Abstract
The coronavirus disease (COVID-19) pandemic has affected nearly all nations globally. The highly contagious nature of the disease puts the healthcare workers at high risk of acquiring infection, especially while handling airway and performing aerosol-generating procedures. The Indian Society of Critical Care Medicine, through this position paper, aims to provide guidance for safe airway management to all healthcare workers dealing with airway in COVID-19 patients.
How to cite this article
Praveen Kumar G, Kulkarni AP, Govil D, Dixit SB, Chaudhry D, Samavedam S, et al. Airway Management and Related Procedures in Critically Ill COVID-19 Patients: Position Statement of the Indian Society of Critical Care Medicine. Indian J Crit Care Med 2020;24(8):630–642.
Keywords: Aerosol, Airway, COVID-19, Droplets, Extubation, Intubation, Nebulization, Tracheostomy, Videolaryngoscopy
Introduction
The coronavirus disease (COVID-19) pandemic has affected over 210 countries worldwide, infecting more than 7 million people.1 Although COVID-19 is multisystem disease, it predominantly affects the lungs, and up to 19% of patients affected develop severe acute respiratory illness (SARI) leading to hypoxic respiratory failure. Of these 5 to 15% of patients need intensive care unit (ICU) admission and invasive mechanical ventilation.2 This translates in to a large number of patients needing emergent airway management. The highly contagious nature of the disease puts the healthcare workers (HCWs) at high risk of acquiring infection while performing aerosol-generating procedures (AGPs) and when in close contact with airway. The dictum “primum non nocere” needs be adhered to as always. However, in these altered circumstances, we also need to protect the HCWs, a precious resource. This is because infection to the HCWs poses a “triple threat” in these circumstances: they cannot continue work and instead become added burden to the overwhelmed healthcare system and pose a hazard by being source of infection to coworkers in particular and community members in general.3
This position paper is meant to be a guide to all HCWs involved in airway management and related procedures in COVID-19 patients. The document only serves as a reference guide and does not intend to replace clinical knowledge or skills of the clinician at the bedside. Implementation of recommendations made in the statement may need to be adapted per the available local resources and expertise. The indications for various airway-related procedures and the ethical issues concerning them is beyond the scope of this document.
Methodology for Development of Position Statement
A team of clinicians experienced in airway management and actively involved in management of COVID-19 patients in the ICU was constituted. All existing literature from January 2020 to May 2020 related to COVID-19 was reviewed. The literature regarding other infectious diseases, especially involving transmission, protection, and airway for severe acute respiratory syndrome (SARS), middle east respiratory syndrome (MERS), and Ebola, was also reviewed. Literature was reviewed in PubMed, Medline, Embase, and in all COVID-19 resource centers of various journals. The key words used for the search included airway, intubation, extubation, videolaryngoscopy, aerosol, droplets, tracheostomy, nebulization, and COVID-19. After the literature review, the experts met and discussed on virtual platforms and through e-mail communications, and all recommendations were debated and discussed extensively before the final recommendations were made. Due to lack of robust literature, recommendations were derived by expert opinion and consensus. Summary of recommendations in shown in Table 1.
Table 1.
Airway management and related procedures in critically ill COVID-19 patients: A summary of recommendations
| 1. | Environment |
| We recommend that all COVID-19 patients should be treated in negative pressure rooms. | |
| We recommend that a minimum of 12 air exchanges per hour should be maintained to dissipate aerosols. | |
| We recommend against the practice of using dedicated rooms for airway procedure. | |
| 2. | Personal protective equipment (PPE) |
| We recommend that all aerosol-generating procedures should be performed with full PPE. | |
| We recommend the use of PAPRs over N95 respirators for aerosol-generating procedures, whenever available. | |
| We recommend using a double pair of gloves for all aerosol-generating procedures. | |
| 3. | Airway management team of HCWs |
| We recommend that each ICU should have an airway team, and should have an intensivist or anesthesiologist who is trained in airway management. | |
| We recommend that number of people in the airway team should not exceed three. | |
| We strongly recommend against having HCWs with comorbid conditions, on immunosuppressive therapy, those aged older than 60 years, and pregnant females as part of airway team. | |
| 4. | Disposable vs reusable airway equipment |
| We recommend use of single-use disposable airway equipment. | |
| We strongly recommend laying down of local protocols for transport and disinfection of equipment for institutions using reusable equipment. | |
| 5. | Barrier devices |
| We recommend use of a barrier device for aerosol-generating procedure. | |
| We do not recommend for or against any specific barrier device. We recommend that the team uses the barrier device which it is familiar with. | |
| We recommend removal of barrier device if it makes airway management difficult. | |
| 6. | Preparation: Airway cart |
| We recommend that every intensive care unit should have an airway cart. | |
| We recommend that the airway cart should be inspected by a senior airway manager, using a checklist, during every shift. | |
| 7. | Preparation: Assessment of airway |
| We recommend use of MACOCHA or HEAVEN criteria for predicting difficult airway. | |
| For teams, which are unfamiliar with these criteria, we recommend that they use criteria, which the team is familiar with. | |
| 8. | Preoxygenation |
| We recommend that all patients should be preoxygenated for 3–5 minutes with 100% oxygen. | |
| We recommend a face mask with tight-fitting seal for preoxygenation. | |
| We recommend use of a viral filter between the mask and the respirator. | |
| We recommend against the use of high-flow nasal cannula oxygen or high-flow oxygen with reservoir bags for preoxygenation | |
| We recommend placing an oxygen mask, over HFNC cannula, if the patient is already on HFNC, and stopping HFNC oxygen flow, before removal of mask for intubation. | |
| 9. | Rapid sequence and delayed sequence intubation |
| We recommend rapid sequence intubation for all COVID-19 patients. | |
| In agitated and uncooperative patient, we recommend delayed sequence intubation. | |
| We recommend higher doses of neuromuscular blocking drugs for rapid achievement of neuromuscular paralysis. | |
| 10. | Oxygenation during apnea and manual ventilation |
| We recommend against the use of apneic oxygenation using HFNC and manual ventilation in patients without severe hypoxia. | |
| In patients with severe hypoxia, if manual ventilation is needed, a two-handed C and E approach is recommended to obtain a tight seal with the face mask. | |
| We recommend use of second-generation supraglottic airway with filter for ventilation during apnea, whenever available. | |
| We recommend use of small tidal volumes in patients requiring manual ventilation. | |
| We strongly recommend against use of high-flow nasal oxygenation for apneic oxygenation. | |
| 11. | Conventional vs videolaryngoscopy |
| We recommend the use of videolaryngoscope over conventional laryngoscope for TI. | |
| We do not recommend for or against any specific videolaryngoscope. | |
| We recommend against the use of videolaryngoscopes with integrated oxygen channels. | |
| We recommend against the first time use of videolaryngoscopes in COVID-19 patients if the operator is not experienced in its use. | |
| We recommend the use of bougie with preloaded endotracheal tube for intubation. | |
| 12. | Use of endotracheal tube clamps |
| We recommend use of endotracheal tube clamps. | |
| We recommend that the clamps be removed only after the inflation of endotracheal tube cuff and the endotracheal tube is connected to the ventilator. | |
| 13. | Confirmation of correct placement of endotracheal tube |
| We recommend the use of capnography for confirmation of tube position. | |
| We recommend against auscultation method as only method for confirmation of tube position. | |
| We do not recommend for or against the use of ultrasonography for confirmation of tube position. An experienced person may use it, but capnographic confirmation is a must for all patients. | |
| 14. | Unanticipated difficult intubation |
| We recommend early use of second-generation supraglottic airway for unanticipated difficult airway. | |
| We recommend cricothyroidotomy by a scalpel and bougie technique. | |
| We recommend against the practice of apneic oxygenation during cricothyroidotomy or during bronchoscopy-aided intubation. | |
| We recommend against the use of percutaneous tracheostomy in unanticipated difficult airway, unless expertise is available and this is deemed life-saving. | |
| 15. | Tracheal extubation |
| We recommend the use of barrier device during extubation. | |
| We recommend against the use of T-piece trials to assess readiness for extubation. | |
| We strongly recommend against the practice of inducing cough to assess readiness for extubation. | |
| We recommend against performance of leak test. | |
| We do not recommend for or against the use of sedatives before extubation. | |
| We recommend against use of routine nebulization after extubation. | |
| We recommend the use of surgical facemask over the patient face, immediately after extubation. | |
| 16. | Percutaneous tracheostomy |
| We recommend against use of percutaneous tracheostomy in nonventilated patients. | |
| We recommend the use of sedation and neuromuscular paralysis during tracheostomy. | |
| We recommend ultrasound over bronchoscopy-aided percutaneous tracheostomy to minimize exposure to HCWs. | |
| 17. | Flexible fiberoptic bronchoscopy |
| We recommend against use of bronchoscopy in nonventilated patients for diagnostic purposes. | |
| When indicated, we recommend that endotracheal tube be clamped and ventilation be paused before insertion of bronchoscope. | |
| We recommend for insertion of bronchoscope through suction port of catheter mount over the main channel of catheter mount. | |
| 18. | Nebulization in COVID-19 patients |
| We recommend against the use of routine nebulization in COVID-19 patients. | |
| We recommend for the use pMDI or DPI in spontaneously breathing, cooperative patient. | |
| We recommend against the use of jet nebulizers in patients where pMDI or DPI can be used. | |
| We recommend the use of mouthpiece over mask for nebulization, when jet nebulizer is used. We recommend use of viral filter on the expiratory port of mouthpiece. We recommend use of viral filter on the expiratory port of mouthpiece. | |
| We recommend against the use of jet nebulizer in ventilated patient. | |
| We recommend the use of mesh nebulizer in ventilated patient. | |
| We recommend that the mesh nebulizer be placed at the Y piece, with filter placed between Y-piece and nebulizer. | |
| 19 | Airway suction in ventilated COVID-19 patients |
| We strongly recommend against the use of open suction. | |
| We recommend the use of closed in-line suction device for airway toileting. | |
| 20. | Airway management during cardiopulmonary resuscitation |
| We recommend early use of advanced airway devices during CPR. | |
| We recommend brief interruption in chest compression to secure the airway with an advanced airway device. | |
| We recommend use of ICU ventilators for ventilation during CPR instead of manual ventilation. |
Understanding the Disease Transmission
COVID-19 is highly contagious, and it has been shown that without proper isolation precautions and physical distancing, every infected person might infect two to three other individuals in general population.4 The risk to the HCWs is increased multifold due to close contact with the infected patient and high-risk procedures performed. Nosocomial transmission of virus to HCWs is a serious problem, and a retrospective analysis revealed that more than 3.8% of all infections was among healthcare personnel.4,5 The main mechanism of transmission of infection to the HCWs is through droplets and aerosols from patient's respiratory tract, especially to those within 2 meters of the patient. The HCWs may also get infected through contact with fomites and linen infected with droplets. The virus remains viable in aerosol for up to 3 hours and for longer periods on surfaces surrounding the patients, thereby increasing the risk of transmission.6
High-risk AGPs
It is known that infectious droplets produced during AGPs differ in droplet size, infectivity, and spread when compared to those produced by natural means, such as cough, sneeze, or speech.7 Airway management increases the risk of transmission of virus to HCWs due to multiple reasons (Box 1). High-risk AGPs performed during airway management in the ICU include preoxygenation (high flow oxygen prior to intubation), tracheal intubation (TI) and extubation, open suction of airway, bag and mask ventilation (especially before TI), manipulation of noninvasive ventilation (NIV) mask and oxygen mask, nebulization, tracheostomy, and cricothyroidotomy. Other interventions like insertion and removal of supraglottic airway devices, bronchoscopy, high flow nasal cannula oxygen also generate aerosols, but to a less extent as compared to TI. The generation of aerosols during chest compressions and defibrillation, although likely, has not been conclusively proven.7–9 However, the viral load of individual patient is variable; thus, these procedures should be considered equally infectious, and same degree of caution should be exercised. Bedside methods to reduce the risk of aerosol generation would be discussed with each individual procedure.
Box 1.
Factors contributing to increased risk of transmission of aerosols during airway management
| 1. HCWs very close to patient's airway or in close contact with each other (if one of them is infected, but asymptomatic). |
| 2. Uncooperative patient due to hypoxia or altered sensorium. |
| 3. Need to remove the surgical or protective mask. |
| 4. Increased risk of coughing due to disease and airway handling and incomplete neuromuscular paralysis. |
Minimizing Risks and Ensuring Safety: General Principles
Environment
All patients with COVID-19 disease should be treated in a negative-pressure room. Care of patients in positive-pressure rooms should be avoided. During the pandemic, the negative-pressure rooms might become scarce, and these rooms can be used for AGPs, especially for high-risk procedures. Certain hospitals might have dedicated rooms for endotracheal intubation, but in view of risks involved in transporting hypoxic and potentially infective patients, this should be avoided.
The time needed for dissipation of aerosol also depends on the number of air exchanges in the room, and it should be maintained above 12 exchanges per hour. With this, the aerosol is cleared with 99% efficiency in <30 minutes.10 In the real world, negative-pressure rooms are finite and therefore not many will be available, as the number of patients increase and therefore airway procedures may need to be performed in compromised environment, as the resources become depleted. This may lead to increased risk of transmission of infection to HCWs.
Recommendations
We recommend that all COVID-19 patients should be preferably treated in negative-pressure rooms.
We recommend that a minimum of 12 air exchanges per hour should be maintained to dissipate aerosols.
We recommend against the practice of using dedicated rooms for airway procedure.
Personal Protective Equipment (PPE)
If possible, minimum number of HCWs should be present during AGPs. All HCWs present near the patient should wear PPEs in the form of head cover or hood, eye protection in the wrap around goggles with shield, N95 respirator or higher level respirators (FFP2 standard/powered air-purifying respirator (PAPR), neck protection, gowns that meet a minimum standards of Association for Advancement of Medical Instrumentation level 2, shoe covers, and minimum of double pair of gloves—overlapping the gown sleeve to protect the wrists while handling the airway.11 Use of double pairs of gloves has been shown to reduce the risk of transmission of infectious particles.11 An additional pair of gloves will also prevent unnecessary soiling of the PPE and thereby wastage of scarce resources.
Powered air-purifying respirators have higher filtration efficiency when compared to N95 respirators and should be used whenever available.12 The PAPRs also do not require prior fit testing and are more comfortable, especially when performing high-risk procedures, as additional shield is not required. When PAPRs are used, special care should be taken while doffing and donning, and proper decontamination should be ensured to reduce the risks associated with reuse. In resource-limited settings where appropriate gowns are not available, it is prudent to use double-layered clothing to reduce the risk of transmission.
Recommendations
We recommend that all AGPs should be performed with full PPE.
We recommend the use of PAPRs over N95 respirators for AGPs, whenever available.
We recommend using a double pair of gloves for all AGPs.
Airway Management Team of HCWs
High-risk AGPs such as TI should be performed by the most experienced clinician in the team. This would minimize the number of attempts at intubation and improve the first-pass success rate. Airway team should be formed in each ICU, and the team should comprise of at least one intensivist or anesthesiologist with expertise in airway management. Training of junior team members should be carried out by simulation on a regular basis, with full donning of PPE, to handle airway contingencies in case of the absence of senior experienced personnel.
Healthcare workers with comorbid conditions, that is chronic kidney disease, cardiac illness, diabetes and hypertension, chronic obstructive pulmonary disease, malignancy, on immunosuppressive therapy, pregnant females, and those aged older than 60 years are considered to be at high risk of contracting the disease and should not be part of airway management team.13
Intubation team generally consists of four to six members, all doing designated tasks.14 This might increase the risks of transmission. In patients with known or suspected COVID-19 disease, the number of people handling the airway should be restricted to three. If additional members are needed, they should ideally remain outside the room, where the patient is managed and enter the room only in special emergent circumstances, after donning full PPE. Team members should be trained in effective closed loop communication, to avoid distress, while performing high-risk procedure and during unanticipated difficulties.
Recommendations
We recommend that each ICU should have an airway team and should have an intensivist or anesthesiologist who is trained in airway management.
We recommend that number of people in the airway team should not exceed three.
We strongly recommend against having HCWs with comorbid conditions, on immunosuppressive therapy, those with aged older than 60 years, and pregnant females as part of the airway team.
Disposable vs Reusable Airway Equipment
It is prudent to use disposable (single use) equipment for airway management considering the risk involved in sterilization and disinfection and also transmission of virus while transporting the equipment. However, this might not be cost effective, and resources such as videolaryngoscopes and bronchoscopes might become scarce as the pandemic grows. Therefore, every institution should formulate local protocols for transport of the used equipment to the central sterile services department (CSSD) and its storage there. It is advisable to have a container filled with 1% sodium hypochlorite and 2% glutaraldehyde within the ICU so that the equipment can directly be placed in the disinfectant before initiating appropriate sterilization.
Recommendations
We recommend use of single-use disposable airway equipment.
We strongly recommend laying down of local protocols for transport and disinfection of equipment for institutions using reusable equipment.
Barrier Devices
Creation of a physical barrier between the patient and person handling the airway has been explored as a method to reduce exposure to aerosols in COVID-19 patients. Multiple such devices have been tried since the beginning of the pandemic.15–17
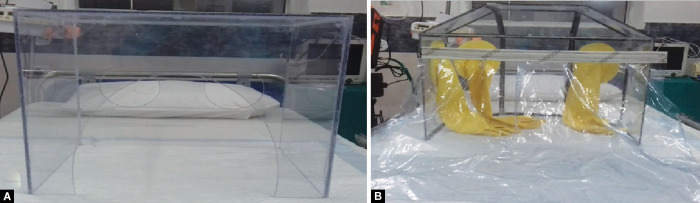
Canelli et al. have described a barrier enclosure device called as aerosol box.17 It is a transparent plastic cube that covers the patient's face with two circular openings through which the clinicians can place his hands and perform the procedure. The major drawback for use of aerosol box is restriction of the hand movements of the operator, thus potentially making airway management more difficult. To overcome this restriction, it is suggested to modify the chamber with one large rectangular opening end to end in the head end of the cube rather than two openings in the sides. But this might increase the risk of transmission of infection. Also, the device has been criticized, as it only redirects the aerosols away toward the foot end of the patient and might still infect the other team members in the room. The device has a potential to increase the difficulty in TI, especially in emergent situations. Innovations to the aerosol chamber have been described. One such innovation includes use of protective long-sleeve gloves in the barrier device with plastic drapes to further reduce transmission. Another innovation suggested is putting of mobile flaps over the foot end of box (Fig. 1).
Figs 1A and B.
Modifications to the aerosol box. (A) Aerosol box; (B) Additional of mobile flaps on the foot end and long sleeve gloves over the holes
The other barrier device described is use of simple plastic drapes covering the face and torso of the patient. While single plastic drape over the patient is much easier to apply, a triple-panel plastic drape technique has been shown to minimize aerosol transmission. In this technique, one drape is placed below the patients head, second covering neck and chest, and third overhead drape with as sticky edge at level of mid sternum.15 Such extensive draping of the patient might cause distress to the patient and increase agitation, when they are awake before intubation (administration of drugs), and therefore complicate airway management.
A portable negative flow isolation chamber was described by Cubillos et al.16 It is a cubical tube frame measuring 60 × 60 × 60 cm, covered by transparent plastic. There are ports for oxygen and suction (to create negative pressure) on the side. The central bar in the middle allows placement of hooks on which equipment can be attached. The prototype is designed to minimize the risk of aerosol, and it can be customized according to the needs and local expertise (Figs 2 and 3).
Figs 2A to C.
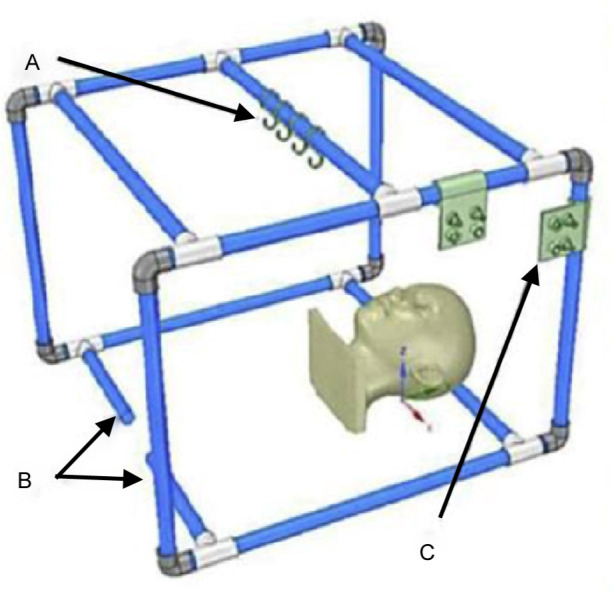
Multipurpose portable negative airflow protection chamber. (A) Hooks to hang airway equipment; (B) Stabilizing tubes to adjust size; (C) Oxygen and nebulizer ports
Fig. 3.

Multipurpose portable negative airflow protection chamber with manikin and equipment inside
In resource-limited settings, and while handling airway outside the ICU, barrier devices might not be available. In such situations, applying plastic drapes over the bed railings is an easy way to minimize risks (Fig. 4)
Figs 4A and B.
(A) Plastic drapes over the railings covering the patient; (B) Bag and mask through the plastic drapes
Albeit multiple such devices have been described, none of them have been proven to reduce transmission of aerosols. Nonfamiliarity with the device might make handling of airway much more difficult, and training by simulation should be done on a regular basis. The authors do not recommend for or against the use of any such device, and the airway team should use the device they are familiar with. In emergent situations, should the airway management become more difficult, the airway manager should not hesitate to remove the device altogether to secure the airway. During TI, these devices will get contaminated and appropriate decontamination protocols should be developed and practiced.
Recommendations
We recommend use of a barrier device for AGP.
We do not recommend for or against any specific barrier device. We recommend that the team uses the barrier device which it is familiar.
We recommend removal of barrier device if it makes airway management difficult.
Principles of TI of COVID-19 Patient
Preparation: Airway Cart
A dedicated COVID-19 airway cart should be prepared and checked by a senior airway manager, using a checklist, at the time of every change of shift. It should contain all essential equipment necessary for intubation and emergency cricothyroidotomy (Box 2). A cardiac arrest cart or resuscitation cart should always be kept just outside the room where the patient is being managed.
Box 2.
COVID-19 airway cart
| 1. Macintosh laryngoscope handles (2) with appropriate size blades (2) |
| 2. Videolaryngoscope, preferably with separate screen |
| 3. Videolaryngoscope with macintosh blade (appropriate sizes) |
| 4. Second-generation supraglottic airway devices (appropriate sizes) such as Proseal or I-gel |
| 5. Endotracheal tubes (appropriate sizes) |
| 6. Oropharyngeal airway (appropriate sizes) |
| 7. Nasopharyngeal airway (appropriate sizes) |
| 8. Tube exchanger/bougie and stylet |
| 9. Transparent face mask |
| 10. AMBU bag or Mapleson circuit |
| 11. Cricothyroidotomy kit including scalpel and bougie |
| 12. Endotracheal tube clamps |
| 13. Nasal oxygen cannula |
| 14. Closed suction catheter system |
| 15. Airway filters (minimum 2) |
| 16. 10 mL syringe for checking the cuff and inflation after intubation |
| 17. Tube ties |
| 18. Lubricant gel |
| 19. Nasogastric tube |
| 20. Surgical gloves (all sizes) |
| 21. Barrier devices: Plastic drapes or transparent aerosol containment chamber or COVID box |
| 22. Unanticipated difficult airway management flow chart |
Recommendations
We recommend that every ICU should have an airway cart.
We recommend that the airway cart should be inspected by a senior airway manager, using a checklist, during every shift.
Preparation: Assessment of Airway
Airway assessment should be performed for every patient and should be clearly documented and communicated between clinicians in every shift. This would help in preparing individualized airway strategy for the patient. MACOCHA score (Box 3) or HEAVEN criteria (Box 4) are easy and reliable methods for assessing difficulty in intubation in ICU.18,19 If the treating team is not familiar with these scores or criteria, they can use any other scoring system for predicting difficult airway, with which they are familiar.
Box 3.
MACOCHA score
| Components | Score |
|---|---|
| Mallampatti class 3 or 4 | 5 |
| Obstructive sleep apnea | 2 |
| Cervical spine movement | 1 |
| Mouth opening | 1 |
| Comatose patient | 1 |
| Hypoxemia (SpO2 < 80%) | 1 |
| Non-anesthesiologist intubator | 1 |
MACOCHA score > 2 predicts a difficult airway
Box 4.
HEAVEN criteria for predicting difficulties in emergency intubation
| Hypoxemia—≤93% at the time of initial laryngoscopy |
| Extremes of size—pediatric patient ≤8 years of age or clinical obesity |
| Anatomic challenge—any structural abnormality that is anticipated to limit laryngoscopic view |
| Vomit/blood/fluid—clinically significant fluid noted in the pharynx or hypopharynx prior to laryngoscopy |
| Exsanguination—suspected anemia raising concerns about limiting safe apnea times |
| Neck mobility issues—limited cervical range of motion |
Presence of each of HEAVEN criteria increases the risk of difficult laryngoscopy and intubation (except hypoxia and exsanguination)
Recommendations
We recommend use of MACOCHA or HEAVEN criteria for predicting difficult airway.
For teams that are unfamiliar with these criteria, we recommend that they use criteria that the team is familiar with.
Preparation: Intubation Team
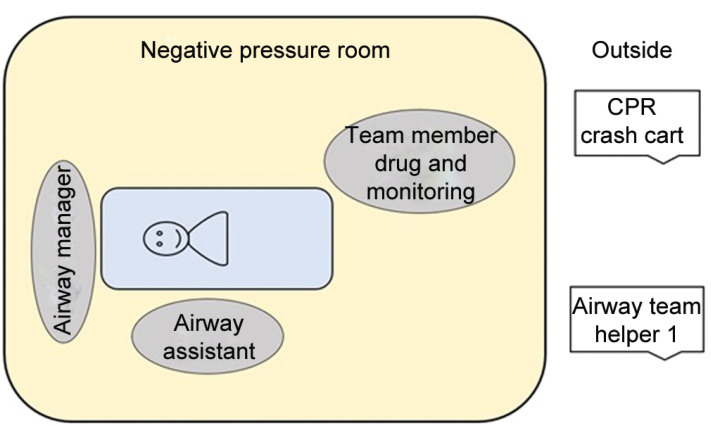
The number of team members inside the intubation room should be restricted to 3. The senior most airway manager should be on the head end of the patient. The second operator, usually designated as airway assistant, should be on one side of the patient. The third team member is the person who administers drugs and monitors the vitals of the patients. One more team member, called the runner, should stand immediately outside the room for getting additional equipment or help (Fig. 5).
Fig. 5.
Airway team for endotracheal intubation
Preparation: Airway Plan
All the team members should be familiar with the airway management strategy for the patient and the trigger for moving from one plan to the next (such as use of bag and mask ventilation or supraglottic airway and emergency cricothyroidotomy). Urgent intubation is best avoided and the team should have adequate time to discuss airway plan and don protective gear for intubation.
Preoxygenation
In nonemergent situation, all patients should be preoxygenated for a period of 3 to 5 minutes. Preoxygenation should be done with face mask with tight-fitting seal connected to the ventilator or manual respirator. Bag and mask ventilation increases the risk of contamination and should preferably be avoided. In non-COVID-19 patients, noninvasive ventilation is commonly used for preoxygenation. This, however, is likely to generate high amounts of aerosol. Therefore, its use should be reserved for patients with severe hypoxia.20 A viral filter should be attached directly to the face mask or as a connection with closed suction unit (Fig. 6). High-flow oxygen with nonrebreathing masks and reservoir bags are not recommended due to increased risk of aerosol generation and suboptimal preoxygenation. A well-fitted high-flow nasal cannula (HFNC) oxygen has shown to produce less aerosols when compared to coughing in experimental trials.21 Nevertheless, these are only experimental studies. As stated previously, viral load of patients could vary, and therefore high-flow nasal cannula cannot be recommended for preoxygenation in all COVID-19 patients. However, if the patient is previously on high flow nasal oxygen, it can be continued with a surgical face mask covering the patients face. High-flow nasal cannula oxygen should be stopped before the face mask is removed and the team takes the position for intubation. If the team plans to use either NIV or HFNC, it safer to do so in patients being managed in negative-pressure rooms. If a barrier device is used, it should be placed before initiating preoxygenation. Placement of a barrier device over an awake patient might increase agitation, and the patient should be clearly explained about the need for the device before its placement.
Fig. 6.
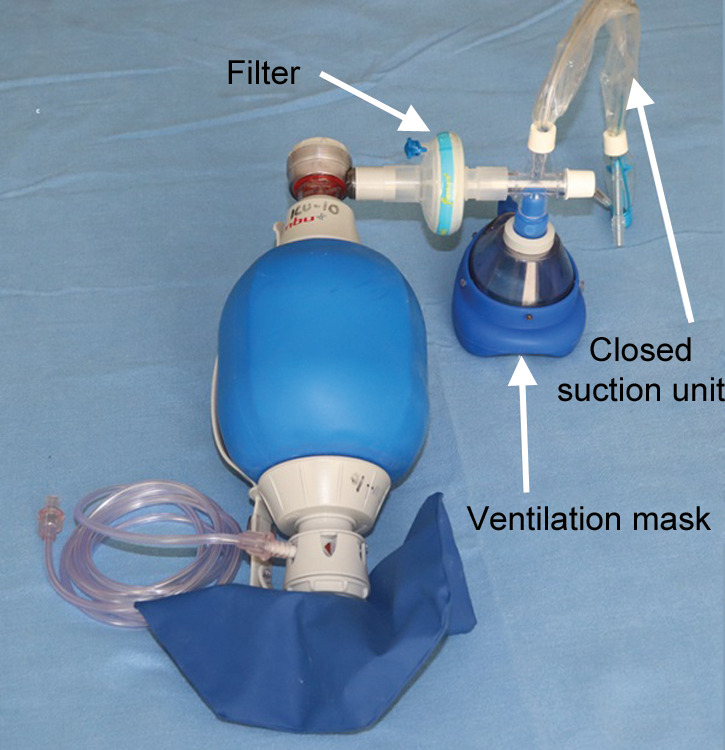
Bag and mask assembly with filter and closed suction
Recommendations
We recommend that all patients should be preoxygenated for 3–5 minutes with 100% oxygen.
We recommend a face mask with tight-fitting seal for preoxygenation.
We recommend use of a viral filter between the mask and the respirator.
We recommend against the use of HFNC oxygen or high-flow oxygen with reservoir bags for preoxygenation
We recommend placing an oxygen mask, over HFNC cannula, if the patient is already on HFNC, and stopping HFNC Oxygen flow, before removal of mask for intubation.
Rapid Sequence and Delayed Sequence Intubation
Rapid sequence intubation should be the default choice for TI. Cricoid pressure can be considered but if applied too early can precipitate cough. Also, it should be withdrawn if difficulty is encountered during intubation. In agitated and uncooperative patients, delayed sequence intubation can be considered. A sedative, mostly Ketamine at a dose of 0.5 to 1 mg/kg body weight, is used to reduce agitation and maintain spontaneous respiration. It helps in adequate preoxygenation and positioning of the patient and reduces combativeness.22 Use of a sedative can also help placement of a barrier device before preoxygenation.
Propofol, etomidate, or ketamine can be used for induction, based on the hemodynamic status of the patient. Rocuronium at a dose of 1.2 mg/kg or Succinyl choline at a dose of 1.5 mg/kg should be used for neuromuscular blockade, as high doses enable rapid achievement of neuromuscular blockade thereby preventing coughing and aerosol generation. If succinyl choline is used, it should be followed by a nondepolarizing muscle relaxant once TI is complete.
Recommendations
We recommend rapid sequence intubation for all COVID-19 patients.
In agitated and uncooperative patient, we recommend delayed sequence intubation.
We recommend higher doses of neuromuscular blocking drugs for rapid achievement of neuromuscular paralysis.
Oxygenation during Apnea and Manual Ventilation
In severely hypoxic COVID-19 patients, it is prudent to minimize the period of apnea. However, if the patient's condition allows, complete apnea, without bag and mask ventilation, is preferred. Endotracheal intubation should be performed once adequate neuromuscular blockade has occurred. Patients with severe hypoxia might not tolerate even short durations of apnea and need manual ventilation during this period of apnea, produced due to administration of neuromuscular blocking drugs. In such patients, once the neuromuscular blocking agent is administered, a tight seal of the face mask should be achieved. A filter should always be placed between the mask and the circuit. Two-handed grip using C and E technique should be preferred over one-handed C and E technique to prevent leaks (Fig. 7). A two-handed V and E grip can also be used based on the comfort of the airway manager. Small tidal volume breaths should be delivered by the airway assistant. If the patient is connected to ventilator through a circle system, disconnection from the ventilator and connecting to a manual respirator might increase the risk of aerosol generation, and risks involved with such an approach should be kept in mind. A second-generation supraglottic airway should be considered for ventilation during apnea in place of bag and mask ventilation. A filter should be inserted over the supraglottic airway before commencing ventilation. Properly inserted second-generation supraglottic airways (such as ProSeal LMA, Supreme LMA, i-gel, SLIPA, and Laryngeal Tube) reduces exposure to aerosols and eases ventilation.
Fig. 7.
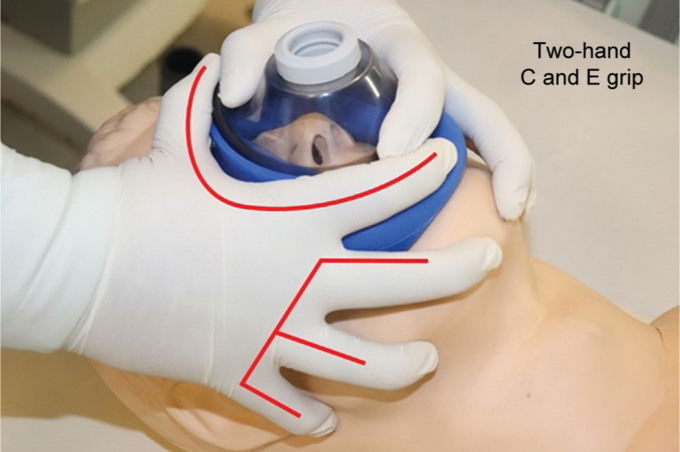
Two-hand C and E technique for complete seal
High-flow nasal cannula oxygenation should not be used (if it was not being used before) for apneic oxygenation due to risks involved to the staff.
Recommendations
We recommend against the use of apneic oxygenation using HFNC and manual ventilation in patients without severe hypoxia.
In patients with severe hypoxia, if manual ventilation is needed, a two-handed C and E approach is recommended to obtain a tight seal with the face mask.
We recommend use of second-generation supraglottic airway with filter for ventilation during apnea whenever available.
We recommend use of small tidal volumes in patients requiring manual ventilation.
We strongly recommend against use of HFNC for apneic oxygenation.
Conventional vs Videolaryngoscopy
When an experienced operator familiar with videolaryngoscope use is available, videolaryngoscope should be preferred over conventional laryngoscope for TI. Videolaryngoscope offers multiple advantages over conventional laryngoscopy. It increases the distance between the operator's head and patient's airway. It improves the view on laryngoscopy, facilitates help from the airway assistant, and during difficult airway improves chances of first-pass success rate.23,24 When using a videolaryngoscope with Macintosh blades or while using a conventional laryngoscope, it is prudent to use a bougie with preloaded endotracheal tube to improve first-pass success rates. We do not recommend for or against any specific videolaryngoscope, but videolaryngoscopes with integrated oxygen channels are best avoided to minimize aerosol exposure.25 It is also preferable to use scopes with a separate screen so that the entire airway team can visualize the procedure and assist in any eventuality. If the airway manager is not familiar with use of videolaryngoscope, he or she should not use it for the first time in such a setting.
Recommendations
We recommend the use of videolaryngoscope over conventional laryngoscope for TI.
We do not recommend for or against any specific videolaryngoscope.
We recommend against the use of videolaryngoscopes with integrated oxygen channels.
We recommend against the first time use of videolaryngoscopes in COVID-19 patients if the operator is not experienced in its use.
We recommend the use of bougie with preloaded endotracheal tube for intubation.
Use of Endotracheal Tube Clamps
Use of endotracheal tube clamps have been suggested to reduce exposure of HCWs to aerosols.26 Albeit disposable clamps are in use, these are not universal, and surgical clamps (forceps) can be used instead to clamp the endotracheal tube before TI and extubation. If a clamped endotracheal tube is used, the clamps should be removed only after the endotracheal tube cuff is inflated, and the endotracheal tube is connected to the ventilator.
Recommendations
We recommend use of endotracheal tube clamps.
We recommend that the clamps be removed only after the inflation of endotracheal tube cuff and the endotracheal tube is connected to the ventilator.
Confirmation of Correct Placement of Endotracheal Tube
Correct placement of endotracheal tube should always be confirmed by capnography. Experienced operators can consider using lung ultrasound for this purpose, that too, when capnography is not available. Three-point or five-point auscultation may not be possible with full PPE and could be hazardous for HCWs. Auscultation method also does not guarantee confirmation of correct endotracheal tube placement, and it is better to look at bilaterally symmetrical chest rise on ventilation as a good clinical indicator; however, it should not be considered as a replacement to capnographic confirmation.
Recommendations
We recommend the use of capnography for confirmation of tube position.
We recommend against auscultation method as only method for confirmation of tube position.
We do not recommend for or against the use of ultrasonography for confirmation of tube position. An experienced person may use it, but capnographic confirmation is a must for all patients.
The steps for endotracheal intubation are summarized in Box 5.
Box 5.
Steps for endotracheal intubation in COVID-19 patients
| 1. Assess the patient for severity of hypoxemia and discuss the plan for intubation. |
| 2. Check the COVID-19 airway cart. |
| 3. Place the barrier device after explaining the purpose to the patient. |
| 4. Preoxygenate with 100% oxygen for 3–5 minutes with a tight-fitting mask and closed circuit with viral filter. |
| 5. If the patient is agitated, consider delayed sequence intubation. Administer 0.5–1 mg/kg of ketamine. |
| 6. Induce the patient with etomidate or ketamine, followed by neuromuscular blockade with rocuronium 1.2 mg/kg or succinyl choline 1.5 mg/kg. |
| 7. Avoid positive pressure ventilation. If needed, deliver small tidal volume breaths with face mask held by two-hand C and E grip. |
| 8. Consider a second-generation supraglottic airway with filter attached, if bag and mask ventilation is difficult or to be avoided, but ventilation deemed necessary. |
| 9. Use videolaryngoscope and insert a preclamped endotracheal tube threaded over a bougie or stylet. |
| 10. Once the tube is inserted, inflate the cuff to a pressure of 20–25 cmH2O. |
| 11. Connect to ventilator or respirator and release the clamp. |
| 12. Confirm the tube position by capnography. |
| 13. Insert a nasogastric tube, if not already placed before. |
| 14. If the patient is a suspected to have COVID-19, it is preferable to collect a sample before leaving the patient. |
| 15. If reusable equipment is used, place it in the bag for later disinfection. |
Unanticipated Difficult Intubation
A detailed description of management of unanticipated difficult airway is beyond the scope of this document. Certain principles specific to COVID-19 would be discussed. A chart depicting options for management of unanticipated difficult airway, such as developed by any of professional societies, should be available with the airway cart.
When rescue bag and mask ventilation is performed, a two-handed C and E grip should be followed. Second-generation supraglottic airway should be used early in airway management to avoid risks of aerosol generation with bag and mask ventilation. If fiberoptic bronchoscopy-aided TI is planned, apneic oxygenation should be avoided. If bronchoscope is used through a supraglottic airway, then positive-pressure ventilation should be avoided.
Cricothyroidotomy is the method of choice for emergency surgical airway. Cricothyroidotomy should be performed by scalpel and bougie technique. Oxygen insufflation during the procedure both through needle and through nasal cannula and face mask increases the risk of aerosol generation and should be completely avoided. The committee does not recommend percutaneous tracheostomy as a rescue procedure but can be considered as a life-saving procedure in exceptional circumstances when expertise is available.
Recommendations
We recommend early use of second-generation supraglottic airway for unanticipated difficult airway.
We recommend cricothyroidotomy by a scalpel and bougie technique.
We recommend against the practice of apneic oxygenation during cricothyroidotomy or during bronchoscopy-aided intubation.
We recommend against the use of percutaneous tracheostomy in unanticipated difficult airway, unless expertise is available, and this is deemed life-saving.
Tracheal Extubation
Risk of aerosol generation with extubation is the same as with intubation, and it is potentially more likely to transmit infection due to lack of neuromuscular paralysis and potential for coughing during extubation.7,8 The barrier precautions for extubation should be same as that for intubation. Patient should meet standard extubation criteria. Patient should be clearly explained the sequence, and a barrier device should be placed. Plastic drapes or aerosol box can be considered. T-piece trial should be avoided, and the patient should be extubated directly from pressure support ventilation or continuous positive airway pressure. Assessment of power by asking the patient to cough should be completely discouraged. Instead, negative inspiratory force on the ventilator should be assessed for respiratory muscle efficiency. Tracheal suction should be performed using closed suction system. Performance of leak test to assess readiness for extubation is controversial. Leak test might increase the risk of aerosol generation and should be avoided. Once patient is extubated, it is prudent to apply a face mask immediately. The practice of nebulization immediately after extubation should not be performed, and the committee strongly recommends against such practice. We do not recommend for or against use of sedatives before extubation, and their use should be considered based on the patient's clinical condition and expertise of the intensivist involved in extubation.
Recommendations
We recommend the use of barrier device during extubation.
We recommend against the use of T-piece trial to assess readiness for extubation.
We strongly recommend against the practice of inducing cough to assess readiness for extubation.
We recommend against performance of leak test.
We do not recommend for or against the use of sedatives before extubation.
We recommend against use of routine nebulization after extubation.
We recommend the use of surgical face mask over the patient face, immediately after extubation.
Percutaneous Tracheostomy
Awake percutaneous tracheostomy in nonintubated patients should not be performed in COVID-19 patients due to risk of aerosol generation, even when tracheostomy is clinically indicated. All efforts should be made to avoid coughing during procedure. It is recommended to use sedation and neuromuscular paralysis for this purpose. Videolaryngoscope should be used instead of conventional laryngoscope, for withdrawing the endotracheal tube. Ultrasound-guided tracheostomy is preferred over bronchoscopy guidance to minimize aerosol generation and also to minimize the number of HCWs involved in the procedure.
Recommendations
We recommend against use of percutaneous tracheostomy in nonventilated patients.
We recommend the use of sedation and neuromuscular paralysis during tracheostomy.
We recommend ultrasound over bronchoscopy aided percutaneous tracheostomy to minimize exposure to HCWs.
Flexible Fiberoptic Bronchoscopy
Bronchoscopy should be avoided for diagnosis of COVID-19 disease.27 In patients with previous negative upper respiratory sample and high clinical suspicion, the World Health Organization recommends a lower respiratory sample for testing, as it has the highest sensitivity for COVID-19 diagnosis.28 Albeit, the odds of aerosol generation with bronchoscopy is much less in comparison with endotracheal intubation,8 and in a non-intubated COVID-19 patient diagnostic bronchoscopy should be avoided. Awake bronchoscopy increases risk of cough, thereby aerosol generation. It also carries high risk of contamination with oropharyngeal and nasopharyngeal secretions.
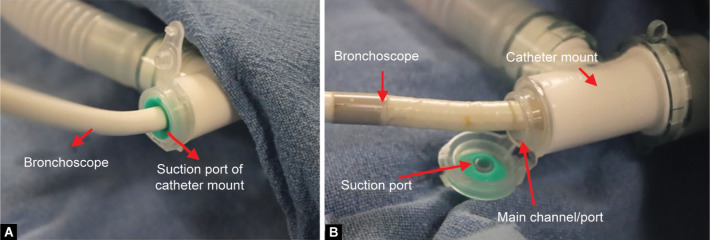
In a hypoxic patient in the ICU, bronchoscopy can worsen hypoxemia. Risks involved in fiberoptic bronchoscopy for diagnostic purposes should be considered in such patients. Bronchoscopy, in ventilated patients, might also be needed for therapeutic purposes such as removal of mucous plug or blood clots. When indicated, to minimize the risk to HCWs, we recommend that bronchoscopy be done under sedation and preferably with neuromuscular paralysis. Before introducing the bronchoscope, we suggest that ventilation should be paused, endotracheal tube be clamped, and then the bronchoscope is introduced through the suction port of the catheter mount. Insertion of the bronchoscope through the main port of the catheter mount increases the exposure to aerosols and should not be practiced (Fig. 8). When indicated, it should be performed with full precautions, as needed for TI, with a barrier device.
Figs 8A and B.
Bronchoscopy. (A) Insertion of bronchoscope through the suction port of catheter mount; (B) Insertion of bronchoscope through the main channel of catheter mount—it increases the risk of aerosol and should be avoided
Recommendations
We recommend against use of bronchoscopy in nonventilated patients for diagnostic purposes.
When indicated, we recommend that endotracheal tube be clamped and ventilation be paused before insertion of bronchoscope.
We recommend for insertion of bronchoscope through suction port of catheter mount over the main channel of catheter mount.
Nebulization in COVID-19 Patients
The evidence about the risk of transmission of infection through aerosols generated by nebulizer is conflicting.8 Aerosols generated by a nebulizer is derived from a medication solution and is not a bio-aerosol as generated during a cough or sneeze. Nevertheless, during nebulization, large amount of droplets are generated, and this increases the risk of contamination of the nearby environment. Hence, nebulization should be used only in patients with absolute indications and with full precautions in negative-pressure rooms.
Nebulization in Nonventilated COVID-19 Patients
Patients with preexisting diseases such as bronchial asthma and COPD, and infected with COVID-19, may require regular use of aerosolized medications for control of bronchospasm. Proper use of pressurized metered dose inhaler (pMDI) and dry powder inhalers (DPI) requires a cooperative patient who can perform various breathing techniques such as coordination of hand and breath, low and steady inspiratory flow, and breath holding. If the patient can perform these maneuvers, it is recommended to use pMDI and DPIs for delivery of aerosolized medications. It is always recommended to use these devices with a spacer or holding chamber for effective drug delivery and to reduce contamination. Clinicians should consider alternative methods of drug delivery, if use of these devices precipitates cough or if the patient's respiratory distress prevents him from performing the requisite techniques.
Jet nebulizers are the most commonly used nebulization technique in nonventilated patients. Although highly efficient in delivery of drug, close to two-third of the droplets are emitted into the environment. A high gas flow of 2 to 10 liters is needed to generate medical aerosols in jet nebulizer.29 This high gas flow along with high concentration of droplets in the environment increases the risk of exposure to HCWs, and thus use of jet nebulizers with a face mask is not recommended in COVID-19 patients. If a jet nebulizer is used, a mouth piece is preferred over a face mask. Expiratory filters that can be used along with jet nebulizers are available, which can capture the expired aerosols and reduce transmission to the environment.30 It should be used only if the treating clinician is familiar with the use of such devices. Instead, a HEPA filter or bacterial filter should be attached to the expiratory port of the mouth piece in order to reduce environmental contamination. The HCWs involved in the therapy should wear full PPE, and it is preferable to use a barrier device during nebulization.
Recommendations
We recommend against the use of routine nebulization in COVID-19 patients.
We recommend for the use pMDI or DPI in spontaneously breathing cooperative patient.
We recommend against the use of jet nebulizers in patients where pMDI or DPI can be used.
We recommend the use of mouth piece over mask for nebulization when jet nebulizer is used. We recommend use of viral filter on the expiratory port of mouth piece.
Nebulization in Ventilated COVID-19 Patients
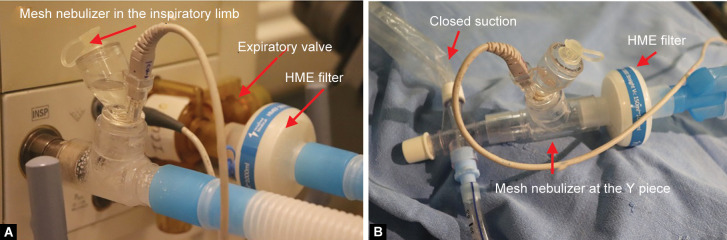
In a ventilated patient, use of pMDI or a jet nebulizer will require disruption of closed circuit and therefore cannot be recommended. Mesh nebulizers should be used whenever an aerosolized drug is to be delivered. The position of mesh nebulizer in the breathing circuit is debatable. Albeit placement of the mesh nebulizer 15 to 40 cm from the Y-piece increases drug delivery, and this position contaminates the breathing circuit. Thus, it is recommended to place the mesh nebulizer at the Y-piece. A viral filter should be placed between the nebulizer and the breathing circuit in order to reduce retrograde contamination of the circuit (Fig. 9). Care must be taken to prevent disruption or disconnection of the circuit at all times. If the mesh nebulizer is placed in the inspiratory limb, proper decontamination and disposal of breathing circuits is necessary to prevent exposure to HCWs.
Figs 9A and B.
Mesh nebulizer in ventilated patient. (A) Proximal placement of nebulizer, note that a HME filter is placed before the expiratory valve; (B) Nebulizer at the Y-piece with proximal filter to avoid decontamination of ventilator tubes
Recommendations
We recommend against the use of jet nebulizer in ventilated patient.
We recommend the use of mesh nebulizer in ventilated patient.
We recommend that the mesh nebulizer be placed at the Y-piece, with filter placed between Y-piece and nebulizer.
Airway Suction in Ventilated COVID-19 Patients
Open suction increases the risk of transmission to HCWs, and it is not recommended. All ventilated patients should be connected to a closed in line suction unit for tracheal suctioning. When the suction device is changed, ventilation should be paused, endotracheal tube should be clamped, and the device should be changed. Care must be taken to minimize disruption in the ventilatory circuit.
Recommendations
We strongly recommend against the use of open suction.
We recommend for the use of closed in line suction device for airway toileting.
Airway Management during Cardiopulmonary Resuscitation
The ethical concerns about cardiopulmonary resuscitation (CPR) are beyond the scope of this document. Chest compressions and defibrillation have been shown to increase the risk of aerosol generation, although the evidence is debatable.8,11 Minimal staff should be present during resuscitation with full PPE. Bag and mask ventilation should be avoided, and early advanced airway using a second-generation supraglottic device or endotracheal intubation should be considered. American heart association has suggested interruption of chest compressions to secure an advanced airway, and once endotracheal intubation is achieved, a HEPA filter should immediately be connected to the endotracheal tube. It is also recommended to ventilate the patient using the ICU ventilators.
Recommendations
We recommend early use of advanced airway devices during CPR.
We recommend brief interruption in chest compression to secure the airway with an advanced airway device.
We recommend use of ICU ventilators for ventilation during CPR instead of manual ventilation.
Conclusion
Airway management in COVID-19 patients could be challenging due to many unknown risks. In such a scenario, it is always best to follow simple, reliable, and familiar techniques that are safe for both the patient and the HCWs.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/?gclid=EAIaIQobChMIofyXveza6QIVyXwrCh3BRApIEAAYASABEgIdcfD_BwE https://covid19.who.int/?gclid=EAIaIQobChMIofyXveza6QIVyXwrCh3BRApIEAAYASABEgIdcfD_BwE Available from:
- 2.Möhlenkamp S, Thiele H. Ventilation of COVID-19 patients in intensive care units. Herz. 2020;(4):1–3. doi: 10.1007/s00059-020-04923-1. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prin M, Bartels K. Social distancing: implications for the operating room in the face of COVID-19. Can J Anesth. 2020;(7) doi: 10.1007/s12630-020-01651-2. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020;(6) doi: 10.1002/jmv.25748. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(2):145–151. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. DOI: [DOI] [PubMed] [Google Scholar]
- 6.Van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lockhart SL, Duggan LV, Wax RS, Saad S, Grocott HP. Personal protective equipment (PPE) for both anesthesiologists and other airway managers: principles and practice during the COVID-19 pandemic. doi.org/10.1007/s12630-020-01673-w. Can J Anesth. 2020 doi: 10.1007/s12630-020-01673-w. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS ONE. 2012;7(4) doi: 10.1371/journal.pone.0035797. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li J, Fink JB, Ehrmann S. High-flow nasal cannula for COVID-19 patients: low risk of bio-aerosol dispersion. Eur Respir J. 2020;55(5):2000892. doi: 10.1183/13993003.00892-2020. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Air | Appendix | Environmental Guidelines | Guidelines Library | Infection Control | CDC. https://www.cdc.gov/infectioncontrol/guidelines/environmental/appendix/air.html https://www.cdc.gov/infectioncontrol/guidelines/environmental/appendix/air.html Available from:
- 11.Verbeek JH, Ijaz S, Mischke C, Ruotsalainen JH, Mäkelä E, Neuvonen K, et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev. 2016;4:CD011621. doi: 10.1002/14651858.CD011621.pub2. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Occupational Safety and Health Administration. Assigned protection factors for the revised respiratory protection standard. https://www.osha.gov/Publications/3352-APF-respirators.pdf. [Accessed March 31, 2020]. https://www.osha.gov/Publications/3352-APF-respirators.pdf
- 13.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020;(13) doi: 10.1001/jama.2020.2648. DOI: [DOI] [PubMed] [Google Scholar]
- 14.Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, et al. Difficult airway society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115(6):827–848. doi: 10.1093/bja/aev371. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matava CT, Yu J, Denning FS. Clear plastic drapes may be effective at limiting aerosolization and droplet spray during extubation: implications for COVID-19. doi.org/10.1007/s12630-020-01649-w. Can J Anesth. 2020:1–3. doi: 10.1007/s12630-020-01649-w. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cubillos J, Querney J, Rankin A, Moore J, Armstrong K. A multipurpose portable negative air flow isolation chamber for aerosol-generating procedures during the COVID-19 pandemic. doi.org/10.1016/j.bja.2020.04.059. Br J Anaesth. 2020:1–3. doi: 10.1016/j.bja.2020.04.059. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Canelli R, Connor CW, Gonzalez M, Nozari A, Ortega R. Barrier enclosure during endotracheal intubation. N Engl J Med. 2020;382(20):1957–1958. doi: 10.1056/NEJMc2007589. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Jong A, Molinari N, Terzi N, Mongardon N, Arnal JM, Guitton C, et al. Early identification of patients at risk for difficult intubation in the intensive care unit: development and validation of the MACOCHA score in a multicenter cohort study. Am J Respir Crit Care Med. 2013;187(8):832–839. doi: 10.1164/rccm.201210-1851OC. DOI: [DOI] [PubMed] [Google Scholar]
- 19.Davis DP, Olvera DJ. HEAVEN criteria: derivation of a new dif fi cult airway prediction tool. Air Med J. 2017;36(4):195–197. doi: 10.1016/j.amj.2017.04.001. DOI: [DOI] [PubMed] [Google Scholar]
- 20.Sullivan EH, Gibson LE, Berra L, Chang MG, Bittner EA. In-hospital airway management of COVID- 19 patients. doi.org/10.1186/s13054-020-03018-x. Crit Care. 2020;24(1):292. doi: 10.1186/s13054-020-03018-x. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hui DS, Chow BK, Lo T, Tsang OTY, Ko FW, Ng SS, et al. Exhaled air dispersion during high-flow nasal cannula therapy versus CPAP via different masks. Eur Respir J. 2019;53(4):1802339. doi: 10.1183/13993003.02339-2018. DOI: [DOI] [PubMed] [Google Scholar]
- 22.Castro de Oliveira BM, Lucas Passos,, de Souza R. Advantages of delayed sequence intubation in selected patients with coronavirus disease (COVID-19). Anesth Analg. 2020 doi: 10.1213/ANE.0000000000004977. DOI: [DOI] [PubMed] [Google Scholar]
- 23.Lewis SR, Butler AR, Parker J, Cook TM, Smith AF. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation. Cochrane Database Syst Rev. 2016;11(11):CD011136. doi: 10.1002/14651858.CD011136.pub2. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hall D, Steel A, Heij R, Eley A, Young P. Videolaryngoscopy increases ‘mouth-to-mouth’ distance compared with direct laryngoscopy. Anaesthesia. 2020;75(6):822–823. doi: 10.1111/anae.15047. DOI: [DOI] [PubMed] [Google Scholar]
- 25.Singh N, Rao PB, Mishra N. Video laryngoscopy in COVID-19 patients: a word of caution. doi.org/10.1007/s12630-020-01677-6. Can J Anesth. 2020:12630. doi: 10.1007/s12630-020-01677-6. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jacob M, Ruivo E, Costa H, Nunez D. An innovative endotracheal tube clamp for use in COVID-19. Can J Anaesth. 2020:1–3. doi: 10.1007/s12630-020-01703-7.2020;19-21. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vergnon J-M, Trosini-Desert V, Fournier C, Lachkar S, Dutau H, Guibert N, et al. Bronchoscopy use in the COVID-19 era. Respir Med Res. 2020:100760. doi: 10.1016/j.resmer.2020.100760. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.WHO. Laboratory testing for coronavirus disease 2019 (COVID-19) in suspected human cases. Interim Guid. 2020. https://www.who.int/publications-detail/laboratory-testing-for-2019-novelcoronavirus-in-suspected-human-cases-20200117 pp. 1–7.https://www.who.int/publications-detail/laboratory-testing-for-2019-novelcoronavirus-in-suspected-human-cases-20200117 Available from:
- 29.Jet AA. Ultrasonic, and mesh nebulizers: an evaluation of nebulizers for better clinical outcomes. Eurasian J Pulmonol. 2014;16(1):1–7. doi: 10.5152/ejp.2014.00087. DOI: [DOI] [Google Scholar]
- 30.Wittgen BPH, Kunst WAP, Perkins WR, Lee KJ, Postmus PE. assessing a system to capture stray aerosol during inhalation of nebulized liposomal cisplatin. J Aerosol Med. 2006;19(3):385–391. doi: 10.1089/jam.2006.19.385. DOI: [DOI] [PubMed] [Google Scholar]