Abstract
SGLT2 inhibitors are reported to have advantages in protecting against heart failure events. However, there are also reports of concerns when given to older persons or persons with geriatric syndrome. Our case is an example of a patient with a history of chronic thyroiditis where the SGLT2 inhibitor triggered a thyroid crisis, and blood catecholamine overload caused takotsubo cardiomyopathy and heart failure.
<Learning objective: SGLT2 inhibitor is a type of medicine for diabetes that has been used frequently. But if we are not careful about underlying disease and clinical course, it might lead to exacerbation of heart failure.>
Keywords: Thyroid crisis, SGLT2 inhibitor, Takotsubo cardiomyopathy, Heart failure
Introduction
SGLT2 inhibitors can protect against heart failure events [1]. However, there are also reports of concern when given to older persons or persons with geriatric syndrome as noted by the Japan Diabetes Society in “Recommendation on Proper Use of SGLT2 Inhibitors” [2]. SGLT2 inhibitors may cause dehydration, cerebral infarction, and diabetic ketoacidosis. Our case is an example of a patient with a history of chronic thyroiditis where the SGLT2 inhibitor triggered a thyroid crisis, and blood catecholamine overload caused takotsubo cardiomyopathy and heart failure.
Case report
This 83-year-old woman had hyperthroidism, hypertension, dyslipidemia, diabetes, and osteoporosis. Her family doctor managed these conditions with candesartan, alfacalcidol, raloxifene, simvastatin, linagliptin, alendronic acid, escitalopram oxalate, and pioglitazone. Pioglitazone was stopped two months previously due to lower leg edema, and trichlormethiazide and empagliflozin were newly added. One month previously, she had a urinary tract infection, and was given levofloxacin for about 1 week. Her other medications remained unchanged, including empagliflozin.
Although her urinary tract infection improved, she suffered from anorexia, malaise, and went to see her family doctor. She was diagnosed with hyperthyroidism and prescribed mercazole. However, she could not take the medication. Furthermore, there was hyperglycemia, a depressed level of consciousness, and abnormalities in cardiac contraction in the electrocardiogram. At this point, she was referred to our hospital.
Admission studies: JCS II – 30, body temperature 37.3℃, blood pressure 122/80 mmHg, pulse rate 128 beats/minute (regular), SPO2 95% (room air), no swelling of the jugular vein, no pale conjunctiva, no enlarged thyroid, no heart murmur, respiratory sounds clear, no rales. No cold sensation from limbs, no leg edema, had reduced skin turgor.
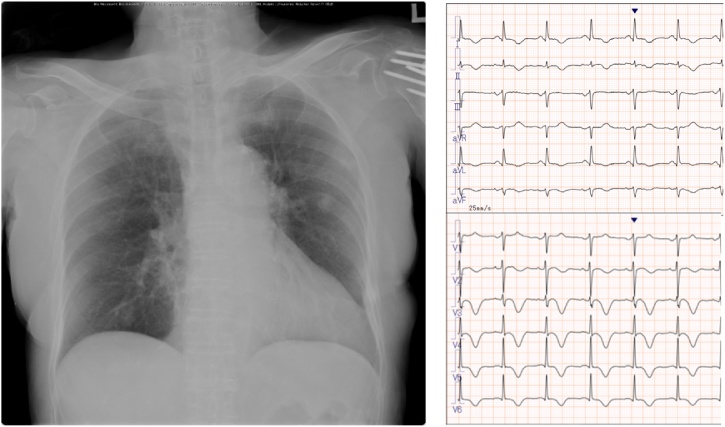
Chest X-ray: cardiothoracic ratio 53%, no congestion, no pleural fluid. 12-Lead electrocardiogram (ECG): heart rate 130/min, sinus rhythm. ST elevation was observed in ll, lll, aVf, V3, V4, and a negative T wave was observed in V4-V6 (Fig. 1).
Fig. 1.
There was no pneumonitis, congestion, or pleural effusion seen on chest X-rays and 12-lead electrocardiogram at admission.
Blood test: mild elevation of creatine phosphokinase and creatine phosphokinase MB, high N-terminal pro-brain natriuretic peptide, troponin T negative, and hyperthyroidism. In addition, there was significant metabolic acidosis with blood gas. Urinary sugar 4+ and ketone bodies 3 + . Later examination found thyrotrophin receptor antibody (-), high thyroid peroxidase antibodies, thyroglobulin antibodies (+), and all three fractions for blood catecholamine were at a high level. Bedside echocardiography: akinesis in the apex and overcontraction in the base and the ejection fraction was about 30%. There were no abnormal findings in the head computed tomography (CT) scan. There were no abnormal findings in the thyroid gland, no congestion, and no pleural effusion from the chest CT scan. Neither pneumonia nor other inflammatory findings were observed.
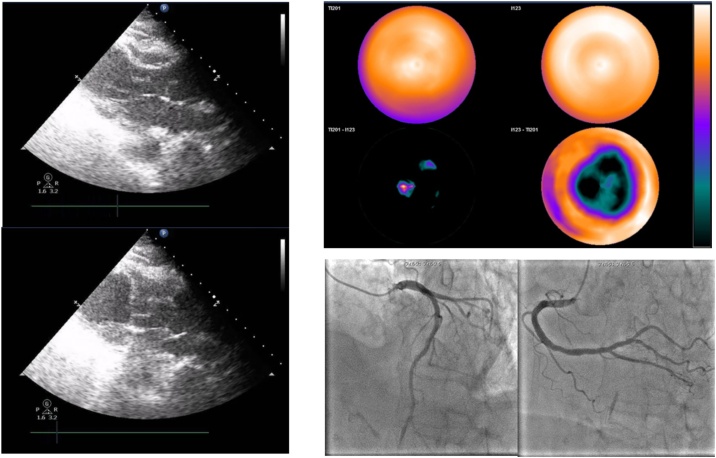
Additional tests at a later date: Thallium/123I-β-methyl-P-iodophenyl-pentadecanoic acid (Tl/BMIPP) dual myocardial scintigraphy: BMIPP mismatch accumulation at the apex (day 16). Coronary catheterization: no significant stenosis (day 35) (Fig. 2).
Fig. 2.
There was non-contraction of the heart apex and over-contraction of the heart base seen by transthoracic echocardiogram (right). There was 〈123〉I-BMIPP in a deficient image with reduced accumulation around the apex and metabolic/blood flow mismatch was detected by 〈201〉TI/〈123〉I-BMIPP dual myocardial single photon emission computed tomography and no coronary stenosis on angiography (left).
A diagnosis of thyrotoxic crisis was made based on increasing free triiodo thyronine and free thyroxine, neurologic symptoms (II-30), tachycardia, cardiac insufficiency, and digestive symptoms. A diagnosis of diabetic ketoacidosis (DKA) was made based on hyperglycemia, progression acidemia, positive keton from urinary analysis, and lower bicarbonate levels. Takotsubo cardiomyopathy was diagnosed from characteristic wall motion, no coronary stenosis, and TI/BMIPP mismatch accumulation (Fig. 2). The emergency cardiac catheterization on the admission day was suspended due to concerns for exacerbation of the thyroid crisis as a result of using the iodine contrast agent (Table 1).
Table 1.
Laboratory findings at admission.
| [Complete blood cell count] | ||
| WBC | 17900 | /μl |
| Neut | 90 | % |
| HGB | 13.1 | g/dl |
| PLT | 29.3^104 | /μl |
| [Biochemistry] | ||
| Na | 147 | mEq/l |
| K | 3.5 | mEq/l |
| AST | 56 | U/L |
| ALT | 35 | U/L |
| LDH | 236 | U/L |
| AMY | 510 | U/L |
| CK | 315 | U/L |
| CK-MB | 42 | U/L |
| BUN | 50.2 | mg/dl |
| Cr | 0.72 | mg/dl |
| eGFR | 57.8 | ml/min/l |
| UA | 13.5 | mg/dl |
| T-Bil | 0.3 | mg/dl |
| CRP | 2.19 | mg/d |
| PCT | 0.52 | ng/mL |
| TP | 7.3 | g/dl |
| Alb | 3.9 | g/dl |
| T-cho | 148 | mg/dl |
| LDL | 89 | mg/dl |
| NT-pro BNP | 17637 | pg/mL |
| Troponin T | (+) | |
| Glu | 352 | mg/dl |
| HbA1c | 9.1 | % |
| FT3 | 4.21 | pg/mL |
| FT4 | 2.59 | ng/dl |
| TSH | 0.01 | μIU/mL |
| TRAb | <0.8 | IU/L |
| TPOAb | 38.7 | IU/mL |
| TGAb | 2518 | IU/mL |
| AD | 243 | pg/mL |
| NAD | 1293 | pg/mL |
| DP | 89 | pg/mL |
| [Blood gas] | ||
| PH | 7.26 | |
| pCO2 | 29.4 | mmHg |
| pO2 | 44.4 | mmHg |
| HCO3 | 12.7 | mmol/L |
| BE | −12.9 | mmol/L |
| Lac | 1.8 | mmol/L |
| [Urinalysis] | ||
| Protein | (-) | |
| Ketone body | (3+) | |
| Glu | (4+) | |
| Nitrous acid | (-) | |
| WBC | (-) | |
WBC, white blood cell; Neut, neutrophil; HGB, hemoglobin concentration; PLT, platelet; AST, aspartate aminotransferase; ALT, alanine aminotransferase; LDH, lactate dehydrogenase; AMY, amylase; CK, creatine phosphokinase; CK-MB, creatine phosphokinase MB; BUN, blood urea nitrogen; Cr, creatinine; eGFR, estimated glomerular filtration rate; UA, uric acid; T-Bil, total bilirubin; CRP, C-reactive protein; PCT, procalcitonin; TP, total protein; Alb, albumin; T-cho, total cholesterol; LDL, low-density lipoprotein; NT-pro BNP, N-terminal pro-brain natriuretic peptide; Glu, glucose; HbA1c, hemoglobin A1c; FT3, free triiodo thyronine; FT4, free thyroxine; TSH, thyroid stimulating hormone; TRAb, thyrotrophin receptor antibody; TPOAb, thyroid peroxidase antibody; TGAb, thyroglobulin antibody; AD, adrenaline; NAD, noradrenaline; DP, dopamine; BE, base excess; Lac, lactate.
Progress
Insulin and sodium bicarbonate were given to adjust blood sugar level and acidemia. In addition, potassium iodide and mercazole were given. At the same time, bisoprolol and landiolol were also given. It was necessary to provide massive fluid replacement to correct dehydration, hyperglycemia, and acidosis. The chest X-ray showed exacerbation in blood congestion and pleural fluids temporarily due to abnormal cardiac wall motion and low cardiac function. However, after additional medications, such as diuretics, the patient's condition did not turn more critical, and the level of consciousness slowly improved. While there were inverted T waves at Ⅱ, aVf, V3, and a remarkable giant negative T wave was seen in V4-V6 on the 12 lead ECG, heart wall motion became normal on the 3rd day of hospitalization. So we were able to control the heart failure and the patient was transferred on the 44th day of hospitalization.
Discussion
The European Society of Cardiology (ESC) reported that SGLT2 inhibitors are effective against heart failure [1], and we were fully aware of the patient's medical history and past treatment and needed to take care of this process after medication. It is said that takotsubo cardiomyopathy often occurs more frequently in postmenopausal women [3].
Especially with the coexistence of thyroid disease, as in this case, it is possible to trigger a thyrotoxic crisis, and the high level of stress from this will bring about takotsubo cardiomyopathy and cause heart failure.
Thyroid disease can be related to takotsubo cardiomyopathy, and 17.7% of takotsubo cardiomyopathy is related to thyroid disease, and of these, 5.9% were due to hyperthyroidism and 11.8% were due to hypothyroidism [4]. In particular, for the elderly, there have also been cases where there was no presentation of typical thyrotoxicosis symptoms and thus caution is warranted [5]. Chronic thyroiditis is in many cases asymptomatic during normal times, and does not require continuous treatment and so it is an easily forgotten disease. However, it is well known to cause thyroid poisoning due to transient indolent thyroiditis, and the recurrence rate is high [6].
Moreover, in thyroid crisis, some sort of stress is added to this thyrotoxicosis, which is a condition that breaks the compensation mechanism of the living body and a condition in which multiple organs malfunction. It is reported that without intervention, lethality is 50-90% [7], and even with early intervention, the fatality rate is 20–30% [8], [9]. Even in a single disease state of thyroid crisis, it is a critical situation. In general, the cause of thyroid crisis is cited with direct incentives and indirect incentives, and DKA is also one of these indirect incentives [10].
In this case, the SGLT2 inhibitor was started two months previously, and as such this drug did not cause takotsubo cardiomyopathy or heart failure directly. However, if a patient has a history of thyroid disease, it is possible to consider that a SGLT2 inhibitor would cause urinary tract infection, dehydration, DKA, and trigger a thyroid crisis.
Conclusion
We report on this clinical course because SGLT2 inhibitors will increasingly be a key drug that are frequently used to treat heart failure and diabetes, and careful observation and administration is warranted for geriatric syndrome patients, aged between 65 and 74 years, because they may go through a lethal clinical course depending on past history.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.McMurray J.J.V., DeMets D.L., Inzucchi S.E., Køber L., Kosiborod M.N., Langkilde A.M. A trial to evaluate the effect of the sodium-glucose co-transporter 2 inhibitor dapagliflozin on morbidity and mortality in patients with heart failure and reduced left ventricular ejection fraction (DAPA-HF) Eur J Heart Fail. 2019;21:665–675. doi: 10.1002/ejhf.1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Committee on the Proper Use of SGLT2 Inhibitors Recommendations on the proper use of SGLT2 inhibitors. Diabetol Int. 2019;11:1–5. doi: 10.1007/s13340-019-00415-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bybee K.A., Prasad A. Contemporary reviews in cardiovascular medicine: stress-related cardiomyopathy syndromes. Circulation. 2008;118:397–409. doi: 10.1161/CIRCULATIONAHA.106.677625. [DOI] [PubMed] [Google Scholar]
- 4.Templin C., Ghadri J.R., Diekmann J., Napp L.C., Bataiosu D.R., Jaguszewski M. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med. 2015;373:929–938. doi: 10.1056/NEJMoa1406761. [DOI] [PubMed] [Google Scholar]
- 5.Al-Salameh A., Allain J., Meimoun P., Benali T., Desailloud R. Takotsubo cardiomyopathy can occur in patients with apathetic hyperthyroidism. Thyroid. 2014;24:400–401. doi: 10.1089/thy.2013.0354. [DOI] [PubMed] [Google Scholar]
- 6.Ozawa Y. Painless (silent) thyroiditis. Nihon Rinsho. 1999;57:1770–1774. (In Japanese) [PubMed] [Google Scholar]
- 7.Fisher J.N. Management of thyrotoxicosis. South Med J. 2002;95:493–505. [PubMed] [Google Scholar]
- 8.Tietgens S.T., Leinung M.C. Thyroid storm. Med Clin North Am. 1995;79:169–184. doi: 10.1016/s0025-7125(16)30090-6. [DOI] [PubMed] [Google Scholar]
- 9.Jameson L., Weetman A. Disorders of the thyroid gland. In: Brawnwald E., Fauci A., Kasper D., editors. Herrison’ principles of internal medicine. 15th edition. McGraw-Hill; New York: 2001. pp. 2060–2084. [Google Scholar]
- 10.Griffiths S., Peak D., Bridwell R.E., Long B. Thyroid storm and diabetic ketoacidosis presenting to the emergency department. Cureus. 2020;12:e6751. doi: 10.7759/cureus.6751. [DOI] [PMC free article] [PubMed] [Google Scholar]