Abstract
Introduction:
Ventilator associated pneumonia (VAP) is defined as nosocomial pneumonia in patients who have mechanical ventilation (MV) for more than 48 hours. The diagnosis of VAP is based on radiological-microbiological examinations. In the United States, the Centers for Disease Control and Prevention (CDC) and the National Health Care Network (NHSN) have an incidence of VAP of 5.8% per 1,000 days on mechanical ventilator.
Aim:
In this study, we had an aim to determine the occurrence of ventilator-associated pneumonia (VAP) in patients with MV who were hospitalized in the intensive care unit.
Method:
The study was retrospective, clinical, conducted in the period from January 1, 2016 until December 31, 2016. In a one-year period, 719 patients of both sex, aged 14 to 91, were hospitalized in the intensive care unit of the Clinic for Anesthesia and Resuscitation of the University Clinical Center in Sarajevo. The study included 250 patients of both sex who had respiratory support with mechanical ventilator. No patient was excluded from the study. As a confirmation of VAP, we used microbiological reports from the patient history documentation. The results were presented statistically through tables and graphs, numerically, by a percentage, and by a mean value with standard deviation.
Results:
Out of the 719 hospitalized patients, 250 or 34.8% underwent controlled ventilation. In 103 or 41.2% of patients some form of pneumonia was confirmed microbiologically. An average patient age on controlled ventilation was 60.4 ± 16.8 years. The mean age of a female patients who were on controlled ventilation was 63.2 ± 16.7, higher than that of male patients, which was 57.8 ± 16.6 years. The most frequent patients were over 60 years of age (52.8%). The shortest hospitalization of patients on controlled mechanical ventilation was 1 day and the longest was 120 days. Average duration of mechanical ventilation was 6.9 ± 10.5 days.
Conclusion:
VAP is a relatively common complication in patients with MV that can increase morbidity and mortality, as well as treatment costs. It is more frequent in females and in the elderly. Medical staff should provide normal maintenance of respiratory functions to a patient who is on MV, which will reduce the risk of VAP.
Keywords: nosocomial infection, ventilator associated pneumonia, intensive care unit, mechanical ventilation
1. INTRODUCTION
Ventilator-induced pneumonia (VAP) is a type of intrahospital infection that occurs after intubation of a patient and initiation of mechanical ventilation (MV). The incidence of VAP is 25-30% of the total number of critically ill in Intensive Care Units. It is accompanied by a high mortality rate (25-75%), increased cost and duration of treatment, and great attention is paid to non-pharmacological and pharmacological measures to prevent its occurrence (1). Early diagnosis has a crucial role, and an antibiotic choice depends on it. MV is performed in patients who for any reason are not able to provide spontaneous breathing to exchange gas in the body. Patients on MV are exposed to the possibility of more frequent occurrence of VAP (2). In recent decades, the causes of VAP are often resistant strains of bacteria, among which the leading role is played by Acinetobacter boumani, Klebsiella pneumoniae and Pseudomonas aeruginosa (3). The patient connected to the MV lung apparatus (ventilator) should be provided with normal maintenance of respiratory function while reducing the risk of developing VAP (4).
2. AIM
The aim of the study was to analyze characteristics of the patients with ventilator-associated pneumonia during one-year period (2016).
3. MATERIAL AND METHODS
The study was a clinical, and retrospective, conducted during the period from January 1, 2016 to December 31, 2016, in ICU at Clinic for Anesthesia and Resuscitation, Clinical Center of the University of Sarajevo (CCUS). During that period, 719 patients were hospitalized. The inclusion criterion was administration of MV. The study included 250 patients who were mechanically ventilated. The study included patients 14 to 91 years old, of both gender. The following variables were collected: age, sex, duration of MV, type of microorganism from endotracheal tube swabs, cannulas and bronchoalveolar lavage fluid. None of the patients was excluded from the.
Statistical data processing was done using the computer program Excel (Microsoft Office Excel 2003) and SPSS 13 for Windows, a computer program for statistical analysis. The data were statistically processed so that the following values were determined: mean and standard deviation, minimum and maximum value. The results were presented in the form of tables and graphs. For category variables, the results were presented as absolute numbers and the percentage frequency of individual categories. The Hi-square test was used to analyze the category variables. The significance of the difference for continuous variables was tested by an independent Student t-test. Values of p <0.05 were considered statistically significant.
4. RESULTS
Out of 719 (100%) hospitalized patients, 250 (34.8%) were on mechanical ventilation (MV), with 121 (48.4%) patients being female, while 129 (51.6%) were male. No statistically significant difference was found in the sexual representation of patients who underwent MV (χ2 = 0.128; p = 0.720).
The mean age of patients on MV was 60.4 ± 16.8 years. The youngest male patient was 14 and the oldest 87 years old. The youngest patient was 19 and the oldest 91 years old. The mean age of female patients who were on MV was higher (63.2 ± 16.7 years) compared to the age of male patients (57.8 ± 16.6 years). A statistically significant difference (p = 0.011) was found in the age of patients with MV in relation to gender. The mean duration of MV patients included in our study was 6.9 ± 10.5 days. Mechanical ventilation in male patients lasted the shortest 1 and the longest 45 days, while in female patients the shortest duration of MV was 1 and the longest 120 days.
Analyzing the duration of MV, we found that it lasted longer in female patients (7.9 ± 13.2 days) compared to male patients (5.9 ± 6.9 days). There was no statistically significant difference (p = 0.138) in the duration of MV in different gender patients (Table 1).
Table 1. Age and duration of controlled mechanical ventilation in relation to the gender of patients. p- probability, NS – non significant.
| Female patients (n=121;48.4%) |
Male patients (n=129;51.6%) |
p | |||||
|---|---|---|---|---|---|---|---|
| Age (years) |
63.2 ± 16.7 | 57.8 ± 16.6 | 0.011 | ||||
| Min. | Max. | Min. | Max. | ||||
| 19 | 91 | 14 | 87 | ||||
| Length of controlled mechanical ventilation (days) | 7.9 ± 13.2 | 5.9 ± 6.9 | NS | ||||
| Min. | Max. | Min. | Max. | ||||
| 1 | 120 | 1 | 45 | ||||
Out of total number of patients on the MV the age group of up to 30 years old had the smallest number of patients, a total of 19 or 7.6%; in the group of patients older than 30 years and up to 60 years old there were 99 (39.6%) patients, while in the age group of over 60 years old there was the largest number of patients, 132 or 52.8%.
A statistically significant difference was found in the prevalence of patients who underwent mechanical ventilation in different age groups (χ2 = 53.59; p <0.0005) (Figure 1).
Figure 1. Percentage representation of patients on MV based on age groups and gender.
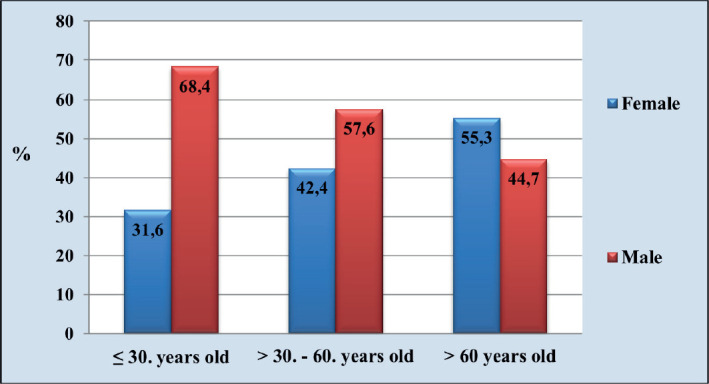
In the age group up to 30 years, there were 6 (31.6%) female patients and 13 (68.4%) of male patients. In the group of patients aged 30 to 60 years, there were 42 (42.4%) female patients and 57 of (57.6%) male patients. 73 (55.3%) female patients and 59 (44.7%) of male patients belonged to the age group of over 60 years old (Figure 1).
Analyzing the point prevalence of VAP, we found that pneumonia was present in 103 (41.2%) patients.. Of the total number of patients on MV with confirmed pneumonia, 53 (51.5%) patients were female, while 50 (48.5%) patients were male. Although higher, the prevalence of female patients with confirmed pneumonia did not differ statistically significantly from that of male patients (χ2 = 0.0194; p = 0.889).
The mean age of patients on MV in whom pneumonia was confirmed was 59.6 ± 16.8 years, with a minimum age of 19 and a maximum age of 90, while the mean age of patients on MV in whom pneumonia was not confirmed was 60.9 ± 16.9 years, with a minimum age of 14 and a maximum age of 91 . There was no statistically significant difference (p = 0.554) between the age of patients with MV in whom pneumonia was confirmed and those in whom it was not. The mean duration of MV in patients with confirmed pneumonia was 12.1 ± 14.4 days and was statistically significantly higher (p <0.0005) compared to the average duration of MV patients in whom pneumonia was not confirmed, which was 3.2 ± 3.3 days.
Female patients with confirmed pneumonia who were on MV had a mean age greater than the age of male patients, but the difference found was not statistically significant [60.8 ± 17.1 years vs. 58.4 ± 16.5 years; p = 0.458]. The youngest patient on MV with confirmed pneumonia was 19 and the oldest was 90 years old, while the youngest patient was 20 and the oldest was 85 years old.
The duration of MV in patients with female pneumonia was 14.0 ± 18.1 days and was higher, but not statistically significant (p = 0.163), compared to the duration of MV in male patients (10.1 ± 8.7 days).
Shortest mechanical ventilation in female patients with pneumonia lasted for 1 day and the longest for 120 days, while in male patients with pneumonia the shortest duration of MV was 2 and the longest was 45 days. Out of the total number of patients with pneumonia who were on MV, 9 or 8.7% of patients belonged to age group of up to 30 years old; in the group of patients older than 30 and up to 60 years old there were 41 (39.8%) of patients, while in the age group over 60 years there was the largest number of patients, 53 or 51.5%. The difference in the prevalence of patients with confirmed pneumonia who underwent MV in different age groups was statistically significant (χ2 = 18.87; p <0.0001). Tube smear analysis in patients with confirmed pneumonia who were on MV showed that the tube smear in 7 (6.8%) patients was sterile, while in 96 (93.2%) patients it was positive.
The most common causative agent isolated from tube swabs that was confirmed in 57 (59.4%) of patients with pneumonia who were on MV was Acinetobacter baumannii. Frequency of other isolates from various samples is shown in the Table 2, .
Table 2. Types and percentage of isolated pathogens of tube, cannula and bronchoalveolar fluid swabs of patients on MV causatives of VAP infection.
| Isolated microorganisms | Swab of tube % |
Swab of cannilla % |
Bronchoalveolar fluid % |
|---|---|---|---|
| Acinetobacter baumanni | 59.4 | 28.6 | 43.1 |
| Klebsiella pneumoni | 10.4 | 7.1 | 7.8 |
| Pseudomonas aeruginosa | 9.4 | 35.7 | 15.7 |
| Meticillin Resistent Staphylococus Aureus (MRSA) | 9.4 | - | 11.8 |
| Acinetobacter boumanni + Klebsiella pneumoniae | 4.2 | - | 7.8 |
| Acinetobacter boumani.+MRSA | 3.1 | 7.1 | - |
| Acinetobacter boumanni + Pseudomonas aeruginosa | 2.1 | 7.1 | 5.9 |
| Klebsiella pneumoniae + MRSA | 1.0 | - | - |
| Pseudomonas aeruginosa + MRSA | 1.0 | - | 2.0 |
| Pseudomonas aeru.+Klebsiella pneum.+MRSA | - | - | 3.9 |
| Acinetobacter b.+Pseudomonas aeru.+Klebsiella pn. | - | - | 2.0 |
| Pseudomonas aeruginosa+Klebsiella pneumonie | - | 14.3 | - |
| Total | 100 | 100 | 100 |
Analysis of cannula swab in patients with confirmed pneumonia who were on MV showed that cannula swab in 89 (86.4%) patients was sterile, while in 14 (13.6%) patients it was positive.
5. DISCUSSION
The causes of VAP are usually bacteria. The primary route of pathogen entry into the trachea is through the tube or by passage of bacteria around the cuff of endotracheal tube. The diagnosis of VAP in our study was made by microbiological processing of a sample taken from the patient’s airway. Laboratory-confirmed diagnosis of VAP was considered to be the isolation of bacteria from a sample of material obtained by tube swab, tracheal cannula, or bronchoaspiration. In our material, the most common causes of VAP were Acinetobacter, Klebsiella and Pseudomonas, alone or in combination with other bacteria. No statistically significant difference was found in the gender representation of patients who were on MV. It is known that the length of mechanical ventilation is directly related to the incidence of pneumonia. The mean duration of MV in patients included in our study was 6.9 ± 10.5 days. According to the results of our study, among the patients who underwent MV, there were (48.4%) female patients, while (51.6%) patients were male. We compared our results with those of other authors who had similar clinical trials. A similar result was found in the study by Sharpe et al. (4) with prolonged MV the incidence of VAP increases. The mean duration of MV in patients with confirmed pneumonia was 12.1 ± 14.4 days and it was statistically significantly higher than in patients without pneumonia (3.2 ± 3.3). No statistically significant difference in the duration of mechanical ventilation of patients of different sexes was found. The mean age of our patients on MV was 60.4 ± 16.8 years. A statistically significant difference was found in the prevalence of patients who underwent MV in different age groups. Most patients were in the group over 60 years with a percentage of 52.8%. In a study by Sharpe et al. the mean age of the subjects was 51.5 ± 19.5 years (4). Pawar et al. reported significant risk factors for VAP: coma, tracheostomy, reintubation, chronic obstructive pulmonary disease (COPD), steroid use, and enteral feeding. The most common isolated pathogens were Pseudomonas aerug., E. coli, Klebsiella pneumoniae, staphylococci, and Acinetobacter with a mortality rate of 16% (5). In a study by Gadani et al. the mortality rate of VAP patients was 29.72% (6). Rakshit et al. reported that half of the patients developed VAP due to Pseudomonas aeruginosa (7). In this study, significant risk factors for the development of VAP were impaired consciousness, re-intubation, emergency intubation, and existing co-morbidities. Joseph et al reported VAP incidence rates of 30.67 and 15.87 per 1000 days of ventilation in two different JINJs (8). Rello and co-workers studied the onset of VAP in the first 48 hours after intubation and pointed to an association between failure in attempts to disengage from MV and the incidence of VAP. They confirmed that frequent system changes during mechanical ventilation, types of humidifiers and methods of their application, are all associated with a more frequent incidence of VAP (9-11).
From the above data, we notice that the most common pathogen isolated from all microbiological analyzes is Acinetobacter baumanii. Acinetobacter baumanii as a multidrug-resistant form is sensitive only to Colistin (12). It is clear from everything that Acinetobacter baumannii is a growing worldwide health problem (13). Severe infections caused by A. baumannii and P. aeruginosa are also often treated with combination therapy, but unlike K. pneumoniae there is no convincing evidence that this achieves a better effect compared to monotherapy. The biggest benefit of combination therapy is that the antibiotic to which the pathogen is sensitive is more likely to be affected. The effect of combination therapy in the form of improved survival has been demonstrated in infections caused by K. pneumoniae, whereas for Acinetobacter and Pseudomonas there is insufficient evidence that any combination is better than monotherapy (14, 15). MV leads to the formation of VAP, but there is probably the possibility of ingestion of microorganisms indirectly through contamination by the action of health workers.
We can see that the results vary from study to study, so we cannot say with certainty whether the parameters of microbiological analysis and all isolated causes are good indicators that pneumonia will develop, but we call them potential causes of pneumonia. Additional research and analysis that will include more parameters and variables in the study should certainly be conducted on this topic.
Future research on this topic, which would include an even larger number of respondents over a longer period of research, would certainly give a more complete picture of it.
6. CONCLUSION
VAP is a relatively common complication in patients with MV that can increase morbidity and mortality as well as treatment costs. It is more common in females and the elderly. The most common causative agent isolated from tube swabs, cannulas, bronchoalveolar lavage fluid is Acinetobacter baumanii.
Patient Consent Statement:
The first author confirms that patients consent to enroll in the study was obtained. The authors certify that they have obtained all appropriate patient consent.
Author contribution:
The first author I.S. and D.A. have made significant contributions to the design, study design, data collection and analysis. I.S., M.T. and H.S. participated in the development of the work and the critical review of the content. Each author gave final approval of the version to be published and they are agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Final proof reading was made by the first author.
Conflict of interest:
There are no conflicts of interest.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Patil Harsha V, Patil Virendra C. Incidence, bacteriology, and clinical outcome of ventilator associated pneumonia at tertiary care hospital. J Nat Sci Biol Med. 2017;8(1):46–55. doi: 10.4103/0976-9668.198360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Damani NN. Priručnik o prevenciji i kontroli infekcije. IV izdanje. Medicinska naklada Zagreb. 2015:117–123. [Google Scholar]
- 3.Dudeck MA, Horan TC, Peterson KD, Allen-Bridson K, Morrell GC, Pollock DA, et al. National Healthcare Safety Network (NHSN) report, data summary for 2009, device associated module. Am J Infect Control. 2011;39:349–367. doi: 10.1016/j.ajic.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 4.Sharpe JP, Magnotti LJ, Weinberg JA, et al. Gender disparity in ventilator-associated pneumonia following trauma: identifying risk factors for mortality. J Trauma Acute Care. Surg. 2014;77(1):161–165. doi: 10.1097/TA.0000000000000251. [DOI] [PubMed] [Google Scholar]
- 5.Pawar M, Mehta Y, Khurana P, Chaudhary A, Kulkarni V, Trehan N. Ventilator-associated pneumonia: Incidence, risk factors, outcome, and microbiology. J Cardiothorac Vasc Anesth. 2003;17:22–28. doi: 10.1053/jcan.2003.4. [DOI] [PubMed] [Google Scholar]
- 6.Gadani H, Vyas A, Kar AK. A study of ventilator-associated pneumonia: Incidence, outcome, risk factors and measures to be taken for prevention. Indian J Anaesth. 2010;54:535–540. doi: 10.4103/0019-5049.72643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rakshit P, Nagar VS, Deshpande AK. Incidence, clinical outcome, and risk stratification of ventilator-associated pneumonia- A prospective cohort study. Indian J Crit Care Med. 2005;9:211–216. [Google Scholar]
- 8.Joseph NM, Sistla S, Dutta TK, Badhe AD, Parija SC. Ventilator-associated pneumonia in a tertiary care hospital in India: Incidence and risk factors. Eur J Inter Med. 2010;21:360–368. doi: 10.3855/jidc.396. [DOI] [PubMed] [Google Scholar]
- 9.Rello J, Diaz E, Roque M, et al. Risk factors for developing pneumonia within 48 hours of intubation. Am J Respir Crit Care Med. 1999;159:1742–1746. doi: 10.1164/ajrccm.159.6.9808030. [DOI] [PubMed] [Google Scholar]
- 10.Rello J, Sa-Borges M, Correa H, et al. Variations in etiology of ventilator- associated pneumonia across four treatment sites. Am J Respir Crit Care Med. 1999;160:608–613. doi: 10.1164/ajrccm.160.2.9812034. [DOI] [PubMed] [Google Scholar]
- 11.Rello J, Sonora R, Jubert P, et al. Pneumonia in intubated patients: role of respiratory airway care. Am J Respir Crit Care Med. 1996;154:111–115. doi: 10.1164/ajrccm.154.1.8680665. [DOI] [PubMed] [Google Scholar]
- 12.Lu Q, Luo R, Bodin L. Efficacy of high-dose nebulized colistin in ventilator-associated pneumonia caused by multidrug-resistant Pseudomonas aeruginosa and Acinetobacter baumannii. Anaesthesiology. 2012;117:1335–1347. doi: 10.1097/ALN.0b013e31827515de. i sur. [DOI] [PubMed] [Google Scholar]
- 13.Torres A, Carlet J. Ventilator- associated pneumonia. European Task Force on Ventilator-Associated Pneumonia. Eur Respir J. 2001;5:1034–1046. doi: 10.1183/09031936.01.17510340. [DOI] [PubMed] [Google Scholar]
- 14.Tamma PD, Cosgrove SE, Maragakis LL. Combination therapy for treatment of infections with Gram-negative bacteria. Clin Microbiol Rev. 2012;25:450–470. doi: 10.1128/CMR.05041-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Batirel A, Balkan II, Karabay O, et al. Comparison of colistin-carbapenem, colistin-sulbactam, and colistin plus other antibacterial agents for the treatment of extremely drug-resistant Acinetobacter baumannii bloodstream infections. Eur J Clin Microbiol Inf Dis. 2014;33:1311–1322. doi: 10.1007/s10096-014-2070-6. [DOI] [PubMed] [Google Scholar]


