Introduction
Granuloma annulare is an inflammatory cutaneous disease that manifests with annular, skin-colored to red-brown papules. It may be localized or generalized, depending on lesion distribution. Patients often seek treatment because of the appearance, psychosocial effect, or symptomatic lesions.1 Classic histopathologic findings include either interstitial histiocytic inflammation or palisading histiocytes surrounding degenerating dermal collagen and mucin.1 Although localized granuloma annulare is often self-limited, with an estimated 50% of patients experiencing resolution within 2 years,1 generalized granuloma annulare is often more challenging to treat because self-resolution is less likely and there is a paucity of high-quality, evidence-based therapies.1,2
The small-molecule Janus kinase (JAK) inhibitors are a relatively new entry to the armamentarium of dermatologic therapies, and may have a specific utility in the treatment of granulomatous diseases.3 Recently, it was reported that the JAK inhibitor tofacitinib, applied as a 2% ointment, led to near resolution of treated lesions in 1 patient with localized granuloma annulare.4 Tofacitinib is selective against JAK1 and JAK3, which are involved in cytokine signaling, including upregulation of interleukin (IL) 2, IL-6, IL-10, and interferon gamma, all of which have been implicated in the pathogenesis of granuloma annulare.5,6
We describe a patient with generalized granuloma annulare treated with topical tofacitinib 2% ointment, applied only to limited lesions on the right arm, who experienced near-complete resolution of her generalized disease. We consider the potential mechanisms of local treatment producing a generalized response and highlight the need for further study of topical tofacitinib in the treatment of generalized granuloma annulare.
Case report
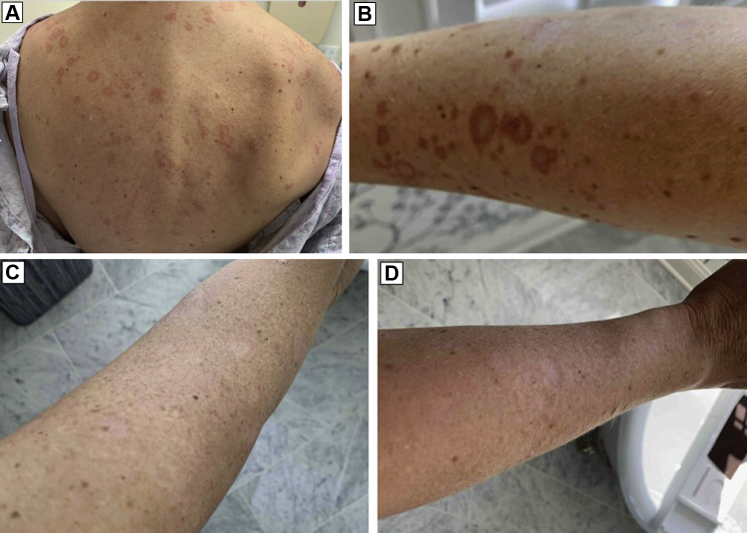
A 46-year-old woman presented for evaluation and management of asymptomatic, annular plaques. Two years before, she had noticed a single lesion on her right arm, with the subsequent development of generalized lesions. A skin examination revealed extensive red to violaceous 1- to 3-cm annular plaques of the face, arms, chest, and back, with preference for sun-exposed sites (Fig 1, A and B). Some lesions exhibited central hypopigmentation, sclerotic changes, or both. Multiple biopsies were notable for granulomatous inflammation with histiocytes, lymphocytes, and multinucleated giant cells throughout the dermis, consistent with granuloma annulare. Alcian blue staining failed to reveal mucin within the granulomas. Elastophagocytosis was absent, making actinic granuloma and annular elastolytic giant cell granuloma less likely. The result for an evaluation for sarcoidosis, including chest imaging and eye examination, was negative. The result for an additional evaluation for hematologic dyscrasias and infectious etiologies was negative.
Fig 1.
Generalized granuloma annulare before and after topical 2% tofacitinib ointment applied to right arm. A and B, Annular, red to violaceous plaques on the trunk and forearm. C and D, Improvement in lesions on upper and lower right arm after 12 weeks of topical tofacitinib.
The patient began receiving hydroxychloroquine (300 mg daily) and topical tacrolimus but achieved no response after 3 months. She transitioned to dapsone (100 mg daily), also without improvement after 1 month, and subsequently discontinued because of anemia. She was then prescribed topical tofacitinib 2% ointment (30-g tube), with instructions to use it twice daily to the right arm only. She confirmed 1 week later that she was applying the medication to her right arm. After 12 weeks, the lesions on her right arm had almost completely cleared (Fig 1, C and D), and she also noted substantial improvement of her contralateral arm and generalized lesions. Her involved body surface area decreased from approximately 10% to less than 1%. She experienced no adverse effects during treatment. She stopped applying the topical tofacitinib after 12 weeks and has had no recurrence of her generalized granuloma annulare in 2 months.
Discussion
Generalized granuloma annulare tends to exhibit a protracted course, rare spontaneous resolution, and poor response to therapy.1,5,7 Many therapeutic options are limited in part by the extent of disease and there exists a need for reliable, evidence-based therapies for this condition. The greater surface area involved in generalized granuloma annulare often precludes treatments that are commonly used in localized granuloma annulare, such as intralesional steroids, high-potency topical steroids, or cryotherapy.7 Patients are often treated with a variety of systemic medications or phototherapy, with variable response rates.7
The patient presented here applied topical tofacitinib 2% ointment to a limited treatment area and experienced near-complete resolution of her widespread granuloma annulare. Together with the prior Case Report describing the efficacy of topical tofacitinib for localized granuloma annulare,4 our case further suggests that topical JAK inhibition deserves additional study in granuloma annulare.
The observation of generalized improvement with localized therapy is intriguing. To our knowledge, this property has not been described for JAK inhibitors in other dermatoses, perhaps because the use of these medications is still relatively uncommon in dermatology. We considered the potential systemic absorption of topical tofacitinib as the mechanism behind improvement of more distant lesions. In patients with atopic dermatitis, measurement of plasma tofacitinib concentration after topical application lends some support to this theory. Among patients with atopic dermatitis who were applying tofacitinib 2% ointment over limited areas, 24% had plasma concentrations of the drug greater than 1 ng/mL a mean of 0.6 hours later.8 For comparison, the mean concentration after a 5-mg oral dose, as used in rheumatoid arthritis, is approximately 17.0 ng/mL.8 The plasma concentration with topical treatment in some patients may be sufficient to produce a therapeutic response at distal lesions.
Alternatively, patients with granuloma annulare may have ongoing systemic inflammation that local treatment may improve. In prior studies, both lesional skin and normal skin in granuloma annulare patients demonstrated upregulation of the T helper cell type 1 cytokine interferon gamma, innate immune tumor necrosis factor α, JAK3, and the T helper cell type 2 cytokine IL-4.9 The finding of these biomarkers in normal skin suggests that granuloma annulare lesions may have a widespread inflammatory influence and treating even a limited area may have favorable systemic effects. Although there are few precedents for local treatment producing a generalized response in an inflammatory dermatosis, a similar phenomenon may occur in id reactions, in which treating a primary lesion can resolve distant manifestations.10
Despite the promise of JAK inhibition in granuloma annulare, this case has several important limitations. It is possible that this patient experienced spontaneous resolution of her granuloma annulare despite its occurring uncommonly in generalized granuloma annulare.7 Alternatively, it is possible that some exogenous factor led to the patient's improvement, such as increased ultraviolet light exposure or other unexplained factors. Again, this seems unlikely because her lesions had been previously present despite many seasonal alterations.
We report near-complete resolution of generalized granuloma annulare with topical tofacitinib 2% ointment applied to only a limited area. Our case highlights the need for further exploration of JAK inhibition in localized and generalized granuloma annulare.
Footnotes
Funding sources: None.
Conflicts of interest: Dr Rosenbach has served as a consultant for Merck, Janssen, aTyr, and Processa, and received research support from Processa. Dr Shields and Mr Durgin have no conflicts of interest to declare.
References
- 1.Thornsberry L.A., English J.C. Etiology, diagnosis, and therapeutic management of granuloma annulare: an update. Am J Clin Dermatol. 2013;14(4):279–290. doi: 10.1007/s40257-013-0029-5. [DOI] [PubMed] [Google Scholar]
- 2.Piette E.W., Rosenbach M. Granuloma annulare: pathogenesis, disease associations and triggers, and therapeutic options. J Am Acad Dermatol. 2016;75(3):467–479. doi: 10.1016/j.jaad.2015.03.055. [DOI] [PubMed] [Google Scholar]
- 3.Rosenbach M. Janus kinase inhibitors offer promise for a new era of targeted treatment for granulomatous disorders. J Am Acad Dermatol. 2020;82(3):e91–e92. doi: 10.1016/j.jaad.2019.06.1297. [DOI] [PubMed] [Google Scholar]
- 4.Damsky W., King B.A. Treatment of granuloma annulare with tofacitinib 2% ointment. JAAD Case Rep. 2020;6(1):69–71. doi: 10.1016/j.jdcr.2019.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang J., Khachemoune A. Granuloma annulare: a focused review of therapeutic options. Am J Clin Dermatol. 2018;19(3):333–344. doi: 10.1007/s40257-017-0334-5. [DOI] [PubMed] [Google Scholar]
- 6.Hodge J.A., Kawabata T.T., Krishnaswami S. The mechanism of action of tofacitinib-an oral Janus kinase inhibitor for the treatment of rheumatoid arthritis. Clin Exp Rheumatol. 2016;34(2):318–328. [PubMed] [Google Scholar]
- 7.Yun J.H., Lee J.Y., Kim M.K. Clinical and pathological features of generalized granuloma annulare with their correlation: a retrospective multicenter study in Korea. Ann Dermatol. 2009;21(2):113–119. doi: 10.5021/ad.2009.21.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Purohit V.S., Ports W.C., Wang C., Riley S. Systemic tofacitinib concentrations in adult patients with atopic dermatitis treated with 2% tofacitinib ointment and application to pediatric study planning. J Clin Pharmacol. 2019;59(6):811–820. doi: 10.1002/jcph.1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Min M.S., Wu J., He H. Granuloma annulare skin profile shows activation of T-helper cell type 1, T-helper cell type 2, and Janus kinase pathways. J Am Acad Dermatol. 2020;83(1):63–70. doi: 10.1016/j.jaad.2019.12.028. [DOI] [PubMed] [Google Scholar]
- 10.Ilkit M., Durdu M., Karakaş M. Cutaneous id reactions: a comprehensive review of clinical manifestations, epidemiology, etiology, and management. Crit Rev Microbiol. 2012;38(3):191–202. doi: 10.3109/1040841X.2011.645520. [DOI] [PubMed] [Google Scholar]