Significance
In the last two decades, over 240,000 American students were on school grounds when a gunman opened fire at their school. While public attention often focuses on the victims who were killed, less is known about the impacts of school shootings on surviving youth. This study represents the largest analysis to date of the effects of school shootings on an important indicator of youth mental health: the use of prescription antidepressants. We find that local exposure to fatal school shootings leads to persistent and significant increases in youth antidepressant use. These impacts are smaller in areas with a higher density of mental health providers who focus on behavioral interventions.
Keywords: school shootings, gun violence, youth mental health, antidepressants
Abstract
While over 240,000 American students experienced a school shooting in the last two decades, little is known about the impacts of these events on the mental health of surviving youth. Using large-scale prescription data from 2006 to 2015, we examine the effects of 44 school shootings on youth antidepressant use. Our empirical strategy compares the number of antidepressant prescriptions written by providers practicing 0 to 5 miles from a school that experienced a shooting (treatment areas) to the number of prescriptions written by providers practicing 10 to 15 miles away (reference areas), both before and after the shooting. We include month-by-year and school-by-area fixed effects in all specifications, thereby controlling for overall trends in antidepressant use and all time-invariant differences across locations. We find that local exposure to fatal school shootings increases youth antidepressant use by 21.4% in the following 2 y. These effects are smaller in areas with a higher density of mental health providers who focus on behavioral, rather than pharmacological, interventions.
School shootings have become frequent tragedies in the United States. Since the shooting at Columbine High in April 1999, there have been over 249 shootings at primary and secondary schools, resulting in the loss of 147 lives (1). Public attention often focuses on the victims who were killed, but an important and understudied question is how survivors fare in the subsequent months and years. While over 240,000 students were on school grounds during a shooting in the past 20 y, little is known about the impacts of these events on the mental health of surviving youth. The large private and social costs of mental illness—especially during childhood—suggest that estimates of the effects of school shootings on mental health may be critical for assessing the overall welfare consequences of these events.*
Existing work on the mental health consequences of school shootings is limited to studies at several schools in the 1980s and 1990s (see refs. 5 and 6 for recent reviews and citations therein). These studies suggest that such events are associated with adverse psychological outcomes, but they rely on small samples, often lack control groups or preexposure data, and use surveys that may be subject to selective response bias (5, 6). Furthermore, it may be hard to extrapolate correlations from 30 to 40 y ago to events happening today.
In this study, we examine the impacts of local exposure to 44 school shootings from 2006 to 2015 on an important indicator of youth mental health: the use of prescription antidepressants.† Our empirical strategy compares the number of antidepressant prescriptions written by providers practicing 0 to 5 miles from a school that experienced a shooting (treatment areas) to the number of prescriptions written by providers practicing 10 to 15 miles away (reference areas), both before and after the shooting. We include month-by-year and school-by-area fixed effects in all specifications, thereby controlling for overall trends in antidepressant use and all time-invariant differences across locations. As communities may differ in their capacity to cope with shooting-related trauma, we further investigate heterogeneity in effects by the local availability of mental health care resources.
Our research design is predicated on the idea that providers practicing very close to an affected school treat patients who are more likely to have been exposed to the event but are otherwise very similar to the patients of providers practicing slightly farther away. As it is unclear ex ante how far from a school the effects of a shooting will extend, we demonstrate how our results change as we use alternative distances between schools and providers to define treatment areas.‡We further examine specifications using two alternative reference areas consisting of the prescriptions written by providers practicing in the vicinity of observationally similar schools that did not experience any shootings.
Our data on antidepressants come from the IQVIA Xponent database and cover the period from January 2006 to March 2015. In contrast to typical claims data that cover either one or a few insurers, the IQVIA data include the near universe of prescriptions irrespective of patients’ insurance coverage or type.§ Our primary analysis focuses on antidepressants prescribed to youth, whom we define as individuals under age 20 (i.e., aged 0 to 19). The IQVIA data are collected directly from pharmacies; as such, they do not include information on the number of patients seen by each provider. As we therefore do not have the population base necessary to construct exact prescription rates, we use the natural log of antidepressant prescriptions as our main outcome. As an alternative outcome, we consider prescription rates calculated as the number of antidepressant prescriptions written to individuals under age 20 by providers practicing in a given area divided by the number of individuals under age 20 living in the same area.
We combine the prescription data with information on school shootings from the Washington Post school shootings database. The data contain all shootings at primary and secondary schools in the United States since 1999 that occurred during school hours and posed a threat to students. To allow for 2 y of prescription data before and after each shooting, we consider school shootings that occurred between January 2008 and April 2013. For each affected school, we identify providers practicing in the treatment and reference areas using practice addresses in the IQVIA data.
Results
Since April 1999, the annual number of school shootings in the United States has ranged from 5 in 2002 to 17 in the first 5 mo of 2018 (SI Appendix, Fig. S1); 240,718 students were enrolled in these schools when they experienced a shooting. Table 1 presents mean characteristics of the 44 schools with shootings in our analysis, out of which 15 resulted in at least one victim death (“fatal” shootings). Relative to the average US school, schools that experienced a shooting had higher average enrollment, were less likely to be private, were more likely to be a high school, and had a higher average share of black students.
Table 1.
Descriptive Statistics
| School shootings | |||
| Fatal | Nonfatal | None | |
| School characteristics | |||
| Enrollment (1,000s) | 1.22 | 0.90 | 0.44 |
| Private | 0.13 | 0.07 | 0.22 |
| High school | 0.40 | 0.55 | 0.15 |
| % White | 0.49 | 0.43 | 0.59 |
| % Black | 0.17 | 0.37 | 0.16 |
| % Reduced lunch | 0.43 | 0.51 | 0.44 |
| Characteristics of shootings | |||
| Victims killed | 2.80 | 0.00 | – |
| Victims injured | 0.47 | 0.76 | – |
| Shooter age | 25.60 | 18.46 | – |
| Shooter male | 0.80 | 0.97 | – |
| Number of schools | 15 | 29 | 127,363 |
| Youth antidepressant prescriptions per 1,000 | |||
| Treatment areas | |||
| Preshooting/postshooting | 7.70/9.52 | 5.64/6.86 | – |
| Reference areas | |||
| Primary, preshooting/postshooting | 8.09/9.05 | 8.71/10.02 | – |
| Alt. A, overall | 6.87 | 10.45 | – |
| Alt. B, preshooting/postshooting | 11.07/12.63 | 7.09/7.95 | – |
The first two columns report averages for schools with shootings in our analysis. The last column reports averages for all US schools. Youth antidepressant prescriptions per 1,000 refer to mean monthly antidepressant prescriptions for individuals under age 20. Treatment (primary reference) areas consist of providers practicing 0 to 5 miles (10 to 15 miles) from schools that experienced a shooting. Alternative (Alt.) reference areas A and B consist of providers practicing 0 to 5 miles from nonshooting schools with the highest predicted shooting probability (A) and with characteristics matched to individual shooting schools (B). We cannot separate preshooting and postshooting prescription rates for alternative reference areas A, as the comparison schools in those areas are not matched to specific shooting dates.
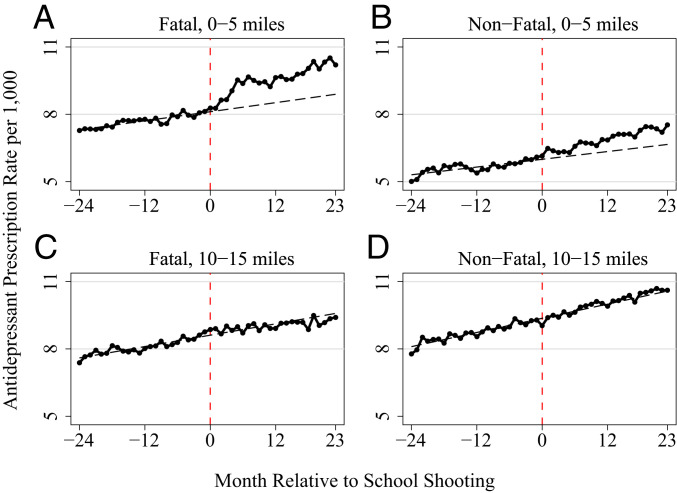
To examine changes in youth antidepressant use surrounding school shootings, we first plot monthly antidepressant prescription rates for individuals under age 20 in the 2 y surrounding a school shooting. We plot prescription rates separately for the treatment and reference areas and for fatal and nonfatal shootings. We further plot linear fits of the data using only preshooting observations; these lines provide counterfactuals for how prescriptions are expected to have progressed in the absence of a school shooting.
As shown in Fig. 1, antidepressant use in the treatment areas increased dramatically following a school shooting and remained at elevated levels through the end of the observation period. There is no apparent trend break in the reference areas. The increase in antidepressant use in the treatment areas is noticeably larger following fatal than nonfatal shootings. Patterns in the raw data therefore point to a persistent effect of fatal school shootings on youth antidepressant use.
Fig. 1.
Youth antidepressant use by month relative to school shootings. The solid black lines show the monthly number of antidepressant prescriptions written to individuals under age 20 by providers located 0 to 5 miles (A and B) or 10 to 15 miles (C and D) from a school that experienced a fatal (A and C) or non-fatal (B and D) shooting per 1,000 individuals under age 20 residing in these areas. The dashed gray lines are linear fits based on regressions using only preshooting observations.
We formalize this analysis using a difference-in-difference design. We regress the natural log of the monthly number of antidepressant prescriptions written for individuals under age 20 in the 2 y surrounding a school shooting on an indicator denoting the postshooting time period, an interaction between the postshooting indicator and an indicator denoting treatment areas, year-by-month fixed effects, and school-by-area fixed effects. The year-by-month fixed effects account for aggregate trends in youth antidepressant use. The school-by-area fixed effects account for all time-invariant differences across locations, including preshooting levels of antidepressant use. We cluster standard errors at the school-by-area level.
The results are presented in Table 2. When the outcome is log antidepressant prescriptions, our coefficient of interest measures the percentage difference in the postshooting change in the number of antidepressant prescriptions written to individuals under age 20 between the treatment and reference areas. As shown in the first column, youth antidepressant use increases by 21.3% in the treatment areas in the 2 y following a fatal school shooting. When extending the postshooting observation window to 3 y, we observe a 24.5% increase. These effects of fatal school shootings are concentrated among shootings that occur in high schools (SI Appendix, Table S2). We find no statistically significant changes in youth antidepressant use following nonfatal school shootings, and results are very similar in percentage terms when we use prescription rates as an alternative outcome.
Table 2.
Effects of school shootings on youth antidepressant use
| Fatal | Nonfatal | |||
| 2 y | 3 y | 2 y | 3 y | |
| ln(antidepressant prescriptions) | ||||
| Treatment × post | 0.213*** | 0.245*** | 0.0187 | 0.0603 |
| (0.064) | (0.079) | (0.060) | (0.053) | |
| Antidepressant prescription rate per 1,000 | ||||
| Treatment × post | 1.982** | 2.645** | 1.674 | 0.348 |
| (0.940) | (1.241) | (1.219) | (0.701) | |
| Relative to mean | 0.206** | 0.297** | 0.163 | 0.037 |
| Schools | 15 | 12 | 29 | 24 |
| Observations | 1,412 | 1,410 | 2,601 | 2,718 |
The table reports output from estimation of our primary difference-indifference specification. We regress measures of antidepressant prescriptions for individuals under age 20 at the school–area–month level on an indicator denoting months in or after a school shooting (“post”), an interaction between the post indicator and an indicator denoting treatment areas, month-by-year fixed effects, and school-by-area fixed effects. The treatment (reference) areas include providers practicing 0 to 5 miles (10 to 15 miles) from an affected school. All regressions are weighted by school enrollment, and standard errors (reported in parentheses) are clustered at the school-by-area level. .
Our difference-in-difference strategy requires that prescriptions would have followed similar trends across the treatment and reference areas in the absence of a school shooting. To examine the validity of this parallel trends assumption and to explore the time path of effects, we estimate quarterly event study specifications. In these models, we replace the postshooting indicator with separate indicators for each of the eight quarters before and after the shooting, omitting the indicator for the quarter before the shooting.
Fig. 2 plots the estimated coefficients from these regressions. The insignificant coefficients before the shooting indicate that there were no differential pretrends across the treatment and reference areas. Within 6 mo of a fatal school shooting, however, antidepressant prescriptions increase by nearly 30% and remain at this elevated level for at least 2 y. As in Table 2, Fig. 2 shows that youth antidepressant use is not affected by nonfatal school shootings.
Fig. 2.
Effects of school shootings on youth antidepressant use. The figure presents output from estimation of event study analogs of our primary difference-in-difference specification, in which we replace the postshooting indicator with separate indicators for each of the eight quarters before and after the shooting. The indicator for the quarter before the shooting is omitted. We plot the coefficients and 95% CIs on the interactions between quarterly event time indicators and the indicator denoting treatment areas.
Prior work has suggested that the negative effects of exposure to violence on children’s cognitive outcomes are temporary (e.g., ref. 9). To examine whether the observed increases in youth antidepressant use fade over time, SI Appendix, Fig. S2 presents estimates from event study specifications that use follow-up windows of 3 to 6 y. Although our sample size diminishes considerably as we extend the observation window, and thus these results may not be generalizable, we find that fatal school shootings lead to increases in youth antidepressant use that persist over these longer time horizons.
Local areas may vary in their capacity to cope with trauma in the aftermath of a school shooting. To investigate whether the impacts of school shootings differ by the availability of local mental health care resources, we examine how our estimates vary across locations with differing densities of providers who treat mental health conditions among children. As different types of providers differ in their focus on pharmacological versus behavioral treatment, we consider both the local density of prescribing providers (physicians in family medicine, pediatrics, and psychiatry) and nonprescribing providers (psychologists and social workers).¶
SI Appendix, Table S3 presents estimates from an augmented version of our difference-in-difference specification that includes triple interactions between the post indicator, the treatment indicator, and terciles of county-level measures of provider densities. We see that there are no significant differences in the effects of fatal school shootings across counties with differing densities of prescribing providers. In contrast, areas with a higher density of nonprescribing practitioners experience significantly smaller increases in youth antidepressant use following a fatal school shooting. This pattern holds even when controlling for the density of prescribing practitioners within each county. This is consistent with the possibility that areas with more psychologists and social workers may rely on nonpharmacological treatment, such as cognitive behavioral therapy, to treat shooting-induced trauma. However, we note that this analysis relies on residual variation in prescriber and nonprescriber densities across only 12 counties represented in our sample of fatal school shootings. The results may therefore be of limited generalizability to other areas.
Discussion
Understanding the mental health consequences of school shootings is critical both for informing cost–benefit analyses of policies aimed at reducing gun violence and for designing programs to help mitigate the consequences of shootings when they do occur. Accordingly, leading scholars across multiple disciplines have recently issued calls for more evidence on the impacts of shootings on survivors (6, 10, 11). Using large-scale prescription data, we document that local exposure to fatal school shootings leads to significant and persistent increases in antidepressant use among American youth.
A large literature suggests that exposure to violence—such as neighborhood crime, domestic violence, and school bullying—has adverse effects on children’s mental health (e.g., refs. 12–17). However, nonrandom selection into violent settings makes it difficult to ascertain causal relationships from previous work (18). We overcome this challenge by leveraging the quasi-random timing of school shootings as a natural experiment. Our work therefore complements existing studies that use natural experiments to examine the impacts of violence on outcomes other than mental health, such as children’s short-term educational and behavioral outcomes (9, 19–30).
Moreover, it is possible that school shootings have different effects on youth mental health than other types of violence. A recent study of police killings of African Americans found a deterioration in the self-reported mental health of black adults due to communal bereavement and increased fear and vigilance (31). Analogously, youth exposed to school shootings may suffer differentially because of the direct connection they feel to victims and the loss of a sense of security at their schools. Notably, we find no differences in effects across areas with differing crime rates (SI Appendix, Table S4), suggesting that fatal school shootings even affect the mental health of students who are already exposed to violence outside of school.
The impacts of school shootings on youth antidepressant use that we find are remarkably persistent. In contrast to the literature on childhood resilience, which suggests that exposure to a single violent event may not have lasting effects (32, 33), we find that exposure to a single, fatal school shooting leads to worse mental health among local youth for years. These lasting impacts are consistent with the development of chronic mental health conditions for which clinical practice guidelines recommend long or indefinite treatment (7, 8). Other factors, such as heightened insecurity in the local community (34, 35), could further contribute to persistent mental health effects.#
Our primary specification compares the number of antidepressant prescriptions written by providers practicing 0 to 5 miles from an affected school to those written by providers practicing 10 to 15 miles away, both before and after the shooting. Two assumptions must hold for this research design to be valid. First, antidepressant prescriptions in these areas must be on parallel trends in the absence of a school shooting. Since providers practicing very close to an affected school are likely to treat patients who are similar—both in terms of sociodemographics and access to mental health care resources—to the patients of providers practicing slightly farther away, we expect this assumption to hold. Consistent with this conjecture, Table 1 shows that mean antidepressant prescription rates before fatal school shootings were similar in our treatment and reference areas (7.70 and 8.09 per 1,000 youth, respectively), while Fig. 1 shows that antidepressant prescription rates were on similar trends across these areas in the 2 y before the event.
Second, our research design requires that providers practicing very close to an affected school are more likely to treat patients who were impacted by the event than providers practicing slightly farther away. If individuals who see providers practicing 10 to 15 miles away from the school are also impacted by the shooting, then our estimates will understate the true effects of school shootings. That said, we found no observable changes in antidepressant prescriptions written by providers practicing 10 to 15 miles from affected schools (Fig. 1), suggesting that such spillovers are not present in our setting.
Nevertheless, to ensure that our results are not driven by our choice of treatment or reference areas, we conduct two additional sets of analyses. First, we estimate specifications that use as alternative reference areas the number of antidepressant prescriptions written by providers practicing 0 to 5 miles from 1) nonshooting schools with the highest predicted probability of experiencing a shooting based on school characteristics (“alternative reference areas A”) and 2) nonshooting schools matched individually to each school that experienced a shooting based on observable characteristics (“alternative reference areas B”).‖ As shown in SI Appendix, section C, analyses using these alternative reference areas yield estimates that are slightly smaller, but statistically indistinguishable, from our baseline model. At the same time, Table 1 shows that our primary reference areas are most similar to the treatment areas in terms of antidepressant prescription rates prior to fatal school shootings, supporting our choice of baseline model.
Second, we assess the robustness of our results to defining treatment areas using distances of 0 to 1 miles, 0 to 2 miles, …, 0 to 9 miles between providers and schools. As shown in SI Appendix, Fig. S5, the effects become more precise as we include providers practicing in larger areas. The estimated effect peaks when defining the treatment area as 0 to 4 miles from a school, but the point estimate is very similar and not statistically different for our primary definition of 0 to 5 miles. As expected, the effects decline as we add providers practicing farther away.
By examining the effects of 44 shootings at primary and secondary schools across the United States, this study provides the largest analysis to date of the impacts of school shootings on youth mental health. While fortunately only 15 of these shootings resulted in any victim deaths, this limited number of events poses statistical challenges when estimating effects separately for fatal and nonfatal shootings. We conduct two additional analyses to address these concerns. First, to verify that no single event is driving our results, we examine the sensitivity of our estimates to dropping each school that experienced a shooting. As shown in SI Appendix, Fig. S6, our estimates are very stable regardless of which school is excluded. Second, our primary specifications cluster standard errors at the school-by-area level. As inference with a small number of clusters may be biased, we also present results using a wild cluster bootstrap in SI Appendix, Table S5 (38). The results remain statistically significant at conventional levels.
Increased antidepressant use following a school shooting could be driven either by increased incidence of mental illness or by increased treatment of existing pathology. Although we cannot definitely identify the relative contributions of these mechanisms, three findings suggest that new pathology is likely a contributing factor. First, to confirm that our results are not driven by changes in local prescribing behavior or interactions with the health care system, we examine the effects of school shootings on the other class of prescriptions available in our data extract: opioids.** As shown in SI Appendix, Fig. S7, we find no effects of school shootings on opioid prescriptions written for youth. Second, to ensure that our results are not driven by changes in treatment for underlying mental health problems, we examine the effects of school shootings on antidepressant use among adults.†† As shown in SI Appendix, Fig. S8, we find no evidence that antidepressant prescriptions for individuals aged 20 and older increase following a local school shooting. Third, as already discussed, we find no differences in effects across areas with differing densities of prescribing providers. If school shootings only lead to treatment of previously untreated pathology, then the effects should be larger in areas with greater undertreatment using medication in the preperiod—that is, areas with fewer prescribers.
One concern with our analysis of heterogeneous effects across areas with different densities of mental health providers is that provider densities are not randomly assigned. It is therefore possible that our findings are driven by other differences across locations that are correlated with the availability of mental health care resources. In particular, if school shootings were less severe (e.g., had fewer fatalities) or individuals were less likely to be insured in places with a higher density of nonprescribing providers, then we could observe smaller effects on antidepressant use in those areas simply due to differences in the severity of the event or access to health care resources. If anything, however, our data indicate that school shootings in counties with a higher density of nonprescribing providers result in slightly more victim fatalities ( = 0.13), and controlling for local insurance rates does not affect our estimates (SI Appendix, Table S6). While additional factors, such as income, may also correlate with cross-sectional variation in mental health resources, we note that confounding factors must be correlated with the density of nonprescribing providers conditional on the density of prescribing providers.
While sizable, the increases in antidepressant use that we document are unlikely to capture the full mental health consequences of school shootings. If local exposure to school shootings increases the use of nonpharmacological treatment, the use of pharmacological treatment with medications other than antidepressants, or the prevalence of untreated mental illness, then our estimates will underestimate the full effects of these events. Furthermore, to the extent that school shootings impact students’ ability to feel secure at school, exposure to these events could lead to worse behavioral, educational, and economic trajectories. As communities continue to grapple with the aftermath of school shootings, more research is needed to assess the full costs of these events for surviving youth.
Materials and Methods
IQVIA Xponent Data.
Data on antidepressant prescriptions from January 2006 to March 2015 come from the IQVIA Xponent database. IQVIA obtains these data directly from over 90% of all retail pharmacies and imputes prescriptions for missing pharmacies to match industry totals. For each prescriber, the data contain the number of antidepressant prescriptions written in each month to individuals in binned age groups. Age is provided in the following bins: 0 to 2, 3 to 9, 10 to 19, 20 to 39, 40 to 59, 60 to 64, 65 to 74, 75 to 84, and 85+. The data further contain prescriber practice addresses in 2014 from the American Medical Association.
Washington Post Data.
The Washington Post school shootings database contains information on acts of gunfire at primary and secondary schools since 1999. The database excludes shootings at after-hours events, accidental discharges that caused no injuries to bystanders, and suicides that posed no threat to other students. The database is updated as facts emerge about individual cases; the version of the database used in this paper is from June 20, 2018. For each shooting, the data include the date, the school’s name and address, the number of victims who were killed or injured, the gender and age of the shooter(s), and whether or not the shooter(s) died. The data further contain characteristics and basic student sociodemographics for the affected schools.
Supplementary Data.
To construct population measures, we aggregate block group-level population counts from the 2010 census across all block groups within 0 to 5 miles and 10 to 15 miles of each school. The census reports population counts for individuals aged 0 to 17 and individuals aged 18 and above. For each area, we estimate the population under age 20 by assuming that the population of individuals aged 18 and 19 is 2/18 of the population aged 0 to 17.
To select schools that are observationally similar to schools that experienced a shooting as alternative reference groups, we use information on school and district characteristics for all primary and secondary schools in the United States for the 2009–2010 school year from the Stanford Education Data Archive (see SI Appendix, section C for additional details).
To examine heterogeneity in effects by mental health care resources, crime rates, and health insurance coverage rates, we use data from the Centers for Disease Control and Prevention (CDC), the Uniform Crime Reporting Program (UCR), and the American Community Survey (ACS), respectively. For each county, the CDC data provide the number of pediatricians, family physicians, psychiatrists, psychologists, and licensed social workers in 2015 per 1,000 children aged 0 to 17; the UCR data provide the number of murders, rapes, robberies, and aggravated assaults in 2006 per 1,000 individuals; and the ACS data provide the percent of individuals under age 65 who had health insurance coverage in 2008.
Sample Selection.
We consider the 48 school shootings that occurred between January 2008 and April 2013. We only keep data for the first shooting that occurred at a given school since 1999 (46 school shootings over our sample window) and for schools with at least one antidepressant prescription written to an individual under age 20 by a provider in the treatment area in each of the relevant 48 mo (44 school shootings). The school shootings included in our main analysis are listed in SI Appendix, Table S1.
Statistical Analysis.
We estimate the following equation separately for fatal and nonfatal school shootings in our primary analysis:
| [1] |
where denotes the natural log of the number of antidepressant prescriptions written to individuals under age 20 in area of school in month , is an indicator that equals one for months in or after a school shooting and zero otherwise, is an indicator that equals one for treatment areas (0 to 5 miles from a school) and zero for reference areas (10 to 15 miles from a school), is a vector of month-by-year fixed effects, is a vector of school-by-area fixed effects, and is an error term. We cluster standard errors at the school-by-area level and weight the regressions by school enrollment. When estimating quarterly event study analogs, we define the shooting quarter as the 3-mo period starting with the month of the shooting. Specifications using alternative reference areas are outlined in SI Appendix, section C.
Supplementary Material
Acknowledgments
We thank J. Currie, D. Cutler, D. Grossman, A. Jena, P. Levine, M. Mello, D. Mordecai, C. Phibbs, and D. Studdert. The statements, findings, conclusions, views, and opinions contained and expressed herein are not necessarily those of IQVIA or any of its affiliated or subsidiary entities.
Footnotes
The authors declare no competing interest.
This article is a PNAS Direct Submission.
*Mental illness in childhood has been shown to have negative long-term impacts on human capital formation and adult economic outcomes, exceeding the impacts of poor physical health conditions such as childhood epilepsy and low birth weight (2, 3). Recent estimates suggest that depression alone costs the US economy over $210 billion/y in lost productivity, missed days of work, and direct health care costs stemming from related physical and mental illnesses (4).
†Antidepressants are frequently used to treat mental health conditions that may be relevant for shooting survivors, including major depressive disorder and posttraumatic stress disorder (7, 8).
‡Among our sample schools included in the School Attendance Boundary Survey, the average school attendance area is 80 square miles (SI Appendix, section D). Students attending schools that experienced a shooting are therefore likely to live within our treatment areas of 5 miles surrounding the school ().
§We only observe the number of prescriptions, not the number of pills or strength of the medication provided with each script. While the number of scripts could increase without the total quantity of antidepressants dispensed rising, more frequent but smaller prescriptions would suggest increased monitoring that in itself is indicative of worsening mental health (7, 8).
¶Although a few states have recently expanded their scope of practice legislation to allow certain psychologists to prescribe some medications, prescribing has traditionally been limited to physicians. Furthermore, while physicians can in principle provide psychotherapy, the vast majority of physicians—even those who specialize in psychiatry—no longer provide behavioral therapy.
#The null effects of nonfatal school shootings are consistent with work underscoring the complex and nonlinear ways in which exposure to trauma influences well-being (e.g., refs. 36 and 37). It is also possible that nonfatal shootings affect other outcomes that are not observed in our data.
‖See SI Appendix, section C for details on the construction of these alternative reference areas.
**Opioid prescriptions for youth are nearly as common as antidepressants: According to our data, there were 10.3 million antidepressant prescriptions for individuals under age 20 across the entire United States in 2010 compared to 9.1 million opioid prescriptions. There is therefore scope for opioid use to respond if individuals were to have greater interaction with the health care system.
††Of course, the mental health of adults could also be directly affected by school shootings.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2000804117/-/DCSupplemental.
Data Availability.
The IQVIA Xponent database is proprietary; interested researchers should contact IQVIA to inquire about purchasing the data. All other datasets used in this study are publicly available online. See SI Appendix, section E for additional details and download links.
References
- 1.Cox J. W., Rich S., Chiu A., Muyskens J., Ulmanu M., More than 240,000 students have experienced gun violence at school since Columbine, Washington Post, January 24, 2020. https://www.washingtonpost.com/graphics/2018/local/school-shootings-database/. Accessed 5 April 2020.
- 2.Currie J., Stabile M., Child mental health and human capital accumulation: The case of ADHD. J. Health Econ. 25, 1094–1118 (2006). [DOI] [PubMed] [Google Scholar]
- 3.Goodman A., Joyce R., Smith J. P., The long shadow cast by childhood physical and mental problems on adult life. Proc. Natl. Acad. Sci. U.S.A. 108, 6032–6037 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greenberg P. E., Fournier A. A., Sisitsky T., Pike C. T., Kessler R. C., The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J. Clin. Psychiatry 76, 155–162 (2015). [DOI] [PubMed] [Google Scholar]
- 5.Lowe S. R., Galea S., The mental health consequences of mass shootings. Trauma Violence Abuse 18, 62–82 (2017). [DOI] [PubMed] [Google Scholar]
- 6.Travers Á., McDonagh T., Elklit A., Youth responses to school shootings: A review. Curr. Psychiatry Rep. 20, 47 (2018). [DOI] [PubMed] [Google Scholar]
- 7.American Psychiatric Association , Practice guideline for the treatment of patients with major depressive disorder. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd.pdf. Accessed 25 August 2020.
- 8.American Psychiatric Association , Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/acutestressdisorderptsd.pdf. Accessed 25 August 2020.
- 9.Sharkey P., The acute effect of local homicides on children’s cognitive performance. Proc. Natl. Acad. Sci. U.S.A. 107, 11733–11738 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rowhani-Rahbar A., Zatzick D., Rivara F., Long-lasting consequences of gun violence and mass shootings. J. Am. Med. Assoc. 321, 1765–1766 (2019). [DOI] [PubMed] [Google Scholar]
- 11.Iancu A., et al. , “After school shootings children and communities struggle to heal.” Health Affairs, July 19, 2019. https://www.healthaffairs.org/do/10.1377/hblog20190717.855810/full/. Accessed 25 August 2020.
- 12.Lowe S. R., Blachman-Forshay J., Koenen K. C., “Epidemiology of trauma and trauma-related disorders: Trauma as a public health issue” in Evidence-Based Treatments for Trauma-Related Psychological Disorders, Schnyder U., Cloitre M., Eds. (Springer, New York, NY, 2015), pp. 11–40. [Google Scholar]
- 13.Fowler P. J., Tompsett C. J., Braciszewski J. M., Jacques-Tiura A. J., Baltes B. B., Community violence: A meta-analysis on the effect of exposure and mental health outcomes of children and adolescents. Dev. Psychopathol. 21, 227–259 (2009). [DOI] [PubMed] [Google Scholar]
- 14.Krug E. G., Mercy J. A., Dahlberg L. L., Zwi A. B., The world report on violence and health. Lancet 360, 1083–1088 (2002). [DOI] [PubMed] [Google Scholar]
- 15.Flannery D. J., Wester K. L., Singer M. I., Impact of exposure to violence in school on child and adolescent mental health and behavior. J. Community Psychol. 32, 559–573 (2004). [Google Scholar]
- 16.Janosz M., et al. , Are there detrimental effects of witnessing school violence in early adolescence? J. Adolesc. Health 43, 600–608 (2008). [DOI] [PubMed] [Google Scholar]
- 17.Mrug S., Loosier P. S., Windle M., Violence exposure across multiple contexts: Individual and joint effects on adjustment. Am. J. Orthopsychiatry 78, 70–84 (2008). [DOI] [PubMed] [Google Scholar]
- 18.Sharkey P., The long reach of violence: A broader perspective on data, theory, and evidence on the prevalence and consequences of exposure to violence. Annu. Rev. Criminol. 1, 85–102 (2018). [Google Scholar]
- 19.Aizer A., “Neighborhood violence and urban youth” in The Problems of Disadvantaged Youth: An Economic Perspective, Gruber J., Ed. (University of Chicago Press, 2007), pp. 275–307. [Google Scholar]
- 20.Sharkey P. T., Tirado-Strayer N., Papachristos A. V., Raver C. C., The effect of local violence on children’s attention and impulse control. Am. J. Publ. Health 102, 2287–2293 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abouk R., Adams S., School shootings and private school enrollment. Econ. Lett. 118, 297–299 (2013). [Google Scholar]
- 22.Burdick-Will J., School violent crime and academic achievement in Chicago. Sociol. Educ. 86, 343–361 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Caudillo M. L., Torche F., Exposure to local homicides and early educational achievement in Mexico. Sociol. Educ. 87, 89–105 (2014). [Google Scholar]
- 24.Sharkey P., Schwartz A. E., Ellen I. G., Lacoe J., High stakes in the classroom, high stakes on the street: The effects of community violence on student’s standardized test performance. Sociol. Sci. 1, 199–220 (2014). [Google Scholar]
- 25.McCoy D. C., Raver C. C., Sharkey P., Children’s cognitive performance and selective attention following recent community violence. J. Health Soc. Behav. 56, 19–36 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beland L. P., Kim D., The effect of high school shootings on schools and student performance. Educ. Eval. Policy Anal. 38, 113–126 (2016). [Google Scholar]
- 27.Monteiro J., Rocha R., Drug battles and school achievement: Evidence from Rio de Janeiro’s favelas. Rev. Econ. Stat. 99, 213–228 (2017). [Google Scholar]
- 28.Heissel J. A., Sharkey P. T., Torrats-Espinosa G., Grant K., Adam E. K., Violence and vigilance: The acute effects of community violent crime on sleep and cortisol. Child Dev. 89, e323–e331 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gershenson S., Tekin E., The effect of community traumatic events on student achievement: Evidence from the beltway sniper attacks. Educ. Finance Policy 13, 513–544 (2018). [Google Scholar]
- 30.Ang D., “The effects of police violence on inner-city students.” Q. J. Econ., in press. [Google Scholar]
- 31.Bor J., Venkataramani A. S., Williams D. R., Tsai A. C., Police killings and their spillover effects on the mental health of black Americans: A population-based, quasi-experimental study. Lancet 392, 302–310 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agaibi C. E., Wilson J. P., Trauma, PTSD, and resilience: A review of the literature. Trauma Violence Abuse 6, 195–216 (2005). [DOI] [PubMed] [Google Scholar]
- 33.Goldstein S., Brooks R. B., Resilience in Children (Springer, 2005). [Google Scholar]
- 34.Studdert D. M., Zhang Y., Rodden J. A., Hyndman R. J., Wintemute G. J., Handgun acquisitions in California after two mass shootings. Ann. Intern. Med. 166, 698–706 (2017). [DOI] [PubMed] [Google Scholar]
- 35.Levine P. B., McKnight R., Firearms and accidental deaths: Evidence from the aftermath of the Sandy Hook school shooting. Science 358, 1324–1328 (2017). [DOI] [PubMed] [Google Scholar]
- 36.Kleim B., Ehlers A., Evidence for a curvilinear relationship between posttraumatic growth and posttrauma depression and ptsd in assault survivors. J. Trauma Stress 22, 45–52 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McDougall P., Vaillancourt T., Long-term adult outcomes of peer victimization in childhood and adolescence: Pathways to adjustment and maladjustment. Am. Psychol. 70, 300–310 (2015). [DOI] [PubMed] [Google Scholar]
- 38.Cameron A. C., Gelbach J. B., Miller D. L., Bootstrap-based improvements for inference with clustered errors. Rev. Econ. Stat. 90, 414–427 (2008). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The IQVIA Xponent database is proprietary; interested researchers should contact IQVIA to inquire about purchasing the data. All other datasets used in this study are publicly available online. See SI Appendix, section E for additional details and download links.