Abstract
Aims and objectives
Utility of pediatric logistic organ dysfunction-2 (PELOD-2) score on day 1 within 1 hour of admission in predicting mortality in children admitted in pediatric intensive care unit (PICU).
Background
Various scoring systems aid to evaluate the patient's mortality risk in the intensive care unit (ICU) by assigning a score and predicting the outcome. Critically ill children are characterized by large variations in the normal body homeostasis. These variations can be estimated by the change of the physiological variables from the normal range. Various scores are constructed from deviations of these changed variables. One such score, the PELOD-2 score, is used to predict mortality of patients admitted in PICU.
Materials and methods
This study was carried out at a tertiary care center in central India to study the utility of PELOD-2 score within 1 hour of admission to predict mortality in patients admitted in PICU.
Results
Total 129 patients were included in this study with mean age of 67 months. The system with highest admission was central nervous system with 42 children and 16.6% mortality, whereas those 7 patients with hematological system involvement had highest mortality of 28.5%. The mortality rate was 15.55%. In our study for PELOD-2 within 24 hours of admission, the area under receiver operating curve was 0.87 and the Hosmer–Lemeshow test was p = 0.42.
Conclusion
Pediatric logistic organ dysfunction-2 score in our study had significant association with mortality along with the Hosmer–Lemeshow goodness-of-fit test showing a good prediction of mortality.
How to cite this article
Deshmukh T, Varma A, Damke S, Meshram R. Predictive Efficacy of Pediatric Logistic Organ Dysfunction-2 Score in Pediatric Intensive Care Unit of Rural Hospital. Indian J Crit Care Med 2020;24(8):701–704.
Keywords: Area under receiving operating curve, Mortality, Pediatric intensive care unit, Pediatric logistic organ dysfunction-2
Introduction
The main objective of the pediatric intensive care unit (PICU) is to prevent mortality by intensively monitoring and treating critically ill children who are considered at high risk of mortality. The capability to estimate patient risk of death is extremely important because these estimates would be useful in achieving many different goals, such as assessing prognosis, intensive care unit (ICU) performance, ICU resource utilization, evaluating therapies by comparative analyzes in quality assessment controlling, and matching severity of illness in clinical studies. The lack of consistency, reliability, and accuracy in physician's subjective opinions concerning patient status necessitates quantitative clinical scores. The scoring systems were developed in response to increasing emphasis on the evaluation and monitoring of health services.1 Pediatric logistic organ dysfunction-2 (PELOD-2) was designed to update and improve the PELOD score, using 3671 consecutive patients in a prospective, observational, multicenter cohort study in 9 French-speaking multidisciplinary, tertiary care PICUs of university affiliated hospitals between June 2006 and October 2007. Data on variables considered for the PELOD-2 score at seven time-points after PICU admission: days 1, 2, 5, 8, 12, 16, and 18, plus PICU discharge. It is highly reliable and sensitive to measure severity of illness and determine the probability of death in PICU.2–4 We hypothesized that even a single PELOD-2 score within 24 hours of admission to PICU would predict mortality and hence the study was carried out.
Materials and Methods
This prospective observational study was carried out in PICU of a tertiary care rural hospital attached to a medical college. The study was approved by the Institutional Ethics committee. All the patients admitted in PICU in the age group 1 month to 16 years were included except if the duration of PICU stay was <24 hours. The PELOD-2 score was calculated within 1 hour of admission. Each patient was evaluated for 10 parameters which includes Glasgow coma scale (GCS), pupillary reaction, mean arterial blood pressure, serum lactate, serum creatinine, PaO2, PaCO2, mechanical ventilation, WBC, and platelet count. Each parameter was given points between 0 and 6 and PELOD-2 score was calculated with a sum total of these points. The highest possible score was 33 and minimum 0. Outcome is recorded as survival and nonsurvival and compared with PELOD-2 score of that patient.
Statistical Analysis
All data were entered in the Microsoft excel spreadsheets and Stata software (Stata 10, Stata corporation, Texas, USA) was used for data analysis. Distribution of data was studied by Kolmogorov–Smirnov test. Qualitative data were summarized using percentage and proportions differences in proportion were compared by Chi-square test and Fischer's exact text. Differences between means were compared by unpaired student's “t” test where data were normally distributed and Mann–Whitney U test was non-normally distributed data. To determine the predictive values for mortality, area under the curve (AUC) of PELOD was defined and compared with outcome. The best cutoff was chosen utilizing sensitivity and specificity from the receiver operating characteristic (ROC) curve of the selected data. Hosmer–Lemeshow goodness-of-fit test was applied to observe for calibration in the study.
Results
Out of the 129 total patients admitted, 73 were males (56.58%) and 56 were females (37.2%) with male to female ratio of 1.3:1. The mean age observed was 67 months. Mortality in males was 16.43% and that in female was observed to be 14.28%. Mortality was highest in 1–11 months age group. The baseline characteristics are shown in the Table 1. Neurological system involvement was the most common system with 32.5% of total included. The system wise mortality in descending order observed was hematological (28%), respiratory (20%), neurological (16.6%), and cardiovascular (16.1%) as shown in Table 2.
Table 1.
Distribution as per age
| Age in months | Total | Survival | Death | % mortality |
|---|---|---|---|---|
| 1–11 | 27 | 18 | 9 | 33.33 |
| 12–23 | 8 | 8 | 0 | 0 |
| 24–59 | 30 | 24 | 6 | 20 |
| 60–143 | 41 | 39 | 2 | 4.87 |
| ≥144 | 23 | 20 | 3 | 13.04 |
| Total | 129 | 109 | 20 | 15.50 |
Table 2.
Distribution according to diagnosis
| System | Total | Survival | Death | % mortality |
|---|---|---|---|---|
| Neurological | 42 | 35 | 7 | 16.6 |
| Cardiovascular | 31 | 26 | 5 | 16.1 |
| Respiratory | 15 | 12 | 3 | 20 |
| Hematological | 7 | 5 | 2 | 28.5 |
| Infectious | 10 | 10 | 0 | 0 |
| Miscellaneous | 24 | 21 | 3 | 12.5 |
| Total | 129 | 109 | 20 | 15.50 |
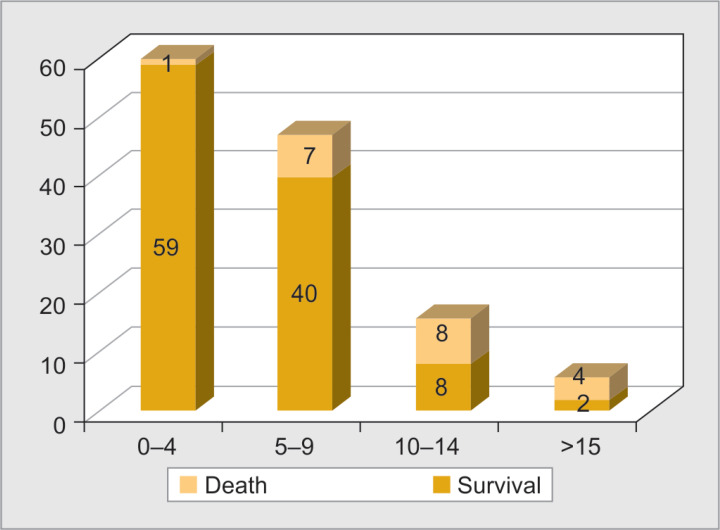
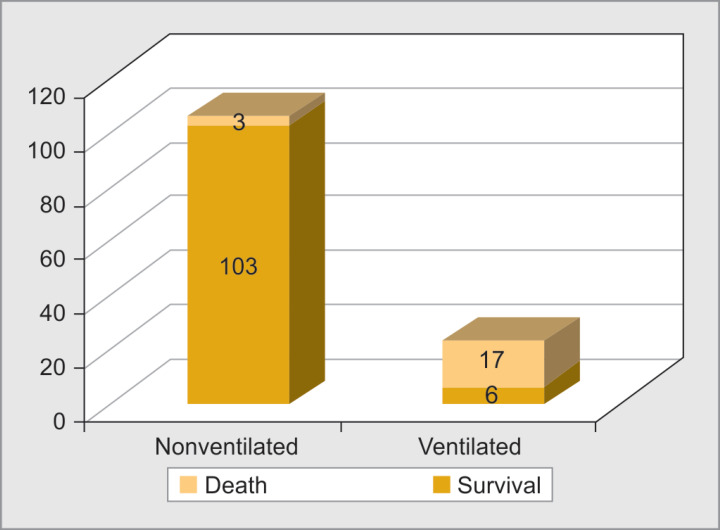
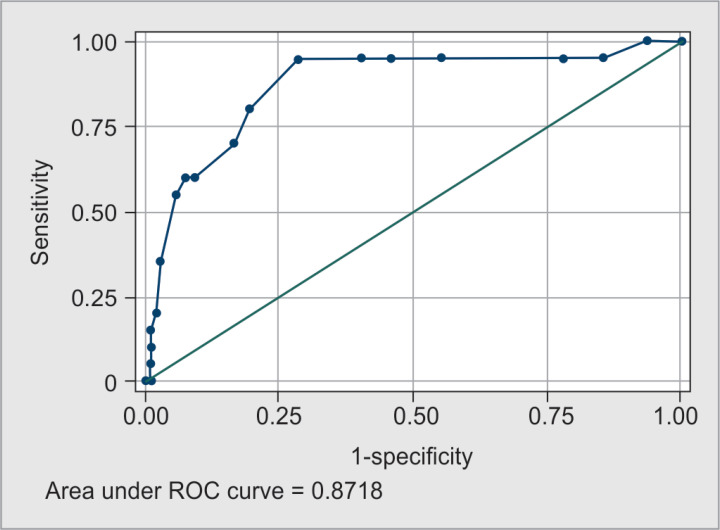
The score was grouped as score 0–4, score 5–9, score 10–14, and score >15. Out of 129 patients admitted in the study (Table 2), 60 patients had a score of 0–4 with 1 death and mortality of 1.6%. Forty-seven patients had score between 5 and 9 with 7 deaths and mortality rate of 14.8%. Mortality observed in group with score 10–14 was 50%. Maximum number of deaths observed in the group with score >15 with mortality rate of 66.6% was statistically significant and was obtained by Mann–Whitney U test. The total PELOD-2 score in the survivors and the nonsurvivors is given in the Table 3 and demonstrated on Figure 1. In our study as shown in Figure 2, 23 got intubated out of which 6 survived and 17 died with mortality rate of 85% and had mean score of 8.6 in nonintubated and 13.7 in intubated patients. The degrees of discrimination among the survivors and the nonsurvivors were calculated using ROC. In our study, area under receiver operating curve (AUROC) of 0.87 indicated a good discrimination (Fig. 3).
Table 3.
Pediatric logistic organ dysfunction-2 score and outcome
| Score | Total | Survival | Death | % mortality |
|---|---|---|---|---|
| 0–4 | 60 | 59 | 1 | 1.6 |
| 5–9 | 47 | 40 | 7 | 14.8 |
| 10–14 | 16 | 8 | 8 | 50 |
| >15 | 6 | 2 | 4 | 66.6 |
| Total | 129 | 109 | 20 | 15.50 |
Fig. 1.
Association between Pediatric logistic organ dysfunction-2 score and outcome
Fig. 2.
Association between invasive ventilation and outcome
Fig. 3.
Receiver operating characteristic (ROC) curve for pediatric logistic organ dysfunction-2 score
Discussion
Thukral et al.5 in their study for the validation of the PELOD score for multiple organ dysfunction in children observed the male to female ratio was 1.78. Infants accounted for 41.2% of the study population. Leteurtre et al.2 also observed that maximum admissions were from age group 1–11 months (29.1%). The gender distribution indicated male preponderance in the above studies similar to our study. Patients with hematological illness had highest mortality followed by respiratory. Patki et al.6 in their study observed that out of the total 120 cases, neurological involvement was highest 32 (26.7%) with mortality being 28%. Whereas, El-Nawawy et al.7 in their study for performance of PELOD and PELOD-2 scores in a PICU in a developing country (Egypt) noted that around 44% cases among total were with respiratory system involvement. In our study of the total admitted, 23 (17.8%) patients were ventilated and 17 out of them died (73.9%). A significant association with mortality and need for ventilation was observed. Similar observation has been observed with many other studies. Zhong et al.8 in their study observed that 14% of the survivors and 78.6% of the nonsurvivors were ventilated with a significant association with mortality (p ≤ 0.001). In our study, the serum lactate levels when high were associated with higher mortality as compared to low lactate levels. Jat et al.9 and Zhong et al.8 found that serum lactate levels to be significantly higher in nonsurvivors. Blood lactate is frequently used to monitor tissue hypoxia. As utilization of pyruvate depends on the presence of oxygen, which decreases in cellular oxygen delivery, results in increased lactate production and blood lactate levels.10 The finding of raised creatinine levels and higher mortality observed in the current study is congruent with the above-mentioned studies. These observations positively implicate association of higher creatinine values and mortality. The renal functions are affected more in age <11 months than any other age group. Immature renal system in these age groups is responsible for serum creatinine levels to be more affected in critically ill patients. In our study, inotropes requirement for >6 hours was considered, where those who needed inotrope support consisted of 22 patients out of which 19 died. Inotropes requirement had statistically significant correlation with mortality (p = 0.0000), corroborating the findings by Rady et al.11 in his study as compared to other studies who found that higher mortality in patients using these drugs. The association of PELOD-2 with outcome obtained suggested maximum mortality in the group with score >15 (66.6%) (Table 4).
Table 4.
Comparison of our study with other studies for area under curve (AUC)
| Study | % mortality | AUC |
|---|---|---|
| Our study | 15.5 | 0.87 |
| Karam et al. | 26.5 | 0.81 |
| Nawawy et al. | 3.1 | 0.91 |
| Zhong et al. | 0.91 | |
| Mathews et al. | 3.3 | 0.78 |
| Thukral et al. | 0.80 |
The association of PELOD-2 with outcome obtained suggested maximum mortality in the group with score >15 (66.6%). The score of ≥8 had maximum sensitivity (80%) and specificity (80.73%) for the mortality. Mortality rate (15.5%) in this study was higher in contrast to that observed in developed countries. Discrimination capacity is assessed using the area under the ROC curve, where 1 is a perfect curve (100% discriminative capacity) and 0.5 is a random chance effect. In our study, PELOD-2 score had AUROC of 0.87 which means that an arbitrary patient who died had 87% chance of having a higher predicted risk than an arbitrary patient who survived. The Hosmer–Lemeshow goodness-of-fit test is the most accepted method for measuring calibration. A high p value suggest good calibration.12 In our study, the day 1 PELOD-2 score showed p value = 0.42 using Hosmer–Lemeshow goodness-of-fit test, thus having a good prediction of mortality.
Ramazani and Hosseini13 found that mean score of PRISM III, PIMS, and PELOD-2 was significant in nonsurvivors compared with survivors (p < 0.001, p < 0.001, and p < 0.0001, respectively) with AUC = 0.803 for PELOD-2 score. They observed that in terms of discrimination power, the performance of PIM3 and PELOD-2 was slightly better than that of the PRISM III. A study performed by Varma et al.14 in similar population using PRISM III score found with ROC of 0.86 was observed with mortality of 14.8%. Being a single-center study, the disease pattern and characteristics were similar. The organ dysfunction predicted in this study reflects a similar disease pathology.
El-Nawawy et al.7 in their study of predicting performance of PELOD and PELOD-2 scores in PICU of developing countries observed that the overall predicted mortality with PELOD was 76 patients and that with PELOD-2 was 50 patients. The observed deaths were 50. Thus, PELOD-2 was found to have a better prediction of mortality with AUC of 0.91 for PELOD-2.
Zhong et al.8 in their study found that day 1 PELOD-2 score and day 1 q PELOD-2 score were effective and able to assess the prognosis of children with sepsis in PICU. The AUC obtain for above were 0.916 and 0.802, respectively.
Mathews et al.15 in their study found that PELOD-2 >20 predicted mortality in 72.2% patients. Based on the ROC curve, PELOD-2 score >16 predicted mortality with a sensitivity 100% and specificity 54.1%. The ROC for PELOD-2 obtained was 0.78.
Karam et al.16 in his study for performance of PELOD-2 in critically ill children requiring plasma transfusions observed that the day 1 PELOD-2 AUC was 0.76 with the Hosmer–Lemeshow test was p = 0.76. The serial evaluation of changes in daily PELOD-2 scores from day 1 demonstrated a significant association with death.
In our study, GCS, invasive ventilation, lactate levels, and inotropes requirement showed significant association with mortality. Independent risk factors for death were mechanical ventilation and neurological failure in the PICU of the Children's Hospital of the University of Cairo in study by Hamshary et al.17
Leclerc et al.18 found that PELOD-2 had AUROC curve = 0.93 and calibration chi-square test for goodness-of-fit = 5.8, p = 0.45 was good. In multicenter binational cohort study of patients <18 years admitted to ICUs in Australia and New Zealand following were in observations. While assessing organ dysfunction using PELOD-2, a score of ≥8 performed best in identifying patients at higher mortality: There were 374 (14.4%) children with a PELOD-2 score ≥8, with a mortality of 22.2 vs 3.0% in those with scores <8 indicating p < 0.001 in study by Schlapbach et al.19
Conclusion
Pediatric logistic organ dysfunction-2 on day 1 of admission score has a strong prediction value to describe organ dysfunction. Mortality rate increases with increase in PELOD-2 score, i.e., higher the PELOD-2 score higher the mortality.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Bhadoria P, Bhagwat AG. Severity scoring systems in paediatric intensive care units. Indian J Anaesth. 2008;52(Suppl 5:):663–675. [Google Scholar]
- 2.Leteurtre S, Duhamel A, Salleron J, Grandbastien B, Lacroix J, Leclerc F. Groupe francophone de réanimation et d′Urgences pédiatriques (GFRUP). PELOD-2: an update of the pediatric logistic organ dysfunction score. Crit Care Med. 2013;41(7):1761–1773. doi: 10.1097/CCM.0b013e31828a2bbd. DOI: [DOI] [PubMed] [Google Scholar]
- 3.Marcin JP, Song J, Leigh JP. The impact of pediatric intensive care unit volume on mortality: a hierarchical instrumental variable analysis. Pediatr Crit Care Med. 2005;6(2):136–141. doi: 10.1097/01.PCC.0000154962.73861.66. DOI: [DOI] [PubMed] [Google Scholar]
- 4.Leteurtre S, Grandbastien B, Leclerc F, Parslow R. Groupe francophone de réanimation et urgences pédiatriques, paediatric intensive care audit network. international comparison of the performance of the paediatric index of mortality (PIM) 2 score in two national data sets. Intensive Care Med. 2012;38(8):1372–1380. doi: 10.1007/s00134-012-2580-6. DOI: [DOI] [PubMed] [Google Scholar]
- 5.Thukral A, Kohli U, Lodha R, Kabra SK, Arora NK. Validation of the PELOD score for multiple organ dysfunction in children. Indian Pediatr. 2007;44(9):683. [PubMed] [Google Scholar]
- 6.Patki VK, Raina S, Antin JV. Comparison of severity scoring systems in a pediatric intensive care unit in India: a single-center prospective, observational cohort study. J Pediat Intensive Care. 2017;6(02):098–102. doi: 10.1055/s-0036-1584811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El-Nawawy A, Mohsen AA, Abdel-Malik M, Taman SO. Performance of the pediatric logistic organ dysfunction (PELOD) and (PELOD-2) scores in a pediatric intensive care unit of a developing country. Eur J Pediatr. 2017;176(7):849–855. doi: 10.1007/s00431-017-2916-x. [DOI] [PubMed] [Google Scholar]
- 8.Zhong M, Huang Y, Li T, Xiong L, Lin T, Li M, et al. Day-1 PELOD-2 and day-2 scores in children with sepsis in the PICU. J Pediatr (Rio J) 2019 doi: 10.1016/j.jped.2019.07.007. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jat KR, Jhamb U, Gupta VK. Serum lactate levels as the predictor of outcome in pediatric septic shock. Indian J Crit Care Med. 2011;15(2):102. doi: 10.4103/0972-5229.83017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hosmer DW, Hosmer T, Le Cessie S, Lemeshow S. A comparison of goodness-of-fit tests for the logistic regression model. Statist Med. 1997;16(9):965–980. doi: 10.1002/(sici)1097-0258(19970515)16:9<965::aid-sim509>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 11.Rady HI, Mohamed SA, Mohssen NA, ElBaz M. Application of different scoring systems and their value in pediatric intensive care unit. Egyptian Pediatric Association Gazette. 2014;62(3-4):59–64. [Google Scholar]
- 12.Meakins J, Long CN. Oxygen consumption, oxygen debt and lactic acid in circulatory failure. J Clin Invest. 1927;4(2):273–293. doi: 10.1172/JCI100123. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramazani J, Hosseini M. Comparison of the predictive ability of the pediatric risk of mortality III, pediatric index of mortality, and pediatric logistic organ dysfunction in medical and surgical intensive care units. J Compr Ped. 2019;10(2):e82830. doi: 10.5812/compreped.82830. DOI: [DOI] [Google Scholar]
- 14.Varma A, Damke S, Meshram R, Vagha J, Kher A, Vagha K. Prediction of mortality by pediatric risk of mortality (PRISM III) score in tertiary care rural hospital in India. Int J Contemp Pediatr. 2017;4(2):322–331. doi: 10.18203/2349-3291.ijcp20170003. DOI: [DOI] [Google Scholar]
- 15.Mathews S, Rajan A, Soans ST. Prognostic value of rise in neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR) in predicting the mortality in paediatric intensive care. Int J Contemp Pediat. 2019;6(3):1052–1058. doi: 10.18203/2349-3291.ijcp20191044. DOI: [DOI] [Google Scholar]
- 16.Karam O, Demaret P, Duhamel A, Shefler A, Spinella PC, Stanworth SJ, et al. Performance of the pediatric logistic organ dysfunction-2 score in critically ill children requiring plasma transfusions. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5053948/ Ann Intensive Care. 2016;6(1):98. doi: 10.1186/s13613-016-0197-6. DOI: Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hamshary AAEE, Sherbini SAE, Elgebaly HF, Amin SA. Prevalence of multiple organ dysfunction in the pediatric intensive care unit: pediatric risk of mortality III versus pediatric logistic organ dysfunction scores for mortality prediction. Prevalência da falência de múltiplos órgãos na unidade de terapia intensiva pediátrica: comparação dos escores pediatric risk of mortality III e pediatric logistic organ dysfunction para predição de mortalidade. Rev Bras Ter Intensiva. 2017;29(2):206–212. doi: 10.5935/0103-507X.20170029. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leclerc F, Duhamel A, Deken V, Grandbastien B, Leteurtre S. Pédiatriques (GFRUP) on behalf of the GF de R et U. Can the pediatric logistic organ Dysfunction-2 score on day 1 be used in clinical criteria for sepsis in children?*. Pediat Crit Care Med. 2017;18(8):758–763. doi: 10.1097/PCC.0000000000001182. DOI: [DOI] [PubMed] [Google Scholar]
- 19.Schlapbach LJ, Straney L, Bellomo R, MacLaren G, Pilcher D. Prognostic accuracy of age-adapted SOFA, SIRS, PELOD-2, and qSOFA for in-hospital mortality among children with suspected infection admitted to the intensive care unit. Intensive Care Med. 2018;44(2):179–188. doi: 10.1007/s00134-017-5021-8. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]