Abstract
Introduction:
Type 2 diabetes mellitus patients with hypertension are at high risk of drug therapy problems since they are subject to receive multiple drug therapies due to comorbidities.
Objectives:
To determine the magnitude of drug therapy problems and its determinants among Type 2 diabetes mellitus patients with hypertension.
Methods:
A cross-sectional study was employed among 423 randomly selected participants based on the inclusion criteria. A structured questionnaire and review of patients’ medical record were employed in the data collection. The classification system used by Cipolle was used to classify and evaluate drug therapy problems. Data were analyzed using Statistical Package for the social sciences version 25.0 software. Multivariate logistic regression analysis was used to identify determinants of drug therapy problems with a statistical significance of p ⩽ 0.05.
Results:
A total of 491 drug therapy problems with a mean of 1.86 ± 0.53 drug therapy problems per patient were identified, and 62.4% (264) of them experienced at least one drug therapy problem. Non-compliance (197, 40.1%), needs of additional drug therapy (119, 24.2%), and dosage too low (91, 18.5%) were the most frequently observed drug therapy problems in the study setting. Anti-diabetic medications (88.4%), statins (44.5%), and aspirin (33.5%) were the most commonly involved drugs in drug therapy problems. The determinants of drug therapy problems were very low family income (adjusted odds ratio = 4.64, p = 0.010), age (45–65 years old) (adjusted odds ratio = 2.55, p = 0.008), presence of comorbidity (adjusted odds ratio = 9.19, p < 0.001), and taking ⩾5 medications (adjusted odds ratio = 2.84, p = 0.001).
Conclusion:
Approximately three out of five patients had one or more drug therapy problems encountered. In this study, the most common types of drug therapy problems were non-compliance, needs additional drug therapy, and dosage too low. Family monthly income, age, comorbidities, and number of medications were the significant determinants of drug therapy problems. Therefore, patient education regarding medication adherence, routine medication review, and strengthening clinical pharmacy services should be promoted.
Keywords: Drug therapy problem, hypertension, type 2 diabetes mellitus, Ethiopia
Introduction
According to the global and regional diabetes prevalence, around 9.3% (463 million people) of the world population had diabetes in 2019. The prevalence is expected to rise to 10.2% (578 million) by 2030 and 10.9% (700 million) by 2045, which contributes to 4.6 million deaths globally.1,2 Diabetes is associated with significant morbidity and mortality in the 21st century, which poses a substantial challenge to the health care system.1 Hypertension is a common comorbidity in diabetic patients. Approximately 66% of these patients lived in developing countries.2,3 Hypertension raises the risk of macrovascular and microvascular complications3–5 and increases mortality risk by 7.2-fold in Type 2 diabetes mellitus (T2DM) patients.6 This condition is even more worse in developing countries.7 Sixty percent of all deaths associated with non-communicable diseases were contributed by T2DM patients with hypertension. Of these, more than three-fourths of the deaths occur in low- and middle-income countries.8
Although pharmacotherapy plays a vital role in T2DM management, achieving targeted blood sugar levels in these patients remains challenging.9 Studies showed that about two-thirds of T2DM patients with hypertension did not achieve target blood sugar level and blood pressure10–12 mainly due to the development of drug therapy problems (DTPs).6,13 In Ethiopia, studies reported that 42.3%–90.5% of these patients experienced at least one DTP,14–17 which are responsible for sub-optimal sugar levels, disease worsening, frequent hospital admission, longer hospital stays,18,19 increased healthcare costs, and mortality.20 Despite all these, approximately 50% of the adverse effects were preventable.21–23 Various studies have shown that age, medication non-adherence, comorbidity, polypharmacy, and history of hospitalization were independent predictors of DTPs.16,24,25
In Ethiopia, studies revealed that DTPs are common in the healthcare system. However, there is a lack of data regarding the magnitude of DTPs and associated factors in T2DM patients with hypertension. Therefore, this study aimed at investigating the magnitude of DTPs and its determinants among these patients at Felege Hiwot Specialized Comprehensive Hospital (FHSCH). This study can provide baseline information to assess the financial and healthcare burden of DTPs. The finding can also be used as an input to design appropriate preventive measures of DTPs among T2DM patients with hypertension.
Methods
Study setting, period, and study design
A cross-sectional study was employed among T2DM patients with hypertension at FHSCH, which is located 665 km to Northwest of Addis Ababa. This teaching hospital offers numerous clinical services for 12 million populations in the catchment area and serves as a referral for other primary and general hospitals. The data were collected from 1 October to 30 December 2019.
Eligibility criteria
All T2DM patients with hypertension aged 18 years and above, who underwent chronic follow-up at FHSCH during the study data collection period, were included. Nonetheless, critically ill patients, mentally ill patients, and patients with incomplete medical records were excluded.
Sample size determination
The sample size was calculated using a single population proportion formula26 as follows
where n = is desired sample size; Zα/2 = is standard normal distribution at 95% confidence level usually 1.96, p = proportion of T2DM patients with hypertension who had DTPs (p = 0.5) and q = proportion of T2DM patients with hypertension who had not DTPs (q = 0.5), and d = marginal error (5% = 0.05)
After adding a 10% contingency, 423 study participants were considered in the study.
Sampling technique and sampling procedure
A simple random sampling technique was used when the study participants came to the clinic for their routine medical checkup. Throughout the data collection period, lists of T2DM patients with hypertension were collected regularly from the outpatient clinic. After eligibility was verified, a unique patient identification number was taken and written on a piece of paper, folded, and stored in a bin. The principal investigators then randomly selected the study participants until they get the required sample size.
Data collection tool and procedure
A structured questionnaire was prepared considering the pretest result, which was conducted in 5% of the sample size at Debre Tabor Referral Hospital, to ensure the validity of the data collection instrument. It contained sociodemographic characteristics, clinically related information, treatment regimens, comorbidities, and a history of hospitalization. The study participants’ sociodemographics were collected during the patients’ hospital visit, while other clinical and medication-related information were retrospectively reviewed from patients’ medical records. Besides, DTPs were evaluated and classified using Cipolle’s DTP identification tool (Online Appendix I).27,28 This classification system is the most commonly used in the Ethiopian healthcare system. The identified DTPs were categorized into seven categories (need additional drug therapy, unnecessary drug therapy, ineffective drug therapy, dose too low, adverse drug reaction, and dose too high and non-compliance). DTPs were assessed by four pharmacists, and the possible causes of DTPs were identified from the patients’ medical records and interviews, in reference to the standard guidelines.7,29–33
Data analysis
The data were analyzed using the statistical program SPSS version 25.0. Descriptive statistics such as frequency, percentage, and mean with standard deviations were computed to describe the independent variables. Logistic regression analysis was performed to investigate the determinants of DTPs. All variables with p < 0.20 in the bivariate analysis were considered for further analysis in the multivariate logistic regression. The odds ratio and confidence interval (95% CI) were reported, and p-value ⩽ 0.05 considered statistically significant.
Ethical considerations
The study was approved by the Ethical Review Board of Debre Tabor University (Approval number: 1987/2019), and subsequent permission was obtained from the Medical Record Department of FHSCH. We have obtained patient written consent to use their medical records while the patient came to the clinic for routine medical checkups. Patients’ personal information and clinical information were recorded by ensuring patient confidentiality.
Operational definition of terms
Adult T2DM patients with hypertension: Patients aged 18 years and above who had both T2DM and hypertension.
Drug therapy problems: Any undesirable event experienced by a patient involves drug therapy that interferes with achieving the desired goals of treatment.27
Medications: Are pharmaceutical products used to treat or prevent diseases.
Results
Sociodemographic characteristics of patients
A total of 423 study participants were included in this study, and more than half (53.2%) were males. The mean age of the study participants was 58.04 ± 11.56 years. In addition, nearly one-third (32.6%) of the study participants were merchants, and the majority (80.4%) were married. In this study, 42.6% and 35.1% of the study participants attended primary school and College/University level of education, respectively. Furthermore, 12.5% and 38.5% were smokers and drinkers, respectively (Table 1).
Table 1.
Sociodemographic characteristics of patients with diabetes and hypertension (n = 423).
| Variables | Categories | Frequency (%) |
|---|---|---|
| Sex | Male | 225 (53.2) |
| Female | 198 (46.8) | |
| Age in years | <45 | 73 (17.3) |
| 45–65 | 251 (59.3) | |
| >65 | 99 (23.4) | |
| Marital status | Single | 4 (0.9) |
| Married | 340 (80.4) | |
| Divorced | 52 (12.3) | |
| Widowed | 27 (6.4) | |
| Occupation | Farmer | 80 (18.9) |
| Employed | 130 (30.7) | |
| Merchant | 138 (32.6) | |
| House wife | 58 (13.7) | |
| Retired | 17 (4.0) | |
| Educational status | No formal education | 73 (17.3) |
| Primary (1–8) | 180 (42.6) | |
| Secondary (9–12) | 21 (5.0) | |
| College/University | 149 (35.1) | |
| Monthly family income | Very low (⩽860) | 46 (10.9) |
| Low (861–3000) | 64 (15.1) | |
| Average (3001–5000) | 99 (23.4) | |
| High (⩾5001) | 214 (50.6) | |
| Smoking status | Smoker | 53 (12.5) |
| Non-smoker | 370 (87.5) | |
| Alcohol consumption | Yes | 163 (38.5) |
| No | 260 (61.5) |
Clinical characteristics of study participants
The mean duration of T2DM with hypertension among study participants was 4.78 ± 2.98 years, and about one-fourth of them (23.9%) had a history of hospitalization. The most frequently diagnosed comorbidities were ischemic heart disease (50.7%), peptic ulcer disease (21.7%), and heart failure (14.5%). Furthermore, half of the patients had an unregulated blood glucose level (55.6%) and blood pressure (54.4%) (Table 2).
Table 2.
Clinical characteristics of patients with diabetes and hypertension (n = 423).
| Variables | Categories | Frequency (%) |
|---|---|---|
| Duration of the disease (years) | Mean ± SD | 4.78 ± 2.98 |
| 1–5 | 331 (78.3) | |
| >5 | 92 (21.7) | |
| History of hospitalization | Yes | 101 (23.9) |
| No | 322 (76.1) | |
| Comorbidities other than HTN | Present | 152 (35.9) |
| Absent | 271 (64.1) | |
| Specific comorbidities (n = 152) | Ischemic heart disease | 71 (46.7) |
| Peptic ulcer disease | 30 (19.7) | |
| Heart failure | 19 (12.5) | |
| Dyslipidemia | 11 (7.2) | |
| Infections | 5 (3.3) | |
| Othersa | 16 (10.5) | |
| FBS at last visit (mg/dL) | <70 | 8 (1.9) |
| 70–130 | 180 (42.6) | |
| >130 | 235 (55.6) | |
| BP at last visit (mmHg) | ⩽140/90 | 193 (45.6) |
| >140/90 | 230 (54.4) |
BP: blood pressure; FBS: fast blood sugar; SD: standard deviation; HTN: hypertension.
Asthma, chronic obstructive pulmonary disease, epilepsy, and thyroid disorder.
Pattern of prescribed medications in T2DM patients with hypertension
Patients used an average of 3.57 ± 1.42 medications per encounter. Most of the patients (87.5%) used oral hypoglycemic agents (OHGA) alone followed by insulin alone (4.3%) and either agent (8.3%) to manage diabetes. In addition, angiotensin-converting enzyme inhibitors (29.1%) and calcium channel blockers (17.7%) were the most frequently prescribed medications for managing hypertension. Furthermore, other groups of widely prescribed drugs include statins (60.8%), aspirin (28.1%), proton pump inhibitors (11.3%), and antibiotics (11.1%) (Table 3).
Table 3.
Prescribed medications among patients with diabetes and hypertension (n = 423).
| Treatment | Categories | Frequency (%) |
|---|---|---|
| Anti-diabetic treatment regimen | OHGA alone | 370 (87.5) |
| OHGA + Insulin | 35 (8.3) | |
| Insulin alone | 18 (4.3) | |
| Specific anti-diabetic medications | Glibenclamide | 14 (3.3) |
| Metformin | 251 (59.3) | |
| Metformin + Glibenclamide | 105 (24.8) | |
| Metformin + Insulin | 35 (8.3) | |
| Anti-hypertensive | Angiotensin-converting enzyme inhibitors | 123 (29.1) |
| Calcium channel blockers | 75 (17.7) | |
| Diuretics | 49 (11.6) | |
| Beta blockers | 25 (5.9) | |
| Combined classes | 151 (35.7) | |
| Other medications | Statins | 257 (60.8) |
| Aspirin | 119 (28.1) | |
| Proton pump inhibitors | 48 (11.3) | |
| Antibiotics | 47 (11.1) | |
| Anti-asthmatics | 17 (4.0) | |
| Othersa | 37 (8.7) | |
| Number of medications per patient | Mean ± SD | 3.57 ± 1.45 |
| Below (<5) | 248 (58.6) | |
| Above (⩾5) | 175 (41.4) |
SD: standard deviation; OHGA: oral hypoglycemic agents.
Amitriptyline, carbamazepine, gabapentin, tramadol, and propylthiouracil.
Magnitude of DTP in T2DM with hypertension patients
In this study, 62.4% (264) of patients experienced one or more DTPs with a mean of 1.86 ± 0.53 DTPs per patient. Besides, the majority of patients with DTPs (70.4%) experienced two or more DTPs. The most frequently observed DTPs were non-compliance (40.1%), needs of additional drug therapy (24.2%), and dose too low (18.5%) (Table 4).
Table 4.
Categories of drug therapy problems among type 2 diabetic with hypertension patients (n = 491).
| Drug therapy problems and causes | Frequency (%) | |
|---|---|---|
| Non-compliance | 197 (40.1) | |
| Forgets to take medications | 73 (14.9) | |
| Drug product too expensive for the patient | 51 (10.4) | |
| Does not understand the instruction | 45 (9.2) | |
| Cannot swallow or self-administer the drug product appropriately | 17 (3.5) | |
| The drug product is not available for the patient | 11 (2.2) | |
| Need additional drug therapy | 119 (24.2) | |
| Preventive drug therapy required | 81 (16.5) | |
| A medical condition that requires treatment | 29 (5.9) | |
| To attain synergistic effect | 9 (1.8) | |
| Dose too low | 91 (18.5) | |
| The dose is too low to produce the desired effect | 57 (11.6) | |
| The dosing is too infrequent to produce the desired effect | 34 (6.9) | |
| Unnecessary drug therapy | 41 (8.4) | |
| Duplication drug therapy | 23 (4.7) | |
| No valid medical indication for the drug therapy at this time | 18 (3.7) | |
| Ineffective drug therapy | 21 (4.3) | |
| Inappropriate drug selection | 21 (4.3) | |
| Adverse drug reaction | 15 (3.1) | |
| Undesirable drug effect | 11 (2.2) | |
| Unsafe or the patient/contraindication | 4 (0.8) | |
| Dose too high | 7 (1.4) | |
| Total number of identified DTPs (mean ± SD) | 491 (1.86 ± 0.53) | |
| Total number of participants with DTPs | 264 (62.4) | |
| Number of DTPs | One | 78 (29.6) |
| Two | 145 (54.9) | |
| ⩾Three | 41 (15.5) | |
DTPs: drug therapy problems; SD: standard deviation.
The combination of metformin and glibenclamide (83, 50.6%), metformin (62, 37.8%), and β-blockers (17, 10.4%) were the most frequently reported drugs involved in DTPs. In addition, statins (73, 44.5%) and aspirin (55, 33.5%) had also contributed to DTPs (Figure 1).
Figure 1.
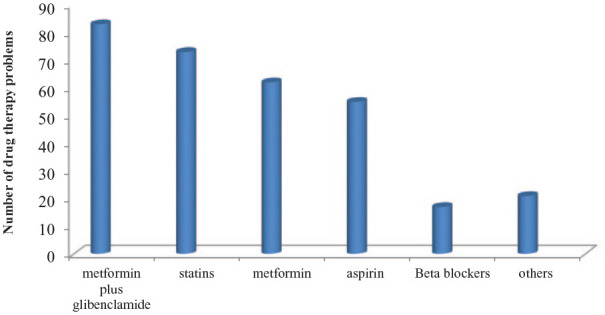
Common drugs involved in each category of drug therapy problems among the study participants.
Determinants of DTPs
The multivariate logistic regression analysis showed that age, monthly family income, comorbidity, and number of medications were determinants of DTPs. Middle-aged patients were three (adjusted odds ratio (AOR) = 2.55, 95% CI: 1.28–5.11, p = 0.008) times more susceptible to DTPs than the younger age patients. In addition, patients with very low monthly family income were five (AOR = 4.64, 95% CI: 1.44–14.99, p = 0.010) times more likely to experience DTPs than high-income patients. Furthermore, patients with comorbidity were nine (AOR = 9.19, 95% CI: 4.78–17.69, p < 0.001) times more likely to have DTPs than their counterparts. Furthermore, patients taking five or more (AOR = 2.84, 95% CI: 1.72–4.70, p = 0.001) were three times more likely to experience DTPs (Table 5).
Table 5.
Univariate and multivariate binary logistic regression analysis of predictors of drug therapy problems.
| Variables | Categories | Drug therapy problem |
Univariate analysis |
Multivariate analysis |
||
|---|---|---|---|---|---|---|
| No, N (%) | Yes, N (%) | COR (95% CI) | AOR (95% CI) | p-value | ||
| Sex | Male | 96 (60.4) | 129 (48.9) | 1 | 1 | |
| Female | 63 (39.6) | 135 (51.1) | 1.60 (1.07–2.38)* | 1.62 (0.91–2.88) | 0.104 | |
| Age | <45 | 36 (22.6) | 37 (14.0) | 1 | 1 | |
| 45–65 | 101(63.5) | 200 (75.8) | 1.93 (1.07–2.38)* | 2.55 (1.28–5.11) | 0.008 | |
| >65 | 22 (13.9) | 27 (10.2) | 1.19 (0.58–2.47) | 1.60 (0.55–4.65) | 0.386 | |
| Marital status | Single | 1 (0.6) | 3 (1.1) | 2.79 (0.26–30.27) | 0.88 (0.05–14.89) | 0.929 |
| Married | 130 (81.8) | 210 (79.5) | 1.50 (0.68–3.29) | 0.98 (0.36–2.68) | 0.971 | |
| Divorced | 16 (10.1) | 36 (13.6) | 2.09 (080–5.44) | 1.13 (0.34–3.76) | 0.839 | |
| Widowed | 12 (7.6) | 15 (5.7) | 1 | 1 | ||
| Family income | Very low (⩾860) | 5 (3.1) | 23 (8.7) | 3.71 (1.37–10.06)* | 4.64 (1.44–14.99) | 0.010 |
| Low (861–3000) | 13 (8.2) | 33 (12.5) | 1.84 (0.94–3.62)* | 1.42 (0.62–3.25) | 0.408 | |
| Average (3001–5000) | 29 (18.2) | 69 (26.1) | 1.92 (1.16–3.16)* | 1.82 (0.91–3.65) | 0.092 | |
| High (⩾5001) | 112 (70.4) | 139 (52.7) | 1 | 1 | ||
| Educational status | Cannot read and write | 29 (18.2) | 44 (16.7) | 1.31 (0.74–2.31) | 0.51 (0.06–4.36) | 0.538 |
| Primary | 57 (35.8) | 123 (46.6) | 1.86 (1.19–2.92)* | 1.34 (0.16–10.97) | 0.787 | |
| Secondary | 5 (3.1) | 16 (6.1) | 2.76 (0.96–7.92)* | 2.24 (0.21–24.14) | 0.507 | |
| Higher education | 70 (44.0) | 81 (30.7) | 1 | 1 | ||
| Occupation | Farmer | 24 (15.1) | 56 (21.2) | 4.28 (1.42–12.90)* | 6.01 (0.47–76.9) | 0.168 |
| Employed | 58 (36.5) | 72 (27.3) | 2.28 (0.79–6.52)* | 3.83 (0.85–17.23) | 0.080 | |
| Merchant | 43 (27.9) | 95 (36.0) | 3.92 (1.36 – 11.27) * | 5.39 (0.46 – 63.40) | 0.180 | |
| House wife | 23 (14.5) | 35 (13.3) | 2.78 (0.91–8.60)* | 2.58 (0.22–30.9) | 0.453 | |
| Retired | 11 (6.9) | 6 (2.3) | 1 | 1 | ||
| Presence of comorbidities | Present | 18 (11.3) | 134 (50.8) | 8.20 (4.74–14.16)* | 9.19 (4.78–17.69) | <0.001 |
| Absent | 141 (88.7) | 130 (49.2) | 1 | 1 | ||
| Smoking status | Yes | 22 (13.8) | 31 (11.7) | 0.84 (0.47–1.51) | 1.19 (0.57–2.51) | 0.646 |
| No | 137 (86.2) | 233 (88.3) | 1 | 1 | ||
| Alcohol intake | Yes | 42 (26.4) | 121 (45.8) | 2.39 (1.56–3.67)* | 1.66 (0.96–2.85) | 0.069 |
| No | 117 (73.6) | 143 (54.2) | 1 | 1 | ||
| Number of medications | <5 | 119 (74.8) | 129 (48.9) | 1 | 1 | |
| ⩾5 | 40 (25.2) | 135 (51.1) | 2.05 (0.21–4.87)* | 2.84 (1.72–4.70) | 0.001 | |
AOR: adjusted odds ratio; COR: crude odds ratio; CI: confidence interval; N: frequency.
p value < 0.20.
Discussion
The higher incidence of DTPs among T2DM patients with hypertension underlines the need for further efforts to improve medication use, which ultimately increases patient safety. Hence, early DTPs detection is warranted to design a relevant mechanism for the prevention and management of DTPs, which is essential to improve patients’ quality of life.6
In this study, approximately two-thirds of patients (62.4%) experienced one or more DTPs. The magnitude is lower than Niriayo et al.34 (83.5%) and Belayneh et al.35 (75.5%) studies. This higher incidence may be due to the different study participants; Niriayo et al.34 targeted heart failure patients while Belayneh et al.35 conducted among medical ward admitted patients. In addition, the mean number of DTPs was 1.86 ± 0.53 per patient, which is in line with the studies by Ayele et al.36 (1.8), Koyra et al.15 (1.8 ± 0.75), and Huri and Wee14 (1.9 ± 1.2). However, it is considerably higher than the finding conducted by Wong (0.9 ± 0.6),37 Demoz et al.17 (1.16 ± 0.42), Nasution et al.38 (1.34), Shareef et al.39 (1.25), and Kumar et al.40 (1.45). On the contrary, the mean number of DTPs is lower than those studies conducted in Nigeria (2.1 ± 1.4),41 Ethiopia (2.06 ± 0.861),42 and Indonesia (2.88 ± 0.23).16 This disparity may be explained by variability in study design, study participants, DTP’s classification used, and who and how DTPs were identified. The higher proportion of study participants developing DTPs in our study does highlight the need for more attention and close monitoring to these patients.
In this study, non-compliance (197, 40.1%), need additional drug therapy (119, 24.2%), and dose too low (91, 18.5%) were the frequently identified DTPs. This is inconsistent with Belayneh et al.,35 who reported that needs additional drug therapy (35.85%) was the most common DTP followed by unnecessary drug therapy (30.19%) and dosage too low (13.2%). Contrastingly, a Spanish study revealed that non-adherence was the frequently identified DTP.43 In addition, the study by Niriayo et al.34 reported that dosage too low (27.8%), ineffective drug therapy (27.6%), and need additional drug therapy (27.4%) were the frequently occurred DTPs. Furthermore, Al Hamid et al.23 targeted cardiovascular and diabetic patients and found that adverse drug reactions and ineffective drug therapy were commonly identified DTPs. Such discrepancy may be explained by the difference in the study participants, medication used, and the method of DTP classification. Healthcare professionals at FHSCH should be encouraged to use standard treatment guideline.
Similar to the studies by Demoz et al.17 and Mamunuwa et al.,44 metformin, statin, and aspirin were the most common drugs that caused DTPs. Besides, in line with Demoz et al.,17 angiotensin-converting enzyme inhibitors and calcium channel blockers were the frequently prescribed medication classes to manage comorbid hypertension conditions.
The multivariate logistic regression model showed that the presence of DTP was significantly associated with middle-aged patients (45–60 years), lower monthly family income, presence of comorbidity, and a higher number of medications. Middle-aged patients (AOR = 2.55 95% CI: 1.28–5.11, p = 0.008) were more likely associated with DTPs than young adult patients. Conversely, Huri and Wee,14 Kumar et al.,40 and Shareef et al.39 found that elderly patients (>60 years of age) were significantly associated with DTPs. This may be due to the lower percentage of elderly patients in our study. The disparity may also be explained by the variance in life expectancy between nations, which is lower in Ethiopia.
In addition, patients with very low monthly family income (AOR = 4.64, 95% CI: 1.44–14.99, p = 0.010) were five times more likely to experience DTPs than high family income patients. Most patients with low monthly family income were non-compliance (unable to pay for their treatment), which is responsible for a higher percentage of DTPs among this group of patients. It is well known that low socioeconomic status has been substantially associated with lower educational level. Lower literacy level is often related to non-compliance. In addition, the majority of patients in developing countries with chronic diseases have restricted access to health insurance, so medical care is costly and ultimately affects treatment adherence.45
Moreover, participants with comorbidity (AOR = 9.19, 95% CI: 4.78–17.69, p < 0.001) were more likely associated with DTP compared to their counterparts. The currently used guidelines allowed the use of one or more medications in comorbid patients. This may contribute to the existence of potentially inappropriate medication, unwanted drug–drug interactions, and polypharmacy that are associated with the development of DTPs.
Furthermore, patients with five or more medications (AOR = 2.84, 95% CI: 1.72–4.70, p = 0.001) were more likely to experience DTPs than patients taking less than five medications. Our finding is consistent with the studies by Koyra et al.,15 Huri and Wee,14 Bain et al.,46 and Gelchu and Abdela.25 The use of a higher number of drugs, polypharmacy, is often related to drug–drug interactions, adverse drug reactions, and medication-related toxicities. Such practice is a common problem in patients with diabetes and hypertension due to the higher prevalence of comorbidities. Hence, before healthcare professionals prescribe a medication, it is important to review and evaluate the patient’s condition.
Limitations of the study
Our study was a cross-sectional study that did not determine the temporal relationship between DTPs and its associated factors. The research did not address the outcomes of DTPs. Hence, it is advisable to undertake a prospective cohort study to determine predictors of DTPs in this patient population and provide appropriate interventions for the identified DTPs. Besides, there was incomplete data as most of the medication and clinical-related patient information were extracted from patient records.
Conclusion
In this study, approximately three out of five study participants had one or more DTPs with 1.86 DTPs per patient. In addition, non-compliance, needs additional drug therapy, and too low dosage were the most frequently identified DTPs. Forgetfulness, lack of preventive drug therapy, prescription of expensive medications, and use of sub-therapeutic dose were the common causes of compliance-related DTPs. Furthermore, patients in middle age, low monthly family income, presence of comorbidity, and patients taking five or more medications should be closely monitored for the development of DTPs. As DTPs are the common healthcare problem in our setting, patient education regarding medication adherence, routine medication review, and strengthening clinical pharmacy services should be promoted.
Supplemental Material
Supplemental material, Data_collection_tool for Magnitude and determinants of drug therapy problems among type 2 diabetes mellitus patients with hypertension in Ethiopia by Belayneh Kefale, Gobezie T Tegegne, Yitayih Kefale, Mulugeta Molla, Amien Ewunetei and Amsalu Degu in SAGE Open Medicine
Supplemental material, Supplemental_material for Magnitude and determinants of drug therapy problems among type 2 diabetes mellitus patients with hypertension in Ethiopia by Belayneh Kefale, Gobezie T Tegegne, Yitayih Kefale, Mulugeta Molla, Amien Ewunetei and Amsalu Degu in SAGE Open Medicine
Acknowledgments
We would like to acknowledge FHSCH medical ward staffs and data collectors for their valuable contribution toward this project.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from the Ethical Review Board of Debre Tabor University prior to data collection, and subsequent permission was obtained from the FHSCH study site department (Approval Number: 1987/2019).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from all subjects before the study.
ORCID iD: Belayneh Kefale  https://orcid.org/0000-0003-4841-0861
https://orcid.org/0000-0003-4841-0861
Supplemental material: Supplemental material for this article is available online.
References
- 1. Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clin Pract 2019; 157: 107843. [DOI] [PubMed] [Google Scholar]
- 2. Chaurasia B, Summers SA. Ceramides-lipotoxic inducers of metabolic disorders. Trend Endocrinol Metab 2015; 26(10): 538–550. [DOI] [PubMed] [Google Scholar]
- 3. Colosia AD, Palencia R, Khan S. Prevalence of hypertension and obesity in patients with type 2 diabetes mellitus in observational studies: a systematic literature review. Diabetes Metab Syndr Obes 2013; 6: 327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hurst C, Thinkhamrop B. The association between hypertension comorbidity and microvascular complications in type 2 diabetes patients: a nationwide cross-sectional study in Thailand. Diabetes Metab J 2015; 39(5): 395–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lastra G, Syed S, Kurukulasuriya LR, et al. Type 2 diabetes mellitus and hypertension: an update. Endocrinol Metab Clin North Am 2014; 43(1): 103–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cipolle R, Strand L, Frakes M. Co-morbidities and drug therapy problems in patients with diabetes. Medication Management Systems Inc, 2013. [Google Scholar]
- 7. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311(5): 507–520. [DOI] [PubMed] [Google Scholar]
- 8. Hall V, Thomsen RW, Henriksen O, et al. Diabetes in Sub Saharan Africa 1999-2011: epidemiology and public health implications: a systematic review. BMC Public Health 2011; 11(1): 564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Munger MA. Polypharmacy and combination therapy in the management of hypertension in elderly patients with co-morbid diabetes mellitus. Drugs Aging 2010; 27(11): 871–883. [DOI] [PubMed] [Google Scholar]
- 10. Allender S, Peto V, Scarborough P, et al. Coronary heart disease statistics. Birmingham: British Heartbreak Forever, 2007. [Google Scholar]
- 11. Ong KL, Cheung BM, Man YB, et al. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension 2007; 49(1): 69–75. [DOI] [PubMed] [Google Scholar]
- 12. Supina AL, Guirguis LM, Majumdar SR, et al. Treatment gaps for hypertension management in rural Canadian patients with type 2 diabetes mellitus. Clin Ther 2004; 26(4): 598–606. [DOI] [PubMed] [Google Scholar]
- 13. Birarra MK, Heye TB, Shibeshi W. Assessment of drug-related problems in pediatric ward of Zewditu Memorial Referral Hospital, Addis Ababa, Ethiopia. Int J Clin Pharm 2017; 39(5): 1039–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Huri HZ, Wee HF. Drug related problems in type 2 diabetes patients with hypertension: a cross-sectional retrospective study. BMC Endocr Disord 2013; 13(1): 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Koyra HC, Tuka SB, Tufa EG. Epidemiology and predictors of drug therapy problems among type 2 diabetic patients at Wolaita Soddo University teaching hospital, southern Ethiopia. Am J Pharmacol Sci 2017; 5(2): 40–48. [Google Scholar]
- 16. Zazuli Z, Rohaya A, Adnyana IK. Drug-related problems in type 2 diabetic patients with hypertension: a prospective study. J Basic Clin Pharm 2017; 11(2): S298–S304. [Google Scholar]
- 17. Demoz GT, Berha AB, Alebachew Woldu M, et al. Drug therapy problems, medication adherence and treatment satisfaction among diabetic patients on follow-up care at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. PLoS ONE 2019; 14(10): e0222985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gastelurrutia P, Benrimoj SI, Espejo J, et al. Negative clinical outcomes associated with drug-related problems in heart failure (HF) outpatients: impact of a pharmacist in a multidisciplinary HF clinic. J Card Fail 2011; 17(3): 217–223. [DOI] [PubMed] [Google Scholar]
- 19. Kaufmann CP, Stämpfli D, Hersberger KE, et al. Determination of risk factors for drug-related problems: a multidisciplinary triangulation process. BMJ Open 2015; 5(3): e006376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gangwar SS, Monisha N, Nachiya J, et al. Impact of medication and psychological behaviour assessment by community pharmacists in type 2 diabetes mellitus patients after hospital stay. Afr Health Sci 2014; 14(3): 539–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Somers A, Robays H, Vander Stichele R, et al. Contribution of drug related problems to hospital admission in the elderly. J Nutr Health Aging 2010; 14(6): 477–482. [DOI] [PubMed] [Google Scholar]
- 22. Nivya K, Sri Sai Kiran V, Ragoo N, et al. Systemic review on drug related hospital admissions: a PubMed based search. Saudi Pharm J 2015; 23(1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Al Hamid A, Aslanpour Z, Aljadhey H, et al. Hospitalisation resulting from medicine-related problems in adult patients with cardiovascular diseases and diabetes in the United Kingdom and Saudi Arabia. Int J Environ Res Public Health 2016; 13(5): 479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yimama M, Jarso H, Desse TA. Determinants of drug-related problems among ambulatory type 2 diabetes patients with hypertension comorbidity in Southwest Ethiopia: a prospective cross sectional study. BMC Res Notes 2018; 11(1): 679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gelchu T, Abdela J. Drug therapy problems among patients with cardiovascular disease admitted to the medical ward and had a follow-up at the ambulatory clinic of Hiwot Fana Specialized University Hospital: the case of a tertiary hospital in eastern Ethiopia. SAGE Open Med 2019; 7: 860401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench 2013; 6(1): 14. [PMC free article] [PubMed] [Google Scholar]
- 27. Cipolle RJ, Strand LM, Morley PC. Pharmaceutical care practice: the patient-centered approach to medication management. New York: McGraw-Hill, 2012. [Google Scholar]
- 28. Bakris GL, Sowers JR. Treatment of hypertension in patients with diabetes: an update. J Am Soc Hypertens 2009; 3(2): 150–155. [DOI] [PubMed] [Google Scholar]
- 29. American Diabetes Association. Standards of medical care in diabetes-2012. Diabetes Care 2012; 35(Suppl. 1): S11–S63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. FMHACA Ethiopia. Standard treatment guidelines for general hospitals, 2014, pp. 69–76, http://www.fmhaca.gov.et/wp-content/uploads/2019/03/STG-General-Hospital..pdf
- 31. Inzucchi S. Diabetes facts and guidelines, 2010-2011. New Haven, CT: Yale Diabetes Center, 2010. [Google Scholar]
- 32. Lacy CF, Armstrong LL, Goldman MP, et al. Drug information handbook. 20th ed. Hudson, OH: Lexi-Comp, 2011. [Google Scholar]
- 33. American Diabetes Association. Standards of medical care in diabetes: 2017 abridged for primary care providers. Clin Diabetes 2017; 35(1): 5–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Niriayo YL, Kumela K, Kassa TD, et al. Drug therapy problems and contributing factors in the management of heart failure patients in Jimma University Specialized Hospital, Southwest Ethiopia. PLoS ONE 2018; 13(10): e0206120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Belayneh YM, Amberbir G, Agalu A. A prospective observational study of drug therapy problems in medical ward of a referral hospital in northeast Ethiopia. BMC Health Serv Res 2018; 18(1): 808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ayele Y, Melaku K, Dechasa M, et al. Assessment of drug related problems among type 2 diabetes mellitus patients with hypertension in Hiwot Fana Specialized University Hospital, Harar, Eastern Ethiopia. BMC Res Notes 2018; 11(1): 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wong IC. Improving medication safety and diabetes management in Hong Kong: a multi-disciplinary approach. Hong Kong Med J 2017; 23(2): 158–167. [DOI] [PubMed] [Google Scholar]
- 38. Nasution A, Khairunnisa K, Tanjung HR. Drug therapy problems in management of hypertensive outpatients admitted to four Indonesian Primary Health Centers. Asian J Pharm Clin Res 2016; 9: 87–90. [Google Scholar]
- 39. Shareef J, Fernandes J, Samaga L. Assessment of clinical pharmacist interventions in drug therapy in patients with diabetes mellitus in a tertiary care teaching hospital. Diabetes Metab Syndr 2016; 10(2): 82–87. [DOI] [PubMed] [Google Scholar]
- 40. Kumar S, Dahal P, Venkataraman R, et al. Assessment of clinical pharmacist intervention in tertiary care teaching hospital of Southern India. Asian J Pharm Clin Res 2013; 6(Suppl. 2): 258–261. [Google Scholar]
- 41. Ogbonna BO, Ezenduka CC, Opara CA, et al. Drug therapy problems in patients with type-2 diabetes in a tertiary hospital in Nigeria. Int J Innov Res Dev 2014; 3(1): 494–502. [Google Scholar]
- 42. Argaw AM, Hiwet TT, Derse BB. Drug therapy problems and determinants among ambulatory type 2 diabetes mellitus patients: pharmacists’ intervention in south-east Ethiopia. Endocrinol Metab Syndr 2019; 8(303): 2161–1017. [Google Scholar]
- 43. Juste AM, Miguel AG, Plou BP, et al. Adherence to treatment of hypertension, hypercholesterolaemia and diabetes in an elderly population of a Spanish cohort. Med Clin 2019; 153(1): 1–5. [DOI] [PubMed] [Google Scholar]
- 44. Mamunuwa N, Jayamanne S, Coombes J, et al. Drug related problems among patients with diabetes; a descriptive analysis of data from an urban hospital in Sri Lanka, 2016, http://repository.kln.ac.lk/handle/123456789/16176
- 45. Salini A, Sajeeth C. Prevalence, risk factors, adherence and non adherence in patient with chronic kidney disease: a prospective study. IJRPC 2013; 3(2): 2231–2781. [Google Scholar]
- 46. Bain KT, Weschules DJ, Tillotson P. Prevalence and predictors of medication-related problems. Pharmacotherapy 2006; 1: 14–26. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Data_collection_tool for Magnitude and determinants of drug therapy problems among type 2 diabetes mellitus patients with hypertension in Ethiopia by Belayneh Kefale, Gobezie T Tegegne, Yitayih Kefale, Mulugeta Molla, Amien Ewunetei and Amsalu Degu in SAGE Open Medicine
Supplemental material, Supplemental_material for Magnitude and determinants of drug therapy problems among type 2 diabetes mellitus patients with hypertension in Ethiopia by Belayneh Kefale, Gobezie T Tegegne, Yitayih Kefale, Mulugeta Molla, Amien Ewunetei and Amsalu Degu in SAGE Open Medicine


