Abstract
Aortic dilation has been increasingly recognized in congenital heart diseases, and aortic dissection is one of the important complications. We report a case of aortic dissection in a patient 31 years after repair of tetralogy of Fallot (TOF) and review reported cases. While aortic dissection is uncommon, aortic dilation is common among patients with repaired TOF and it appeared progressive in some patients. Based on the reported cases, progressive aortic dilation appeared as the pre-requisite for aortic dissection, although other factors might be involved. Regular surveillance and monitoring for aortic complications should be incorporated into clinical practice.
<Learning objective: Aortic dilation is common but aortic dissection is uncommon in patients with tetralogy of Fallot, and threshold for prophylactic surgery is lacking. Recognition of progressive aortic dilation is important to identify patients at risk of aortic dissection in tetralogy of Fallot.>
Keywords: Aortic dissection, Tetralogy of Fallot
Introduction
There has been increasing concern of aortic involvement in various congenital heart diseases especially in patients late after repair of tetralogy of Fallot (TOF) [1]. This appears more worrying when some patients develop serious complications such as aortic dissection [2], [3], [4], [5], [6], although the prevalence of aortic dissection in TOF appears low, with estimated prevalence of thoracic aortic dissection among repaired TOF patients to be 6 per 10,000 admissions [6]. Here we report our case of aortic dissection in a 35-year-old Chinese man 31 years after repair of TOF and review the cases reported in the literature.
Case report
The index patient, who was a chef, was diagnosed with TOF and underwent surgical repair involving infundibular resection via high transverse right ventriculotomy and closure of ventricular septal defect at 4 years of age. He remained asymptomatic after the operation and was followed up in our unit all along. He had serial cardiac magnetic resonance imaging (CMRI) as part of our protocol for long-term management of repaired TOF. The two CMRI performed at 29 years old and 32 years old respectively revealed mild dilation of right ventricle, satisfactory right ventricular systolic function, mild pulmonary regurgitation, but mild interval growth of aortic root dilation from 4.8 cm to 5.1 cm. Losartan was started in view of aortic root dilation. Holter monitoring at 32 years old revealed no significant arrhythmia. He has no microdeletion of 22q11.2 on polymerase chain reaction. It was as planned to monitor his aortic root closely, but he defaulted and stopped losartan. He returned for routine follow-up visit by 35 years of age and losartan was resumed. On enquiry, he reported no change in exercise tolerance and no palpitations. However, he reported intermittent chest discomfort in the past few months. His body weight and height were 72.6 kg and 176 cm respectively. Blood pressure was normal (114/64 mmHg). Transthoracic echocardiogram showed mildly dilated right atrium and right ventricle, good right ventricular systolic function, moderate pulmonary regurgitation, left ventricular size at upper limit of normal, and trileaflet aortic valve with moderate aortic regurgitation. The most striking findings included markedly dilated aortic root up to 7.96 cm and a flap-like structure within the aortic root. An urgent computed tomography (CT) was performed and revealed markedly dilated ascending aorta from the aortic root to the aortic arch with maximal dimension of 8.8 × 7.6 cm at the ascending thoracic aorta. A dissection flap was noted extending from just distal to the aortic valve to the descending thoracic aorta at the level of 9th thoracic vertebra (Fig. 1, Fig. 2). There was no extension of flap into the brachiocephalic, left common carotid artery and subclavian artery, all of which were supplied by true lumen. Both true and false lumen were well opacified. He showed no features of Marfan syndrome and there was no family history of hypertension or aortic dissection. Bentall operation was urgently performed. Intra-operatively a dissecting ascending aortic aneurysm with a tear just above the non-coronary cusp commissure was found, and both coronary ostia were intact. The operation was successful. Histology of the aortic valves showed myxoid degeneration and focal calcification. There is no evidence of infective endocarditis. Histology of the aortic wall showed a dissection flap, involving the outer third of the aortic wall. Alcian blue stain showed small pools of mucin within the elastic lamina, in keeping with mild cystic medial degeneration. The false lumen was lined by fibromuscular tissue, without elastic laminae. He made a satisfactory recovery after the operation. One year after Bentall operation, CT aortogram showed residual aortic dissection distal to the origin of the left subclavian artery to 8th thoracic vertebra level (Fig. 3). All brachiocepahalic vessels and mesenteric vessels were patent. Transthoracic echocardiogram showed good function of prosthetic aortic valve with no paravalvular leak. CMRI showed mildly dilated right ventricle with good right ventricular systolic function, mild pulmonary regurgitation, and normal left ventricular size and function.
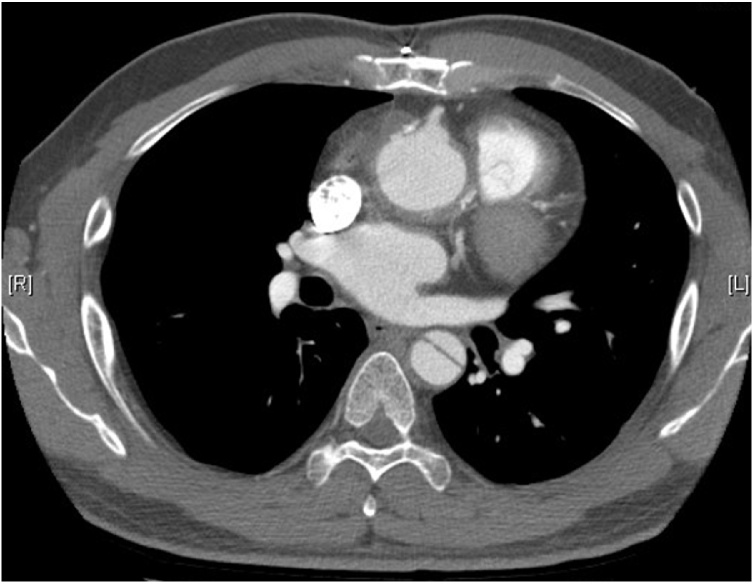
Fig. 1.
Computed tomography aortogram showing the dilated ascending aorta and the dissection flap.
Fig. 2.
Reformatted three-dimensional computed tomography aortogram showing the dilated ascending aorta.
Fig. 3.
Computed tomography aortogram showing neo-aortic root after Bentall operation.
Discussion
Aortic root dilation and aortic dissection have been recognized as one of the problems after TOF repair [1], [2], [3], [4], [5], [6]. Recently, Egbe et al. [6] estimated prevalence of thoracic aortic dissection among repaired TOF patients to be 6 per 10,000 admissions and mean age on admissions to be 49.8 ± 7.2 years, respectively, based on retrospective review of the National Inpatient Sample in the USA over 14 years. The associated risk factors were found to be: age >60 years, male sex, and hypertension. However, there were no data on the aortic dimension among those cases. On the other hand, to the best of our knowledge, there were 4 reported cases [2], [3], [4], [5] of aortic dissection after repair of TOF reported other than in the prevalence study [6] (Table 1). They were all male which was compatible with the prevalence study. On the contrary, the age of these 5 reported cases were younger (being less than 40 years of age) than that of 11 admissions reported in Egbe et al. [6]. Further, hypertension was not consistently found among these 5 patients. Other risk factors including bicuspid aortic valve, Marfan syndrome, and aortitis were all negative. There was one young patient with 22q11 deletion among the case reports.
Table 1.
Summary of case reports of aortic dilation and dissection in patients with repaired tetralogy of Fallot.
| Author, year of report / country | Sex/age | Duration after TOF repair | Associated conditions | Max AoR dimension preceding dissection | Max AoR dimension at presentation | Extent of dissection | Aortic root surgery | Outcome |
|---|---|---|---|---|---|---|---|---|
| Kim et al., 2005 / South Korea [2] | M/30y | 9y | – | N/A | 70.5 mm | Both iliac arteries | Bentall operation | Survived |
| Rathi et al., 2005 / United States [3] | M/36y | 30y | – | N/A | 93 × 83 mm | N/A | Unknown | Unknown |
| Konstantinov et al., 2010 / Australia [4] | M/18y | 18y | 22q11 deletion | N/A | 60 × 70 mm | RCCA | Valve-sparing aortic root replacement + resection of subaortic fibromuscular obstruction | Survived |
| Wijesekera et al., 2014 / Canada [5] | M/60y | 46y | Obese (BMI 33 kg/m2) | 53 mm (2 years before dissection) | 55 mm | Right coronary cusp | Bentall operation | Survived |
| Current report, 2019 / Hong Kong | M/35y | 31y | – | 51 mm (3 years before dissection) | 88 × 76 mm | DA at T9 level | Bentall operation | Survived |
Abbreviations: AoR, aortic root, CMD, cystic medial degeneration, DA, descending aorta, N/A, information not available, RCCA, right common carotid artery, T9, 9th thoracic vertebra.
Note: Bicuspid aortic valve, Marfan syndrome or aortitis have not been described in all these cases.
While aortic dimensions were not reported in the prevalence study, all the reported patients had significant aortic dilation at the time of dissection (60–93 mm) which might support that aortic dissection occurred in a dilated aortic root with abnormal wall stress. Furthermore, our case showed progressive dilation of aortic root from 48 mm to 51 mm over years. Similarly, Konstantinov et al. [4] also reported the aortic root dilation progressed over a few years in their patients although the rate was not mentioned. Therefore, regular assessment of aortic root dilation is recommended in view of its progressive nature. Although aortic root dilation has been well-recognized in repaired TOF, severe aortic complications and dissection were uncommon events as reflected by Egbe et al. [6] as well as the isolated case reports [2], [3], [4], [5].
The aortic dimension threshold for prophylactic aortic root surgery has been described in the guidelines for non-congenital degenerative heart disease [7], but not specified in the updated guidelines on congenital heart diseases [8], [9]. Therefore, watchful observation has been recommended [10]. Furthermore, many patients with repaired TOF might require surgical intervention of right ventricular outflow tract or residual ventricular septal defect which further confounded the decision and the timing of concomitant aortic surgery. In our case, the last aortic dimension was 51 mm before dissection and the progression rate was estimated to be 1 mm per year, in which aortic root replacement would not be considered. However, the patient defaulted follow-up for 3 years before dissection, and it is difficult to ascertain if there was sudden progression of aortic root dimension beyond 51 mm. Nevertheless, this might further suggest progressive aortic dilation as a pre-requisite for aortic dissection. Therefore, close monitoring of a progressively, albeit slowly, dilated aortic root in patients with repaired TOF should be exercised. It has been our institutional policy to routinely assess aortic root size by echocardiography or CMRI on a regular basis. Besides, counselling and educating patients on the potential progression of the disease is equally important to improve their adherence to follow-up appointments or assessments, and hence timely management.
Conclusion
Progressive aortic root dilation appeared preceding aortic dissection in repaired TOF. Assessment of aortic root size and patient education on aortic disease should be integrated as part of the follow-up management in patients with repaired TOF. Although the prevalence of aortic dissection appeared low, and the dissection threshold remained further refined, patients with repaired TOF and dilated aortic root, even though the progression rate is slow, should be regularly monitored.
Conflict of interest
The authors declare that there is no conflict of interest.
Acknowledgment
The author would like to thank Kenneth Ho for his clerical work in preparing the manuscript.
References
- 1.Mongeon F.P., Gurvitz M.Z., Broberg C.S., Aboulhosn J., Opotowsky A.R., Kay J.D. Aortic root dilatation in adults with surgically repaired tetralogy of Fallot: a multicenter cross-sectional study. Circulation. 2013;127:172–179. doi: 10.1161/CIRCULATIONAHA.112.129585. [DOI] [PubMed] [Google Scholar]
- 2.Kim W.-H., Seo J.-W., Kim S.-J., Song J., Lee J., Na C.-Y. Aortic dissection late after repair of tetralogy of Fallot. Int J Cardiol. 2005;101:515–516. doi: 10.1016/j.ijcard.2004.03.026. [DOI] [PubMed] [Google Scholar]
- 3.Rathi V.K., Doyle M., Williams R.B., Yamrozik J., Shannon R.P., Biederman R.W.W. Massive aortic aneurysm and dissection in repaired tetralogy of Fallot: diagnosis by cardiovascular magnetic resonance imaging. Int J Cardiol. 2005;101:169–170. doi: 10.1016/j.ijcard.2004.05.037. [DOI] [PubMed] [Google Scholar]
- 4.Konstantinov I.E., Fricke T.A., d’Udekem Y., Robertson T. Aortic dissection and rupture in adolescents after tetralogy of Fallot repair. J Thorac Cardiovasc Surg. 2010;140:e71–e73. doi: 10.1016/j.jtcvs.2010.06.045. [DOI] [PubMed] [Google Scholar]
- 5.Wijesekera V.A., Kiess M.C., Grewal J., Chow R., Raju R., Leipsic J.A. Aortic dissection in a patient with a dilated aortic root following tetralogy of Fallot repair. Int J Cardiol. 2014;174:833–834. doi: 10.1016/j.ijcard.2014.04.167. [DOI] [PubMed] [Google Scholar]
- 6.Egbe A.C., Crestanello J., Miranda W.R., Connolly H.M. Thoracic aortic dissection in tetralogy of Fallot: a review of the National Inpatient Sample Database. J Am Heart Assoc. 2019;8 doi: 10.1161/JAHA.119.011943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Erbel R., Aboyans V., Boileau C., Bossone E., Bartolomeo R.D., Eggebrecht H. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. Eur Heart J. 2014;35:2873–2926. doi: 10.1093/eurheartj/ehu281. [DOI] [PubMed] [Google Scholar]
- 8.Stout K.K., Daniels C.J., Aboulhosn J.A., Bozkurt B., Broberg C.S., Colman J.M. 2018 AHA/ACC guideline for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e698–e800. doi: 10.1161/CIR.0000000000000603. [DOI] [PubMed] [Google Scholar]
- 9.Kuijpers J.M., Mulder B.J.M. Aortopathies in adult congenital heart disease and genetic aortopathy syndromes: management strategies and indications for surgery. Heart. 2017;103:952–966. doi: 10.1136/heartjnl-2015-308626. [DOI] [PubMed] [Google Scholar]
- 10.Stulak J.M., Dearani J.A., Burkhart H.M., Sundt T.M., Connolly H.M., Schaff H.V. Does the dilated ascending aorta in an adult with congenital heart disease require intervention? J Thorac Cardiovasc Surg. 2010;140:S52–S57. doi: 10.1016/j.jtcvs.2010.08.052. [DOI] [PubMed] [Google Scholar]