcifications in the upper-outer aspect of the breast from the patient's initial diagnostic mammogram (blue circle). The calcifications were described as grouped coarse, round, and punctate.
A stereotactic biopsy was performed on the group 2 calcifications and pathology yielded benign breast tissue and fibrocystic, non-proliferative changes. This finding was determined by the radiologists to be concordant with imaging.
She returned 7 months later for a right diagnostic mammogram (Fig. 3). At this time, a biopsy clip with a few, faint, residual calcifications were noted in the lower-inner aspect (group 2). The previously visualized calcifications in the upper-outer breast (group 1) were no longer visualized with a single coarse calcification remaining. No magnification images were acquired. The interpreting radiologist concluded that since these calcifications were no longer seen, they were probably benign, (BIRADS 3) [2]. A follow-up mammogram was recommended in 5 months to correlate with the patient's annual mammogram.
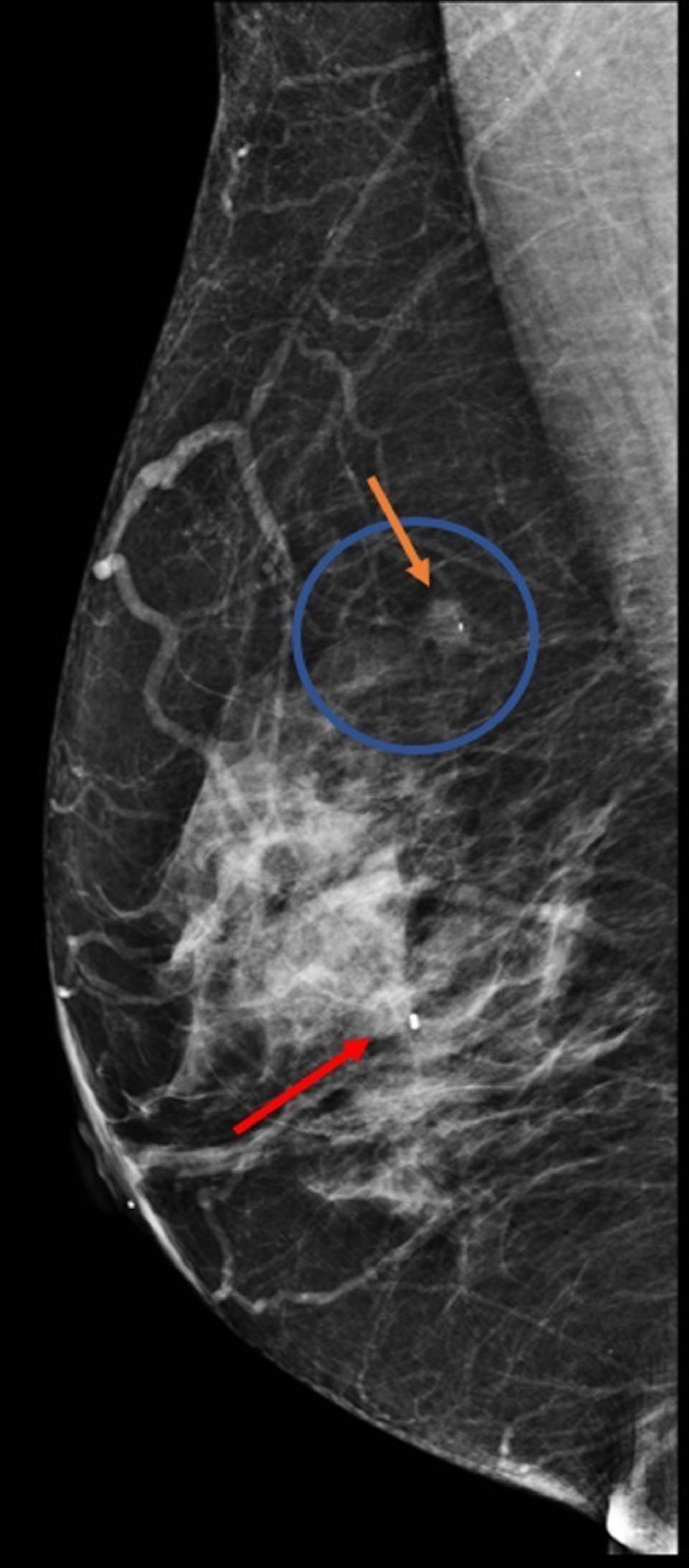
Fig. 3.
Mammographic images of the right breast from the patient's diagnostic mammogram performed 7 months after the mammogram in Figure 2. The group 2 calcifications in the lower-inner aspect of the breast had been biopsied with a benign concordant result and a biopsy clip with a few faint surrounding residual calcifications are seen (red arrow). The group 1 calcifications in the upper-outer aspect posterior depth were decreased with a single coarse calcification remaining (blue circle); however, a new mass is forming the region of the disappearing calcifications (orange arrow). This mass was not mentioned by the interpreting radiologist.
On the diagnostic mammogram 5 months later, a new 1.9 × 1.3 × 1.0 cm irregular, equal-density mass was identified with an indistinct margin with one internal coarse calcification in the upper-outer right breast in the region of prior group 1 calcifications (Fig. 4A). This was also seen on magnification views (Fig. 4B).
Fig. 4.
Diagnostic mammogram with MLO view (A) and magnification view (B) from the patient's diagnostic mammogram 5 months after the diagnostic mammogram in Fig. 3 which demonstrated increased size of the mass in the area of prior disappearing group 1 calcifications (blue circle) in the upper-outer aspect of the breast with a single internal coarse calcification. The red arrow again shows previous biopsied benign and concordant calcifications.
Targeted ultrasound in the region of the mass seen on mammography demonstrated a new 1.8 × 1.2 × 0.8 cm irregular mass with angular margins at 10 o'clock, 6 cm from the nipple (Fig. 5). This correlated with mammography findings in the upper-outer breast. This lesion was deemed highly suspicious of malignancy (BIRADS 5) [2]. No abnormal axillary lymph nodes were seen sonographically. Consequently, ultrasound-guided biopsy was recommended.
Fig. 5.
Ultrasound Image. The patients's ultrasound from her third diagnostic mammogram (Fig. 4). Transverse ultrasound image from 10 o'clock 6 cm from the nipple which correlates with the region of new soft tissue mass in the upper-outer breast and demonstrates a 1.8 cm irregular mass with angular margins. This mass was deemed highly suspicious of malignancy and was given a BIRADS 5. Ultrasound-guided biopsy was recommended and yielded invasive ductal carcinoma.
Biopsy of the mass was successful with pathology yielding malignant invasive ductal carcinoma without ductal carcinoma in situ. Pathology results were deemed concordant with imaging. The patient underwent breast magnetic resonance imaging to evaluate extent of disease which showed multiple irregular masses in a linear distribution contiguous with the biopsy-proven mass. The patient decided to undergo simple mastectomy over breast-conserving therapy which was preceded by neo-adjuvant chemotherapy. Final surgical pathology designated a Nottingham combined pathology grade of III consistent with poorly differentiated carcinoma. The tumor was estrogen receptor positive (52% of tumor nuclei), progesterone receptor negative, HER2 negative, and KI 67 positive (98% of tumor nuclei). The margins were clear and 4 excised lymph nodes were benign.
Discussion
Spontaneous resolving breast calcifications is an infrequently reported occurrence; but it is likely an uncommon but not rare finding [3], [4], [5], [6]. Seymour et al. conducted the largest respective review of 108,000 screening mammographs and identified 37 cases of disappearing benign and intermediate microcalcifications (0.03%) [3]. And, this research is congruent with the finding of Parker et al. who found 17 cases of disappearing calcifications from 18,000 mammograms over a 6-month period (0.09%); however, only one case was suspicious of malignancy [5]. Radiologists have observed resolving breast calcifications before, even if it has been subliminal and/or dismissed without being considered significant [5].
Seymour et al. was the first to relate resolving calcifications to malignancy [3]. They divided cases into group A, benign-appearing calcifications, and group B, indeterminant calcifications [3]. All 15 women in group A demonstrated no significant change at repeat mammogram at 36 months and no cancers were identified in a 51.5-month follow-up period. In group B, 22 patients had indeterminant microcalcifications and 8 women developed cancers. Importantly, all of the 8 cases also had a new finding such as a mass, architectural distortion, increased density or suspicious macrocalcifications nearby. These findings are similar to the present case where disappearing calcifications were related to the development of a new soft tissue mass [3].
Similarly, a case report by Mesurolle et al. linked spontaneous resolution of a small cluster of microcalcifications which were initially judged to be probably benign (BIRADS 3) with breast carcinoma [6]. However, in the conclusion the authors stated that these microcalcifications should have been classified as BIRADS category 4 and considered suspicious [6]. Of note, the disappearance of these microcalcifications was contemporaneous with the presence of a new underlying mass as in the present case report.
The Mesurolle et al. case is similar to the presented one where the initial diagnostic mammogram interpreted the new grouped calcifications in the upper-outer right breast as probably benign and a BIRADS 3 was given [6]. In retrospect, the new grouped calcifications (group 1) in this case report would have been more accurately describe as coarse heterogenous and given a BIRADS 4B category [2]. Specifically, the group 1 calcifications that disappeared were variable in size and shape and smaller than <1 mm fitting the BIRADS description of coarse heterogenous [2]. A single larger (>1 mm) coarse calcification was associated with the grouped calcifications but did not disappear and its presence may have been partially why the interpreting radiologist initially categorized the calcifications initially as coarse and benign-appearing. Importantly per BIRADS, when new isolated grouped coarse heterogenous calcifications are identified, there is a small (<15%) but real chance of malignancy [2]. In such scenarios, BIRADS 3 should be avoided [2].
Therefore, in the present case, the new, grouped coarse heterogenous calcifications (group 1) should have been more accurately described as BIRADS 4B and offered biopsy. Additionally, when following up grouped indeterminate or even previously characterized benign-appearing calcifications, the radiologist should be wary of when these calcifications decrease or disappear as underscored by the present case report and the case report by Mesurrolle et al. [6].
It should be noted that there is very high inter-reader variability in terms of coarse heterogenous calcifications as these calcifications are on a continuum ranging pleomorphic to coarse heterogenous to coarse/popcornlike-like to dystrophic calcifications often complicating assessment [2]. Consequently, even in a case where previously benign-appearing calcifications have disappeared, the area should be further scrutinized and magnification views should be considered.
All reported cases of resolving calcifications linked to malignancy have been associated with a new nearby parenchymal abnormality [3,6]. This finding underscores the importance of staying vigilant on follow-up examinations for new abnormalities, especially in cases with resolving calcifications. Moreover, it is recommended that radiologists have a low threshold for magnification views of a region where calcifications disappeared to decrease the likelihood of missing a nearby parenchymal abnormality. Additional magnification views may have helped the interpreting radiologist identify the new mass in the area of the disappearing calcifications on the post-biopsy diagnostic mammogram (Fig. 3). It should be noted satisfaction of search likely contributed to the radiologist's misinterpretation of the new mass in the region of the disappearing calcifications on the post-biopsy mammogram as the group 1 calcifications had disappeared in the area of interest and the group 2 calcifications had been recently biopsied with a benign result.
This case report adds to the limited literature associating the disappearance of calcifications with malignancy. Although certain morphologies of breast calcifications are associated with carcinoma, the dynamics of breast calcification formation and disappearance are poorly understood. The mechanism of disappearance likely is dissolution rather than extrusion via the ductal system as gradual fading has been detailed but no case has reported calcifications progressing towards the nipple [8]. It is also unclear if the resolving calcifications are coincidentally correlated with the malignant process, if the malignant process is the cause for the disappearance of the calcifications directly, if the malignant process triggers an immune response where macrophages clear the calcifications indirectly or if the calcifications are a marker of a malignant process from the beginning. Therefore, it should be cautioned in the interpretation of this manuscript that the disappearance of benign-appearing calcifications may be completely coincidental and not at all physiologically related to the development of the nearby malignancy. Future work is encouraged on the underlying pathophysiology of calcification resorption.
As mentioned earlier, evaluation of benign-appearing and suspicious-appearing calcifications is still vulnerable to inter-reader variability. The studies cited above have been conducted over multiple decades and in different countries and during this time the BI-RADS and breast imaging lexicons have changed and have varied geographically limiting extrapolation of combined analysis between present studies [7].
Importantly, spontaneous resolving calcifications are by definition not secondary to treatment for breast carcinoma (i.e., surgery, radiotherapy, chemotherapy, or hormonal therapy). Their disappearance in these scenarios has been reported and is not classified as spontaneous [3,8,9]. Additionally, cases of resolving parenchymal calcifications have been reported in patients with renal failure and secondary hyperparathyroidism [8].
Conclusion
We present a case of postmenopausal woman who had spontaneously resolving coarse heterogenous calcifications contemporaneous with the formation of a soft tissue mass which was pathologically an invasive ductal carcinoma. This study adds to the limited number of published studies associating disappearing calcifications contemporaneous with a proven malignancy. While the majority of benign-appearing spontaneous resolving microcalcifications are likely related to a benign process, radiologists should be aware of the association of indeterminate disappearing calcifications with the development of malignancy, especially in the presence of a newly forming soft tissue mass.
Footnotes
Sources of support and acknowledgements that require acknowledgement: None.
Competing Interests: The authors have declared that no competing interests exist.
Acknowledgments: None.
Patient Consent Statement: Patient consent was not needed for the present case report as no patient identifiers are present, it is not a rare diagnosis and all images have been deidentified.
References
- 1.Sickles EA, D'Orsi CJ, Basset L. ACR BI-RADS Atlas, Breast Imaging Reporting and Data System. 5th Edition. Radiology AC of, editor. Reston VA; 2013. ACR BI-RADS Mammography. [Google Scholar]
- 2.D’Orsi CJ, Sickles EA, Mendleson EB, Morris EA. American College of Radiology; Reston, VA: 2013. ACR BI-RADS Atlas, Breast Imaging Reporting and Data System. [Google Scholar]
- 3.Seymour HR, Cooke J, Given-Wilson RM. The significance of spontaneous resolution of breast calcification. Br J Radiol. 1999;72(August 1998):3–8. doi: 10.1259/bjr.72.853.10341682. [DOI] [PubMed] [Google Scholar]
- 4.Fewins HE, Whitehouse GH, Leinster SJ. The spontaneous disappearance of breast calcification. Clin Radiol. 1988;38(3):257–261. doi: 10.1016/s0009-9260(88)80522-1. [DOI] [PubMed] [Google Scholar]
- 5.Parker D, Clark L, McLelland R, Daughtery K. Disappearing breast calcifications. Radiology. 1989;172(3):677–680. doi: 10.1148/radiology.172.3.2772174. https://www.ncbi.nlm.nih.gov/pubmed/2772174 Available from: [DOI] [PubMed] [Google Scholar]
- 6.Mesurolle B, Halwani F, Pelsser V, Gagnon JH, Kao E, Tremblay F. Spontaneous resolving breast microcalcifications associated with breast carcinoma. Breast J. 2005;11(6):478–479. doi: 10.1111/j.1075-122X.2005.00136.x. [DOI] [PubMed] [Google Scholar]
- 7.Seymour H, Given-wilson R, Wilkinson L, Cooke J. Letter to the editor: resolving breast microcalcifications. 2000;20(2):307–8. [DOI] [PubMed]
- 8.Rovno HDS, Feig SA, Hughes JS, Hurford MT, Karasick D, Filippone E. Cases of the day- breast imaging case of the day. Spontaneous disappearing benign calcifications of the breast. Radiographics. 1998;18:1599–1604. doi: 10.1148/radiographics.18.6.9821202. [DOI] [PubMed] [Google Scholar]
- 9.Adwani A, Lowe S, Ebbs SR. Disappearing microcalcification after neoadjuvant chemotherapy - a case report. Eur J Surg Oncol. 2000;26(1):98–100. doi: 10.1053/ejso.1999.0748. [DOI] [PubMed] [Google Scholar]