Abstract
Objective
The clinical efficacy of platelet-rich plasma (PRP) as adjuvant therapy in patients undergoing arthroscopic repair of meniscal injury remains controversial. This meta-analysis was performed to evaluate the clinical efficacy of PRP in the treatment of meniscal injury and provide evidence for the selection of clinical treatment options.
Methods
A computer-based search of the PubMed, Embase, and Cochrane Library databases was performed to retrieve articles using the search terms “platelet-rich plasma” and “menisci.” Quality evaluation and data extraction were performed. The combined effect was assessed using RevMan version 5.3 software.
Results
Three randomized controlled trials and three cohort studies involving 293 patients were included in the meta-analysis. There were no significant differences in the International Knee Documentation Committee score or Lysholm score between the experimental and control groups. The failure rate and visual analog scale score were significantly lower and the degree of active flexion was significantly higher in the experimental group than in the control group.
Conclusion
The findings of this meta-analysis suggest that PRP injection can effectively enhance the efficacy of arthroscopic repair of meniscal injury, reduce the failure rate and severity of pain, and improve active flexion.
Keywords: Platelet-rich plasma, adjuvant therapy, arthroscopic meniscal repair, meniscal injury, meta-analysis, failure rate, pain, active flexion
Introduction
The menisci are major components of the knee joint. Their mechanical functions include load conduction, stress dispersion, vibration cushioning, and joint stabilization. Meniscal injuries are common in the field of clinical orthopedics. However, the articular cartilage has weak capability of regeneration and repair1,2; therefore, if meniscal injuries are not repaired in a timely manner, articular cartilage degeneration can accelerate and lead to knee osteoarthritis.3–5 With the current emphasis on meniscal function and the clinical application of arthroscopy, arthroscopic meniscal repair or suture repair has become the standard treatment for meniscal injury. However, clinical challenges associated with such treatment include maximal retention of the meniscus, improvement of the regeneration and self-repairing abilities of the meniscus, and increasing the success rate of meniscal suture repair under arthroscopy.
In recent years, intra-articular injection of platelet-rich plasma (PRP) for the treatment of knee osteoarthritis has been increasingly used in the clinical setting. PRP is a platelet concentrate prepared from autologous whole blood. Studies have confirmed that PRP contains abundant growth factors and has a significant effect on promoting tissue healing, repair, and regeneration.6–8
A recent systematic review on PRP in meniscal repair did not perform a qualitative synthesis because of the heterogeneity of previous studies.9 Therefore, we performed a comprehensive and multi-angle analysis of PRP treatment of meniscal injury in terms of pain, knee joint function, range of motion, and the failure rate based on the most recently published randomized controlled trials (RCTs) and cohort studies. Our goal is to provide reliable evidence for the use of PRP in the clinical treatment of meniscal injury.
Materials and methods
The present meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses. This meta-analysis did not require ethical approval because it only involved a secondary analysis of information already published in scientific databases.
Search method for identification of studies
The search strategy was based on the standards formulated by the Cochrane Collaboration. Subject words and free words were “platelet-rich plasma,” “thrombocyte-rich plasma,” “meniscus,” and “menisci.” Boolean operators were used to search for relevant papers in the PubMed, Embase, and Cochrane Library databases. Additionally references within relevant articles were manually retrieved. Article retrieval was performed in PubMed as follows: Search (((“Meniscus” [MeSH]) OR ((((((((((Menisci) OR disk, knee) OR disk, knee joint) OR knee cartilage) OR knee disk) OR knee joint cartilage) OR semilunar cartilage) OR Semilunar Cartilages) OR Cartilage, Semilunar) OR Cartilages, Semilunar))) AND ((“Platelet-Rich Plasma” [MeSH]) OR (((Plasma, Platelet-Rich) OR Platelet Rich Plasma) OR thrombocyte rich plasma)).
Eligibility criteria
Inclusion criteria
Studies that met all of the following criteria were considered for inclusion.
The study involved male or female patients with meniscal injury in the left or right knee joint.
Patients who received PRP injection were included in the experimental group, and those who received placebo injection or no injection were included in the control group.
The article contained complete original data including at least one of the following: visual analog scale (VAS) score, International Knee Documentation Committee (IKDC) score, Lysholm score, active flexion, and failure rate.
The data were true and credible. Indicators that could be transformed into binary or continuous variables were used.
Exclusion criteria
Studies that met one or more of the following conditions were excluded from this meta-analysis.
The study included patients with a clear history of trauma before the onset of meniscal injury.
The study included patients with arthritis.
The study included patients with diabetes, rheumatic disease, severe cardiovascular disease, infection, or immunosuppression.
The study included patients with hematological disease (coagulopathy) or liver and kidney dysfunction, patients receiving anticoagulant therapy, or patients who had used nonsteroidal anti-inflammatory drugs for more than 5 days.
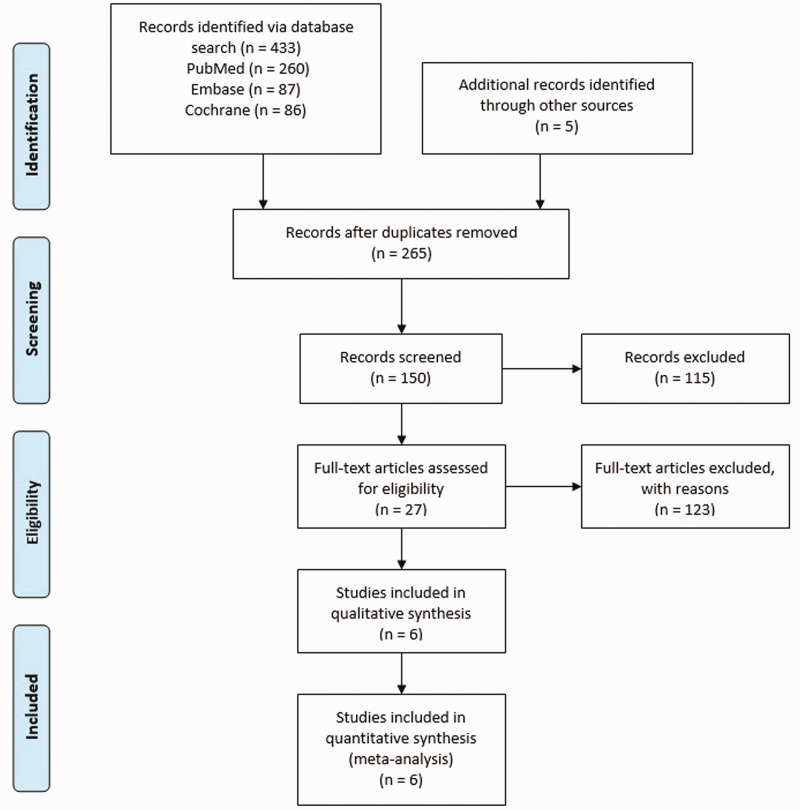
A flowchart of the study selection for the present meta-analysis is shown in Figure 1.
Figure 1.
Flowchart of study selection in the present meta-analysis.
Outcome measures
The following outcome measures were used to evaluate the curative effects.
IKDC score: The IKDC score can be used to evaluate various diseases of the knee joint. It can be used to comprehensively evaluate subjective symptoms and objective signs of the knee joint, with a higher score indicating a better therapeutic effect.
Lysholm score: The Lysholm scale is a questionnaire-like rating scale that is used to evaluate various knee joint diseases. The scale allows for simple and clear evaluation of the local function of the patient’s knee joint. This score is more inclined to reflect the life of the general population, with a higher score indicating a better curative effect. Greater changes in the score are indicative of better curative effects.
Active flexion: This is used to evaluate the degree of knee flexion, with greater knee flexion indicating better postoperative recovery.
Change in VAS score: This refers to the change in the VAS score relative to the baseline. A smaller change in the VAS score indicates a better curative effect.
Failure rate: Failure of surgery implies that repeat meniscectomy is required after the operation. The failure rate can be used to evaluate the effect of the operation.
Assessment of methodological quality
Two investigators independently used the Jadad scale to evaluate the quality of the included RCTs, with scores of <4 indicating low quality.7 The Newcastle–Ottawa Scale (NOS) was used to assess the quality of the cohort studies, with scores of <5 indicating low quality. When the two investigators did not agree with each other, a third investigator was asked to help resolve the disagreement after a discussion between the two investigators.
Data collection
Two investigators independently extracted data from all feasible studies according to a standard data extraction form. Any objections were resolved as described above.
If the data reported in the article were incomplete, the corresponding author was contacted by e-mail to obtain the original data; however, no response was received. In some cases, if the standard deviation was not reported and no response was obtained from the authors, we referred to the article published by Hou et al.10 The range or median was estimated or the method described in the Cochrane Handbook for Systematic Reviews of Interventions was used to convert the data, and the standard deviation was estimated based on the confidence interval (CI).
Statistical analysis
Heterogeneity among the included studies was tested and analyzed using the chi-squared test. When I2 > 50%, a random-effects model was used; otherwise, a fixed-effects model was used. The relative risk was calculated for binary variables, and the standardized mean difference (SMD) was calculated for continuous variables.8 The 95% CI estimates and the hypothesis test results for each variable were listed in a forest plot. Outcome indicators with significant heterogeneity were excluded from the literature one after the other, and a sensitivity analysis was performed to assess the source of heterogeneity. The results of more than 10 articles at one time were tested for publication bias using a funnel plot and Egger’s test. Statistical analyses were performed using RevMan version 5.3 (The Nordic Cochrane Centre, Copenhagen, Denmark).
Results
Search results and characteristics of selected studies
Of the 265 potentially suitable pieces of literature, 6 studies involving 293 patients met our inclusion criteria11–16 (Figure 1). Of these six studies, three were RCTs and three were cohort studies. The experimental group comprised 157 patients and the control group comprised 136 patients. The quality of each RCT was scored according to the Jadad scale, and that of each cohort study was evaluated using the NOS. The basic characteristics and scores of the included studies are shown in Table 1. The outcomes are shown in Table 2. The Jadad scale scores ranged from 5 to 7, and two articles were of high quality. The NOS scores ranged from 5 to 6, and three articles were of high quality.
Table 1.
Main characteristics of all eligible studies included in the meta-analysis.
| Authors, year [Ref] | Research type |
Patients (n) |
Mean age (years) |
Follow-up (months) |
Jadad/NOS | |||
|---|---|---|---|---|---|---|---|---|
| Surg | NS | Surg | NS | Surg | NS | |||
| Pujol et al., 2014 [11] | Cohort | 17 | 17 | 28.3 | 32.3 | 30 | 34 | 5 |
| Duif et al., 2015 [12] | RCT | 15 | 20 | 64.1 | 64.3 | 12 | 12 | 5 |
| Griffin et al., 2015 [13] | Cohort | 53 | 44 | 26 | 35 | 48 | 48 | 6 |
| Kaminski et al., 2018 [14] | RCT | 21 | 18 | 30 | 26 | 54 | 54 | 7 |
| Dai et al., 2019 [15] | Cohort | 14 | 15 | 32.4 | 30.3 | 20.6 | 20.6 | 6 |
| Kaminski et al., 2019 [16] | RCT | 37 | 22 | 44 | 46 | 23 | 23 | 7 |
RCT, randomized controlled trial; Surg, surgical intervention; NS, nonsurgical intervention; NOS, Newcastle–Ottawa Scale.
Table 2.
Selection of surgical outcomes.
| Authors, year [Ref] |
IKDC score |
Lysholm score |
VAS score |
Active flexion |
Failure rate |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Surg | NS | Surg | NS | Surg | NS | Surg | NS | Surg | NS | |
| Pujol et al. 2014 [11] | 90.7 ± 13 | 87.9 ± 25.25 | 135 ± 6.25 | 130 ± 6.25 | 1/17 | 2/17 | ||||
| Duif et al., 2015 [12] | 83.2 ± 18 | 70 ± 17.1 | −1.5 ± 2.27 | −0.7 ± 2.11 | ||||||
| Griffin et al., 2015 [13] | 69 ± 26 | 76 ± 17 | 66 ± 31.9 | 89 ± 9.7 | 125 ± 11.25 | 119 ± 10 | 4/15 | 5/29 | ||
| Kaminski et al., 2018 [14] | 97.56 ± 0.63 | 84.77 ± 0.92 | −5.37 ± 0.1 | −4.17 ± 0.11 | 3/20 | 9/17 | ||||
| Dai et al., 2019 [15] | 79.8 ± 9.6 | 74.6 ± 11.6 | −2.9 ± 1 | −1.8 ± 1.21 | ||||||
| Kaminski et al., 2019 [16] | 85.98 ± 0.52 | 88.12 ± 0.89 | −3.62 ± 0.07 | −2.36 ± 0.09 | 13/27 | 19/27 | ||||
Data are presented as mean ± standard deviation or number of patients.
IKDC, International Knee Documentation Committee; VAS, visual analog scale; Surg, surgical intervention; NS, nonsurgical intervention.
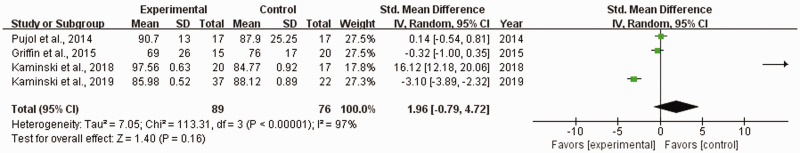
IKDC score
Four studies11,13,14,16 reported IKDC scores among 165 patients. When I2 = 97%, a random-effects model was used. There was no significant difference in the IKDC score between the experimental and control groups (SMD, 1.96; 95% CI, −0.79 to 4.72). The sensitivity analysis showed that after excluding two studies conducted by Kaminski et al.,14,16 the I2 decreased to 0% and the conclusion was not altered (Figure 2).
Figure 2.
Forest plot of International Knee Documentation Committee score.
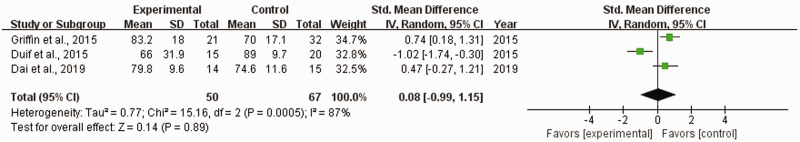
Lysholm score
Three studies12,13,15 reported the Lysholm score among 117 patients. When I2 = 87%, a random-effects model was used. There was no significant difference in the Lysholm score between the experimental and control groups (SMD, 0.08; 95% CI, −0.99 to 1.15). The sensitivity analysis showed that after excluding the study conducted by Griffin et al.,13 the I2 decreased to 0% and the Lysholm score in the experimental group was significantly higher than that in the control group (SMD, 0.64; 95% CI, 0.19–1.10; P = 0.005) (Figure 3).
Figure 3.
Forest plot of Lysholm score.
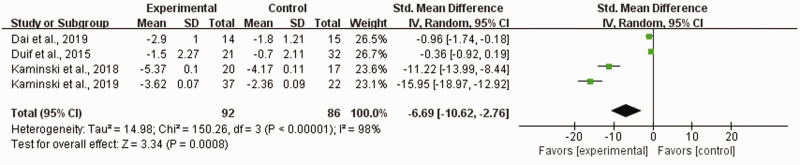
Change in VAS score
Four studies12,14–16 reported the VAS score among 178 patients. When I2 = 98%, a random-effects model was used. The change in the VAS score in the experimental group was significantly smaller than that in the control group (SMD, −6.69; 95% CI, −10.62 to −2.76; P = 0.0008). The sensitivity analysis showed that after excluding the studies conducted by Kaminski et al.,14,16 the I2 decreased to 34% and the conclusion was not altered (SMD, −0.60; 95% CI, −1.17 to −0.03; P = 0.04) (Figure 4).
Figure 4.
Forest plot of visual analog scale score change.
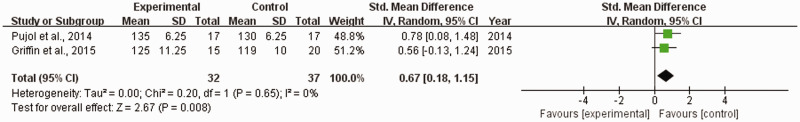
Active flexion
Two studies11,13 reported on active flexion among 69 patients. When I2 = 0%, a random-effects model was used. The range of active flexion in the experimental group was significantly greater than that in the control group (SMD, 0.67; 95% CI, 0.18–1.15; P = 0.008) (Figure 5).
Figure 5.
Forest plot of active flexion.
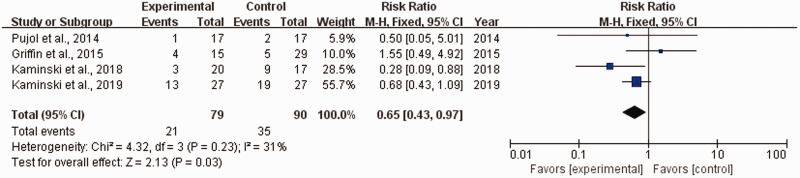
Failure rate
Four studies11,12,14,16 reported on the failure rate among 169 patients. When I2 = 31%, a random-effects model was used. The failure rate in the experimental group was significantly lower than that in the control group (relative risk, 0.65; 95% CI, 0.43–0.97; P = 0.03) (Figure 6).
Figure 6.
Forest plot of failure rate.
Discussion
Surgery combined with PRP is more effective than surgery alone for meniscal injuries. In the present meta-analysis, the postoperative VAS score decreased more obviously and active flexion of the knee was greater in the experimental group than in the control group. Although there were no significant differences in the IKDC and Lysholm scores between the experimental and control groups, the failure rate was significantly lower in the experimental group than in the control group. These findings suggest that PRP has obvious advantages in the treatment of meniscal injuries.
The failure rate is the most important outcome index of meniscal injury. We aim to preserve as much of the meniscus as possible and improve its regeneration and self-healing abilities. The results of this meta-analysis showed that treatment of meniscal injury with PRP yielded a lower collapse rate. This positive effect may be due to the tissue improving the delivery of factors such as fibroblast growth factor, transforming growth factor-β1, platelet-derived growth factor, vascular endothelial growth factor, and PRP.17 These growth factors are considered to promote chemotaxis, angiogenesis, collagen matrix synthesis, and cell proliferation.18 This phenomenon may depend on the release of a mixture of growth factors and the triggering of synovial tissue to create a more balanced intra-articular environment. Recent studies have linked synovium-derived stem cells with cartilage regeneration because of these cells’ potential for cartilage formation and the encouraging results of cartilage repair in experimental studies.19 Thus, the risk of repair failure can be effectively avoided.
The VAS score is used to evaluate pain. In this meta-analysis, the change in the VAS score was significantly smaller in the experimental group than in the control group; in other words, the pain intensity was lower in the experimental group than in the control group. In the sensitivity analysis, two articles by Kaminski et al.14,16 were omitted; as a result, the I2 decreased to 34% and the conclusion remained unchanged. The heterogeneity might have been the result of a longer follow-up time in the studies conducted by Kaminski et al.14,16; i.e., the pain intensity was low at the last follow-up, resulting in high heterogeneity. A previous study showed that high concentrations of cell growth factors in PRP may not only promote stem cell proliferation and differentiation but also inhibit inflammation.20 This may be the theoretical basis for the use of PRP injection to relieve pain and improve knee joint function in a short period of time.
The IKDC and Lysholm scores are used to evaluate postoperative recovery of basic knee joint functions. The results of the studies included in this meta-analysis showed no significant differences in the IKDC and Lysholm scores between the experimental and control groups. However, while the results of the sensitivity analysis on the IKDC score remained unchanged, the Lysholm score was significantly higher in the experimental group than in the control group. In other words, the functional recovery of the knee joint was better in the experimental group than in the control group. This requires further investigation based on a larger number of studies. This might have occurred because of the small number of cases; different physical conditions of the patients, such as age, body mass index, and the extent and location of meniscal injury; and smoking. Age and body mass index affect collagen synthesis and cartilage degeneration in the knee joint, which in turn affect the repair of meniscal injury. A recent study showed that smoking affects meniscal healing.21 Among the studies included in this meta-analysis, only the study conducted by Griffin et al.13 investigated the influence of smoking on meniscal injury. Although the difference was not significant, the IKDC score was higher in the experimental group than in the control group. This finding may be confirmed by a study involving a larger sample size and a longer follow-up period.
The degree of active flexion was greater in the experimental group than in the control group. This might have occurred because PRP can reduce joint swelling and effusion; additionally, pain alleviation is conducive to active and passive functional exercises, leading to natural expansion of the scope and level of knee motion.12
Strengths and limitations
This meta-analysis comprehensively evaluated several indicators related to the treatment of meniscal injury. The degree of change was considered when scoring the indicators to remove the impact of different baseline conditions and make the results more objective.
This meta-analysis had two main limitations. (1) Neither regression analysis nor other methods were used to identify the source of heterogeneity, and publication bias was not evaluated because fewer than 10 studies were included. (2) There are no uniform standards for PRP preparation and application, which may have led to heterogeneity among the studies.
Conclusion
The findings of this meta-analysis suggest that PRP exhibits obvious advantages in the treatment of meniscal injury. Although the IKDC and Lysholm indicators did not improve significantly in the short-term follow-up, PRP injection can reduce postoperative pain, improve knee flexion, and decrease the failure rate of the operation.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD
Wenlai Guo https://orcid.org/0000-0002-3494-9076
References
- 1.Mankin HJ. The response of articular cartilage to mechanical injury. J Bone Joint Surg 1982; 64: 460–466. [PubMed] [Google Scholar]
- 2.Hunter W. Of the structure and disease of articulating cartilages. Clin Orthop Relat Res 1995; 42: 3–6. [PubMed] [Google Scholar]
- 3.Buckwalter JA, Martin J, Mankin HJ. Synovial joint degeneration and the syndrome of osteoarthritis. Instr Course Lect 2000; 49: 481–489. [PubMed] [Google Scholar]
- 4.Espejo-Reina A, Serrano-Fernández JM, Martín-Castilla B, et al. Outcomes after repair of chronic bucket-handle tears of medial meniscus. Arthroscopy 2014; 30: 492–496. [DOI] [PubMed] [Google Scholar]
- 5.Noyes FR, Barber-Westin SD. Management of meniscus tears that extend into the avascular region. Clin Sports Med 2012; 31: 65–90. [DOI] [PubMed] [Google Scholar]
- 6.Yamada Y, Ueda M, Naiki T, et al. Autogenous injectable bone for regeneration with mesenchymal stem cells and platelet-rich plasma: tissue-engineered bone regeneration. Tissue Eng 2004; 10: 955–964. [DOI] [PubMed] [Google Scholar]
- 7.Eppley BL, Pietrzak WS, Blanton M. Platelet-rich plasma: a review of biology and applications in plastic surgery. Plast Reconstr Surg 2006; 118: 147e–159e. [DOI] [PubMed] [Google Scholar]
- 8.Miron R, Fujioka-Kobayashi M, Bishara M, et al. Platelet rich fibrin and soft tissue wound healing: a systematic review. Tissue Eng Part B Rev 2017; 23: 83–99. [DOI] [PubMed] [Google Scholar]
- 9.Haunschild ED, Huddleston HP, Chahla J, et al. Platelet-rich plasma augmentation in meniscal repair surgery: a systematic review of comparative studies. Arthroscopy 2020; 36: 1765–1774. [DOI] [PubMed] [Google Scholar]
- 10.Hou XW Shi JP, andChen X.. How to estimate the mean and standard deviation based on the median, range and sample size when conducting meta-analysis. Chinese Journal of Evidence-based Medicine 2015; 15: 484–487. doi:10.7507/1672-2531.20150080 [Google Scholar]
- 11.Pujol N, De Chou ES, Boisrenoult P, et al. Platelet-rich plasma for open meniscal repair in young patients: Any benefit? Knee Surg Sports Traumatol Arthrosc 2015; 23: 51–58. [DOI] [PubMed] [Google Scholar]
- 12.Duif C, Vogel T, Topcuoglu F, et al. Does intraoperative application of leukocyte-poor platelet-rich plasma during arthroscopy for knee degeneration affect postoperative pain, function and quality of life? A 12-month randomized controlled double-blind trial. Arch Orthop Trauma Surg 2015; 135: 971–977. doi:10.1007/s00402-015-2227-5 [DOI] [PubMed] [Google Scholar]
- 13.Griffin JW, Hadeed MM, Werner BC, et al. Platelet-rich plasma in meniscal repair: does augmentation improve surgical outcomes? Clin Orthop Relat Res 2015; 473: 1665–1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaminski R, Kulinski K, Kozar-Kaminska K, et al. A prospective, randomized, double-blind, parallel-group, placebo-controlled study evaluating meniscal healing, clinical outcomes, and safety in patients undergoing meniscal repair of unstable, complete vertical meniscal tears (bucket handle) augmented with platelet-rich plasma. Biomed Res Int 2018; 2018: 9315815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dai WL, Zhang H, Lin ZM, et al. Efficacy of platelet-rich plasma in arthroscopic repair for discoid lateral meniscus tears. BMC Musculoskelet Disord 2019; 20: 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaminski R, Maksymowicz-Wleklik M, Kulinski K, et al. Short-term outcomes of percutaneous trephination with a platelet rich plasma intrameniscal injection for the repair of degenerative meniscal lesions. A prospective, randomized, double-blind, parallel-group, placebo-controlled study. Int J Mol Sci 2019; 20: 856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cole BJ, Seroyer ST, Filardo G, et al. Platelet-rich plasma: where are we now and where are we going? Sports Health 2010; 3: 203–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jain NK, Gulati M. Platelet-rich plasma: a healing virtuoso. Blood Res 2016; 51: 3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kubosch EJ, Lang G, Furst D, et al. The potential for synovium derived stem cells in cartilage repair. Curr Stem Cell Res Ther 2018; 13: 174–184. [DOI] [PubMed] [Google Scholar]
- 20.Marx RE. Platelet-rich plasma (PRP): what is PRP and what is not PRP? Implant Dent 2001; 10: 225–228. [DOI] [PubMed] [Google Scholar]
- 21.Uzun E, Misir A, Kizkapan TB, et al. Factors affecting the outcomes of arthroscopically repaired traumatic vertical longitudinal medial meniscal tears. Orthop J Sports Med 2017; 5: 2325967117712448. [DOI] [PMC free article] [PubMed] [Google Scholar]