Abstract
International trends currently favour greater use of mandatory immunization. There has been little academic consideration or comparison of the existence and scope of mandatory immunization internationally. In this paper, we examine mandatory immunization in 28 Global NITAG (National Immunization Technical Advisory Group) Network (GNN) countries, including countries from every WHO region and World Bank income level classification. We found that although mandatory immunization programs, or mandatory elements within broader immunization programs, are relatively common, jurisdictions vary significantly with respect to the immunizations required, population groups affected, grounds for exemptions, and penalties for non-compliance. We also observed some loose associations with geography and income level. Based on these data, we categorized policies into a spectrum ranging from Narrow to Broad scope.
Keywords: Law, Policy, Vaccines, Mandatory vaccination, International comparisons, Global NITAG Network
1. Introduction
In the 2017 Assessment Report of the Global Vaccine Action Plan (GVAP), the World Health Organization’s (WHO) Strategic Advisory Group of Experts on Immunization (SAGE) noted a need to understand the variety of ways in which legislation and regulation have been used to advance or undermine the cause of immunization [1]. Given the public health threat posed by low or slumping immunization rates, some countries have implemented, or have considered implementing, mandatory immunization. Although there is no globally standardized definition of ‘mandatory immunization’, it is generally exemplified by requiring certain vaccinations at the individual level to control a vaccine-preventable disease at the population level [2]. For present purposes, we define it as the governmental imposition of vaccination of an identified group with refusal, if permitted at all, being possible only through a formal ‘opt-out’ procedure (for example, obtaining a medically-indicated exemption due to allergy), independent of whether a legal or economical consequence exists for improper refusal [3], [4], [5].
In this article, we present findings from the National Immunization Technical Advisory Group (NITAG) Environmental Scan, a pilot project funded by a small contract from the WHO’s Department of Immunization, Vaccines and Biologicals in 2018. It received ethics approval from the Research Ethics Board of the IWK Health Centre in Halifax, Nova Scotia, Canada (Ethics Approval No. 1023718). The Project surveyed Global NITAG Network (GNN) countries on a range of issues relating to their NITAGs and National Immunization Programs (NIPs). We report the binary presence or absence of mandates within NIPs, and their scope as shaped by the mandated vaccines, applicable population groups, and permitted exemptions. These 28 countries represent a broad range of low, lower-middle, upper-middle, and high-income countries as defined by the World Bank, as well as all six WHO regions.
Although this kind of landscape analysis has been conducted on a regional level [6], [7], and across high-income settings [8], there does not appear to be any recent academic consideration of the content and scope of mandatory immunization on a cross-regional international scale.
2. Methods
The primary means of data collection in the NITAG Environmental Scan was a secure online survey developed iteratively by the research team, with questions and structure refined through team interactions. The survey, available in both English and French, was piloted for comprehensibility and answerability with the help of five reviewers from three different WHO regions, all of whom were familiar with NITAGs. All GNN country members (40 as of June 2018) were invited to participate in the survey by a national representative drawn from the GNN Secretariat list; they entered the survey via a password-protected portal. The survey was open from June-September 2018, with three reminders issued by the GNN Secretariat.
The online survey contained 48 questions in three primary components, as follows:
-
1.
Tick-box questions tabulated quantitatively using simple descriptive statistics;
-
2.
Free-text comments analyzed qualitatively for specific jurisdictional insights and themes; and
-
3.
Requests for legal and/or policy instruments (provided via URL or email).
In addition to questions around NITAG governance and operation, the survey inquired after the existence and content of any mandatory elements of national immunization programs. Respondents in countries with mandatory elements were then asked:
-
1.
What vaccinations were required by law;
-
2.
What population groups were subject to mandates; and
-
3.
What grounds, if any, were available for requesting exemptions.
Wherever possible, answers were corroborated through independent desktop research seeking official (governmental) and peer-reviewed sources. We reviewed government webpages (e.g., Ministries of Justice, Health, Public Health Agencies, and online legislation registries), a range of legal repositories (e.g., Vaccine European New Integrated Collaborative Effort [VENICE], International Labor Organization’s National Legislation database [NATLEX]), UN, WHO global and regional policy webpages, and academic literature accessed through Google Scholar, WestLaw and WorldLII. We then supplied results of this research to national experts in the country to verify results and/or seek clarity around certain aspects of the instruments provided.
3. Sample and limitations
The Project received responses from 28 of GNN 40 countries. This represents a response rate of 70%, a strong majority of the GNN countries worldwide at the time the survey was issued in 2018. Of those 28 responding countries, 27 (all respondent countries save Nigeria) provided information about mandatory immunization in their country. Our sample comprises a broad range of countries in terms of size (geography and population) and government structures (federal and unitary), representation from all six WHO regions (Africa: 7; Americas: 5; Eastern Mediterranean: 1; Europe: 8; South-East Asia: 5; Western Pacific: 2), and all World Bank income level classifications (Low: 6; Lower-Middle: 5; Upper-Middle: 6; High: 11).
As membership in the GNN is voluntary, it is likely that our emphasis on this self-selecting group means that our respondents (and our findings) are indicative of countries for whom immunization is a strong priority. In other words, countries with NITAGs that have proactively joined the GNN and responded to the survey might have a different profile than those who have not enrolled in the GNN, or who did not respond to the survey invitation. Nonetheless, given the scope of our sample, we expect that our findings would likely be repeated across the GNN, and it is not entirely clear what new information could be found by a broader investigation within the GNN absent different and further inquiries.
The above highlights several limitations that must be explicitly addressed. First, we acknowledge that, by the end of 2018, there were 114 NITAGs worldwide meeting GVAP process criteria. The sample of GNN-associated NITAGs (40) is therefore approximately one-third of all NITAGs, and our 28 respondents represent 25% of functional NITAGs (and 12% of all countries worldwide). Thus, although our data provide an important and interesting snapshot representing all regions, any trends observed in a sample of this size cannot be generalized globally. Related to this, the sample does not include any small-country cluster that might share immunization resources and structures (such as the Caribbean). Inclusion of such clusters could introduce new forms, processes, and observations.
A second caveat relates to the limitation on the number of questions we could reasonably pose in the survey and still expect sufficient response rates. This meant that we did not ask respondents about the reasons for the presence or absence of mandatory immunization, as this inquiry would be more amenable to a survey focused entirely on mandates.
Third, immunization in some countries is governed at the subnational level which means that a single country may exhibit heterogeneity in both their NIPs and mandates. For example, in Canada and the USA, immunization programs are designed and developed, and mandates imposed (or not), at the provincial and state levels respectively. Mandatory immunization currently exists in only two Canadian provinces (Ontario and New Brunswick; previously, Manitoba also had mandatory immunization). Although all 50 US states impose some mandatory immunization, the particular vaccines required and the procedures for enforcement vary widely from state to state [2]. As such, it is not always entirely appropriate to talk about ‘national’ programs and mandates, or to draw overly general conclusions (in relation to, for example, significance of geography) from the data.
The final limitation is with respect to the fact that vaccination policy is an ever-changing function of government agendas, public health objectives, economic constraints, and practical realities. Accordingly, while our data represents (to the best of our knowledge) an accurate picture of mandatory immunization in these 27 countries as of summer 2018, it is likely – particularly in light of the ongoing COVID-19 pandemic – that in at least some jurisdictions, vaccination practice and policy has changed.2
4. Results and interpretation
Just over half (14 of 27) of the responding countries indicated some mandatory element(s) in their NIP (Table 1 ; note that we were not able to independently verify the existence of mandatory immunization in Côte d’Ivoire). Given the almost pervasive emphasis on autonomy and consent to treatment in the medical setting, this represents a relatively high rate of compulsory treatment. However, these raw data tell only a partial story, for the reality is more complex and nuanced than the numbers convey. In the following sections, we examine more closely the nature and extent of the mandates, taking into account the following factors:
-
1.
Number of vaccines mandated;
-
2.
Population groups subject to mandate;
-
3.
Exemptions from mandates; and
-
4.
Sanctions and enforcement for failure to vaccinate.
Table 1.
Presence of Mandates by Country, Region and Income Level.
| Country | WHO Region | Income Level | Population (mil) | Mandate | Legal Instrument |
|---|---|---|---|---|---|
| Côte d’Ivoire | African | Lower-Middle | 25.8 | Yes, Nationally* | Uncertain* |
| Ethiopia | African | Low | 98.7 | No | – |
| Nigeria | African | Lower-Middle | 201 | No Response | – |
| Tanzania | African | Low | 55.9 | No | – |
| Togo | African | Low | 7.5 | No | – |
| Uganda | African | Low | 40 | Yes, Nationally | Legislation |
| Zimbabwe | African | Low | 15.1 | No | – |
| Argentina | Americas | High | 45 | Yes, Nationally | Decree |
| Canada | Americas | High | 37.8 | Some Provinces | Regulation |
| Chile | Americas | High | 19.1 | Yes, Nationally | Decree |
| USA | Americas | High | 330 | Yes, All States | Legislation |
| Uruguay | Americas | High | 3.5 | Yes, Nationally | Decree |
| Jordan | Eastern Med. | Upper-Middle | 10.6 | Yes, Nationally | Uncertain† |
| Albania | European | Upper-Middle | 2.8 | Yes, Nationally | Legislation |
| Armenia | European | Upper-Middle | 2.9 | No | – |
| Belgium | European | High | 11.5 | Yes, nationally | Legislation |
| Germany | European | High | 83 | No‡ | – |
| Kazakhstan | European | Upper-Middle | 18.6 | Yes, Nationally | Decree |
| Latvia | European | High | 1.9 | Yes, Nationally | Regulation |
| Sweden | European | High | 10 | No | – |
| UK | European | High | 66.4 | No | – |
| Indonesia | S-E Asia | Lower-Middle | 267 | Yes, Nationally | Decree |
| Maldives | S-E Asia | Upper-Middle | 0.375 | Yes, Nationally | Legislation |
| Nepal | S-E Asia | Low | 29.6 | No | – |
| Sri Lanka | S-E Asia | Lower-Middle | 21 | No | – |
| Timor-Leste | S-E Asia | Lower-Middle | 1.4 | No | – |
| Australia | W. Pacific | High | 25.5 | No | – |
| China | W. Pacific | Upper-Middle | 1,400 | No | – |
*We were unable to corroborate the existence of mandatory immunization in Côte d’Ivoire.
†We were unable to verify the legal basis for mandatory immunization in Jordan.
‡At the time of our survey, Germany did not have mandatory immunization. However, in March 2020, the Measles Protection Act came into force, mandating measles immunity for certain individuals, including children and health care workers.
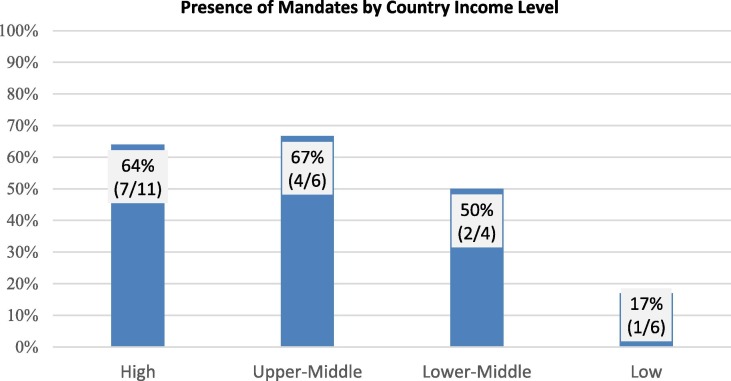
Before exploring these factors, however, we made several observations from the raw data. For example, country affluence or income level does seem to influence the presence of mandatory immunization (Fig. 1 ). Drawing on categories applied by the World Bank, high and upper-middle income countries appear more likely to have a mandatory NIP element than lower-middle and low-income countries. For example, seven of the 11 high-income countries (64%), and four of the six upper-middle-income countries (67%) reported having mandatory elements in their NIPs. Conversely, just one of the six low-income countries, Uganda, reported a mandatory element. More detailed empirical case studies would be necessary to uncover the policy reasons for the presence or absence of mandates within NIPs. Nonetheless, it may be reasonable to infer that lower-income countries have fewer human and financial resources to undertake, administer, and enforce mandatory immunization, or that programs are less mature and potentially still evolving. Conversely, given the burden of disease in low-income countries and the difficulties that residents thereof sometimes face in accessing healthcare, demand for, and public acceptance of, vaccines may be quite robust, negating the need for mandates.
Fig. 1.
Presence of Mandates by Country Income Level.
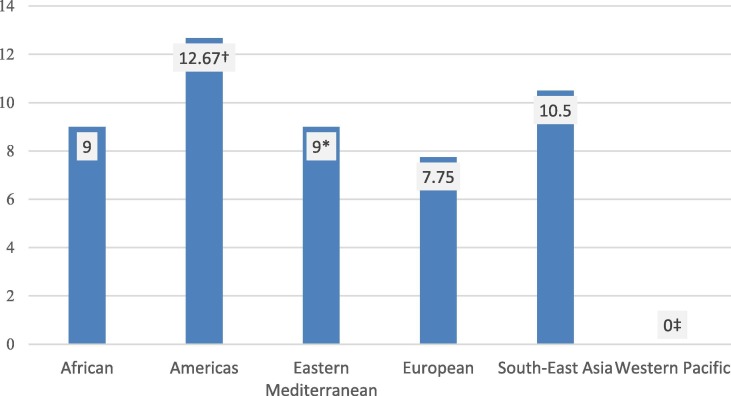
In addition to the economic component, some association was observed between geographic region and the existence of mandates. For two regions – Europe and South-East Asia – no clear association was observed; mandates existed in exactly half of the respondent countries. The one Eastern Mediterranean region respondent (Jordan) reported mandatory immunization, but no regional conclusion can be drawn from a single response; the similarly small sample of two Western Pacific countries (China and Australia) reporting no mandatory immunization is not helpful. However, mandatory programs appeared to be somewhat less common in the African region, with only two of the six responding countries (33%) reporting a mandatory element. Conversely, all five respondent countries from the Americas (100%) reported mandatory immunization.3 This strong response suggests a trend in that region toward mandatory immunization that is not fully explained by income level. Although all the respondent countries in the Americas were high- or upper-middle income, income status alone is probably not a sufficient explanation because just two of six high-income countries outside the Americas reported mandatory immunization. Furthermore, countries in the Americas appear to have much broader or inclusive mandates. Excluding Canada and the USA (due to variation across subnational jurisdictions4 ), respondent countries in the Americas required immunization against an average of 12.7 diseases, with the next broadest mandates found in South-East Asia (10.5 diseases). Respondents from all other regions fell below the total average of 10.2 diseases covered (Fig. 2 ).
Fig. 2.
Average Number of Mandatory Childhood Immunizations by WHO Region. *Includes only one country. †Excludes Canada and the USA due to subnational variation in those countries. ‡There were no Western Pacific countries reporting mandatory immunization in our survey.
All told, there may be something about the approach to immunization, the developmental history of the public health and immunization field, or the politico-legal culture in the Americas that makes mandatory immunization more palatable or feasible as a policy option. Incentivization of healthcare workers, urbanization/remoteness, public health infrastructure, cold chain issues, and public trust of government or health authorities could also play a role, with potentially profound differences between the Americas and other regions. A full explanation for this apparent link would require a more focused empirical case study.
4.1. Vaccines mandated
For countries reporting the presence of a mandatory element in their NIP, we asked which vaccines were required. The responses reveal a great variety of vaccine schedules and a broad spectrum of vaccines that are mandated, with no country mandating all scheduled vaccines (Table 2, Table 3 ). For example, Belgium mandates just a single childhood vaccination (polio), whereas Argentina mandates 16 childhood vaccinations. The average number of mandated vaccines across respondents was 10.2.
Table 2.
Mandatory Childhood Immunizations.
| Country |
BCG |
Tdap1 |
Polio2 |
HIB |
Rota. |
Meas. |
Rubella |
Mumps |
Hep. B |
Menin. |
Pneum. |
HPV |
Yellow |
Other | Totals | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 5 | S | 1 | 5 | S | 1 | 5 | S | 1 | 5 | S | 1 | 5 | S | 1 | 5 | S | 1 | 5 | S | 1 | 5 | S | 1 | 5 | S | 1 | 5 | S | 1 | 5 | S | 1 | 5 | S | 1 | 5 | S | |||
| Albania | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 9 | |||||||||||||||||||||||
| Argentina | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 16 | |||||||||||||||||
| Belgium | ✓ | 1 | |||||||||||||||||||||||||||||||||||||||
| Chile | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 11 | |||||||||||||||||||||
| C d’Ivoire | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 8 | ||||||||||||||||||||||||||||||||
| Indonesia | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ (no age) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 13 | ||||||||||||||||||||||
| Jordan | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 9 | |||||||||||||||
| Kazakh. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 9 | |||||||||||||||||||||||||||
| Latvia | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 14 | |||||||||||||
| Maldives | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 8 | ||||||||||||||||||||||||||||||
| Togo | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 12 | ||||||||||||||||||||||||||||
| Uganda | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 10 | ||||||||||||||||||||||||||||||
| Uruguay | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 12 | |||||||||||||||||
| Totals | 12 | 11 | 13 | 12 | 7 | 12 | 11 | 9 | 11 | 3 | 9 | 8 | 3 | 4 | |||||||||||||||||||||||||||
Note Canada and the USA are excluded from the Table due to significant subnational variability in those countries.
Key The number ‘1′ represents children under one year old. The number ‘5′ represents children one year and older, but less than five years old. The letter ‘S’ represents children, of any age, who are attending school.
The ‘Totals’ in the bottom row refer to the total number of countries which have mandated for at least one age group the vaccine identified in the column.
The ‘Totals’ in the far-right column refer to the total number of vaccines for which each country has erected a mandate. Each column counts as one regardless of whether there is one, two, or three checkmarks.
The ‘Other’ column signals additional vaccines that are mandated (and reported as ‘other vaccines’ in the survey). A single checkmark could refer to one or more other vaccines; the actual number is reflected in the figure in the ‘Totals’ row in the far-right column. For details on these additional vaccines, see Table 3.
Includes DTwP, DTaP, Td.
Includes IPV or OPV.
Table 3.
Other Mandatory Childhood Immunizations.
| Country | Hepatitis A | Influenza | Japanese Encephalitis | Typhoid | Tick-Borne Encephalitis | Varicella |
|---|---|---|---|---|---|---|
| Argentina | 1 year | 6–24 months | – | – | – | 15 months |
| Indonesia | Unspecified Age | – | 9 months to 15 years(Bali only) | Unspecified Age | – | – |
| Latvia | – | 6–24 months | – | – | Unspecified Age | 12–15 months and seven years |
| Uruguay | 15 and 21 months | – | – | – | – | 12 months and five years |
Every mandating country required the polio vaccine, reflecting the historical global burden and long-standing international efforts to eradicate polio [3], [4]. Measles, BCG, and Tdap/DTwP/DTaP/Td (grouped together in our survey due to their nearly ubiquitous concurrent administration) were the second most commonly mandated vaccines, with every mandating jurisdiction (including vaccine-requiring Canadian provinces and all US states) except Belgium reporting their inclusion. Also of note are the HPV and Rotavirus vaccines, which, despite being relatively new, have approximately 50% of countries reporting their inclusion. In addition to the vaccines listed in Table 2, mandates in some countries included hepatitis A, influenza, Japanese encephalitis, typhoid, tick-borne encephalitis, and varicella. Of these, the most common mandatory vaccines were hepatitis A and Japanese encephalitis, with four and two respondent countries respectively mandating their use.
4.2. Populations subject to mandate
Survey participants in countries with mandatory immunization were asked about specific populations subject to mandates (i.e., age [children under 1 and 5 years of age and school-aged children – that is, any childhood immunizations required after entry to school], life events [such as immunizations required prior to daycare or school enrolment], and occupation [healthcare workers, military personnel]). They were also given the opportunity to identify any other population groups subject to mandatory vaccination. Finally, they were asked the year in which mandatory immunization was introduced for that specific population.
Amongst countries with mandatory elements to their NIP, children under one year of age and under five years of age were by far the most frequently subject to mandatory vaccination, with 12 of the 14 respondent countries (86%) reporting specific provisions for these groups. Mandatory immunization upon school enrolment, and for school-aged children were also highly prevalent. For example, eight of the 14 responding countries (57%) reported requiring immunization for school enrolment and for school-aged children. This likely reflects policy recognition of the importance to individual health of immunization relatively early in life, together with the public health objective of facilitating herd immunity [17], particularly in relatively enclosed school environments.
With respect to other targeted populations, seven of the 14 respondent countries (50%) reported mandating vaccinations for healthcare workers. Respondents from six countries (Argentina, Belgium, Chile, Indonesia, Maldives, and Uganda) indicated that they also require immunization for other specific populations. The most common ‘other’ category was pregnant women and/or women of childbearing age, although two countries (Indonesia and Maldives) reported mandating vaccinations (or proof of immunization) for travellers, particularly Hajj and Umrah pilgrims, and for other, unspecified, ‘at-risk populations’. For further specifics on target populations, see Table 4 .
Table 4.
Populations Subject to Mandatory Immunization and Year Implemented (if available).
| Country | Children < 1 Year | Children < 5 Years | School-Age Children | Day-care Enrolment | School Enrolment | Health Care Workers | Military | Other |
|---|---|---|---|---|---|---|---|---|
| Albania | Since 2016 | Since 2016 | Since 2016 | Since 2016 | Since 2016 | Since 2016 | – | – |
| Argentina | Since 1983 | Since 1983 | Since 1983 | – | Since 1983 | Since 1992 | – | Yes |
| Belgium | Since 1966 | – | – | – | – | Yes | Yes | Yes |
| Canada (ON, NB) | – | – | – | – | Yes | – | Yes | – |
| Chile | Yes | Yes | Yes | – | – | – | – | Yes |
| Côte d’Ivoire | Yes | Yes | Yes | Yes | Yes | – | Yes | – |
| Indonesia | Since 1956 | Since 2013 | Since 1997 | – | Since 1997 | Yes | Yes | Yes |
| Jordan | Since 1979 | Since 1979 | Since 1979 | Since 1979 | Since 1979 | Since 2000 | Since 2000 | – |
| Kazakhstan | Yes | Yes | Yes | – | Yes | Yes | Yes | – |
| Latvia | Since 2000 | Since 2000 | – | – | – | Since 2000 | Since 2000 | – |
| Maldives | – | Since 2012 | – | – | – | – | – | Since 2012 |
| Uganda | Since 2017 | Since 2017 | Since 2017 | Since 2017 | Since 2017 | Since 2017 | – | Since 2017 |
| United States | No answers provided; requirements vary by state | |||||||
| Uruguay | Since 1982 | Since 1982 | – | – | – | Since 2005 | – | – |
| Total | 11 | 11 | 8 | 4 | 8 | 9 | 7 | 7 |
Notes
Regarding ‘Other’ Column Argentina: Pregnant and/or child-bearing age women (Td and influenza), the elderly (influenza and pneumococcal), and other at-risk populations (influenza and pneumococcal) have mandated vaccines.
Belgium: Certain educational or daycare staff, certain animal workers or researchers.
Chile: Pregnant woman (dTp), adults over age 65 (pneumococcal).
Indonesia: Pregnant and/or child-bearing age women (Td), travellers (meningococcal), travellers and military personnel to endemic areas (yellow fever), and healthcare workers in private hospitals (Hepatitis B) have mandated vaccines.
Maldives: Pregnant and/or child-bearing age women (unspecified) and travellers (influenza, meningococcal, polio) have mandated vaccines.
Uganda: Pregnant and/or child-bearing age women (tetanus) other at-risk populations (unspecified) have mandated vaccines.
4.3. Exemptions from mandates
In rights-conscious societies, many public services will contain some degree of flexibility to account for differences in individual circumstances. As such, an important aspect of any mandatory NIP will be the availability and scope of exemptions from the mandate. Respondents were therefore asked about the circumstances under which an exemption to any mandatory vaccines will be granted. Exemptions can be categorized broadly into medical and non-medical exemptions. Medical exemptions are granted to individuals who cannot safely receive a vaccine, usually due to suspected or demonstrated allergic reaction to a vaccine component, or in the presence of immunosuppression. Non-medical exemptions include those granted for any other reason; most commonly for religious, philosophical, or other personal objections to immunization [5].
Every respondent country reported allowing exemptions in the event of medical contra-indication (Table 5 ). However, such exemptions are not granted equally across countries. As there is no universally-agreed upon definition of a valid medical exemption for immunization, what constitutes valid grounds in one jurisdiction may not necessarily satisfy another jurisdiction’s requirements (even within the same country) [6]. Further, for any given jurisdiction, the presence or absence of non-medical exemptions may also impact how frequently medical exemptions are requested and granted. For example, in California, USA, the proportion of medical exemptions granted more than doubled (from 0.17% to 0.51%) the year after personal belief exemptions were prohibited and the grounds for medical exemptions were broadened [7].
Table 5.
Mandatory Immunization and Exemptions.
| Country | WHO Region | Income Level |
Exemptions |
|||
|---|---|---|---|---|---|---|
| Medical Contraindication | Philosophical Objection | Religious Objection | Personal Belief | |||
| Albania | European | Upper-Middle | ✓ | |||
| Argentina | Americas | High | ✓ | |||
| Belgium | European | High | ✓ | |||
| Canada | Americas | High | ✓ | ✓ | ✓ | ✓ |
| Chile | Americas | High | ✓ | |||
| Côte d’Ivoire | African | Lower-Middle | ✓ | |||
| Indonesia | S-E Asia | Lower-Middle | ✓ | ✓ | ||
| Jordan | Eastern Med. | Upper-Middle | ✓ | |||
| Kazakhstan | European | Upper-Middle | ✓ | |||
| Latvia | European | High | ✓ | |||
| Maldives | S-E Asia | Upper-Middle | ✓ | |||
| Uganda | African | Low | ✓ | |||
| USA | Americas | High | ✓ | Most states | Most states | |
| Uruguay | Americas | High | ✓ | |||
As shown in Table 5, non-medical exemptions appear far less common in our sample – perhaps unsurprisingly, given that mandatory vaccination is directly undermined by easy access to non-medical exemptions [8]. In our survey, only Canada, Indonesia, and the USA reported allowing exemptions for religious, philosophical, personal, or conscientious objections to vaccination. Again, in the USA, the grounds for exemption vary by state. Although most states allow exemptions based on religious or personal belief, five states5 permit exemptions only for medical contraindication [9].
To discourage the use of non-medical exemptions, some jurisdictions impose additional requirements before such an exemption may be granted. For example, in Ontario, Canada, parents must file a sworn statement of conscience or religious belief with a Medical Officer of Health, and must additionally attend an education session on the benefits and risks of immunization prior to obtaining a non-medical exemption [10]. It is unclear how effective these measures are at reducing the use of non-medical exemptions.
4.4. Sanctions and enforcement for failure to vaccinate
The policy objectives advanced by mandating immunization may be seriously undermined if there are no consequences for failure to comply, and no actual enforcement of the mandate. For reasons of survey length, we did not ask direct questions about enforcement dispositions and practices. However, we did pose questions about penalties for non-compliance (Table 6 ).
Table 6.
Sanctions for Failure to Immunize.
| Country |
Type of Sanction |
||
|---|---|---|---|
| Loss of Access to Services | Fine (Maximum) | Incarceration | |
| Albania | May be denied school entry | ||
| Argentina | 5,000 pesos (US$84) | ||
| Belgium | Sanctions depend on judicial decision; typically a fine. | ||
| Canada | May be denied school entry | ||
| Chile | No sanctions reported or found by authors | ||
| Côte d’Ivoire | No sanctions reported or found by authors | ||
| Indonesia | No sanctions reported or found by authors | ||
| Jordan | May be denied school entry* | ||
| Kazakhstan | No sanctions reported or found by authors | ||
| Latvia | May be denied school entry | ||
| Maldives | May be denied school entry | 3000 rufiyaa (US$194) | |
| Uganda | May be denied school entry | 240,000 shillings (US$65) | Imprisonment for up to 6 months |
| USA | May be denied school entry | ||
| Uruguay | No sanctions reported or found by authors | ||
We were unable to corroborate the sanction for Jordan.
Penalties vary considerably between countries. Most jurisdictions reported relatively benign, non-compelling, or non-existent sanctions. The approaches taken by these countries largely correspond with the Level 3 and Level 4 legislative approaches to immunization proposed by the Sabin Institute [11]; that is, mandatory provisions are prescribed either administratively (e.g., as a requirement for school entry) or by law, but such provisions are not supported by serious sanctions, nor by consistent or strong enforcement of those sanctions [12]. Conversely, some respondent countries reported much more severe sanctions. Four countries – Argentina, Belgium, the Maldives, and Uganda – impose fines for failure to immunize. In Uganda, vaccine refusers may additionally face incarceration for up to 6 months [13]. These countries would likely correspond to Sabin Institute’s Level 5 approaches – that is, mandatory provisions are prescribed by law, and sanctions are imposed for failure to comply.
Again, however, sanctions are distinct from enforcement. Regardless of the nature or severity of sanctions for failure to vaccinate, actual enforcement of the mandate is necessary to make the mandate real. Our preliminary, albeit incomplete, evidence shows that enforcement varies considerably between jurisdictions, and is not always in compliance with statutory instruction. One respondent, for example, stated that although in their jurisdiction, schools are required to ensure that students are immunized, the penalties for not getting vaccinated are “not very strict”. In other countries, enforcement provisions might be ignored except in the case of an imminent epidemic. Our limited data on this issue suggests that significant discretion is exercised in the determination of whether to enforce mandates. This is an important aspect of mandatory immunization that is worthy of further empirical research.
5. Discussion
This study reveals a spectrum of approaches to mandatory immunization. At one end of the spectrum is a very narrow or largely permissive approach. Under this approach, a very small number of vaccines are mandated, or the groups subject to mandatory vaccination is limited, or both. The calculus for setting these very narrow or modest targets in relation to vaccines administered or groups compelled is not clear from the responses given or the instruments examined. This approach could be informed by:
-
•
national desires to exercise sovereignty in favour of more direct adoption of international policies when otherwise seeking to meet international obligations;
-
•
national political ambitions to control specific diseases, and to not expend political or economic capital on broader mandates;
-
•
local disease and cultural conditions that favour a generally permissive or autonomy-privileging approach (i.e., lower social acceptance of vaccination, which would entail expenditure of political capital, or high social acceptance of vaccination, which may negate the need to mandate); or
-
•
acute or persistent supply-side management issues such as shortages of healthcare workers and stock-outs of vaccines (either nationally or locally).
Any one or more of these could be in operation in any given jurisdiction, but determining their presence would require detailed investigation.
In our data, Belgium exemplifies this narrow or largely permissive approach; it mandates just one childhood vaccine – polio – and only for newborns.6 Within Canada, the province of Manitoba previously exemplified this approach; until its 2009 restructuring of provincial public health regulations, Manitoba required children to demonstrate immunity to measles only (via immunization or natural infection) prior to entry into Grade-1.7 [14].
Such a narrow approach may have certain advantages. First, mandating only a few vaccines, instead of many, for a small group of people, instead of a larger group of people, will result in lesser financial (ie, vaccine procurement) and administrative (ie, vaccine delivery and monitoring) burdens on the state. In practice, of course, the financial savings may be modest, especially for countries that publish a relatively inclusive recommended immunization schedule of publicly funded vaccines (as do both Belgium and Manitoba).8 In such circumstances, the financial savings may be insignificant, and unlikely to be the driver behind such policies. A more pertinent advantage of this narrow approach may be the avoidance of perceptions of government coercion. Mandatory immunization is, by its nature, coercive [15]; compelling individuals to receive vaccinations may have unintended negative (political) consequences. Many populations, perhaps especially in fragile states, have legitimate concerns relating to trust in their governments and fear of government officials [16]. Attempts by some countries to implement broader mandatory immunization policies have incited some public backlash and increased attention to negative vaccine messages in the media [8]. Mandatory immunization programmes that do not include sufficiently accessible exemptions may run afoul of religious or other rights. On the other hand, allowing overbroad exemptions may encourage ‘gaming’ within the system [8].
Ultimately, a narrow or permissive approach to mandates may provide governments with a greater ability to take a balanced and flexible approach to immunization. It may offer an avenue for imposing a strong but otherwise gentle ‘nudge’ in relation to diseases considered essential to control given local conditions with only minimal encroachment on individual freedoms (thereby maintaining public support). Such nudge strategies may include public education campaigns and positive, science-based messaging, and they can be more easily revised for the prevailing situation than can legislated mandates.
At the other end of the spectrum is a broad and more inclusive approach to mandates, which requires a relatively large number of vaccinations for a relatively large segment of the population (including specified target groups). As with the narrow approach, this approach was not widely represented in our data. It is perhaps best exemplified by Argentina and Indonesia, which require 16 and 13 childhood vaccinations respectively. Argentina additionally requires vaccines for healthcare workers, women who are pregnant and/or postpartum, and the elderly. Indonesia requires vaccines for healthcare workers, women who are pregnant and/or of child-bearing age, some military personnel, and certain travellers. The advantages and disadvantages to a broad or inclusive approach are roughly the inverse of the narrow or permissive approach. Essentially, it prioritizes prevention through compelled uptake and coverage, while risking public resistance for government infringements – real or perceived – to bodily or religious integrity. This approach may also be more expensive to administer and deliver, not only because of increased procurement costs, but also because of potentially increased monitoring and enforcement costs.
As one might expect, most respondent countries fall between the two ends of the spectrum, though they lean toward the broader or more inclusive approach. It is not clear from the data the extent to which countries falling between these extremes do so as a matter of conscious policy choice. Other shaping factors may be vaccine supply issues, national capacity in relation to program delivery, or constitutional conditions. For example, these rather simple characterizations are insufficient to convey the complexity of the approaches taken by countries like Canada and USA, where healthcare is a constitutionally devolved and fragmented policy field. In such countries, decisions about mandatory immunization are made largely at subnational levels. This within-country diversity of approach toward mandates can be profound, and generates challenges. For example, it can create uncertainty and stress when residents move from one jurisdiction to another with different immunization schedules and mandatory elements [17]. To counteract this uncertainty, a robust national vaccine monitoring system seems advisable. However, to date, no such system exists nationally in either Canada or the USA, although most states do possess local monitoring databases [18], [19].
In addition to the narrow (or largely permissive) and broad (or largely inclusive) continuum, there is a continuum for enforcement which may map loosely but imperfectly on the above continuum. In this regard, approaches on one end can be described as loose (and again permissive), and on the other end as tight (or coercive). The former, exemplified by Belgium and certain Canadian provinces/territories, applies no substantial consequences for failure to vaccinate. In jurisdictions where few or no vaccines are mandated, and few or no target groups are identified for specific treatment, the loose approach would be expected. In jurisdictions falling closer to the broad/inclusive approach to mandates, tighter or more coercive controls may be expected. In our sample, only Uganda legislated the possibility of imprisonment, whereas Argentina, Belgium, the Maldives, and Uganda all imposed fines. Seven countries (Table 6) stipulated the possibility of denial of school entry for children. Although the latter might be characterized as a positive coercive approach (i.e., forming a gateway to public services, with possible work-arounds), the former are negative coercive measures. A further factor in identifying the character of any given jurisdiction is to assess the actual application or enforcement of sanctions, which was beyond the scope of the Project.
6. Conclusions
This project generated data on the status and nature of mandatory vaccination in GNN countries, providing the following insights:
-
•
Obvious diversity occurs in the number of childhood vaccines mandated, ranging from one (Belgium) to 16 (Argentina), with the average being 10.2 per country.
-
•
Every mandating jurisdiction within our survey required vaccination against polio. Measles, BCG, and Tdap/DTwP/DTaP/Td immunizations were the second most commonly mandated.
-
•
Children were by far the most common population group subject to mandatory immunization; healthcare workers were second, mandated in over half of our respondent jurisdictions (nine of 14 jurisdictions = 64%).
-
•
Exemptions from mandates for medical purposes were universal. Non-medical exemptions were far rarer (three of 14 jurisdictions = 21%).
-
•
Sanctions for failure to immunize vary broadly, ranging from no penalty, to loss of access to social services (most particularly admission to school), monetary fines, and incarceration. Further, there appears to be some variance between countries as to how strictly immunization mandates are enforced.
Our findings show the existence of a variety of general approaches to mandatory immunization. This heterogeneity in approaches to NIPs and the treatment of mandates within them speaks volumes. Although differences in disease burdens and healthcare incentives are almost certainly key factors, the differences that exist between countries with respect to legal and healthcare cultures should not be ignored, and these social differences might be more significant shapers of policy choices than actual disease risks and burdens.
Furthermore, although our data suggest that mandatory immunization plays a significant role in these countries, it is not clear whether the trends noticed here (e.g., wide variety, with the majority of systems occupying the broad or inclusive end of the approaches spectrum) would be reflected worldwide. More detailed and coordinated regional case studies of the situation are warranted to offer a global picture. Such investigations could illuminate the extent to which mandatory immunization actually increases immunization rates, an association very difficult to establish [8]. Without robust evidence to support mandates, or differences in policies within mandatory immunization schemes, policymakers are forced to act solely on social, political, or financial grounds, which undermines the notion of evidence-informed policymaking.
Having said that, a very recent study [20] did find slightly higher but statistically significant immunization rates for measles and pertussis vaccines in countries with mandatory immunization (i.e., 3.71% and 2.14% higher, respectively). However, the authors acknowledge the inherent difficulty in accounting for the numerous factors that influence coverage rates. Therefore, these results must be interpreted cautiously. Furthermore, the data and analysis were restricted to 29 European countries (only seven of which mandated vaccination). Research from an international perspective in this area is scarce, likely due to the vast heterogeneity in approaches to mandatory immunization worldwide, which poses challenges for generalizability, and by the absence of funding to undertake a suitably robust multi-jurisdictional project.
We have highlighted some of the key factors that are relevant to shaping and operating a mandatory NIP. These factors are likely to:
-
•
Expand or contract the NIP by including or excluding vaccines, target groups, and exemptions;
-
•
Influence the operation and efficiency of the NIP by allowing or excluding exemptions, and by managing them in certain ways; and
-
•
Bear on the actual immunization rates achieved by the NIP by implementing sanctions (or not), and by enforcing the NIP’s mandates (or not).
Countries with mandatory NIPs – or those considering imposing mandatory elements within their NIP – should consciously, cautiously, and collaboratively consider which approach best reflects the political, legal, and healthcare values of their country, as well as their collective public health objectives and risks.
“All authors attest they meet the ICMJE criteria for authorship.”
CRediT authorship contribution statement
Shawn H.E. Harmon: Formal analysis, Methodology, Formal analysis, Visualization, Writing - original draft. David E. Faour: Formal analysis, Data curation, Writing - original draft, Visualization. Noni E. MacDonald: Conceptualization, Methodology, Investigation, Resources, Writing - review & editing, Project administration. Janice E. Graham: Methodology, Writing - review & editing. Christoph Steffen: Resources, Funding acquisition, Writing - review & editing. Louise Henaff: Resources, Project administration, Writing - review & editing. Stephanie Shendale: Resources, Project administration, Writing - review & editing. The Global NITAG Network 2018 Survey Correspondents: Validation.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors wish to thank the WHO Department of Immunization, Vaccines, and Biologicals for the funding of this research, as well as for providing translations into English for the texts of a number of very technical legal documents. They also wish to thank the GNN member countries who participated in the survey, and the specific respondents who answered our queries.
Footnotes
Funding: This work was supported by the World Health Organization Department of Immunization, Vaccines and Biologicals.
Indeed, representatives from Argentina, China, Zimbabwe, and Germany have informed us that in at least those countries, new vaccine laws have been or are set to be proclaimed into force since the 2018 GNN survey.
Although the mandatory elements in Canada and the USA do vary by subnational jurisdiction.
The sub-national jurisdictions (provinces and states respectively), which have authority over the implementation of the immunization programs within these districts, have resulted in (at times significant) variation across those countries. However, it should be noted that these subnational jurisdictions appear also to have relatively broad mandates – Ontario and New Brunswick require immunization against 9 and 11 infectious diseases, respectively, for school entry, with similar – though varying – numbers for US states.
California, Maine, Mississippi, New York, and West Virginia.
Belgium does also require immunizations for certain other (adult) population groups, but even they tend to be fairly restrictive in nature (for example, requiring tetanus immunization for agricultural workers and animal researchers, as opposed to broader mandates found in other countries such as requiring influenza vaccination for all adults over age 65 or for all pregnant women).
Currently, all vaccinations in Manitoba are voluntary.
A true assessment of the financial cost and saving associated with mandates would, of course, go beyond procurement and delivery, and would also have to take into account the costs of subsequent morbidity, hospitalization, and mortality from vaccine preventable diseases.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2020.09.053.
Appendix A: List of 2018 survey correspondents by GNN country
The authors would like to extend their sincere gratitude to the following individuals and institutions for their invaluable assistance in the preparation of this manuscript:
Albania: Iria Preza, Albanian Institute of Public Health.
Argentina: Daniel Stecher, Comisión Nacional de Inmunización, Ministerio de Salud, Argentina.
Armenia: Armenian National Advisory Committee on Immunization (NACI).
Australia: Hope Peisley, Australian Government Department of Health.
Belgium: Veerle Mertens, Belgian Superior Health Council.
Canada: National Advisory Committee on Immunization (NACI).
Chile: Jaime Cerda. Departamento de Salud Pública, Facultad de Medicina, Pontificia Universidad Católica de Chile; Magdalena Bastías, Departamento de Inmunizaciones, Ministerio de Salud, Chile.
China: Ma Chao, National Immunization Program, Chinese CDC.
Côte d’Ivoire: The Comité National d’Experts Indépendants pour la Vaccination et les vaccins de la Côte d’Ivoire (CNEIV-CI).
Ethiopia: Ethiopian National Immunization Technical Advisory Group (ENITAG).
Germany: Thomas Harder, Robert Koch Institute.
Indonesia: The Indonesian Technical Advisory Group on Immunization (ITAGI).
Jordan: Najwa Khuri-Bulos, University of Jordan.
Kazakstan: Lyazzat Yeraliyeva, Deputy Head of the Kazakhstan Advisory Commission on Immunization (ACI).
Latvia: Dace Zavadska, Rīgas Stradiņa Universitāte.
Maldives: Ahmed Faisal, Indira Gandhi Memorial Hospital.
Nepal: Anindya Sekhar Bose, WHO Nepal.
Sweden: Reference Group for National Vaccination Programmes.
Timor-Leste: National Immunization Technical Advisory Group Timor Leste (NITAG TL).
Togo: Groupe technique consultative pour la vaccination-Togo (GTCV-Togo).
Uganda: Celia Nalwadda, Uganda National Academy of Sciences.
Uruguay: Comisión Asesora de Vacunaciones.
Sri Lanka: Deepa Gamage, Epidemiology Unit, Ministry of Health, Sri Lanka.
Tanzania: Alex Mphuru, Immunization and Vaccine Development (IVD) Program of the Ministry of Health.
UK: Andrew Earnshaw, Public Health England.
USA: Advisory Committee on Immunization Practices (ACIP).
Zimbabwe: Joan Marembo, EPI Manager and Nhamo Gonah, NITAG Chairperson, Department of Paediatrics, Chitungwiza Central Hospital.
Appendix B. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Strategic Advisory Group of Experts on Immunization. 2017 Assessment Report of the Global Vaccine Action Plan; 2017.
- 2.Skinner E. State Vaccination Policies: Requirements and Exemptions for Entering School. LegisBrief. 2017;25:48. [PubMed] [Google Scholar]
- 3.Bhutta Z.A., Orenstein W.A. Scientific declaration on polio eradication. Vaccine. 2013 doi: 10.1016/j.vaccine.2013.04.024. [DOI] [PubMed] [Google Scholar]
- 4.Polio Working Group of the PHAC Committee to Advise on Tropical Medicine and Travel. Statement on Poliovirus and the International Traveller; n.d.
- 5.Simon G.R., Byington C., Diasio C., Edwards A.R., Holmes B., Arauz Boudreau A.D., et al. Medical versus nonmedical immunization exemptions for child care and school attendance. Pediatrics. 2016 doi: 10.1542/peds.2016-2145. [DOI] [PubMed] [Google Scholar]
- 6.Stadlin S., Bednarczyk R.A., Omer S.B. Medical exemptions to school immunization requirements in the United States - Association of state policies with medical exemption rates (2004–2011) J Infect Dis. 2012 doi: 10.1093/infdis/jis436. [DOI] [PubMed] [Google Scholar]
- 7.Delamater P.L., Leslie T.F., Yang Y.T. Letters: Change in medical exemptions from immunization in California after elimination of personal belief exemptions. JAMA - J Am Med Assoc. 2017 doi: 10.1001/jama.2017.9242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MacDonald N.E., Harmon S., Dube E., Steenbeek A., Crowcroft N., Opel D.J., et al. Mandatory infant & childhood immunization: Rationales, issues and knowledge gaps. Vaccine. 2018;36 doi: 10.1016/j.vaccine.2018.08.042. [DOI] [PubMed] [Google Scholar]
- 9.National Conference of State Legislators. States With Religious and Philosophical Exemptions From School Immunization Requirements; 2020. https://www.ncsl.org/research/health/school-immunization-exemption-state-laws.aspx.
- 10.Government of Ontario. Immunization of school pupils act. Canada; 1990.
- 11.SABIN Vaccine Institute. Legislative Landscape Review: Legislative Approaches to Immunization Across the European Region; 2018.
- 12.Trumbo S.P., Silver D., Domenti O., Gasoyan H., Paatashvili E., Gellin B.G., et al. Strengthening legal frameworks for vaccination: The experiences of Armenia, Georgia, and Moldova. Vaccine. 2018 doi: 10.1016/j.vaccine.2018.10.069. [DOI] [PubMed] [Google Scholar]
- 13.Immunisation Act, 2017. Uganda; n.d.
- 14.Government of Manitoba. Public Health Act, Diseases and Dead Bodies Regulation; n.d.
- 15.Lantos J.D., Jackson M.A., Opel D.J., Marcuse E.K., Myers A.L., Connelly B.L. Controversies in Vaccine Mandates. Curr Probl Pediatr Adolesc Health Care. 2010 doi: 10.1016/j.cppeds.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. Global Vaccine Safety Blueprint 2.0 (Draft 1); 2019.
- 17.MacDonald N.E., Bortolussi R., Finlay J., McDonald J.C., Onyett H., Robinson J.L., et al. A harmonized immunization schedule for Canada: A call to action. Paediatr Child Health (Oxford) 2011 doi: 10.1093/pch/16.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Laroche J.A., Diniz A.J. Immunisation registers in Canada: Progress made, current situation, and challenges for the future. Eurosurveillance. 2012 doi: 10.2807/ese.17.17.20158-en. [DOI] [PubMed] [Google Scholar]
- 19.Murthy N., Rodgers L., Pabst L., Fiebelkorn A.P., Ng T. Progress in childhood vaccination data in immunization information systems — United States, 2013–2016. Morb Mortal Wkly Rep. 2017 doi: 10.15585/mmwr.mm6643a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vaz O.M., Ellingson M.K., Weiss P., Jenness S.M., Bardají A., Bednarczyk R.A., et al. Mandatory Vaccination in Europe. Pediatrics. 2020 doi: 10.1542/peds.2019-0620. e20190620. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.