Abstract
Diabetic retinopathy (DR) is the leading cause of legal blindness in the United States. Considering the increasing incidence of DR, it is extremely important to detect the most cost-effective tools for DR screening, so as to manage this surge in demand and the socioeconomic burden it places on the health care system. Despite the advances in retinal imaging, analysis techniques are still superseded by expert ophthalmologist interpretation. Teleophthalmology presents an immense opportunity, with high rates of sensitivity and specificity, to manage the steadily increasing demand for eye care of patients with diabetes, but challenges remain in the delivery of practical, viable, and clinically proven solutions.
Keywords: Diabetic retinopathy, Screening, Teleophthalmology
Abstract
La retinopatía diabética (RD) es la causa principal de ceguera legal en los Estados Unidos. Teniendo en cuenta la creciente incidencia de RD, es extremadamente importante detectar las herramientas más económicas para su cribado, para poder gestionar esta demanda creciente, así como la carga socioeconómica que supone para el sistema sanitario. A pesar de los avances en términos de imagen retiniana, las técnicas de análisis siguen siendo reemplazadas por la interpretación de los oftalmólogos expertos. La tele-oftalmología se presenta como una gran oportunidad, con altas tasas de sensibilidad y especificidad, para gestionar el aumento constante de la atención ocular en los pacientes diabéticos, aunque la aportación de soluciones clínicamente probadas sigue suponiendo un reto.
Palabrasclave: Retinopatía diabética, Cribado, Tele-oftalmología
Introduction
According to the American Telemedicine Association, Telemedicine is defined as the “the use of medical information exchanged from one site to another via electronic communications to improve a patient’s health status”.1 Due to the increasing needs for more accessible, financially affordable and effective health-care services, telemedicine has emerged as an alternative method for the assessment of specialized evidence-based approach, which can be offered in a cost-effective manner especially in underserved and remote populations. Taking into account that the estimated number of diabetics projected to reach 642 million by the year 2040,2 the incidence of ocular complications secondary to diabetes is also expected to increase substantially. Historically, current screening strategies for detecting diabetic retinopathy (DR) have poor compliance, but technological development can enhance access to care. Establishing mechanisms to overcome geographic and financial barriers to access is vital for preventing visual disability.3 The burden of implying immediate and cost-effective screening for patients with diabetic retinopathy (DR) via distant imaging of the retina has become one of the most widely used applications of telemedicine in Ophthalmology.4
The concept of teleophthalmology for the screening and management of patients with diabetic retinopathy
DR consists a leading cause of blindness all over the world, especially in the working-age population of developed countries.2 It must be underlined though that early detection and timely intervention can contribute in preventing the diabetes-related ocular complications.5 Lifelong routine retinal evaluation in combination with appropriate treatment have reduced the risk of severe loss of vision to less than 2% per person and 4% per eye. Typically, the retinal evaluation of eyes with DR is based on an in-person assessment with an eye care specialist and fundoscopy through dilated pupils. The purpose of the examination is to assess the severity of DR by detecting retinal lesions and provide clinicians adequate information in order to decide about the required therapeutic interventions and organize an appropriate follow-up. As can be inferred, due to the immense increase of the global number of patients with diabetes mellitus, the time investment needed from every ophthalmologist (in order to evaluate all diabetics at least once annually) will also rise exponentially over the next few years.6 Therefore, it appears that the concept of in-person examinations is neither practical nor sustainable in the settings of modern health care. Even if government and non-governmental agencies provide increased support, a large proportion of patients with DR will not receive the recommended minimum of an annual eye examination.7, 8 A wide spectrum of psychological, social, medical and financial parameters (need for pupil dilation, patient’s age, educational status, health insurance coverage, transportation costs, poor patient awareness, and limited access to eye care services) can affect the effective implementation of recommended screening guidelines.7, 8, 9, 10, 11, 12 Interestingly, even in urban areas with easier access to specialized eye care, the annual DR screening appointments can be missed due to the lack of awareness, the struggle in booking appointments and the long waiting times.10, 13, 14 The difficulty of adherence to the recommended annual retinal assessment of diabetics has been recorded in all socio-economic levels.9 The importance of routine retinal evaluations to identify eyes at risk for visual loss was recognized by eye care providers approximately 40 years ago. Nowadays, the diabetes-related visual loss affects significant rates of the population causing continuous strain at the health care systems. Although the traditional in-person strategy remains essential it may not be enough to meet the minimum standards for preventing visual loss. Therefore, the needs of modern health care call for an immediate modification in the overall approach of DR evaluation and for this reason the health systems have started using tele-ophthalmology to address this issue.4 Several studies from different countries have indicated that the implementation and use of telematic screening can be successful from patient, caregiver, and authorities’ point of view.15, 16, 17, 18, 19, 20 Characteristically, Park and Mansberger reported the results of a multicenter randomized clinical trial that compared the effectiveness of telemedicine with non-mydriatic cameras to the traditional care by eye care providers. They underlined that telemedicine with non-mydriatic cameras detected diabetic retinopathy, as well as other visually significant eye disease, such as glaucoma or vascular occlusions.21
Remote retinal imaging: accuracy and reliability
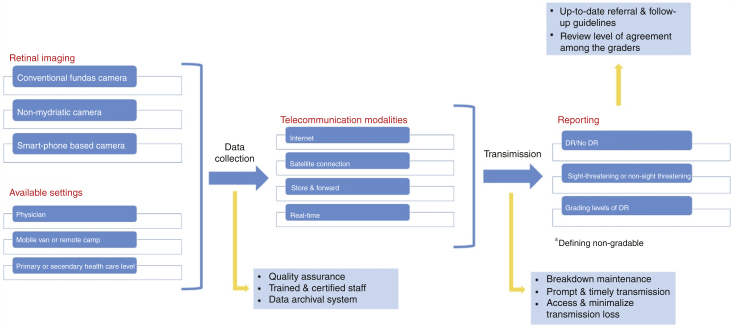
Tele-ophthalmology programs have facilitated the identification of DR cases by utilizing digital retinal imaging22, 23 [Fig. 1]. Several studies have shown that the sensitivity (62.5%–98.2%) and specificity (76.6%–98.7%) of tele-ophthalmology in diagnosing DR are comparable to those of the traditional clinical examinations.24, 25 Boucher et al.9 studied 291 cases of diabetic patients who underwent DR screening using a non-mydriatic camera and clinical examination (complete ophthalmological examination and dilated fundoscopy) in a community-based population. The fundus photographs were transmitted to the hospital server through the File Transfer Protocol (FTP), in order to be assessed; quality analysis was done at the hospital reading center. Of the 291 study participants, 81.7% had fundus photographs of adequate quality for interpretation. Additionally, the image quality was similar to their previous studies.26, 27 The use of non-mydriatic fundus imaging facilitated screening thresholds for referrals of mild non-proliferative DR (NPDR) and moderate NPDR with a sensitivity of 97.1% and 53.3%, respectively, and specificity of 95.5% and 96.9%, respectively. Individuals with severe NPDR were accurately detected 100% of the time using a screening threshold of mild retinopathy. Consequently, telemedicine provided a reliable and highly acceptable tool for DR screening, as it can attract an important number of individuals with diabetes and recruit patients that could be otherwise missed by the current strategies of screening. A relevant study by Perrier et al.27 compared two, three, and four 45-degree non-mydriatic fundus imaging with the ETDRS9 standard stereoscopic 30-degree fields. In comparison with the ETDRS standard fields, they found that using two 45-degree non-mydriatic images sensitivity and specificity of screening for mild or severe DR (ETDRS grade 35 or greater) were 87.5% and 92.3%, respectively. On the other hand, using 3 and four non-mydriatic images provided corresponding values of 88.9% and 94.6%, and 88.9% and 91.9%, respectively.
Fig. 1.
Algorithm for the screening of diabetic retinopathy.
Liesenfeld et al.25 compared the results of DR evaluation of 129 cases by 2-field 50-degree non-stereo digital fundus images and by slit-lamp fundoscopy carried out by an ophthalmologist. The sensitivity of detecting eyes with DR at risk [at least moderate NPDR and/or presence of clinically significant macular edema (CSME)] using digital photography among the reading centres varied from 70% to 92% (median, 85%) and specificity varied from 73% to 95% (median, 90%) at a 95% confidence interval (CI). It was recommended that combining photography and measurement of visual acuity could improve screening and threshold referral.
Gomez-Ulla et al.28 assessed the efficiency of digital retinal images for the evaluation of DR. It was shown that there was an agreement between DR grading from digital images and clinical eye examination. Therefore it appears that the digital fundus images correctly assessed the presence or absence of DR.
Shi et al.29 carried out a systematic review and meta-analysis of 20 articles and found that the pooled sensitivity of telemedicine was higher than 80% in detecting the absence of DR and low-or high risk PDR; higher than 70% in recording mild or moderate NPDR diabetic macular edema (DME), and CSME; and 53% in severe NPDR detection. Finally, pooled specificity exceeded 90%, with the exception of mild NPDR, where specificity was 89%.
Access and cost-effectiveness
The efficiency of a tele-ophthalmology program is based on its ability to limit the burden on the health system by offering services to the target population by using limited health care resources. Population-based interventions require two important parameters; decent levels of diagnostic accuracy and cost-effective evidence-based care.4 It has been estimated that only 50%–90% of the population will need specialized eye care, whereas less than 10% will require further management for vision-threatening DR.30 The in-person clinical evaluation of diabetes-related retinal complications may often be inefficient, taking into account that more cost-efficient tools such as remote retinal photography are gradually becoming more available.
Nathoo et al.31 reported the results of the assessment of 394 diabetics (788 eyes) using tele-ophthalmology. Out of them only 27.2% had DR and over a 2-year interval telemedicine contributed in saving approximately 450 round trips, showing that tele-ophthalmology can be efficiently used for DR screening. Although these figures indicate the reduced travel time and cost for a rural-population it does not take into account the cost saved from time away from work or lost wages during eye consultations.
A relevant study for the rural population India studied the use of tele-ophthalmology as a tool for DR screening in order to assess its cost-effectiveness when compared with no screening.32 This study highlighted that the cost of quality-adjusted life-years (QALYs) for this application of telemedicine was cost-effective when compared to no screening at all. Despite the fact that DR monitoring via tele-ophthalmology programs was initially used for rural and distant populations with limited access to eye care, later studies indicated that it may also be useful in urban settings. Chin et al.10 utilized non-mydriatic fundus photography as a tool for DR screening among patients with poor compliance to their annual eye check-up in both rural (872 participants from remote medical clinics at Native American Indian reservations) and urban areas (517 patients from a primary care clinic at an urban academic medical center). All participants had a diagnosis for diabetes and confirmed that they have not had a dilated fundus examination within the last 12 months. Images acquired were sent electronically to a retinal specialist who carried out a remote review. It was shown that digital images were of sufficient quality for evaluation.
Tele-ophthalmology based on mobile imaging units can ameliorate DR screening and decrease the possibility of poor compliance or lost follow-up appointments.13 Digital images from both eyes of 3505 diabetics were acquired via 3 different mobile units around different provinces of Canada. After obtaining the fundus images, retinal specialists reviewed this material in order to organize further consultations and management of the disease. Interestingly, a mean of 85.6% individuals did not require a further referral, suggesting that ophthalmology assessments through telemedicine can save significant time and can contribute in prioritizing patients that need further interventions [Fig. 2].
Fig. 2.
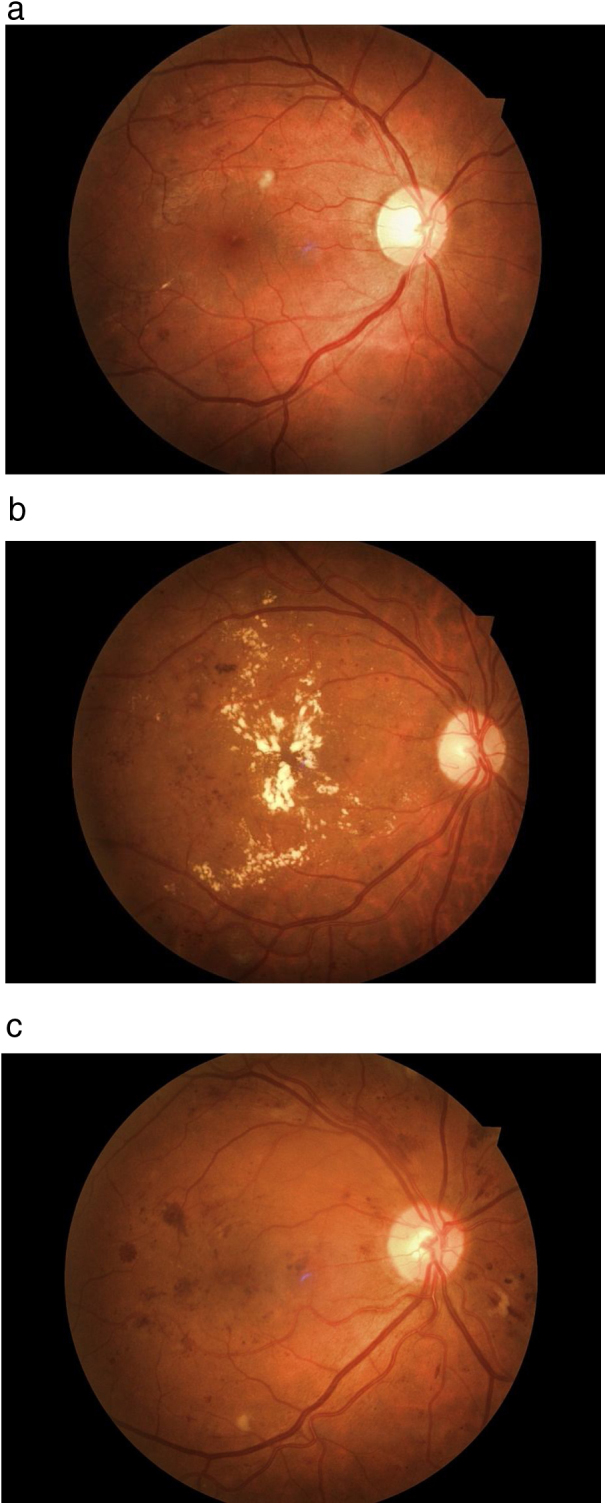
Fundus photography (right eye) of a patient with background diabetic retinopathy. This patient needs regular monitoring and good control of diabetes. (b) Fundus photography of the right eye of a diabetic patient with severe diabetic maculopathy with multiple hard exudates that should be referred for further assessment and management by a medical retina specialist. (c) Fundus photography (right eye) of a patient with diabetic macular oedema, cotton wool spots and retinal hemorrhages. This is a case of a moderate to severe non-proliferative diabetic retinopathy that calls for treatment with panretinal laser photocoagulation and intravitreal injections with anti-VEGF (Vascular Endothelial Growth Factor) agents.
According to another study that was carried out in the United States33 higher rates of diabetics are keen on undergoing a tele-ophthalmology screening, while the vast majority of them does not require further follow-ups until their next annual examination. In a primary care setting, the long-term effectiveness of telemedicine in DR screening examinations in comparison with traditional clinical examination, may contribute more frequent screening examinations and can be considered as a useful tool for the monitoring of these patients. In a similar manner with the above mentioned studies, most patients did not warrant a further referral to an eye care specialist.34
Patients’ perceptions on tele-ophthalmology
Telemedicine is a validated, cost-effective method to improve monitoring.35 However, the acceptability of telemedicine as a novel screening tool from patients consists one of the most important parameters of its efficiency. Patients appear to perceive tele-ophthalmology as a highly acceptable approach for their DR screening.9 After completing a relevant questionnaire the majority of patients (90.8%) expressed that they found it as a very acceptable method for monitoring if an ophthalmologist was not available. Furthermore, 82% (239 patients) declared their preference for this type of screening over the traditional approach, as they considered it faster, easier, more accessible and convenient. Eighteen per cent of participants indicated that they would prefer a personal interaction, whereas 3.2% stated that they do not trust the validity of digital retinal imaging. Interestingly, 95% underlined their preference to have their next DR examination via a telemedicine system and be referred to an eye specialist only if required. Additionally, most of the participants (91%) signified their intention of being more compliant in the future if they are monitored with this new screening approach. Subsequently, tele-ophthalmology strategy for DR screening may persuade more individuals to attend a regular retinal screening. Similarly, a study conducted in Kenya36 revealed that diabetics find a tele-ophthalmology approach more convenient and helpful compared to traditional clinical examination
Valikodath et al.35 explored the factors that may influence patients’ attitudes toward telemedicine. Their study showed that in overall patients were keen on participating in a telemedicine programme. Their attitudes were influenced by their perceptions and health, but not their demographics. Those individuals that were receptive focused on convenience, while those that were unreceptive underlined their patient-doctor relationship or having long-standing diabetes mellitus. The results from this study indicated that tele-ophthalmology should be designed for people who are in need and receptive to similar programmes.
The keys to successful implementation
The high costs of setting the initial capital outlay consist one of the primary burdens of a successful DR screening program. The two main investments are related with the staff training and the digital fundus cameras.4 Gomez-Ulla et al. analyzed the costs of tele-ophthalmology program in order to compare them with the clinical assessment by an eye specialist.37 The study took into account several factors including the capital expenditure, human resource component, lost time and wages of patients during screening, patient travel expenses, and the cost of subsequent consultation for patients who required further management. From the perspective of a public health system, the cost for clinical fundoscopy is less due to the lower capital expenditure and maintenance costs. On the other hand, tele-ophthalmology offers lower travel costs and lost wages for the patients. Additionally, ungradable images because of poor field definitions, media opacities and small pupil size may cause further limitations to the implementation of telemedicine in DR monitoring.34 As can be expected due to the increased rates of cataracts in diabetic patients, telemedicine programs with digital non-mydriatic fundus cameras may have a higher percentage of ungradable images. The presence of images that cannot be properly graded lead to more referrals and in-person examinations with an ophthalmology and subsequently to increased expenses that diminish the cost-effectiveness of the program.
Overcoming the burden of ungradable retinal photographs and ensuring quality are both inextricably correlated with the successful implementation and sustainability of such a program. Standardized and verified protocols, sufficient training of photographers, and probably allowing some re-adjustments through a defined protocol for selective mydriasis, if required, are some of the most substantial parameters.13, 33 Some studies have underlined the importance of pupil dilation in improving the image quality in reducing the ungradability.38, 39 It must be taken into consideration though that mydriasis may influence the patients’ perspective regarding telemedicine’s high acceptability.4
Probably, the implementation of scanning laser ophthalmoscopy with ultrawide field (UWF) imaging technology can contribute in obtaining images of higher quality with a better field of view even in non-dilated patients.40 A relevant study compared the rate of ungradable retinal photographs between non-mydriatic multifield fundus photography (NMFP) and non-mydriatic UWF imaging. The study showed that the ungradable rate per patient was substantially lower in images acquired from UWF imaging compared to NMFP. Notably, non-mydriatic UWF imaging limited the amount of images that could not be graded by 81%. Moreover, UWF imaging increased the ability of detecting DR from 11.7% to 24.2% (P < 0.0001) and referable DR (moderate NPDR or DME or worse) from 6.2% to 13.6% (P < 0.0001). Finally, more severe cases of DR could be detected based on the existence of mainly peripheral lesions observed only with UWF images, suggesting that UWF can be very helpful in organizing large population-based tele-ophthalmology DR screening programs.40
In overall, the results of such a program are not immediate, and may be moderate in the early years of the implementation, before they gradually start to improve.41 Although early recognition and treatment of diabetic retinopathy is of proven value in reversing or preventing loss of vision, the infrastructure to detect cases that require treatment is not yet universally available.42 The familiarity of patients and primary care providers with tele-ophthalmology needs to be enhanced, so that issues regarding compliance will be curtailed.43 Consequently, in order to ensure good medical practice and provide quality health care services, tele-ophthalmology programs need to be well organized and ready to encounter their main challenges [Table 1].
Table 1.
Summary of major challenges in the implementation of tele-ophthalmology for diabetic retinopathy screening.
| Quality of care | Quality of care appears to be causing a significant degree of skepticism for ophthalmologists. This derives from the fact that tele-ophthalmology interferes with the classic attitude of a physician’s clinical examination and personal interaction with his or her patients. |
| Liability | Possible standard malpractice considerations have to be taken into account, especially in cases where there may be relevant gaps in the laws of each country |
| Image quality | Teleophthalmology programs must take into account that the ungradable rate is a critical issue. In cases of an ungradable image, that encounter becomes unusable. The patient will not benefit, and it drains resources from the program. Reduction of ungradable images will increase the financial sustainability and clinical effectiveness of the program. |
| Workflow | Validated protocols are required in order to clearly delineate workflow and roles/responsibilities. Additionally, the time burden on physicians needs to assess all cases should also be estimated. |
| Security | Data encryption, password protection, and adherence to federal regulations, compliant backup and archiving must to be in accordance with all devices, from workstations to mobile devices. |
| Financing and reimbursement | Financial sustainability can be a substantial challenge, especially for programs that are not university-based or are not part of a federal program. |
| Patient perceptions | The patient’s attitude, satisfaction and compliance to a tele-ophthalmology program should be assessed at regular intervals. |
| Training of health care providers | All professionals involved in such screening programs must receive appropriate training regarding DICOM [Digital Imaging and Communications in Medicine] standards and compliance, regulations, as well as hardware and software that will be used. |
| Confusion of scope | Every tele-ophthalmology project should clearly define its scope, objectives and targets regarding the health care services provided. |
Conclusions and future perspectives
The national DR screening tele-ophthalmology program in the United Kingdom has been described as one of the most successful programs. It has underlined the importance of monitoring DR and its complications together with alterations of the overall glycemic status. Notably, DR is not any longer considered as a leading cause of blindness in England and Wales.44 The concept of this program was to identify the target population and provide a functional referral system for patients that required further management. Additionally, a continuous program of quality assurance and control was carried out.
A multidisciplinary collaborative approach for DR screening must be undertaken by more countries in order to improve retinopathy evaluation rates. A primary care physician or an endocrinologist can be the first point of contact for the majority of the diabetics, as this strategy can increase the probability of having a retinal screening.6 Therefore, if primary care or multispecialty clinics are equipped with fundus cameras, especially in areas without access to eye care specialists. Interestingly, several studies have shown that properly trained primary care physicians can reliably evaluate fundus images.45, 46 Decent training and education on diabetes and its ocular complications can further improve our understanding and improve the screening among diabetics.11 Future studies and randomized control trials are require in order to improve our strategies and approach leading to improved tele-ophthalmology services that will cover efficiently a wider population.
Disclosure of potential conflicts of interest
All authors declare that there is no conflict of interest.
Funding sources
All authors declare that they received no funding for this study.
Copyright statement
The Corresponding Author, has the right to assign on behalf of all authors and does assign on behalf of all authors, a full assignment of all intellectual property rights for all content within the submitted study in any media known now or created in the future, and permits this study (if accepted) to be published and to be fully exploited within the remit of the assignment as set out in the assignment which has been read.
Acknowledgement
We have no acknowledgements to be mentioned.
References
- 1.American Telemedicine Association . 2016. Telemedicine nomenclature.http://www.americantelemed.org/resources/nomenclature#.V1MQ8_krJhE Accessed May 1, 2016. [Google Scholar]
- 2.International Diabetes Federation . 7th ed. 2015. IDF diabetes atlas.http://www.idf.org/diabetesatlas Accessed October 2, 2017. [Google Scholar]
- 3.Pasquel F.J., Hendrick A.M., Ryan M., Cason E., Ali M.K., Narayan K.V. Cost-effectiveness of different diabetic retinopathy screening modalities. J Diabetes Sci Technol. 2016;10(March (2)):301–307. doi: 10.1177/1932296815624109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salongcay R.P., Silva P.S. The role of teleophthalmology in the management of diabetic retinopathy. Asia-Pacific J Ophthalmol (Philadelphia, Pa) 2018;7(1):17–21. doi: 10.22608/APO.2017479. [DOI] [PubMed] [Google Scholar]
- 5.Mohamed Q., Gillies M.C., Wong T.Y. Management of diabetic retinopathy: a systematic review. JAMA. 2007;298:902–916. doi: 10.1001/jama.298.8.902. [DOI] [PubMed] [Google Scholar]
- 6.Tayapad J.B., Bengzon A.U., Valero S.O. Implementation and pilot data on diabetic retinopathy in a teleophthalmology program at a multispecialty primary care clinic. Philipp J Ophthalmol. 2014;39:90–93. [Google Scholar]
- 7.Mukamel D.B., Bresnick G.H., Wang Q. Barriers to compliance with screening guidelines for diabetic retinopathy. Ophthalmic Epidemiol. 1999;6:61–72. doi: 10.1076/opep.6.1.61.1563. [DOI] [PubMed] [Google Scholar]
- 8.Gower E.W., Silverman E., Cassard S.D. Barriers to attending an eye examination after vision screening referral within a vulnerable population. J Health Care Poor Underserved. 2013;24:1042–1052. doi: 10.1353/hpu.2013.0134. [DOI] [PubMed] [Google Scholar]
- 9.Boucher M.C., Nguyen Q.T., Angioi K. Mass community screening for diabetic retinopathy using a nonmydriatic camera with telemedicine. Can J Ophthalmol. 2005;40:734–742. doi: 10.1016/S0008-4182(05)80091-2. [DOI] [PubMed] [Google Scholar]
- 10.Chin E.K., Ventura B.V., See K.Y. Nonmydriatic fundus photography for teleophthalmology diabetic retinopathy screening in rural and urban clinics. Telemed J E Health. 2014;20:102–108. doi: 10.1089/tmj.2013.0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brechner R.J., Cowie C.C., Howie L.J. Ophthalmic examination among adults with diagnosed diabetes mellitus. JAMA. 1993;270:1714–1718. [PubMed] [Google Scholar]
- 12.Liu Y., Swearingen R. Diabetic eye screening: knowledge and perspectives from providers and patients. Curr Diab Rep. 2017;17:94. doi: 10.1007/s11892-017-0911-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boucher M.C., Desroches G., Garcia-Salinas R. Teleophthalmology screening for diabetic retinopathy through mobile imaging units within Canada. Can J Ophthalmol. 2008;43:658–668. doi: 10.3129/i08-120. [DOI] [PubMed] [Google Scholar]
- 14.Adriono G., Wang D., Octavianus C. Use of eye care services among diabetic patients in urban Indonesia. Arch Ophthalmol. 2011;129:930–935. doi: 10.1001/archophthalmol.2011.147. [DOI] [PubMed] [Google Scholar]
- 15.Vujosevic S., Midena E. Diabetic retinopathy in Italy: epidemiology data and telemedicine screening programs. J Diabetes Res. 2016;2016 doi: 10.1155/2016/3627465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crossland L., Askew D., Ware R. Diabetic retinopathy screening and monitoring of early stage disease in Australian general practice: tackling preventable blindness within a chronic care model. J Diabetes Res. 2016;2016 doi: 10.1155/2016/8405395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eszes D.J., Szabó D.J., Russell G. Diabetic retinopathy screening using telemedicine tools: pilot study in Hungary. J Diabetes Res. 2016;2016 doi: 10.1155/2016/4529824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raman R., Bhojwani D.N., Sharma T. How accurate is the diagnosis of diabetic retinopathy on telescreening? The Indian scenario. Rural Remote Health. 2014;14(4):2809. [PubMed] [Google Scholar]
- 19.Sim D.A., Mitry D., Alexander P. The evolution of teleophthalmology programs in the United Kingdom: beyond diabetic retinopathy screening. J Diabetes Sci Technol. 2016;10(February (2)):308–317. doi: 10.1177/1932296816629983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Owsley C., McGwin G., Lee D.J. Diabetes eye screening in urban settings serving minority populations: detection of diabetic retinopathy and other ocular findings using telemedicine. JAMA Ophthalmol. 2015;133(February (2)):174–181. doi: 10.1001/jamaophthalmol.2014.4652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park D.W., Mansberger S.L. Eye disease in patients with diabetes screened with telemedicine. Telemed J E Health. 2017;23(February (2)):113–118. doi: 10.1089/tmj.2016.0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Silva P.S., Cavallerano J.D., Pacheco E.P. Diabetic retinopathy in Southeast Asia: a call for ocular telehealth programs. JAFES. 2012;27:176–179. [Google Scholar]
- 23.Wilson C., Horton M., Cavallerano J. Addition of primary care-based retinal imaging technology to an existing eye care professional referral program increased the rate of surveillance and treatment of diabetic retinopathy. Diabetes Care. 2005;28:318–322. doi: 10.2337/diacare.28.2.318. [DOI] [PubMed] [Google Scholar]
- 24.Surendran T.S., Raman R. Teleophthalmology in diabetic retinopathy. J Diabetes Sci Technol. 2014;8:262–266. doi: 10.1177/1932296814522806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liesenfeld B., Kohner E., Piehlmeier W. A telemedical approach to the screening of diabetic retinopathy: digital fundus photography. Diabetes Care. 2000;23:345–348. doi: 10.2337/diacare.23.3.345. [DOI] [PubMed] [Google Scholar]
- 26.Boucher M.C., Gresset J.A., Angioi K. Effectiveness and safety of screening for diabetic retinopathy with two nonmydriatic digital images compared with the seven standard stereoscopic photographic fields. Can J Ophthalmol. 2003;38:557–568. doi: 10.1016/s0008-4182(03)80109-6. [DOI] [PubMed] [Google Scholar]
- 27.Perrier M., Boucher M.C., Angioi K. Comparison of two, three and four 45 degrees image fields obtained with the Topcon CRW6 nonmydriatic camera for screening for diabetic retinopathy. Can J Ophthalmol. 2003;38:569–574. doi: 10.1016/s0008-4182(03)80110-2. [DOI] [PubMed] [Google Scholar]
- 28.Gomez-Ulla F., Fernandez M.I., Gonzalez F. Digital retinal images and teleophthalmology for detecting and grading diabetic retinopathy. Diabetes Care. 2002;25:1384–1389. doi: 10.2337/diacare.25.8.1384. [DOI] [PubMed] [Google Scholar]
- 29.Shi L., Wu H., Dong J. Telemedicine for detecting diabetic retinopathy: a systematic review and meta-analysis. Br J Ophthalmol. 2015;99:823–831. doi: 10.1136/bjophthalmol-2014-305631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fong D.S., Aiello L.P., Ferris F.L., III Diabetic retinopathy. Diabetes Care. 2004;27:2540–2553. doi: 10.2337/diacare.27.10.2540. [DOI] [PubMed] [Google Scholar]
- 31.Nathoo N., Ng M., Rudnisky C.J. The prevalence of diabetic retinopathy as identified by teleophthalmology in rural Alberta. Can J Ophthalmol. 2010;45:28–32. doi: 10.3129/i09-220. [DOI] [PubMed] [Google Scholar]
- 32.Rachapelle S., Legood R., Alavi Y. The cost-utility of telemedicine to screen for diabetic retinopathy in India. Ophthalmology. 2013;120:566–573. doi: 10.1016/j.ophtha.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 33.Mansberger S.L., Gleitsmann K., Gardiner S. Comparing the effectiveness of telemedicine and traditional surveillance in providing diabetic retinopathy screening examinations: a randomized controlled trial. Telemed J E Health. 2013;19:942–948. doi: 10.1089/tmj.2012.0313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mansberger S.L., Sheppler C., Barker G. Long-term comparative effectiveness of telemedicine in providing diabetic retinopathy screening examinations: a randomized clinical trial. JAMA Ophthalmol. 2015;133:518–525. doi: 10.1001/jamaophthalmol.2015.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Valikodath N.G., Leveque T.K., Wang S.Y. Patient attitudes toward telemedicine for diabetic retinopathy. Telemed J E Health. 2017;23(March (3)):205–212. doi: 10.1089/tmj.2016.0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kurji K., Kiage D., Rudnisky C.J. Improving diabetic retinopathy screening in Africa: Patient satisfaction with teleophthalmology versus ophthalmologist-based screening. Middle East Afr J Ophthalmol. 2013;20:56–60. doi: 10.4103/0974-9233.106388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gomez-Ulla F., Alonso F., Aibar B. A comparative cost analysis of digital fundus imaging and direct fundus examination for assessment of diabetic retinopathy. Telemed J E Health. 2008;14:912–918. doi: 10.1089/tmj.2008.0013. [DOI] [PubMed] [Google Scholar]
- 38.Banaee T., Ansari-Astaneh M.R., Pourreza H. Utility of 1% tropicamide in improving the quality of images for tele-screening of diabetic retinopathy in patients with dark irides. Ophthalmic Epidemiol. 2017;24:217–221. doi: 10.1080/09286586.2016.1274039. [DOI] [PubMed] [Google Scholar]
- 39.Murgatroyd H., Ellingford A., Cox A. Effect of mydriasis and different field strategies on digital image screening of diabetic eye disease. Br J Ophthalmol. 2004;88:920–924. doi: 10.1136/bjo.2003.026385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Silva P.S., Horton M.B., Clary D. Identification of diabetic retinopathy and ungradable image rate with ultrawide field imaging in a national teleophthalmology program. Ophthalmology. 2016;123(June (6)):1360–1367. doi: 10.1016/j.ophtha.2016.01.043. [DOI] [PubMed] [Google Scholar]
- 41.Pareja-Ríos A., Bonaque-González S., Serrano-García M. Tele-ophthalmology for diabetic retinopathy screening: 8 years of experience. Arch Soc Esp Oftalmol. 2017;92(February (2)):63–70. doi: 10.1016/j.oftal.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 42.Gonzalez F., Castro A.F. Publication output in telemedicine in Spain. J Telemed Telecare. 2005;11(1):23–28. doi: 10.1177/1357633X0501100106. [DOI] [PubMed] [Google Scholar]
- 43.Liu Y., Zupan N.J., Swearingen R. Identification of barriers, facilitators and system-based implementation strategies to increase teleophthalmology use for diabetic eye screening in a rural US primary care clinic: a qualitative study. BMJ Open. 2019;9(2) doi: 10.1136/bmjopen-2018-022594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scanlon P.H. The English National Screening Programme for diabetic retinopathy 2003-2016. Acta Diabetol. 2017;54(June (6)):515–525. doi: 10.1007/s00592-017-0974-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rodriguez Villa S., Alonso Alvarez C., de Dios Del Valle R. Five-year experience of tele-ophthalmology for diabetic retinopathy screening in a rural population. Arch Soc Esp Oftalmol. 2016;91:426–430. doi: 10.1016/j.oftal.2016.01.023. [DOI] [PubMed] [Google Scholar]
- 46.Andonegui J., Serrano L., Eguzkiza A. Diabetic retinopathy screening using tele-ophthalmology in a primary care setting. J Telemed Telecare. 2010;16:429–432. doi: 10.1258/jtt.2010.091204. [DOI] [PubMed] [Google Scholar]