Abstract
Background:
With the interruption of elective activity during the coronavirus disease 2019 (COVID-19) pandemic, a reorganisation of health care for patients with inflammatory bowel disease (IBD) was warranted. We aimed to investigate the effectiveness of a dedicated contact centre service (CCS) on the reorganization of a high-volume IBD centre and on the continuity of care during the COVID-19 outbreak.
Methods:
We compared the CCS services provided to 3680 IBD patients and clinical outcomes before (January–February 2020) and during (March–April 2020) the COVID-19 period. We further included, as comparator, data from March to April of the previous year (2019).
Results:
During the outbreak, the CCS received an increase of 10.2% of contacts, from 881, in January–February 2020, to 971 (p = 0.02). An increase of 6% in CCS activities was also reported in comparison with March–April 2019 (from 914 to 971 in March–April 2020, p = 0.71). Before COVID-19, in both periods most contacts (67% in January–February 2020 and 60% in March–April 2019) required information about clinical activity, while fewer (33% in January–February 2020 and 40% in March–April 2019) requested logistic information. During the pandemic, most contacts (65.1%) asked to speak with a physician, 23.7% asked for information, while 11.1% wanted to cancel/postpone their appointments. Among all the information, 66% concerned COVID-19. In March–April 2020, 259 outpatient visits were booked, but were all replaced by phone consultations. No difference was detected in the number of intravenous biological administrations (307 versus 296, p = 0.64), surgeries (10 versus 9, p = 0.82) and urgent hospitalisations (10 versus 12, p = 0.67) before and during the COVID-19.
Conclusion:
The CCS was an effective tool in the reorganization of the IBD centre. Scheduled visits were replaced by phone calls. The main clinical outcomes were maintained in the COVID-19 period. Virtual follow-up using the CCS could be implemented after the pandemic to optimise the resources of the IBD centre.
Keywords: contact centre, COVID-19, inflammatory bowel disease, telemedicine
Introduction
Since February 2020, when the acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak began in Italy, hospitals have had to adapt and restructure their units to deal with this urgent new critical situation.1,2 The majority of resources were shifted towards the coronavirus disease 2019 (COVID-19) pandemic, and most Italian hospitals began to intensively reduce elective visits and endoscopy to address the increased need for intensive care units. Therefore, all physicians needed to reset clinical priorities and change the standards of quality of care.1,3,4
Inflammatory bowel diseases (IBD) are chronic, relapsing conditions that require close management that involves a tight control to prevent flare-ups and disease complications in order to guarantee an adequate quality of life.5,6 Therefore, IBD patients require regular and active follow up to manage their condition.7
The interruption of elective activity established by the Italian government impacted negatively on the outcome of IBD treatment by determining negative emotions such as fear and anxiety among patients and clinicians. In this scenario, IBD patients were worried about their ongoing treatment due to the potential increased risk of infections, especially for those treated with immunosuppressive and biological therapies. In addition, patients were concerned about the lack of a close follow-up visit, prolonged waiting time for their next appointments and potential communication issues or delayed interactions with the IBD team. Thus, it was essential to develop and implement an alternative source of care that included remote monitoring, virtual visits, helplines and drug delivery to homes, to better support IBD patients and thereby guarantee continuity of care. This method of home patient telematic management has been called ‘telemedicine’. Several studies have shown the feasibility of implementing telemedicine in IBD practices through various technological platforms; this turns out to have many benefits, such as improved disease knowledge, high rate of adherence, a decrease in hospitalisations, urgent visits and steroid use.8–11
Since 2012, our IBD team at the University of Naples Federico II (Italy) has taken advantage of the use of a dedicated IBD contact centre service (CCS) that includes a helpline and mail service to facilitate communication between physicians and patients and address logistic issues. This system is well-accepted by patients, as witnessed by high satisfaction rates. Accordingly, in our daily clinical practice, the CCS has led to substantial changes in the management of IBD patients.12 The advantages of this phone/e-mail service were highlighted during this pandemic. Therefore, our aim was to assess the effect of a dedicated IBD CCS on the fast reorganisation of our daily practice and on the clinical outcome during the COVID-19 outbreak versus the pre-COVID-19 period. We further analysed the role of the CCS as a reliable tool for reassuring IBD patients.
Materials and methods
We conducted a retrospective observational study to evaluate changes in CCS activities provided to 3680 IBD patients followed up in a high-volume tertiary academic centre at the University Federico II of Naples by comparing activities during COVID-19 (March–April 2020) with the pre-COVID-19 period (January–February 2020). Moreover, we included as comparator CCS activities data from March and April 2019.
Established in 2012, this helpline service is active from Monday to Friday, from 9:00 to 17:00 and is managed by expert operators belonging to Medical Service society (Contact Centre Close to Care© TOPS, Rome, Italy). Patients may contact the CCS for either medical information (IBD-helpline) or non-medical information (IBD-call centre). The IBD-helpline, managed by physicians of our IBD team, handles all requests for medical consultations, such as side effects of drugs, withdrawal of medications, and/or missed doses of medications and flare-up, whereas non-IBD requests are managed and sorted immediately by the call centre operators, and include requests for information about logistics, laboratory tests, appointments, and payment methods. In addition, if a patient needs to communicate urgently with a doctor, the operators will advise the physicians of the IBD team who will then contact the patient.
To assess the impact of the IBD CCS on the continuity of care during the COVID-19 pandemic, we compared the activities that occurred in the 2 months before COVID-19 with those that occurred during the COVID-19 pandemic: March and April 2020. In detail, we compared the number of phone calls received, missed appointments, urgent visits, hospitalisations, rate of intravenous biologic administration and surgeries. Moreover, we investigated, through an anonymous questionnaire administered by phone operators, the rate of satisfaction based on a 10- point Likert scale where 1 indicated ‘not satisfied’ and 10 ‘highly satisfied’. Finally, we evaluated, through a multiple-choice questionnaire, the effectiveness of the CCS and medical staff in supporting IBD patients during the complex situation.
Statistical analysis
Data obtained were transferred to Microsoft Excel and exported to STATA Version 14 (StataCorp LLC, College Station, TX, USA). The descriptive analysis was estimated on continuous variables as well as percentages and proportions of the categorical variables. The differences between percentages of CCS activities and major clinical outcomes (calculated on 3680 IBD patients) before and after the COVID-19 era were determined using chi-square. Differences were considered significant when p < 0.05. The number of biologic administrations during the two periods were compared by daily means. Furthermore, the delta (%) of the CCS activities and clinical outcomes before and during COVID-19 were recorded.
Results
Our IBD electronic database included a total of 3680 IBD patients in active follow up until April 2020. During the COVID-19 outbreak, the contacts received by our CCS increased by 10.2%, from 881 in January–February 2020 to 971 in March–April 2020 (p = 0.02). Demographic data are detailed in Table 1.
Table 1.
Demographic data of IBD contacts to the CCS.
| Overall population | Pre-COVID 19 (January–February 2020) |
During COVID-19 (March–April 2020) |
|
|---|---|---|---|
| IBD patients contacted CCS number (n) | 1852 | 881 | 971 |
| Disease n (%): | |||
| CD | 1056 (57%) | 489 (55.5%) | 567 (58.4%) |
| UC | 741 (40%) | 354 (40.2%) | 387 (39.8%) |
| IBD-unclassified | 55 (3%) | 38 (4.3%) | 17 (1.8%) |
| Sex n (%): | |||
| M | 1037 (56%) | 494 (56.1%) | 543 (55.9%) |
| F | 815 (44%) | 387 (43.9%) | 428 (44.1%) |
| Age n (%): | |||
| 14–20 yr. | 315 (17%) | 154 (17.5%) | 161 (16.6%) |
| 21–30 yr. | 407 (22%) | 184 (20.9%) | 223 (23%) |
| 31–40 yr. | 241 (13%) | 115 (13%) | 126 (13%) |
| 41–50 yr. | 333 (18%) | 151 (17.2%) | 182 (18.7%) |
| 51–60 yr. | 315 (17%) | 159 (18.1%) | 156 (16.1%) |
| > 60 yr. | 241 (13%) | 118 (13.3%) | 123 (12.7%) |
CCS, contact centre service; CD, Crohn's disease; COVID-19, coronavirus disease 2019; IBD, inflammatory bowel disease; UC, ulcerative colitis; yr, years.
An increase of 6% in CCS activities was also reported in comparison with March and April 2019 (from 914 in March–April 2019 to 971 in March–April 2020, p = 0.71). In the pre-COVID-19 period, most contacts concerned an update of clinical activity of the disease (60% March–April 2019 versus 67% January–February 2020), while fewer patients requested logistic information (33% in January–February 2020 and 40% in March–April 2019). No patients called to postpone or cancel appointments, although the rate of missed appointments without previous notice was 2%.
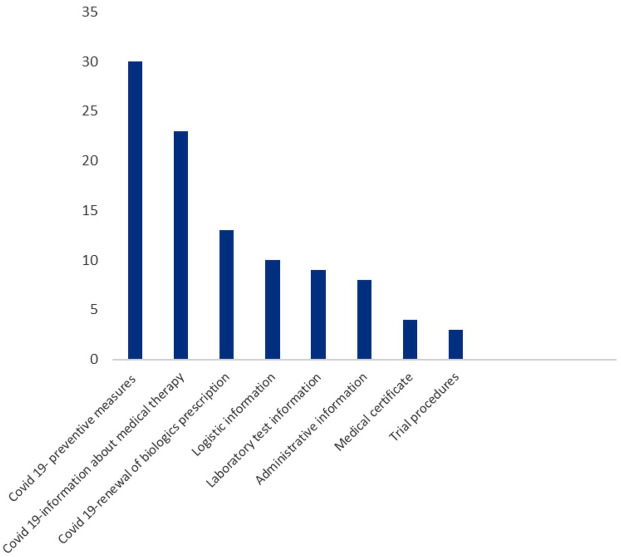
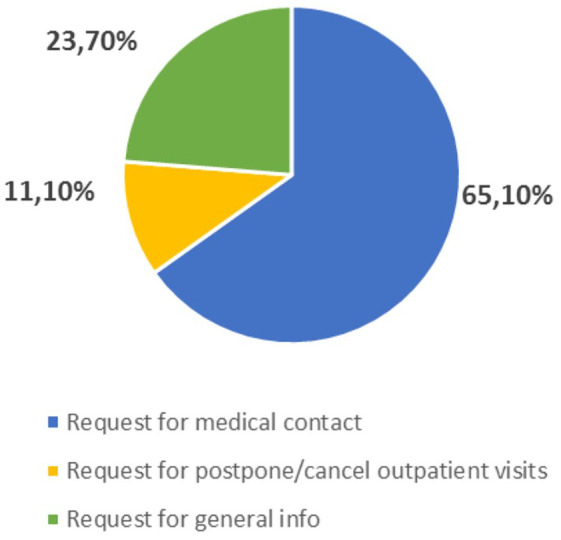
In the COVID-19 period, the majority (65.1%) of inbound calls were of patients that asked to speak with a physician of our IBD team. Out of the latter calls, 84.6% sought to update medical staff about their current clinical activity of disease, 9.7% wished to communicate the results of laboratory tests, and 5.7% concerned general medical information. In addition, 23.7% patients requested information, while 11.1% wanted to cancel or postpone their appointment dates because of fears of coming to hospital (Figure 1). A further analysis of the requested information showed that 66% calls were related to the COVID-19 pandemic. In detail, 30% concerned preventive measures to follow when visiting the hospital for biological therapy, 23% concerned information about ongoing medical treatments and 13% were related to the renewal of medical prescriptions. While, 10% of information concerned logistic issues, 9% clarification on laboratory tests to perform, 8% were administrative contacts and 3% were related to trial procedures (Figure 2).
Figure 1.
Type of request received at CCS during COVID-19 outbreak.
CCS, contact centre service; COVID-19, coronavirus disease 2019.
Figure 2.
Details of information received at CCS during COVID-19 outbreak.
CCS, contact centre service; COVID-19, coronavirus disease 2019.
In January and February 2020, the number of booked follow-up outpatient visits was 295; 25 of them (8%) were missed due to patient’s decisions. Of note, based on the 881 contacts at CCS, 80 visits (9%) were carried out for urgent needs. In March and April 2020, 259 follow-up visits were originally booked but did not take place due to Government regulations. All the visits were replaced by phone calls with physicians of our IBD team. Out of 971 contacts made during the COVID-19 period, 50 calls (5%) were converted to urgent visits that required face-to-face evaluations due to perianal Crohn's disease (CD), severe flare-up, and occurrence of sub-acute obstructions.
With regard to clinical outcomes, no significant difference was detected in the rate of intravenous biological administration before and during the COVID-19 period (p = 0.64.). In the pre-COVID-19 period, the number of intravenous biological administration was 307, with a mean of 7 ± 1.63 standard deviation (SD) per day. Similarly, during the pandemic, the number of infusions was 296 with the same mean of 7 ± 1.3 per day. Conversely, there was a significant decrease in terms of the rate of overall inpatient during COVID-19 due to cancellation of most elective admissions (p < 0.01). Specifically, before the COVID-19 pandemic, we recorded a total of 158 IBD-related hospital admissions. Among them, 36 were registered as new access to day patient service: day hospital (DH) that is, patients attend the hospitals generally for intravenous iron supplementation or blood transfusions without requiring overnight stay, 99 scheduled access to DH and 13 elective hospitalisations, whereas during the COVID-19 period we registered a total of 96 hospital admissions involving 12 new DH access and 72 scheduled access to DH. However, there was no difference in the number of urgent hospitalisations (10 pre-Covid-19 versus 12 during Covid-19, p = 0.67). Furthermore, the rate of surgery did not differ significantly between pre-COVID-19 and during COVID-19 periods (10 versus 9 surgeries; p = 0.82.) (Table 2). Finally, contact centre operators randomly selected a sample of 100 patients from the database to evaluate their rate of satisfaction and the feeling of reassurance by CCS during the COVID-19 period. A total of 95% of patients reported that they were highly satisfied with the CCS, while 5% were moderately satisfied. Concerning the feeling of relief, 78% of patients reported to be reassured only through the CCS, whereas 22% felt more confident by interacting also with physicians.
Table 2.
CCS activity and clinical outcomes of 3680 IBD patients before and during COVID-19 outbreak.
| Pre- COVID-19 (January–February 2020) |
During COVID-19 (March–April 2020) |
p | Delta (during versus pre COVID-19 period) |
|
|---|---|---|---|---|
| Inbound calls, (n) | 881 | 971 | p < 0.02 | +10.2% |
| Number of outpatient visits, (n) | ||||
| -Scheduled | 270 | − | NA | − |
| -Urgent | 80 | 50 | p < 0.01 | −37.5% |
| Number of missed appointments, (n) | 25 | − | NA | |
| Number of virtual visits, (n) | − | 259 | NA | |
| Biologics infusions, (n) | 307 | 296 | p = 0.64 | −3.6% |
| Biologics infusions (per day), mean ± SD | 7 ± 1.63 | 7 ± 1.3 | p = 0.9 | |
| Overall hospitalisation, (n) | 158 | 96 | p < 0.01 | −39.2% |
| - New DH access | 36 | 12 | p < 0.05 | −66.7% |
| - Scheduled DH | 99 | 72 | p = 0.03 | −27.3% |
| - Elective Hospitalisation | 13 | 0 | p < 0.01 | − |
| -Urgent hospitalisation | 10 | 12 | p = 0.67 | +20% |
| Surgeries, (n) | 10 | 9 | p = 0.82 | −10% |
CCS, contact centre service; COVID-19, coronavirus disease 2019; DH, day hospital; IBD, inflammatory bowel disease; NA, not applicable; SD, standard deviation; yr, years.
Discussion
The COVID-19 pandemic has revolutionized the existing health care system. It is crucial to maintain high quality of care for IBD patients. The role of physicians is not only to cure symptoms but also to care for and support their patients.13 Therefore, IBD teams must reassure patients and emphasise adherence to medication, provide preventive recommendations and assess infection risk. In the COVID-19 context, a shift towards virtual clinics is required. Alternative sources of care, including remote monitoring, virtual follow up, and helplines have been included in daily practise to facilitate communication, prevent loss of follow up visits and educate patients on preventive measures.14–16
To maintain high quality care for IBD patients during the COVID-19 outbreak, our helpline service, managed by the medical IBD team has proved to be a reliable tool for reorganising IBD activity in a short time by converting most physical follow-up visits to virtual follow ups. The centre also provides education resources by inviting patients to explore the websites of the national IBD society (IG-IBD) and the National Patients’ Association (AMICI) in order to promote patient empowerment and encourage treatment adherence.17,18
During the COVID-19 outbreak, we registered an increase (+10%) in the number of contacts, most of which request information on how to deal with ongoing therapy, infective risk, preventive measures and drug delivery (renewal of biologics prescriptions). In addition, other patients used different modes of healthcare delivery including mail and social platform such as AMICI.
To avoid any potential bias related to the selection of the pre-COVID-19 period we used as comparator for March–April 2020 the same months in 2019. Indeed, even though in the South of Italy the pandemic spread in early March 2020, the breaking news of pandemic could have determined fears and worries in most patients worldwide.
The replacement of outpatient visits with phone follow-ups helped to improve and optimise the IBD team workflow for patient care, and increase patient compliance since there were no missed virtual visits due to patient’s decision. Consequently, we would prevent the risk of loss of follow-up visits and overcrowded clinics post-COVID-19, and thereby save time to address more urgent and relevant medical issues. Given that our IBD centre has been flooded by requests for non-medical information from patients, the CCS also helps to provide most of the non-medical information requests, especially those related to logistic issues, such as changes of appointment dates due to fear of coming to the hospital or booking new appointments. On the contrary, no contacts were made to change/cancel or postpone appointments in the pre-COVID-19 period, even though we registered 2% of missed appointments without previous notice.
Notably, during phone calls, medical staff can discriminate between flare-up and symptoms exacerbated by negative emotions, identify IBD patients at risk and eventually establish in a short time if the patient requires an urgent visit. Importantly, urgent activity for IBD patients was not interrupted during the COVID-19 period even though the number of urgent outpatient visits decreased compared with the pre-COVID-19 period due to patient’s reluctance to come to the hospital. Patients receiving virtual follow ups were encouraged to call the CCS if they had symptoms. In addition, we were able to screen patients prior to infusion appointments, and to rule out symptoms considered secondary to or associated with COVID-19, so the infusion centre was maintained safe at all times. It is noteworthy that we also received few patients from the North of Italy because they returned home and thereby modified their infusion centre according to the nearest distance.
Of note, bowel ultrasonography service was interrupted in the COVID-19 period as it was considered postponable and all follow-up visits were delayed. In addition, laboratory centres were overwhelmed and therefore could not provide faecal calprotectin service. However we believe that non-invasive monitoring tools will play a crucial role for the application of treat to target approach in the post COVID-19 era.19
Most patients were concerned about the risk of infection, especially those treated with biologics and immunosuppressive therapies.20 Hence, the use of virtual follow up visits was an effective approach to face all these issue by meeting the patient’s needs and fears. The susceptibility of IBD patients to COVID-19 due to intestinal receptor angiotensin-converting enzyme 2 (ACE2) expression is a topic of intense debate. To date, there is no evidence of an increased frequency of COVID-19 cases in IBD patients, even though the results of further investigations are expected.21 However, accumulating data indicate that maintenance therapy should be continued because there was no increased risk of negative COVID-19 outcomes in IBD patients related to the use of tumour necrosis factor (TNF) antagonist or any other immunosuppressive drug.22,23 Conversely, the SECURE-IBD registry, which aims to prospectively collect data of patients with IBD infected with SAR-CoV-2, showed that corticosteroids were considered strong risk factors for adverse COVID-19 outcomes.24,25
Remarkably, despite reorganisation of our IBD centre, continuity of care was achieved, since the rate of surgery and biological infusions did not differ before and during the COVID-19 pandemic. Regarding the rate of inpatient admissions, we found a significant decrease in overall hospitalisations during the COVID-19 era because all elective hospitalisations due to polypectomy, endoscopic mucosal resection and balloon dilatation were postponed. Nevertheless, there was no difference in the rate of urgent IBD-related hospital admissions. In addition, all access for clinical trials were delayed because they were considered postponable according to legislative limitations. With regard to observational trials that did not require medical intervention, we arranged phone call visits to update follow-up case report forms.
It is noteworthy that the questionnaires confirm that, during the COVID-19 outbreak, the CCS contributed significantly to reassuring patients. Indeed, most patients (78%) felt reassured only using CCS, while 22% felt more confident after interacting with physicians. Moreover, 95% of respondents reported being satisfied with the care provided by the CCS. We believe that the long-term relationships of our IBD team with our patients played an additional role in boosting the confidence of IBD patients.
This study has several strengths: it is the first report on the role of a dedicated IBD CCS in a clinical setting in reorganising the daily activities of a high volume IBD unit in a short time due to COVID-19. The replacement of elective visits with phone calls (and e-mails) substantially reduced the number of physical follow-up visits, thus reducing the risk of overcrowded clinic and freeing up more time to address relevant issues and urgent visits. Importantly, the CCS may be useful even after COVID-19 in reorganizing the follow-up of IBD patients, by converting most physical visits to virtual follow-ups. In addition, given the lack of studies on strategies to reassure IBD patients during this pandemic, our experience provides insight into how to support patients and foster medical adherence.
This study has several limitations. COVID-19 did not have the same exponential impact in the South of Italy as it did in the North of Italy. Therefore, our health system in Southern Italy did not require a massive re-allocation of intensive care facilities and resources, including personnel, beds, and space. Accordingly, the achievement of the continuity of care was facilitated by the relatively low prevalence of COVID-19 in Campania compared with Lombardy (the most seriously affected region in Italy),26 so we were able to respond to the needs of IBD patients and meet this unprecedented challenge.
In the future, our experience could be the starting point for investing in new alternative sources of care in medicine and increasingly personalised patient care to ensure continuity of care. In conclusion, we hope our results will encourage IBD centres to evaluate the usefulness of a dedicated CCS in their clinical practice in the post-COVID-19 era.
Acknowledgments
The authors would like to thank the Contact Centre Close to Care©TOPS, Rome, Italy and Alessia Leonetti for her support in revisioning the manuscript.
Footnotes
Author contributions: OM Nardone - study conception and design, data acquisition, interpretation of results, writing & editing of the manuscript, tables and approval.
F Castiglione - study conception and design, interpretation of results, editing of the manuscript, critical review of the manuscript, revision, overall supervision and final approval.
A Rispo - study conception and design, interpretation of results, editing of the manuscript, critical review of the manuscript, revision, overall supervision and final approval.
GD De Palma - critical review of the manuscript, revision, overall supervision and final approval
A Testa; N Imperatore; L Pellegrini; AD Guarino; S Ricciolino; M Patturelli - data collection;
All authors approved the final version of the manuscript
Conflict of interest statement: The authors declare that there is no conflict of interest.
Ethics: Ethical approval was not required since there was no direct involvement of human subjects. Therefore, patient consent is not handled in this study.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Guarantor of the article: Fabiana Castiglione
ORCID iD: Olga Maria Nardone  https://orcid.org/0000-0002-9554-4785
https://orcid.org/0000-0002-9554-4785
Contributor Information
Olga Maria Nardone, Gastroenterology, Department of Clinical Medicine and Surgery, University of Naples Federico II, Via Pansini 5, Naples, 80131, Italy.
Antonio Rispo, Gastroenterology, Department of Clinical Medicine and Surgery, University Federico II of Naples, Naples, Italy.
Anna Testa, Gastroenterology, Department of Clinical Medicine and Surgery, University Federico II of Naples, Naples, Italy.
Nicola Imperatore, Gastroenterology, Department of Clinical Medicine and Surgery, University Federico II of Naples, Naples, Italy Gastroenterology and Endoscopy Unit, AORN Antonio Cardarelli, Naples, Italy.
Lucienne Pellegrini, Gastroenterology, Department of Clinical Medicine and Surgery, University Federico II of Naples, Naples, Italy.
Alessia Dalila Guarino, Gastroenterology, Department of Clinical Medicine and Surgery, University Federico II of Naples, Naples, Italy.
Simona Ricciolino, Gastroenterology, Department of Clinical Medicine and Surgery, University Federico II of Naples, Naples, Italy.
Marta Patturelli, Gastroenterology, Department of Clinical Medicine and Surgery, University Federico II of Naples, Naples, Italy.
Giovanni De Palma, Surgical Endoscopy, Department of Clinical Medicine and Surgery, University Federico II of Naples, Naples, Italy.
Fabiana Castiglione, Gastroenterology, Department of Clinical Medicine and Surgery, University Federico II of Naples, Naples, Italy.
References
- 1. Danese S, Cecconi M, Spinelli A. Management of IBD during the COVID-19 outbreak: resetting clinical priorities. Nat Rev Gastroenterol Hepatol 2020; 17: 253–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Center JHUCR. Coronavirus COVID-19 global cases, https://coronavirus.jhu.edu/map.html (2020, accessed 10 May 2020).
- 3. Fiorino G, Allocca M, Chaparro M, et al. ‘Quality of care’ standards in inflammatory bowel disease: a systematic review. J Crohns Colitis 2019; 13: 127–137. [DOI] [PubMed] [Google Scholar]
- 4. Allocca M, Fiorino G, Furfaro F, et al. Maintaining the quality standards of care for inflammatory bowel disease patients during the COVID-19 pandemic. Clin Gastroenterol Hepatol 2020; 18: 1882–1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ungaro R, Mehandru S, Allen PB, et al. Ulcerative colitis. Lancet 2017; 389: 1756–1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Torres J, Mehandru S, Colombel JF, et al. Crohn’s disease. Lancet 2017; 389: 1741–1755. [DOI] [PubMed] [Google Scholar]
- 7. Colombel JF, Narula N, Peyrin-Biroulet L. Management strategies to improve outcomes of patients with inflammatory bowel diseases. Gastroenterology 2017; 152: 351–361.e5. [DOI] [PubMed] [Google Scholar]
- 8. George L, Cross R. Telemedicine platform myIBDcoach reduces hospitalisations and outpatient gastroenterology visits in patients with IBD. BMJ Evid Based Med 2019; 24: 37–38. [DOI] [PubMed] [Google Scholar]
- 9. Li SX, Thompson KD, Peterson T, et al. Delivering high value inflammatory bowel disease care through telemedicine visits. Inflamm Bowel Dis 2017; 23: 1678–1681. [DOI] [PubMed] [Google Scholar]
- 10. Siegel CA. Placing value on telemedicine for inflammatory bowel disease. Am J Gastroenterol 2019; 114: 382–383. [DOI] [PubMed] [Google Scholar]
- 11. de Jong MJ, van der Meulen-de Jong AE, Romberg-Camps MJ, et al. Telemedicine for management of inflammatory bowel disease (myIBDcoach): a pragmatic, multicentre, randomised controlled trial. Lancet 2017; 390: 959–968. [DOI] [PubMed] [Google Scholar]
- 12. Castiglione F, Imperatore N, Testa A, et al. Efficacy of a “contact center-based communication” in optimizing the care of inflammatory bowel diseases. Dig Liver Dis 2016; 48: 869–873. [DOI] [PubMed] [Google Scholar]
- 13. Imperatore N, Rispo A, Lombardi G. The price of being a doctor during the COVID-19 outbreak. Gut 2020; 69: 1544–1545. [DOI] [PubMed] [Google Scholar]
- 14. D’Amico F, Peyrin-Biroulet L, Danese S. Inflammatory bowel diseases and COVID-19: the invisible enemy. Gastroenterology 2020; 158: 2302–2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. An P, Ji M, Ren H, et al. Prevention of COVID-19 in patients with inflammatory bowel disease in Wuhan, China. Lancet Gastroenterol Hepatol 2020; 5: 525–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Scaldaferri F, Pugliese D, Privitera G, et al. Impact of COVID-19 pandemic on the daily management of biotechnological therapy in inflammatory bowel disease patients: reorganisational response in a high-volume Italian inflammatory bowel disease centre. United European Gastroenterol J. Epub ahead of print 21 May 2020. DOI: 10.1177/2050640620929133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Italian Group for the study of Inflammatory Bowel Disease. Press e news, https://igibd.it/IT/press-e-news/ (accessed 10 May 2020).
- 18. AMICI Onlus. Covid-19 | Centri MICI in Italia, https://amiciitalia.eu/categorie/notizie-evidenza/covid-19-centri-mici-italia (accessed 5 May 2020).
- 19. Nardone OM, Rispo A, Castiglione F. Noninvasive monitoring of inflammatory bowel disease in the post COVID-19 era. Dig Liver Dis. Epub ahead of print 19 July 2020. DOI: 10.1016/j.dld.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. D’Amico F, Rahier J-F, Leone S, et al. Views of patients with inflammatory bowel disease on the COVID-19 pandemic: a global survey. Lancet Gastroenterol Hepatol 2020; 5: 631–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Neurath MF. Covid-19 and immunomodulation in IBD. Gut 2020; 69: 1335-1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bezzio C, Saibeni S, Variola A, et al. Outcomes of COVID-19 in 79 patients with IBD in Italy: an IG-IBD study. Gut 2020; 69: 1213–1217. [DOI] [PubMed] [Google Scholar]
- 23. Hanzel J, Ma C, Marshall JK, et al. Managing inflammatory bowel disease during COVID-19: summary of recommendations from gastrointestinal societies. Clin Gastroenterol Hepatol 2020; 18: 2143–2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brenner EJ, Ungaro RC, Gearry RB, et al. Corticosteroids, but not TNF antagonists, are associated with adverse COVID-19 outcomes in patients with inflammatory bowel diseases: results from an international registry. Gastroenterology 2020; 159: 481–491.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lukin DJ, Kumar A, Hajifathalian K, et al. Baseline disease activity and steroid therapy stratify risk of COVID-19 in patients with inflammatory bowel disease. Gastroenterology. Epub ahead of print 29 May 2020. DOI: 10.1053/j.gastro.2020.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet 2020; 395: 1225–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]