Abstract
Juvenile idiopathic arthritis (JIA) is a group of childhood inflammatory arthropathies that affects multiple joints including the spine, particularly the cervical region. There is paucity of literature regarding JIA in the lumbosacral spine; the few published studies which discuss imaging findings in the lumbosacral spine only include cohorts of older children and adolescents. We present a 22-month-old boy with refusal to walk, in which plain radiographs and contrast-enhanced magnetic resonance imaging of the lumbosacral spine suggested a diagnosis of JIA.
Keywords: Juvenile idiopathic arthritis, Lumbosacral, Sacral, Spine, Periarticular, Osteopenia, Facet
Introduction
Juvenile idiopathic arthritis (JIA) consists of a spectrum of childhood inflammatory arthropathies including oligoarticular, polyarticular (seronegative or seropositive), and systemic onset subtypes [1]. Most cases affecting the spine cause atlantoaxial subluxation, synovitis, and ankylosis of the cervical region [2]. The lumbosacral spine may rarely be affected, and published studies have only described this occurrence in the adolescent age group [3]. We present seronegative polyarticular JIA of the lumbosacral spine initially suspected on radiographs and subsequently confirmed by magnetic resonance imaging (MRI) in a toddler.
Case presentation
A 22-month-old previously healthy boy presented to multiple chiropractors and his primary care physician with three months duration of intermittent limp due to right hip and left knee pain that flared every evening and after naps. Hip radiographs were reportedly normal at the time of these visits. The child then presented to our hospital emergency department with a fever (101°F) and acute onset refusal to walk. Physical examination demonstrated decreased range of motion and joint effusions in both knees. The initial laboratory findings were notable for a normal white blood cell count and increased erythrocyte sedimentation rate and C-reactive protein. Rheumatoid factor, C3 and C4 complement, and antinuclear antibodies were negative. Additional antibodies against dsDNA, CCP, nRNP SM IgG, Smith IgG, Scl-70 IgG, SS-A IgG, and SS-B IgG were negative. Radiographs of the left knee confirmed a large joint effusion, and radiographs of the lumbosacral spine demonstrated periarticular osteopenia in the pedicles and lamina of S1, S2, and possibly S3 and S4 (Fig. 1). Subsequently performed contrast-enhanced MRI of the lumbosacral spine revealed synovial enhancement of the right facet joint, thickening and enhancement of the ligamentum flavum, marrow edema at the pars interarticularis extending to the lamina and pedicles, and surrounding paraspinal soft tissue enhancement at the L5-S1 level (Fig. 2). Disc spaces were normal. No further imaging was obtained.
Fig. 1.
(a) Lateral radiograph of the lumbosacral spine demonstrates periarticular osteopenia in the pedicles (red arrows) and facet joint (yellow arrow) of S1 and S2, which are less conspicuous on the (b) anteroposterior view. Note, the hips appear grossly normal.
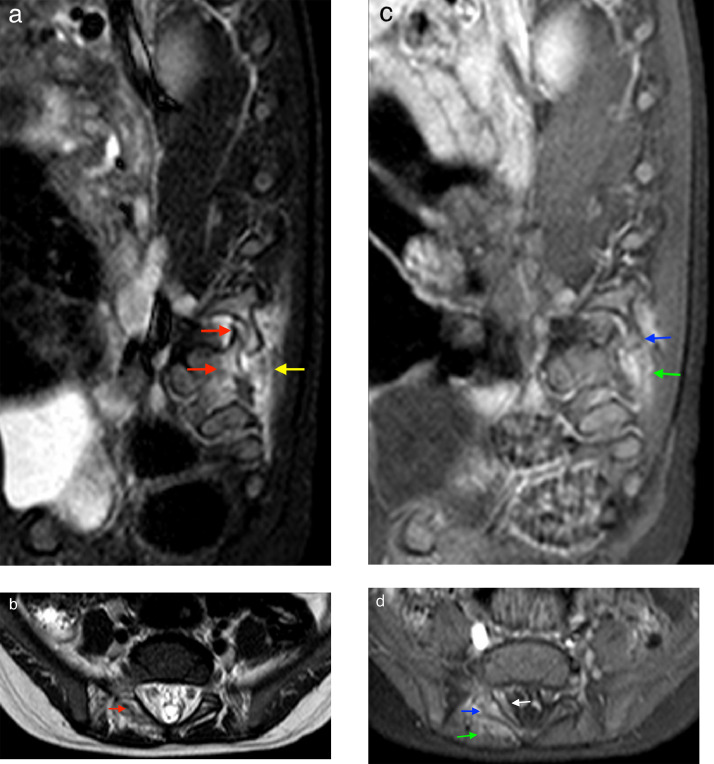
Fig. 2.
MRI of the lumbosacral spine. (a) Sagittal and (b) axial STIR images through the right L5-S1 facet reveals bone marrow edema in the right articular processes of L5 and S1 (red) with surrounding soft tissue edema (yellow). (c) Sagittal and (d) axial postcontrast T1 image at the S1 level reveals enhancement of the right lamina (blue), thickening and enhancement of the ligamentum flavum (white), and surrounding paraspinal soft tissue enhancement (green).
A constellation of clinical symptoms, laboratory results, and imaging features yielded a diagnosis of seronegative juvenile idiopathic arthritis. The patient was treated with naproxen with mild improvement of symptoms and plans were made to begin methotrexate treatment.
Discussion
Juvenile idiopathic arthritis consists of a spectrum of childhood inflammatory arthropathies found in children under 16 years old which are divided into various subtypes based on the affected joints, presence of certain antibodies, and clinical symptomatology [1]. Different subtypes include oligoarticular, polyarticular, systemic onset, enthesitis-related arthritis, psoriatic JIA, juvenile onset rheumatoid arthritis, and juvenile onset ankylosing spondylitis [1]. Although the underlying etiology is unclear, JIA is considered an autoimmune disease involving synovial hypertrophy that progresses to inflammation of the cartilage and ultimately damage to the subchondral bone [2]. JIA affects, in order of decreasing frequency, the knees, hand and wrists, hips, ankles and foot, and cervical spine [1].
Imaging evaluation of JIA involves primarily radiography and MRI [4]. Early radiographic changes include soft tissue swelling, periarticular osteopenia, and epiphyseal remodeling and widening. The first radiological signs can be mild and therefore challenging to recognize [5]. Spinal involvement in JIA occurs most frequently in the cervical region, in which ankylosis, periarticular osteopenia, and synovitis are the predominant features [2]. To our knowledge, there is no literature on periarticular osteopenia and synovitis in JIA of the lumbosacral spine, particularly in a toddler. A retrospective review conducted on 50 mostly female patients from ages 7.0-18.7 years described lumbar spine manifestations on MRI: endplate irregularities in 30%, deformed vertebrae in 21%, and intervertebral disc degeneration in 35% [3]. Vendhan et al. described 38% of subjects having apophyseal joint synovitis detected by a contrast-enhanced lumbar spine MRI in a cohort where the mean age was 16.7 years [6].
Subtle demineralization in the lumbosacral spine, specifically the pedicles and lamina as seen in our case, might be the only findings on radiography to suggest the diagnosis of JIA. In such instances intravenous contrast-enhanced MRI is warranted to confirm synovitis and to determine extent of disease, as evidence suggests that MRI is more sensitive than plain radiography [2]. As in our case, facet joint synovial enhancement, ligamentum flavum enhancement and thickening, and underlying marrow edema of the pedicles and lamina are rarely described features of juvenile idiopathic arthritis, particularly in the lumbosacral spine. Facet joint synovial enhancement and marrow edema overlap with characteristic cervical spine findings, although ankylosis was not present in our patient. Whereas cervical spine involvement indicates poorer prognosis, the role of lumbosacral spine involvement in disease progression, outcome, and response to treatment remains unknown.
Conclusion
Periarticular osteopenia in the lumbosacral spine is a subtle radiographic sign of juvenile idiopathic arthritis. Some features of JIA in the lumbosacral spine overlap with those found in the cervical spine. Our case demonstrates the importance of carefully assessing for focal osteopenia on lumbosacral spine radiographs as it might be the first clue to the diagnosis of JIA.
Footnotes
Patient Consent: Formal consents are not required for the use of entirely anonymized images from which the individual cannot be identified- for example, X-rays, ultrasound images, pathology slides or laparoscopic images, provided that these do not contain any identifying marks and are not accompanied by text that might identify the individual concerned.
Competing Interests: The authors have no competing interests to declare.
References
- 1.Sudoł-Szopińska I, Matuszewska G, Gietka P, Płaza M, Walentowska-Janowicz M. Imaging of juvenile idiopathic arthritis. Part I: Clinical classifications and radiographs. J Ultrasonogr. 2016;16(66):225–236. doi: 10.15557/JoU.2016.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Munir S, Patil K, Miller E, Uleryk E, Twilt M, Spiegel L. Juvenile idiopathic arthritis of the axial joints: a systematic review of the diagnostic accuracy and predictive value of conventional MRI. Am J Roentgenol. 2014;202(1):199–210. doi: 10.2214/AJR.12.10475. [DOI] [PubMed] [Google Scholar]
- 3.Toiviainen-Salo S, Markula-Patjas K, Kerttula L, Soini I, Valta H, Mäkitie O. The thoracic and lumbar spine in severe juvenile idiopathic arthritis: magnetic resonance imaging analysis in 50 children. J Pediatr. 2012;160(1):140–146. doi: 10.1016/j.jpeds.2011.06.030. [DOI] [PubMed] [Google Scholar]
- 4.Johnson K. Imaging of juvenile idiopathic arthritis. Pediatr Radiol. 2006;36(8):743–758. doi: 10.1007/s00247-006-0199-x. [DOI] [PubMed] [Google Scholar]
- 5.Cohen P, Job-Deslandre C, Lalande G, Adamsbaum C. Overview of the radiology of juvenile idiopathic arthritis (JIA) Eur J Radiol. 2000;33(2):94–101. doi: 10.1016/s0720-048x(99)00152-7. [DOI] [PubMed] [Google Scholar]
- 6.Vendhan K, Sen D, Fisher C, Ioannou Y, Hall‐Craggs MA. Inflammatory changes of the lumbar spine in children and adolescents with enthesitis‐related arthritis: magnetic resonance imaging findings. Arthrit Care Res. 2014;66(1):40–46. doi: 10.1002/acr.22201. [DOI] [PMC free article] [PubMed] [Google Scholar]