Abstract
Clavicle injuries are common in ice hockey, and a number of high-profile fractures and dislocations have occurred in elite hockey players in recent years. Acromioclavicular joint injuries, clavicle fractures, and sternoclavicular joint injuries are some of the most frequent hockey-related injuries treated by orthopaedic surgeons, and familiarity with the management of these injuries and sport-specific considerations for treatment and recovery are critical. Injuries involving the clavicle can sometimes be life-threatening, and subtle findings on physical examination and radiographic studies can have profound implications for treatment. The recent literature pertinent to the diagnosis and treatment of clavicle-related injuries in ice hockey players was reviewed and compiled into a clinical commentary. For ice hockey players, the upper extremity was traditionally considered a relatively well-protected area. However, given the evolution of the game and its protective equipment, the upper extremity now accounts for the majority of youth ice hockey injuries, of which clavicle injuries comprise a significant proportion. Acromioclavicular joint injuries are the most common injury in this population, followed closely by clavicle fractures. Sternoclavicular joint injuries are rare but can be associated with serious complications. The treatment of these injuries often differs between athletes and the general population, and surgical indications continue to evolve in both groups. Although the evidence regarding clavicle injuries is ever-increasing and the treatment of these injuries remains controversial, clavicle injuries are increasingly common in ice hockey players. Rule and equipment changes, most notably the increased use of flexible boards and glass, have been shown to significantly decrease the risk of clavicle injuries. We also recommend compulsory use of shoulder pads, even at a recreational level, as well as continued enforcement and evolution of rules aimed at reducing the rate of clavicle injuries. Future research should focus on equipment design changes directed toward clavicle injury prevention, standardized return-to-play protocols, and studies weighing the risks and benefits of nonoperative management of controversial injuries, such as type III acromioclavicular joint dislocations and diaphyseal clavicle fractures.
Keywords: shoulder, ice hockey, clavicle, acromioclavicular, sternoclavicular
Ice hockey is a popular, fast-paced contact sport played throughout the world. Considered to be one of the fastest and most aggressive sports, ice hockey is a unique team sport that requires strength, agility, balance, skill, and aggression. Playing on a solid ice surface surrounded by rigid composite boards, players move on sharp skates at speeds reaching up to 48 km/h.28 Sticks made of aluminum or composite material are used to shoot a vulcanized rubber puck on the opposing goal with speeds reaching up to 100 mph.13 Male players are allowed to body-check opposing players in order to separate them from the puck; although women’s ice hockey prohibits body-checking, bodily contact is still a part of the game. Given the high speed and physicality of the game, ice hockey players are predisposed to a variety of injuries.5,8,18,27,36
The combination of open-ice checking, board collisions, and use of hockey sticks has been postulated to account for the high incidence of upper extremity injuries in hockey.28 For ice hockey players, the upper extremity was traditionally considered a well-protected area. However, given the evolution of the game and of its protective equipment, upper extremity injuries are now among the most common injuries sustained by ice hockey players, and injury rates have increased over the past several years.25,29 In a study evaluating the incidence of injuries at the World Junior Ice Hockey Championships between 2006 and 2015, the shoulder was the most common location for an upper body injury, with acromioclavicular (AC) joint sprains accounting for 59% of those injuries.37 The ice hockey community has historically been effective at driving reductions in injury rates by changing the rules governing equipment, rink construction, and gameplay, most notably in the areas of head, face, and cervical spine injuries.8 Clavicle injuries, however, have not yet received the same level of attention despite their high incidence.
Clavicle injuries are common in high-impact sports like ice hockey and can include AC joint sprains, clavicle fractures, and sternoclavicular (SC) joint injuries (Figure 1). The high speeds involved in ice hockey and the need for flexible shoulder pads that balance safety for the wearer and other players contribute to a high incidence of clavicle injuries. The purpose of this review article was to summarize the latest research and review the current concepts in the treatment of clavicle injuries in ice hockey players.
Figure 1.
Overview of clavicle anatomy and classification systems by area of injury. AC, acromioclavicular; CC, coracoclavicular; Lig, ligament; SC, sternoclavicular.
Acromioclavicular Joint
The AC joint is the most commonly injured shoulder structure in ice hockey players, and AC joint sprains or dislocations are the common shoulder injuries in National Collegiate Athletic Association ice hockey players.25 The mechanism of injury is typically by direct contact of the shoulder with another player or an apparatus, such as the boards or glass surrounding the ice surface, which drives the acromion inferiorly, causing a sprain or tear in the AC and/or coracoclavicular (CC) ligaments. AC joint injuries are categorized according to the Rockwood classification (Table 1), which helps guide management of these injuries.
TABLE 1.
Rockwood Classification and Management for AC Joint Injuriesa
| Type | Ligament | Physical Examination | Radiographic Findings | Treatment |
|---|---|---|---|---|
| I | AC sprain CC normal |
AC joint tenderness; no instability | Normal | Nonoperative |
| II | AC torn CC sprain |
AC joint horizontal instability, reducible | AC joint disruption; CC distance <25% contralateral | Nonoperative |
| III | AC torn CC torn |
Prominent distal clavicle, reducible | CC distance 25%-100% contralateral | Controversial |
| IV | AC torn CC torn |
Skin tenting, posterior fullness, irreducible | Lateral clavicle displaced posterior through trapezius (visible on axillary radiograph) | Operative |
| V | AC torn CC torn |
Shoulder droop; no improvement with shrug, irreducible | Increased CC distance >100% contralateral | Generally operative |
| VI | AC torn CC torn |
Rare; irreducible; other associated injuries; paresthesias | Inferior dislocation of lateral clavicle either in subacromial or subcoracoid position underneath conjoint tendon | Operative |
aAC, acromioclavicular; CC, coracoclavicular.
Patients often present with swelling, limited range of motion, and tenderness or localized pain at the joint. Physical examination is typically notable for a tender, prominent bump representing the distal end of the clavicle, which is caused by the weight of the arm and shoulder girdle bringing the acromion down while the clavicle remains in place due to the pull of the sternocleidomastoid and trapezius muscles. It is important to recognize any threat to skin caused by the injury (usually with type III or V injuries) or, in rare cases, neurovascular compromise. Type IV injuries may present with deformity caused by posterior displacement of the clavicle.
Initial radiographic workup should include anteroposterior (AP), scapular-Y, and axillary radiographs.28 Views including both AC joints are often helpful in assessing the degree of displacement, which affects classification and management of the injuries. Weighted views are unnecessary and may exacerbate pain in acutely injured players without a clear benefit in terms of diagnosis.28
Initial management of AC joint injuries involves cryotherapy, rest, activity modification, and use of a sling for comfort.13,32 Type I and II injuries can be managed definitively with rest, cryotherapy, strengthening, and progressive range of motion exercises. Anesthetic injections into the AC joint can be helpful for pain management. Ideal treatment of type III injuries remains controversial in sports medicine. Although the majority of patients can be managed nonoperatively with use of a sling and early progressive motion, some surgeons prefer operative management for younger, active, overhead athletes (in the absence of level 1 evidence to support operative intervention).39 However, type III AC joint injuries may successfully be managed nonoperatively in ice hockey players, according to levels 4 and 5 evidence.18,39 Further complicating decisions about treatment of type III AC joint injuries is the increasing focus on the effect of AP stability of the AC joint—assessed on imaging modalities, such as a cross-body adduction radiograph. This has led some to advocate for the subdivision of these injuries into IIIA (stable) and IIIB (unstable) injuries, which could potentially guide the indications for operative management.38 Return to play after type I, II, or III injuries is predicated upon the return of full range of motion, normal strength, and minimal discomfort. Type IV, V, and VI injuries usually require surgical intervention; however, even high-level players can be treated nonoperatively with success.28
A variety of acute repair and reconstruction options have been described. In addition to the operative indications based on the Rockwood classification of injury, operative management has also been recommended when considering management of players who exhibit scapular maltracking early in the rehabilitation process.2 Surgical treatment of AC joint injuries should be approached cautiously because of the complication profile of operative intervention. Carofino and Mazzocca4 described a widely adopted anatomic double-tunnel CC ligament reconstruction; however, there are concerns that the holes can serve as stress risers and lead to fracture for contact athletes.28 Delayed fracture after return to sports has been reported and is directly attributable to the operative intervention (Figure 2).21 To counteract this risk, some authors have recommended a nonanatomic technique that is performed by drilling 1 hole in order to minimize the risk of refracture at the expense of mild anteriorization of the clavicle; however, there remains no consensus at this time in terms of the optimal surgical treatment for AC joints.
Figure 2.
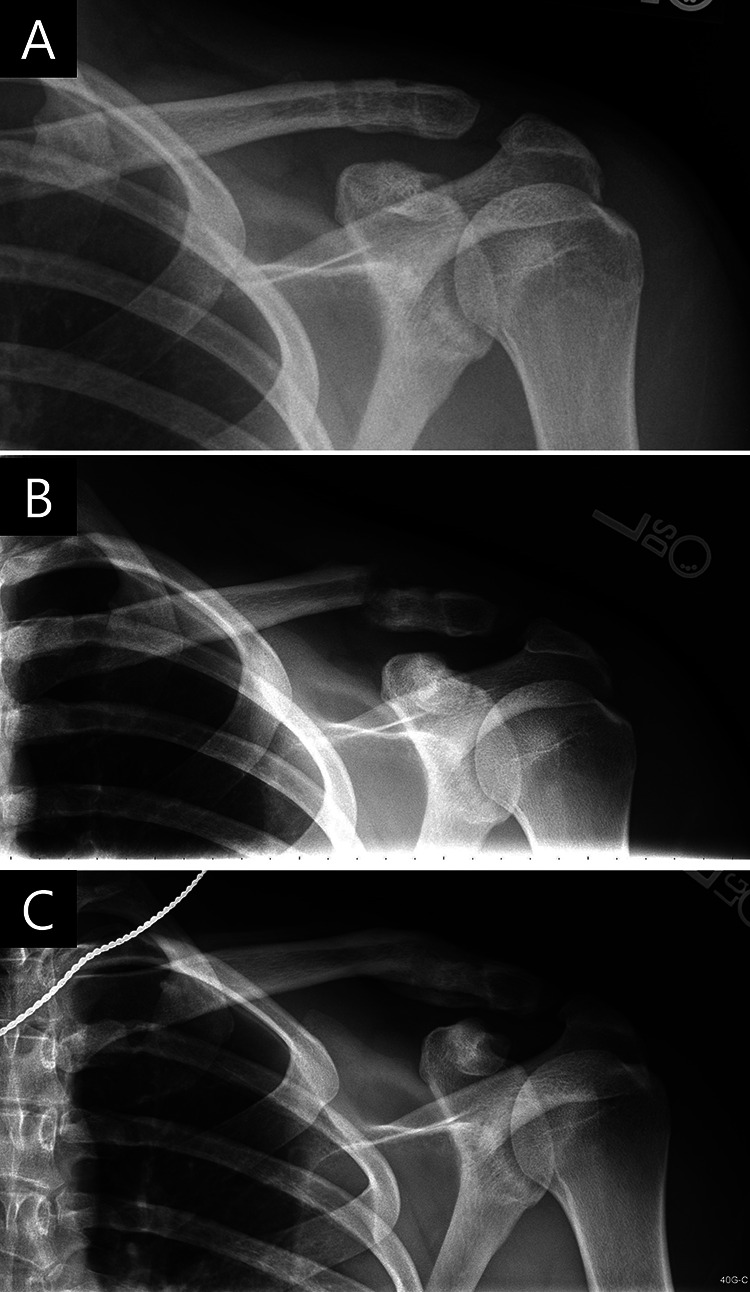
(A) Rockwood type III acromioclavicular (AC) joint injury in an ice hockey player treated with AC ligament reconstruction. (B) After sufficient postoperative recovery and graduated return to play, the same player reported shoulder pain after a separate incident just over 1 year after surgical intervention, resulting from a collision into the boards. A distal clavicle fracture about one of the bone tunnels from the reconstruction is demonstrated. A decision was made for nonoperative management. (C) At 1 year after injury, the player had successful return to play. Images courtesy of Gregory Lervick, MD (Minneapolis, Minnesota).
Studies have reported a mean of 5 practices missed and approximately 2.5 games missed for male collegiate hockey players who sustained AC joint injuries.8 Players often return to play a few days to 2 weeks after a Rockwood type I injury, 2 to 3 weeks after type II injuries, and up to 6 to 12 weeks after type III injuries.28 Players with injuries of types III through VI that need surgery can require up to 6 months to return to play because of concern for fracture through the drill holes used for the AC joint reconstructions.
Some special considerations for AC joint injuries are specific to the sport of ice hockey itself. AC joint-padded Sully braces can sometimes be helpful for symptom management in these injuries during the return to play phase. Taping and extra padding to the area underneath the shoulder pads may also improve comfort for athletes by dissipating contact forces and acting as a form of preemptive pain management18 (Figure 3).
Figure 3.

Athletic taping of acromioclavicular joint injury in youth ice hockey player.
Custom tailoring of shoulder pads may be necessary to minimize discomfort caused by AC joint separations and/or allow for braces to be used effectively. As with all injuries in a contact sport, such as hockey, AC joint separation should be managed using a graduated return to play that slowly reintroduces drills involving checking in a practice setting before return to game play.
Clavicle Fracture
Clavicle fracture, another common ice hockey injury,12,18 has received increased attention recently in the media because of a number of high-profile ice hockey players sustaining this injury. Studies have shown that clavicle fractures proportionally occur most often in individuals aged 15 to 19 years.26 McCarthy et al22 found that among US high school athletes from 2008 to 2017, boys’ ice hockey players had the highest incidence of clavicle fractures, followed by lacrosse, football, and wrestling athletes. As the singular bone connecting the axial and appendicular skeletons in the upper extremity, the clavicle is at high risk of fracture from direct falls onto the shoulder, as well as from direct impact to the clavicle, which can occur by direct body contact with another hockey player or impact with the boards or ice.
Patients will often present with pain, deformity, and—in severe cases—skin tenting over the clavicle. Physical examination should include a thorough neurovascular examination and particular attention to the status of the skin overlying the fracture.
Initial imaging workup should include an AP view of the clavicle, as well as a 45° cephalad view, which eliminates overshadowing from the ribs.28 Clavicle fractures with potential involvement of either the AC or the SC joints may merit a computed tomography (CT) scan to assess for intra-articular extension.
The classification of clavicle fractures is complex and is determined first by the location of the fracture within the clavicle (group I, midshaft; group II, distal third; group III, proximal third) per the Allman and Neer classification.14 Group I (midshaft) fractures are the most common and account for 80% of clavicle fractures. These may be further subdivided into nondisplaced (<100% displacement) and displaced fractures, although the indications for surgical treatment of these fractures remain controversial. Group II (distal-third) clavicle fractures are subdivided in greater detail per the Neer classification (Table 2) because nuances about the location of the fracture with respect to the CC ligaments have significant influence on union rates and operative indications. Clinical studies have demonstrated rates of nonunion >20% in association with nonoperative management of type IIA and IIB distal clavicle fractures, although the ultimate clinical outcome in a distal clavicle nonunion may be acceptable for certain patient populations. The high rate of nonunion is attributable to the fact that in type II fractures, the CC ligaments are no longer connected to the diaphysis of the clavicle due to either the location of the fracture medial to the ligaments (type IIA) or the conoid ligament itself being torn (type IIB). As a result, typical fracture fixation is insufficient for these types of fractures, and the vast majority of surgeons use adjuncts—such as hook plates, locking plates, cerclage wires, tension bands, or suture anchors—of which no single gold standard treatment has been identified in meta-analyses.33 Group III (proximal-third) fractures are rare, representing <5% of clavicle fractures.
TABLE 2.
Neer Classification of Distal-Third Clavicle Fractures
| Type | Location | Status of Coracoclavicular Ligaments | Prognosis/Treatment |
|---|---|---|---|
| I | Lateral to coracoclavicular ligaments | Conoid and trapezoid intact | Typically nonoperative |
| IIA | Medial to coracoclavicular ligaments | Conoid and trapezoid intact | Typically operative because of high rates of nonunion with nonoperative management |
| IIB | Between coracoclavicular ligaments | Conoid torn, trapezoid intact (or both torn) | Typically operative because of high rates of nonunion with nonoperative management |
| III | Intra-articular involving acromioclavicular joint | Conoid and trapezoid intact | Typically nonoperative but may develop posttraumatic acromioclavicular arthritis over time |
| IV | Physeal fracture/periosteal sleeve avulsion in skeletally immature | Conoid and trapezoid intact | Typically nonoperative |
| V | Comminuted | Conoid and trapezoid intact but attached to a fragment separate from rest of clavicle | Typically operative |
It is generally recommended that when a clavicle fracture is treated nonoperatively, athletes have up to 6 weeks of noncontact activities, with return to skating and introduction of contact taking up to 8 to 12 weeks or when full motion and strength is regained, assuming evidence of healing on radiographs.18,21,31 Studies have reported that high-level athletes may safely return to at high-risk sports sooner than can the average nonathlete patient after surgical treatment.10,30 In a study of National Hockey League hockey players with clavicle fractures, 10 patients underwent surgery and returned to the ice in 65 days compared with 5 patients who were treated nonoperatively and returned to play at 97 days.10 The authors reported 1 refracture in the nonoperative group that ultimately required surgery to heal.
The evidence surrounding operative management of clavicle fractures in the general population has seen a number of evolutions over the past few decades. The most recent evidence demonstrates a benefit in terms of reduced nonunion rate when displaced midshaft clavicle fractures are treated surgically, but this benefit comes with a considerable rate of postoperative complications and reoperations.9 Furthermore, many midshaft clavicle fracture nonunions remain asymptomatic, even in high-level athletes.9 Similarly, the indications for operative management of clavicle fractures in collision athletes are controversial, but outcomes are generally favorable in this population (Table 3).
TABLE 3.
Current Evidence Regarding Operative Treatment of Midshaft Clavicle Fractures in Collision Athletesa
| Lead Author (Year) | Level of Evidence | Inclusion Criteria | Management | Average Time to RTS |
|---|---|---|---|---|
| Hebert-Davies10 (2018) | 3: retrospective cohort | NHL players with clavicle fracture treated operatively vs nonoperatively | 10 operative, 5 nonoperative | 65 d operative, 97.6 d nonoperative |
| Jack15 (2017) | 4: retrospective case series | NFL players treated with operative management of clavicle fracture | 16 players operative fixation | 94.1% RTS at mean of 211.3 d postoperatively |
| Jack16 (2017) | 4: retrospective case series | NFL players treated with nonoperative management of clavicle fracture | 30 players nonoperative | 96.9% RTS at mean of 244.6 d (1-y survival rate after treatment, 93.5%) |
| Ranalletta30 (2015) | 4: retrospective case series | Closed type IIB fracture; within 3 wk from injury; aged 16-60 y; intention to RTS postoperatively | Plate fixation | 94% RTS at mean of 68 d (for athletes participating in high-impact/collision sports) |
| Meisterling24 (2013) | 4: retrospective case series | Displaced midshaft clavicle fracture treated with plate fixation; intention to RTS postoperatively | Plate fixation | 83 d; 84 d RTS football 23% RTS ≤6 wk postoperatively 67% RTS ≤12 wk |
| Lindeman20 (2019) | 4: retrospective case series | 90 patients aged 13-22 y; athletes treated with locking plate ORIF of clavicle fracture | Plate fixation | 100% of patients in athlete group who desired to RTS did so within 2 mo postoperatively |
aNFL, National Football League; NHL, National Hockey League; ORIF, open reduction internal fixation; RTS, return to sports.
Special sport-specific considerations for clavicle fractures in ice hockey players are similar to those for AC joint injuries with respect to extra padding and/or bracing. In general, the physician should note the player’s preferred shooting side in making decisions about return to play. Most of the motion associated with shooting the puck—including abduction and external rotation—occurs with the shooting-side shoulder (ie, skaters who shoot from their right side will incur more motion on their right shoulder). Thus, a right-shooting player with a history of previous right-side clavicle or shoulder injury may have more pain than a player with a left-sided injury.
Sternoclavicular Joint
Injuries to the SC joint are much less frequent than are other shoulder injuries in contact sport athletes, accounting for 3% of all shoulder injuries and <1% of all dislocations throughout the body.11 Although the clavicle is the first bone to ossify, the medial clavicular physis does not completely fuse until approximately 25 years of age. Although true SC joint dislocations have been reported in hockey players, SC joint injuries are much more frequently found to be fractures involving the medial clavicle physis, given the weak connection near the SC junction.19 Considering the delayed closure of the medial clavicle physis, all athletes younger than 25 years carry a risk for this injury.28 Injuries to the SC joint in skeletally immature athletes should thus be treated as growth plate injuries until proven otherwise by imaging.35
The most common mechanism of injury is direct impact to the shoulder with an anteriorly or posteriorly directed force. The patient will often feel a “pop” at the time of impact, followed by pain, swelling, and tenderness in the SC joint region.
On physical examination, a bony prominence may be present over the SC joint in the setting of anterior dislocation. Posterior dislocations may present with an indentation and require a thorough evaluation in the operating room to assess for signs of impingement of vital posterior structures, with a cardiothoracic surgeon available to treat vital structures if needed.28 SC joint dislocations should always be part of the differential diagnosis when one is evaluating an athlete after direct shoulder impact; if an SC joint dislocation is missed, potentially fatal outcomes can occur secondary to damage of underlying mediastinal structures directly behind the medial clavicle.13,23,34 SC joint dislocations can also mimic other conditions that occur in athletes, such as pneumothorax, bronchospasm, chest wall injury, clavicle fractures, first rib synchondrosis injuries, and physeal stress fractures.11
The initial workup of SC joint injuries should include an AP chest radiograph to rule out other causes of focal pain and to evaluate thoracic structures. A serendipity view, where the imaging beam is pointed 40° cephalad, can help determine superior or inferior displacement of the clavicle; however, subtle subluxations can still be missed on radiographs.6,34 Axial CT remains the most definitive modality to evaluate SC joint position and compression of mediastinal structures and can also be used to identify subtle medial one-third clavicular fractures that may present similarly to SC joint dislocations. Diagnostic ultrasonography is an emerging modality that can provide a rapid and dynamic view of the SC joint, as well as confirmation of reduction after injury.6 If there is concern for vascular injury or impingement, intravenous contrast studies should be obtained. Magnetic resonance imaging can be considered in lieu of CT when one is evaluating a suspected physeal injury in pediatric ice hockey players.1
Nonoperative treatment without reduction for anterior SC joint dislocations in athletes younger than 25 years can provide excellent outcomes because physeal remodeling is sufficient to heal these injuries without intervention.17 Athletes with acute posterior SC joint injuries should be taken to the operating room for closed reduction (with possible open reduction in cases of intrathoracic injury, failed closed reduction, or symptomatic AP instability), with a cardiothoracic surgeon available to treat vital structures if needed.34
No standardized guidelines are available for return to sports after recovery from a posterior SC joint dislocation. Our recommendation is for the athlete to wear a sling for 4 to 6 weeks if the injury was treated via an open reduction. The hockey player should undergo at least 6 weeks of physical therapy after the sling is removed before making a return to full contact. We allow for skating on the ice with no contact as early as 8 weeks after injury. The goal is to return to full play around 12 weeks at the earliest.
Conclusions and Future Implications
Any physician caring for ice hockey players must be familiar with injuries involving the clavicle. For ice hockey players, the upper extremity is traditionally considered a well-protected area; however, the upper extremity remains highly vulnerable to injury in ice hockey players and accounts for the highest percentage (44%) of youth ice hockey injuries.12 Within the upper extremity, the shoulder is the most common area injured, with partial or complete AC joint sprains comprising the majority of injuries in ice hockey players. Clavicle fractures follow closely behind AC joint injuries in terms of incidence, and an increasing number of studies have examined the management of clavicle fractures in collision athletes.7,9,10,30,31 SC joint injuries, although less frequent than both AC joint and clavicle injuries, are the most critical injuries to recognize and treat safely in this population.
A thorough physical examination involving inspection and palpation of the entire clavicle is warranted, and the radiographic workup of these injuries can be quite complex. The treatment of choice for injuries about the clavicle is highly dependent on the complex classifications presented in this review, as well as on clinical judgment, consideration of timing of the injury with respect to the hockey season, and the player’s future career choices.
As for specific recommendations for rule and equipment changes that may help prevent clavicle injuries, the following have either been proposed or enacted by leagues around the world:
Flexible boards and glass (ie, avoiding seamless glass) with rounded corners36: It is noteworthy that shoulder injuries are disproportionately caused by contact with the boards when compared with injuries to other body parts (59%-63% in 1 study,36 as opposed to 24%-36% for injuries in general).37 Studies have demonstrated a statistically significant reduction in the shoulder injury rate associated with the use of flexible boards and glass (0.9/1000 player-games vs 2.2/1000 player-games with traditional boards).36
Shoulder protection: We recommend mandated shoulder protection—even at a recreational level, where some adults choose to forgo shoulder pads—because of research identifying lack of protective equipment as a major risk factor for injuries.3
Rules enforcement: Enforcement of existing rules designed to prevent dangerous plays should be improved, similar to how rules limiting checking from behind and hits targeting the head have been changed and/or reemphasized at the collegiate and professional levels in recent years.8
The above recommendations must be balanced with considerations regarding athlete performance and marketability of the game, especially at the professional level.
Future areas of study in this realm should focus on equipment modifications to be made to shoulder pads in ice hockey to minimize the incidence of injuries to the AC joint, clavicle, and SC joint. Return to play and rehabilitation guidelines should be further studied and standardized for return to the ice. It has previously been reported that of all sports-related fractures, clavicle fractures have the third longest timeframe for return to sports and as many as 20% of athletes are unable to return to sports.31 Finally, the indications for operative management of midshaft clavicle fractures have evolved significantly in recent years, as results are suggesting faster return to play when compared with nonoperative treatment in an athletic population. This warrants future study and discussion, particularly for nonprofessional athletes. Further studies examining functional and radiographic outcomes, as well as more detailed return to play studies, would be helpful in guiding the treatment of injuries involving the clavicle in ice hockey.
Hockey is a high-intensity, fast-growing sport that can cause upper extremity injuries involving the entire clavicle from the AC joint to the SC joint. Injuries involving the clavicle have had significant effects on high-profile players, and injuries in this area can sometimes be life-threatening. Because subtle findings on physical examination and radiographic studies can have profound implications for treatment—and ultimately, functional outcome of the athlete—physicians treating these athletes should maintain up-to-date knowledge about the current concepts in diagnosing and treating these injuries.
Footnotes
Final revision submitted March 20, 2020; accepted April 6, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: W.N.L. has received hospitality payments from Zimmer Biomet. C.A.P. is a team physician for USA Hockey and has received educational and research support from Arthrex and hospitality payments from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Beckmann N, Crawford L. Posterior sternoclavicular Salter-Harris fracture-dislocation in a patient with unossified medial clavicle epiphysis. Skeletal Radiol. 2016;45(8):1123–1127. [DOI] [PubMed] [Google Scholar]
- 2. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology, part III: the SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19(6):641–661. [DOI] [PubMed] [Google Scholar]
- 3. Caputo P, Mattson DJ. Recreational ice hockey injuries in adult non-checking leagues: a United States perspective. J Sports Sci Med. 2005;4(1):58–65. [PMC free article] [PubMed] [Google Scholar]
- 4. Carofino BC, Mazzocca AD. The anatomic coracoclavicular ligament reconstruction: surgical technique and indications. J Shoulder Elbow Surg. 2010;19(2)(suppl):37–46. [DOI] [PubMed] [Google Scholar]
- 5. Crowley SG, Trofa DP, Vosseller JT, et al. Epidemiology of foot and ankle injuries in National Collegiate Athletic Association men’s and women’s ice hockey. Orthop J Sports Med. 2019;7(8):2325967119865908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ernberg LA, Potter HG. Radiographic evaluation of the acromioclavicular and sternoclavicular joints. Clin Sports Med. 2003;22(2):255–275. [DOI] [PubMed] [Google Scholar]
- 7. Fanter NJ, Kenny RM, Baker CL III, Baker CL., Jr Surgical treatment of clavicle fractures in the adolescent athlete. Sports Health. 2015;7(2):137–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Flik K, Lyman S, Marx RG. American collegiate men’s ice hockey: an analysis of injuries. Am J Sports Med. 2005;33(2):183–187. [DOI] [PubMed] [Google Scholar]
- 9. Guerra E, Previtali D, Tamborini S, Filardo G, Zaffagnini S, Candrian C. Midshaft clavicle fractures: surgery provides better results as compared with nonoperative treatment: a meta-analysis. Am J Sports Med. 2019;47(14):3541–3551. [DOI] [PubMed] [Google Scholar]
- 10. Hebert-Davies J, Agel J. Return to elite-level sport after clavicle fractures. BMJ Open Sport Exerc Med. 2018;4(1):e000371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hellwinkel JE, McCarty EC, Khodaee M. Sports-related sternoclavicular joint injuries. Phys Sportsmed. 2019;47(3):253–261. [DOI] [PubMed] [Google Scholar]
- 12. Hostetler SG, Xiang H, Smith GA. Characteristics of ice hockey-related injuries treated in US emergency departments, 2001-2002. Pediatrics. 2004;114(6):e661–e666. [DOI] [PubMed] [Google Scholar]
- 13. Irvine JN, Jr, Lynch S, Hanypsiak BT, Popkin CA. Lower extremity injuries in ice hockey: current concepts. Am J Orthop (Belle Mead NJ). 2018;47(11):1–17. [DOI] [PubMed] [Google Scholar]
- 14. Holder J, Kolla S, Lehto S. Clavicle fractures: Allman and Neer classification. J Adv Radiol Med Image. 2017;2(1):1–11. [Google Scholar]
- 15. Jack RA II, Sochacki KR, Navarro SM, McCulloch PC, Lintner DM, Harris JD. Performance and return to sport after clavicle open reduction and internal fixation in National Football League players. Orthop J Sports Med. 2017;5(8):2325967117720677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jack RA II, Sochacki KR, Navarro SM, McCulloch PC, Lintner DM, Harris JD. Performance and return to sport after nonoperative treatment of clavicle fractures in National Football League players. Orthopedics. 2017;40(5):e836–e843. [DOI] [PubMed] [Google Scholar]
- 17. Jaggard MK, Gupte CM, Gulati V, Reilly P. A comprehensive review of trauma and disruption to the sternoclavicular joint with the proposal of a new classification system. J Trauma. 2009;66(2):576–584. [DOI] [PubMed] [Google Scholar]
- 18. Laprade RF, Surowiec RK, Sochanska AN, et al. Epidemiology, identification, treatment and return to play of musculoskeletal-based ice hockey injuries. Br J Sports Med. 2014;48(1):4–10. [DOI] [PubMed] [Google Scholar]
- 19. Lee JT, Nasreddine AY, Black EM, Bae DS, Kocher MS. Posterior sternoclavicular joint injuries in skeletally immature patients. J Pediatr Orthop. 2014;34(4):369–375. [DOI] [PubMed] [Google Scholar]
- 20. Lindeman RW, Lanier BS, Parsell DE, Ramsey JR. Clinical outcomes for open reduction internal fixation of midshaft clavicle fractures in adolescent/post-adolescent athletes utilizing a two month return to play protocol. Orthop J Sports Med. 2019;7(7)(suppl 5):2325967119S00381. [Google Scholar]
- 21. Martetschläger F, Gaskill TR, Millett PJ. Management of clavicle nonunion and malunion. J Shoulder Elbow Surg. 2013;22(6):862–868. [DOI] [PubMed] [Google Scholar]
- 22. McCarthy MM, Bihl JH, Frank RM, Salem HS, McCarty EC, Comstock RD. Epidemiology of clavicle fractures among US high school athletes, 2008-2009 through 2016-2017. Orthop J Sports Med. 2019;7(7):2325967119861812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McClaskey D, Dartt C. Triple deked by a negative X-ray. Clin J Sport Med. 2016;26(4):e99. [Google Scholar]
- 24. Meisterling SW, Cain EL, Fleisig GS, Hartzell JL, Dugas JR. Return to athletic activity after plate fixation of displaced midshaft clavicle fractures. Am J Sports Med. 2013;41(11):2632–2636. [DOI] [PubMed] [Google Scholar]
- 25. Melvin PR, Souza S, Mead RN, Smith C, Mulcahey MK. Epidemiology of upper extremity injuries in NCAA men’s and women’s ice hockey. Am J Sports Med. 2018;46(10):2521–2529. [DOI] [PubMed] [Google Scholar]
- 26. Mölsä J, Kujala U, Myllynen P, Torstila I, Airaksinen O. Injuries to the upper extremity in ice hockey: analysis of a series of 760 injuries. Am J Sports Med. 2003;31(5):751–757. [DOI] [PubMed] [Google Scholar]
- 27. Mosenthal W, Kim M, Holzshu R, Hanypsiak B, Athiviraham A. Common ice hockey injuries and treatment: a current concepts review. Curr Sports Med Rep. 2017;16(5):357–362. [DOI] [PubMed] [Google Scholar]
- 28. Popkin CA, Nelson BJ, Park CN, et al. Head, neck, and shoulder injuries in ice hockey: current concepts. Am J Orthop (Belle Mead NJ). 2017;46(3):123–134. [PubMed] [Google Scholar]
- 29. Popkin CA, Schulz BM, Park CN, Bottiglieri TS, Lynch TS. Evaluation, management and prevention of lower extremity youth ice hockey injuries. Open Access J Sports Med. 2016;7:167–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ranalletta M, Rossi LA, Piuzzi NS, Bertona A, Bongiovanni SL, Maignon G. Return to sports after plate fixation of displaced midshaft clavicular fractures in athletes. Am J Sports Med. 2015;43(3):565–569. [DOI] [PubMed] [Google Scholar]
- 31. Robertson GA, Wood AM. Return to sport following clavicle fractures: a systematic review. Br Med Bull. 2016;119(1):111–128. [DOI] [PubMed] [Google Scholar]
- 32. Simovitch R, Sanders B, Ozbaydar M, Lavery K, Warner JJ. Acromioclavicular joint injuries: diagnosis and management. J Am Acad Orthop Surg. 2009;17(4):207–219. [DOI] [PubMed] [Google Scholar]
- 33. Stegeman SA, Nacak H, Huvenaars KH, Stijnen T, Krijnen P, Schipper IB. Surgical treatment of Neer type-II fractures of the distal clavicle: a meta-analysis. Acta Orthop. 2013;84(2):184–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Thomas DP, Davies A, Hoddinott HC. Posterior sternoclavicular dislocations—a diagnosis easily missed. Ann R Coll Surg Engl. 1999;81(3):201–204. [PMC free article] [PubMed] [Google Scholar]
- 35. Tompkins M, Bliss J, Villarreal R, Solga P. Posterior sternoclavicular disruption with ipsilateral clavicle fracture in a nine-year-old hockey player. J Orthop Trauma. 2010;24(4):e36–e39. [DOI] [PubMed] [Google Scholar]
- 36. Tuominen M, Stuart MJ, Aubry M, Kannus P, Parkkari J. Injuries in men’s international ice hockey: a 7-year study of the International Ice Hockey Federation Adult World Championship Tournaments and Olympic Winter Games. Br J Sports Med. 2015;49(1):30–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tuominen M, Stuart MJ, Aubry M, Kannus P, Parkkari J. Injuries in world junior ice hockey championships between 2006 and 2015. Br J Sports Med. 2017;51(1):36–43. [DOI] [PubMed] [Google Scholar]
- 38. Upper Extremity Committee of ISAKOS. ISAKOS upper extremity committee consensus statement on the need for diversification of the Rockwood classification for acromioclavicular joint injuries. Arthroscopy. 2014;30(2):271–278. [DOI] [PubMed] [Google Scholar]
- 39. Willimon SC, Gaskill TR, Millett PJ. Acromioclavicular joint injuries: anatomy, diagnosis, and treatment. Phys Sportsmed. 2011;39(1):116–122. [DOI] [PubMed] [Google Scholar]



