Abstract
A sigmoid septum is a state of angulation between the basal interventricular septum and the ascending aorta. Although considered to have no clinical importance, it may cause left ventricular outflow tract obstruction (LVOTO) in a hypercontractile state. Percutaneous transluminal septal myocardial ablation (PTSMA) is a catheter-based therapy aimed at improving drug-refractory symptoms in patients with hypertrophic obstructive cardiomyopathy. Few studies have reported the use of PTSMA for patients with LVOTO caused by sigmoid septum.
We present a successful case of a 71-year-old female patient who presented with a long history of exertional dyspnea. The presence of a sigmoid septum was revealed on echocardiography. At rest, the left ventricular outflow tract pressure gradient was low and there were no signs of systolic anterior motion (SAM) of the mitral valve; however, during Valsalva maneuver, the gradient increased significantly, and SAM could be seen. We successfully performed PTSMA, resulting in a significant lowering of the pressure gradient and disappearance of SAM. The patient’s symptoms dramatically improved by the following day.
<Learning objective: In some clinical settings, left ventricular outflow tract obstruction caused by sigmoid septum results in cryptogenic exertional dyspnea. This case highlights the importance of an accurate diagnosis through Valsalva maneuver during echocardiogram and demonstrates the effectiveness of percutaneous transluminal septal myocardial ablation for symptomatic sigmoid septum.>
Keywords: Left ventricular outflow tract obstruction, Sigmoid ventricular septum, Percutaneous transluminal septal myocardial ablation
Introduction
A sigmoid septum is a state of angulation between the basal interventricular septum and the ascending aorta, and is considered to have no clinical importance [1]; however, it may cause left ventricular outflow tract obstruction (LVOTO) in a hypercontractile state. Percutaneous transluminal septal myocardial ablation (PTSMA) is a catheter-based therapy aimed at improving drug-refractory symptoms in patients with hypertrophic obstructive cardiomyopathy (HOCM) [2]. Nonetheless, few studies have reported the effectiveness of PTSMA in patients with LVOTO caused by sigmoid septum. In the current report, we present the case of a patient who was successfully treated using this procedure.
Case report
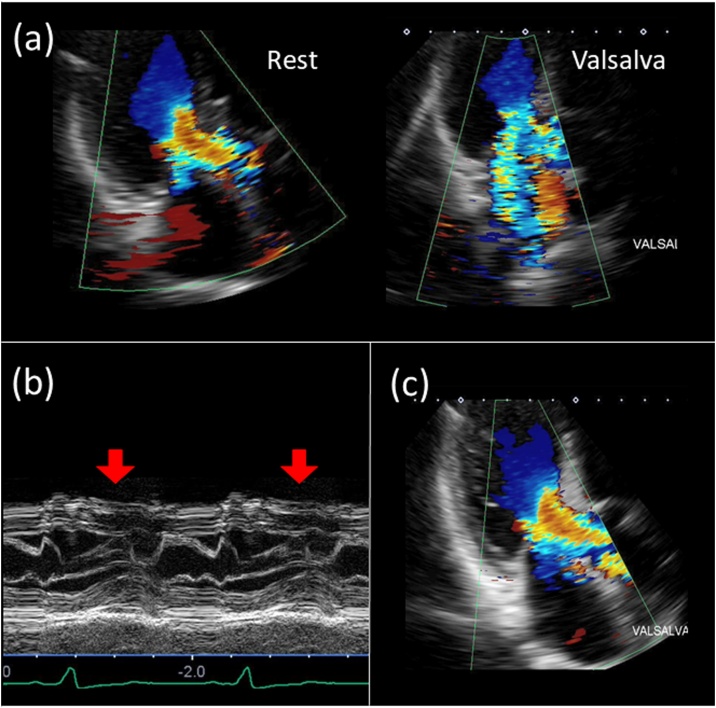
A 71-year-old woman presented to our hospital with a long history of exertional dyspnea of unknown cause on climbing the stairs or having a shower [New York Heart Association (NYHA) class III]. Her previous medical history included hypertension and dyslipidemia and she had a pacemaker which was implanted for complete atrioventricular block. She was taking losartan 25 mg daily, amlodipine 2.5 mg daily, verapamil 40 mg daily, and rosuvastatin 2.5 mg daily and had no family history of heart disease. Her serum B type natriuretic peptide level was 87.2 pg/mL, and chest X-ray revealed no signs of pulmonary edema or pleural effusion. A transthoracic echocardiogram showed almost normal left ventricular function (left ventricular ejection fraction of 58%, no asynergy), no sign of left ventricular hypertrophy, and the presence of a sigmoid septum. Left ventricular outflow tract (LVOT) pressure gradient was 10.4 mmHg and there were no signs of systolic anterior motion (SAM) of the mitral leaflet at rest. However, during Valsalva maneuver, the gradient increased to 85.2 mmHg and severe mitral regurgitation (MR) occurred with a significant SAM of the mitral leaflet (Fig. 1a and b). We discontinued amlodipine and verapamil, and initiated bisoprolol 1.25 mg daily, but no significant symptomatic relief was observed. A decision to perform PTSMA was therefore made. Written informed consent was obtained from this patient before PTSMA procedure.
Fig. 1.
Echocardiographic findings before and after procedure. (a) Transthoracic echography at rest and during Valsalva maneuver. At rest, there were no signs of mitral valve regurgitation (MR), but severe MR appeared during Valsalva maneuver. (b) M-mode shows systolic anterior motion. (c) MR dramatically improved immediately after the procedure.
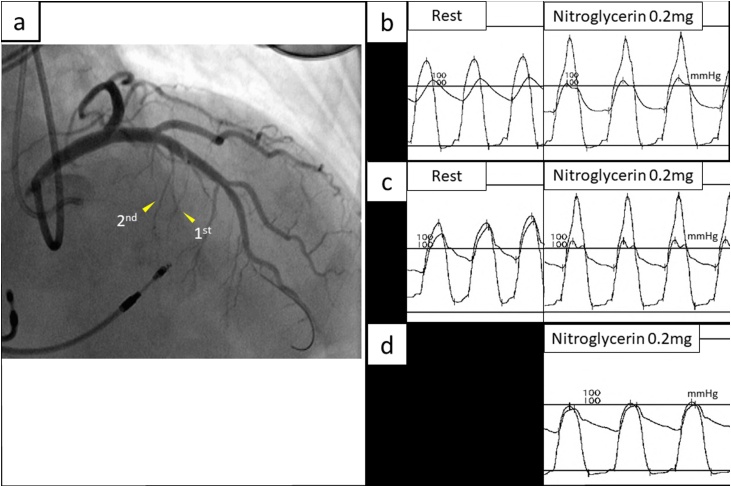
Prior to the procedure, because her ventricle lead was implanted to the right ventricular mid-septum, a temporary pacemaker was inserted at the apex of the right ventricle in anticipation for atrioventricular block. Her coronary angiography showed several septal branches which could be potential candidates for PTSMA (Fig. 2a). We measured LVOT pressure gradient by inserting a pressure wire into the left ventricle. Although the gradient was 56 mmHg at rest, it eventually increased to 134 mmHg after nitroglycerine loading (0.2 mg) (Fig. 2b). A contrast echocardiogram was performed to identify adequate septal branch; we inflated an over-the-wire balloon within the septal branch followed by an injection of echo contrast consisting of a combination of carbon dioxide gas and iodine contrast agent. After confirming enhancement of the target area by echo contrast, we performed the first ablation using 0.5 mL of absolute ethanol (Fig. 2a). Although the gradient was reduced to 19 mmHg at rest, it subsequently increased to 69 mmHg after 0.2 mg nitroglycerin loading (Fig. 2c). A second ablation was therefore performed. We injected 0.3 mL of absolute ethanol into another septal branch. After nitroglycerin loading, the pressure gradient was reduced to 4 mmHg (Fig. 2d), and the procedure was concluded.
Fig. 2.
Coronary angiogram and peri-procedural aorta-left ventricular pressure gradient. (a) Coronary angiogram. The targets of the first ablation and second ablation are shown with the arrows. (b) Aorta-left ventricular pressure gradient measured by pressure wire before percutaneous transluminal septal myocardial ablation procedure (56 mmHg at rest and 134 mmHg after nitroglycerin loading). (c) The pressure gradient after the first ablation (19 mmHg at rest and 69 mmHg after nitroglycerin loading). (d) The pressure gradient after the second ablation (4 mmHg after nitroglycerin loading).
A postoperative transthoracic echocardiogram demonstrated a 13.0 mmHg LVOT pressure gradient during Valsalva maneuver, without evidence of SAM, and MR was significantly reduced to trivial (Fig. 1c). The patient’s symptoms dramatically improved by the following day, and she could climb the stairs and shower without experiencing dyspnea (NYHA class I). Up until at least 6 months following the procedure, the patient was free of exertional dyspnea.
Discussion
A sigmoid septum is a morphological change characterized by a diminished angle between the basal interventricular septum and the ascending aorta. This cardiac malformation has been considered to happen as a result of aging, and has no pathophysiologic and clinical significance [3], [4]; however, it can sometimes cause LVOTO in clinical settings such as catecholamine excess, exercise overload, sympathetic activation, anemia, and dehydration [5].
Although a number of patients suffer from this functional abnormality, medical or catheter therapies for sigmoid septum are not well established. A previous report indicated that a class Ia antiarrhythmic drug, cibenzoline, attenuates LVOT pressure gradient in patients with sigmoid septum [6], however adverse events of the drug such as fatal arrhythmias and hypoglycemia are sometimes critical in elderly patients. Therefore, PTSMA, a safer and less invasive catheter therapy, may be useful in the treatment of LVOTO caused by sigmoid septum.
Since LVOT pressure gradient in patients with sigmoid septum is usually absent or very low at rest, making a correct diagnosis is often challenging. The cause of the symptoms experienced by our patient was unclear for a long time. Therefore, it is important to perform echocardiography in the setting of decreased preload and hypercontractile ventricular state. The Valsalva maneuver is a simple and safe traditional method which works by increasing intrathoracic pressure and reducing venous return; a reduced preload subsequently narrows the LVOT, resulting in dynamic obstruction. However, this maneuver is not always physiological and requires patients’ understanding and cooperation during the procedure, which is sometimes difficult especially for older patients. In addition, we have to be careful for the patients who need to avoid sympathetic nervous activation, such as aortic dissection or abnormal high blood pressure. Therefore, in this case, we performed nitroglycerin loading test to reduce preload and afterload during the PTSMA procedure. Although this method is uncommonly used, it can be a simple, rapid, and reproducible method because of the short-acting and definite characteristics of nitroglycerin. In the echocardiogram room, however, this method carries a risk of hemodynamic collapse caused by abnormal intraventricular flow dynamics, known as ‘suicide left ventricle’ [7].
LVOTO occurs not only due to HOCM but also due to other conditions such as sigmoid septum, post mitral surgery, takotsubo cardiomyopathy, and sub-aortic membrane. Kobayashi et al. reported the changes of LVOT pressure gradient with various conditions, and the rate of sigmoid septum in the patients with LVOTO was only 4% (3/73) [8]. In the report, almost all patients with LVOTO were treated by a combination of negative inotropic agents such as disopyramide or antiarrhythmic agents with and without β-blockers. However, despite the treatment with multiple negative inotropic agents, patients with sigmoid septum tended to have greater residual pressure gradient than other conditions, which may imply the necessity for safer and effective treatment options for patients with LVOTO due to sigmoid septum.
There is little information about the comparison of the effect of PTSMA between patients with HOCM and sigmoid septum. Veselka et al. reported mid-term outcomes of alcohol septal ablation for HOCM in patients with sigmoid versus neutral ventricular septum [9]. Although the delta pressure gradients did not differ between these two groups, the total alcohol volume and the number of ablated branches were lower in the sigmoid septum group. Although still speculative, we currently consider that morphological differences between HOCM and sigmoid septum might explain somewhat different procedural characteristics between them. In general, the heart with sigmoid septum usually has thinner basal septum than that with HOCM. Also, the heart with sigmoid septum usually has a short-range, focal obstruction in LVOT. As a result, the amount of myocardium causing intraventricular obstruction might be smaller than that of HOCM. Therefore, we currently speculate that PTSMA might be more effective for patients with LVOTO due to sigmoid septum than for those with HOCM. Further investigation will be necessary to confirm our speculation.
Sigmoid septum, often seen in elderly patients, has become a common finding in this aging population. Appropriate diagnosis of LVOTO caused by sigmoid septum, may enable symptom alleviation through the PTSMA procedure.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.Hioki H., Izawa A., Miura T., Motoki H., Aizawa K., Koshikawa M. Dynamic left ventricular outflow tract obstruction due to anemia in a 71-year-old patient with sigmoid septum. J Cardiol Cases. 2010;1:e144–e146. doi: 10.1016/j.jccase.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maekawa Y., Akita K., Takanashi S. Contemporary septal reduction therapy in drug-refractory hypertrophic obstructive cardiomyopathy. Circ J. 2018;82:1977–1984. doi: 10.1253/circj.CJ-18-0575. [DOI] [PubMed] [Google Scholar]
- 3.Goor D., Lillehei C.W., Edwards J.E. The ‘sigmoid septum’: variation in the contour of the left ventricular outlet. Am J Roentgenol Radium Ther Nucl Med. 1969;107:366–376. [PubMed] [Google Scholar]
- 4.Toth A.B., Engel J.A., McManus A.M., McManus B.M. Sigmoidity of the ventricular septum revisited: Progression in early adulthood, predominance in men, and independence from cardiac mass. Am J Cardiovasc Pathol. 1988;2:211–223. [PubMed] [Google Scholar]
- 5.Auer J., Berent R., Weber T., Lamm G., Eber B. Catecholamine therapy inducing dynamic left ventricular outflow tract obstruction. Int J Cardiol. 2005;101:325–328. doi: 10.1016/j.ijcard.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 6.Konishi C., Shiraishi J., Muraguchi N., Ohtsuki K., Inoue M., Tatsumi T. Beneficial effect of cibenzoline on left ventricular pressure gradient with sigmoid septum. Circ J. 2004;68:968–971. doi: 10.1253/circj.68.968. [DOI] [PubMed] [Google Scholar]
- 7.Bartunek J., Sys S.U., Rodrigues A.C., van Schuerbeeck E., Mortier L., de Bruyne B. Abnormal systolic intraventricular flow velocities after valve replacement for aortic stenosis mechanisms, predictive factors, and prognostic significance. Circulation. 1996;93:712–719. doi: 10.1161/01.cir.93.4.712. [DOI] [PubMed] [Google Scholar]
- 8.Kobayashi S., Sakai Y., Taguchi I., Utsunomiya H., Shiota T. Causes of an increased pressure gradient through the left ventricular outflow tract: a West Coast experience. J Echocardiol. 2018;16:34–41. doi: 10.1007/s12574-017-0352-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Veselka J., Tomasov P., Zemánek D. Mid-term outcomes of alcohol septal ablation for obstructive hypertrophic cardiomyopathy in patients with sigmoid versus neutral ventricular septum. J Invasive Cardiol. 2012;24:636–640. [PubMed] [Google Scholar]