Abstract
Objectives: To evaluate the prevalence of total hip arthroplasty (THA) and total knee arthroplasty (TKA) in a population of former National Football League (NFL) players. Methods: Participants were 3913 former NFL players (participation in years 1960–2019) who completed either an online or mailed survey that included self-reported TKA and THA, year(s) of surgery and date of birth. The prevalence of TKA and THA was reported by age category and compared to published cohorts of athlete populations and general population of non-athletes in the USA. Results: 12.3% and 8.1% of sample reported TKA and THA, respectively. The prevalence of both TKA and THA was higher in former NFL players compared to US non-athletes across all ages. Prevalence of TKA was not statistically higher than in other former athlete cohorts but performed at younger ages. The prevalence of TKA and THA was higher than in other cohorts of former NFL players. Conclusion: Former NFL players had higher prevalence of arthroplasty than the general population, suggesting prior participation in American-style football may contribute to elevated risk for arthroplasty at younger ages. Understanding risk factors in style of play, lifestyle and other contributors is important to improve joint health of this population.
Keywords: American football, Osteoarthritis, Knee surgery, Hip, Sports medicine
INTRODUCTION
There has been a rise in the prevalence of total hip arthroplasty (THA) and total knee arthroplasty (TKA) in the USA over the past 30 years, particularly in younger populations.1 Studies have examined the prevalence of THA and TKA in former professional athletes including soccer players,2 rugby players3 and other athletes in impact sports.4 To date, two studies have reported on THA and TKA in former National Football League (NFL) players.5 6 In one study of players who participated in Super Bowl III in 1969 (age 62±3y, n=36), two-thirds reported arthritis, seven had TKA and one had THA.6 Another study examining data from former players in years 1929–2001 (n=2432) reported age, joint injuries, weight and playing position as risk factors associated with increased risk of TKA and THA, with reported prevalence of 7.7% and 4.6%, respectively.5 While both studies provide a historical understanding of the risk of TKA and THA in this population, neither provides recent prevalence in former players, nor compares prevalence rates across age to the general population and other professional athletes. Further studies suggest that high body mass index (BMI),7 8 weight gain9 and intensive physical activity at work7 are risk factors for TKA and THA. Given that former NFL players have some of the highest BMIs among athletes, experience weight gain throughout their careers10 and regularly engage in intensive physical activity, we hypothesised this population may be at increased risk for total joint arthroplasties, higher than previously reported. To test this hypothesis, we evaluated the prevalence of arthroplasty in former NFL players by age and compared the rate of arthroplasty in former NFL players to that in the general US population and other athlete cohorts.
METHODS
The Football Players Health Study (FPHS) at Harvard University is an ongoing study evaluating health outcomes in former American-style football (ASF) players. The methods of recruitment for this cohort and verification of eligibility to participate have been noted previously.10 Living former ASF players were identified using the NFL Player Association and online public source Pro Football Reference who participated during years 1960 to present. Former players with verified contact information were each sent a 76-question survey including items regarding their health status. This included report of prior TKA and THA queried as follows: ‘Since leaving active professional football have you had any of the following surgical procedures: (knee joint replacement) or (hip joint replacement)?’ Participants who answered ‘Yes’ also reported approximate year(s) of surgery. Responses were collected and tabulated using REDCap (Vanderbilt, Nashville, Tenn)11 12 for online surveys or Scantron (Scantron Corporation, Tustin, CA, USA) for paper surveys. For participants with history of multiple joint arthroplasties (including the same joint or bilateral joint replacement), the date of initial surgery was used as the index measure to determine the age at the time of arthroplasty. Participants reporting history of both knee and hip arthroplasty were also reported using the date for first surgery as index case for each arthroplasty and were reported in prevalence of hip and knee arthroplasty in the total cohort. Statistical analyses were conducted with R (R Core Team, 2018).
χ 2 tests were used to identify differences in arthroplasty prevalence between the FPHS cohort and the general population and other athlete populations, using published values in other cohorts. Date of birth and year of arthroplasty were used to determine approximate age at the time of arthroplasty. The study was approved by the institutional review board (IRB) at Harvard T.H. Chan School of Public Health (Protocol:18-1365) and Beth Israel Deaconess Medical Center (2014P000308). Waiver of documentation of consent was obtained from the reviewing IRBs. All participants received a copy of the consent and participation was optional.
RESULTS
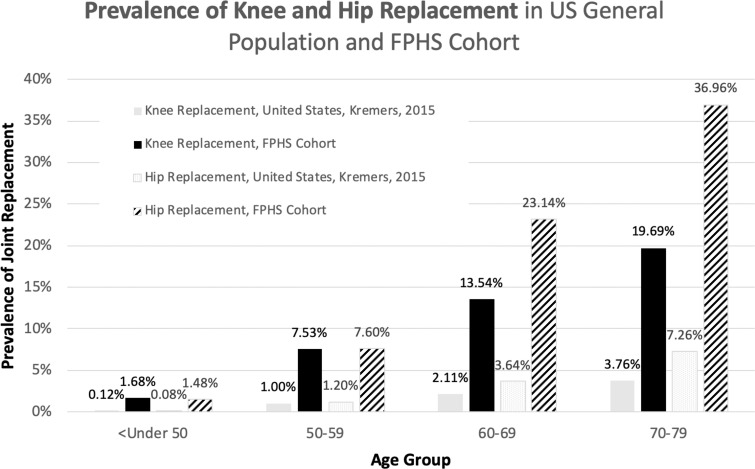
Of 15 643 eligible former players, 3913 agreed to participate (average age 52.4 years). TKA and THA were reported in 12.3% and 8.1% of participants, respectively (tables 1 and 2). The prevalence of arthroplasty increased across age and was higher for TKA compared to THA (figure 1). The prevalence of TKA was higher than THA for all age groups above 60 years.
Table 1.
Prevalence of knee and hip joint replacement by age at the time of the survey in FPHS cohort
| Knee joint replacement (89 responses missing) |
Hip joint replacement (114 responses missing) |
|||
|---|---|---|---|---|
| Age category (years) | Yes | No | Yes | No |
| <50 | 24 (1.48%) | 1596 (98.52%) | 27 (1.68%) | 1584 (98.32%) |
| 50–59 | 69 (7.60%) | 839 (92.40%) | 68 (7.53%) | 835 (92.47%) |
| 60–69 | 180 (23.14%) | 598 (76.96%) | 104 (13.54%) | 664 (83.85%) |
| 70–79 | 170 (36.96%) | 290 (63.04%) | 90 (20.85%) | 367 (79.15%) |
| 80+ | 28 (46.67%) | 32 (53.33%) | 18 (29.51%) | 43 (70.49%) |
| Total | 471 (12.31%) | 3355 (87.71%) | 307 (8.08%) | 3492 (91.92%) |
FPHS, Football Players Health Study.
Table 2.
Prevalence of knee and hip joint replacement by reported age at the time of surgery in FPHS cohort
| Age category (years) | TKA | THA |
|---|---|---|
| <40 | 24 (5.10%) | 19 (6.19%) |
| 40–49 | 55 (11.68%) | 42 (13.68%) |
| 50–59 | 135 (28.66%) | 90 (29.32%) |
| 60–69 | 147 (31.21%) | 90 (29.32%) |
| 70–79 | 56 (11.89%) | 27 (8.79%) |
| 80+ | 1 (0.21%) | 3 (0.98%) |
| Total | 418 (53, or 11.25%, missing year of TKA) |
271 (36, or 11.73%, missing year of THA) |
% Reflects the percentage of joint replacement that occurred in that age category.
FPHS, Football Players Health Study; THA, total hip arthroplasty; TKA, total knee arthroplasty.
Figure 1.
Prevalence of total knee arthroplasty and total hip arthroplasty was reported by age category of former NFL Players with the Football Players Health Study (FPHS) cohort and general US population. Knee arthroplasty was more common that hip arthroplasty for both populations. Arthroplasty was more common for FPHS cohort than general US population across all ages. NFL, National Football League.
When compared to the prevalence of arthroplasty in the general population,1 the prevalence in the FPHS cohort was significantly higher in each age category (table 3). The prevalence of THA reported in FPHS cohort age 50–59 years exceeded the prevalence for nearly every age category in the general population, including the 90+ category.1
Table 3.
Prevalence of knee and hip joint replacement in age-comparable males in the general population and in the FPHS cohort
| Kremers, 2015 (general population) | FPHS cohort N=3,913 | |||||
|---|---|---|---|---|---|---|
| n | % | n | % | P value | ||
| Knee replacement | ||||||
| <50 | ||||||
| Yes | 85 195 | 0.08 | 24 | 1.48 | <0.005 | |
| Total | 105 709 894 | 1620 | ||||
| 50–59 | ||||||
| Yes | 245 935 | 1.20 | 69 | 7.60 | <0.005 | |
| Total | 20 512 532 | 908 | ||||
| 60–69 | ||||||
| Yes | 510 244 | 3.64 | 180 | 23.14 | <0.005 | |
| Total | 14 029 131 | 778 | ||||
| 70–79 | ||||||
| Yes | 541 038 | 7.26 | 170 | 36.96 | <0.005 | |
| Total | 7 447 964 | 460 | ||||
| Kremers, 2015 (general population) | FPHS cohort N=3,913 | |||||
| n | % | n | % | P value | ||
| Hip replacement | ||||||
| <50 | ||||||
| Yes | 122 401 | 0.08 | 27 | 1.68 | <0.005 | |
| Total | 105 709 894 | 1611 | ||||
| 50–59 | ||||||
| Yes | 205 995 | 1.00 | 68 | 7.52 | <0.005 | |
| Total | 20 512 532 | 904 | ||||
| 60–69 | ||||||
| Yes | 295 869 | 2.11 | 104 | 13.54 | <0.005 | |
| Total | 14 029 131 | 768 | ||||
| 70–79 | ||||||
| Yes | 280 383 | 3.76 | 90 | 19.69 | <0.005 | |
| Total | 7 447 964 | 457 | ||||
FPHS, Football Players Health Study.
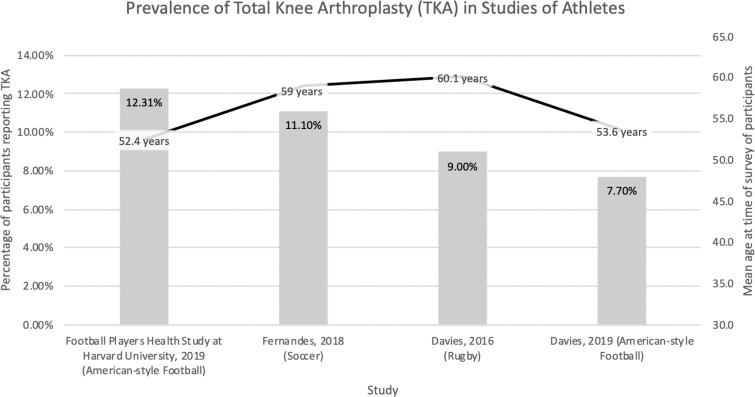
Former players in the FPHS cohort were, on average, younger than other professional athlete populations in which joint arthroplasty has been studied, including another cohort of former NFL players (all p<0.05, figure 2). Despite being younger, the overall prevalence of TKA for former NFL players (12.3%) was non-statistically higher than 9% reported in rugby players3 and 11.1% reported in soccer players2 (p=0.1235 and 0.1794, respectively). The FPHS cohort also had a higher prevalence of both reported knee (12.3% vs 7.7%, p<0.001) and hip replacement as compared to the Davies cohort of former ASF players (8.1% vs 4.6%, p<0.001).5
Figure 2.
Total knee arthroplasty was performed at younger ages within the Football Players Health Study (FPHS) compared to studies in other athlete populations and a separate report in former NFL players. Overall prevalence data were non-statistically different between groups. NFL, National Football League.
DISCUSSION
Our results demonstrate that former NFL players have an overall prevalence of 12.3% and 8.1% for TKA and THA, respectively. This study adds to the limited reports of arthroplasty in former NFL players and is the largest cohort report to date. Furthermore, this study expands upon findings of Davies et al 5 with rates of TKA and THA higher in the current study population than previously observed in former NFL players participating in a more distant era from 1929 to 2001.5
Differences in TKA between sports
The prevalence of TKA was similar to other non-ASF athlete populations but performed at a younger age. Compared to the general population, former NFL players had higher rates of TKA and THA across all ages. The mechanism for higher rate of arthroplasty in former NFL players is unknown; we hypothesise that the combination of traumatic joint injuries, higher playing weight and other factors may contribute. Previous studies suggest that the combined effects of physical activity at work,7 BMI,7 8 joint injuries associated with osteoarthritis5 and weight gain are risk factors for arthroplasty.9
Future directions
The current report expands on earlier findings from an ongoing study evaluating the largest cohort of former NFL players, the FPHS at Harvard University. An earlier report identified early-life weight gain during the time of high school to college was independently associated with the development of cardiometabolic disease, sleep apnoea and chronic pain.10 When separated by field position, linemen gained greater weight than non-linemen and were also more likely to be classified as having chronic pain.10 The current findings from this report on high rate of arthroplasty, along with prevalence of potential risk factors from other populations, illustrate the need for translational strategies to address the high and premature rate of arthritis and joint disease. Treatment should address modifiable risk factors in this cohort and include lifestyle factors of diet and exercise to lower BMI. However, the interconnectivity of other disease states suggests a model of care addressing obstructive sleep apnoea,13 metabolic syndrome,14 along with mood and neurocognitive issues, which may influence pain experience and thresholds. Addressing inflammation burden may be important given the known association to disease states including metabolic syndrome,14 obstructive sleep apnoea15 and neuroinflammation that has been postulated to contribute to widespread pain.16 In addition, new treatments that address the underlying inflammatory joint catabolic pathways may be targets for early intervention with new injectable medications and orthobiological agents.17–19
Limitations
Limitations include the possibility of selection bias. It is not possible to know whether players who underwent arthroplasty were more or less likely to enrol in this study. The self-reported data in our study may overestimate the true prevalence of TKA and THA. However, there appears to be good agreement between self-reported data and hospital data in TKA and THA.9 Our cross-sectional design and comparison to former athlete populations precludes determination of explanatory mechanisms specific to sport, including forces sustained during sport, differences in pain threshold and documented weight gains through sports participation. The study design limits accounting precisely for determinants of health that influence the outcome of having an arthroplasty, both in the general US population and within our former NFL population studied. Despite these limitations, this study represents the largest study to date to report prevalence rates for TKA and THA in former NFL players.
Conclusion
Our study identified higher rates of THA and TKA within former NFL players than previously reported in a contemporary cohort. Although the rate of TKA was not statistically different compared to former rugby and soccer players, the younger age of our cohort suggests an earlier burden of advanced joint disease and symptomatic joint pain in former NFL players. The high rate of arthroplasty in this population requires further investigation to identify methods for injury prevention and to optimise treatment of arthritis.
What are the new findings.
The prevalence of total knee arthroplasty and total hip arthroplasty within the cohort of former National League Football (NFL) players was 12.3% and 8.1%, respectively.
Findings suggest former NFL players have total knee arthroplasty at younger average age but at similar rates to other sport populations of soccer and rugby.
The elevated rate of total hip arthroplasty and total knee arthroplasty of former NFL players compared to the general US population across ages suggests a sport-specific style of play, athlete characteristics, health co-morbidities and other lifestyle factors need to be further explored.
The young age of this cohort suggests further translational research is needed to understand methods to optimise non-surgical management of knee and hip injuries.
Acknowledgments
The authors have no conflicts of interest to disclose. We would like to thank the study participants, advisors and staff of the Football Players Health Study. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the National Football League Players Association, Harvard Medical School, Harvard University or its affiliated academic healthcare centres, or the Massachusetts General Hospital.
Twitter: Adam Tenforde @AdamTenfordeMD.
Contributors: AST, BC, JB, AB, RZ were responsible for the conception and design of the work. All authors were responsible for analysis and interpretation of the data, were responsible for drafting and revising the manuscript and provided final approval of the version to be published, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work.
Funding: AST, BC, JB, JBS, MW, ALB and RZ received research funding from the Football Players Health Study at Harvard University, which was funded by a grant from the National Football League Players Association. Funding agencies had no role in study design, data collection or analysis. Funding agencies also had no role in the preparation of the manuscript.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
REFERENCES
- 1. Maradit Kremers H, Larson DR, Crowson CS, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am 2015. Sep 2;97: 1386–97. 10.2106/JBJS.N.0114110.2106/JBJS.N.01141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fernandes GS, Parekh SM, Moses J, et al. Prevalence of knee pain, radiographic osteoarthritis and arthroplasty in retired professional footballers compared with men in the general population: a cross-sectional study. Br J Sports Med 2018;52:678–83. 10.1136/bjsports-2017-097503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Davies MAM, Judge AD, Delmestri A, et al. Health amongst former rugby union players: a cross-sectional study of morbidity and health-related quality of life. Sci Rep 2017. Sep 28;7:11786 10.1038/s41598-017-12130-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tveit M, Rosengren BE, Nilsson JA, et al. Former male elite athletes have a higher prevalence of osteoarthritis and arthroplasty in the hip and knee than expected. Am J Sports Med 2012;40:527–33. 10.1177/0363546511429278 [DOI] [PubMed] [Google Scholar]
- 5. Davies MAM, Kerr ZY, DeFreese JD, et al. Prevalence of and risk factors for total hip and knee replacement in retired National Football League athletes. Am J Sports Med 2019;47:2863–70. 10.1177/0363546519870804 [DOI] [PubMed] [Google Scholar]
- 6. Nicholas SJ, Nicholas JA, Nicholas C, et al. The health status of retired American football players: Super Bowl III revisited. Am J Sports Med 2007;35:1674–9. 10.1177/0363546507302219 [DOI] [PubMed] [Google Scholar]
- 7. Apold H, Meyer HE, Nordsletten L, et al. Risk factors for knee replacement due to primary osteoarthritis, a population based, prospective cohort study of 315,495 individuals. BMC Musculoskelet Disord 2014;15:217 10.1186/1471-2474-15-217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Changulani M, Kalairajah Y, Peel T, et al. The relationship between obesity and the age at which hip and knee replacement is undertaken. J Bone Joint Surg Br 2008;90:360–3. 10.1302/0301-620X.90B3.19782 [DOI] [PubMed] [Google Scholar]
- 9. Apold H, Meyer HE, Nordsletten L, et al. Weight gain and the risk of knee replacement due to primary osteoarthritis: a population based, prospective cohort study of 225,908 individuals. Osteoarthritis Cartilage 2014;22:652–8. 10.1016/j.joca.2014.03.002 [DOI] [PubMed] [Google Scholar]
- 10. Churchill TW, Krishnan S, Weisskopf M, et al. Weight gain and health affliction among former national football league players. Am J Med 2018;131:1491–8. 10.1016/j.amjmed.2018.07.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 2019;95:103208 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kanbay A, Kokturk O, Pihtili A, et al. Obstructive sleep apnea is a risk factor for osteoarthritis. Tuberk Toraks 2018;66:304–11. 10.1183/13993003.congress-2016.PA340 [DOI] [PubMed] [Google Scholar]
- 14. Courties A, Sellam J, Berenbaum F. Metabolic syndrome-associated osteoarthritis. Curr Opin Rheumatol 2017;29:214–22. 10.1097/BOR.0000000000000373 [DOI] [PubMed] [Google Scholar]
- 15. Guven SF, Turkkani MH, Ciftci B, et al. The relationship between high-sensitivity C-reactive protein levels and the severity of obstructive sleep apnea. Sleep Breath 2012;16:217–21. 10.1007/s11325-011-0492-2 [DOI] [PubMed] [Google Scholar]
- 16. Ji RR, Nackley A, Huh Y, et al. Neuroinflammation and central sensitization in chronic and widespread pain. Anesthesiology 2018;129:343–66. 10.1097/ALN.0000000000002130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hochberg MC, Guermazi A, Guehring H, et al. Effect of intra-articular sprifermin vs placebo on femorotibial joint cartilage thickness in patients with osteoarthritis: the FORWARD randomized clinical trial. JAMA 2019; Oct 8. 322: 1360–70. 10.1001/jama.2019.14735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Huebner K, Frank RM, Getgood A. Ortho-biologics for osteoarthritis. Clin Sports Med 2019;38:123–41. 10.1016/j.csm.2018.09.002 [DOI] [PubMed] [Google Scholar]
- 19. Oo WM, Yu SP, Daniel MS, et al. Disease-modifying drugs in osteoarthritis: current understanding and future therapeutics. Expert Opin Emerg Drugs 2018;23:331–47. 10.1080/14728214.2018.1547706 [DOI] [PubMed] [Google Scholar]