Abstract
Background:
Symptom management for infants, children and young people at end of life is complex and challenging due to the range of conditions and differing care needs of individuals of different ages. A greater understanding of these challenges could inform the development of effective interventions.
Aim:
To investigate the barriers and facilitators experienced by patients, carers and healthcare professionals managing symptoms in infants, children and young people at end of life.
Design:
A mixed-methods systematic review and meta-analysis was undertaken (PROSPERO ID: CRD42019124797).
Data sources:
The Cochrane Library, PROSPERO, CINAHL, MEDLINE, PsycINFO, Web of Science Core Collection, ProQuest Dissertations & Theses Database, Evidence Search and OpenGrey were electronically searched from the inception of each database for qualitative, quantitative or mixed-methods studies that included data from patients, carers or healthcare professionals referring to barriers or facilitators to paediatric end-of-life symptom management. Studies underwent data extraction, quality appraisal, narrative thematic synthesis and meta-analysis.
Results:
A total of 64 studies were included (32 quantitative, 18 qualitative and 14 mixed-methods) of medium-low quality. Themes were generated encompassing barriers/facilitators experienced by carers (treatment efficacy, treatment side effects, healthcare professionals’ attitudes, hospice care, home care, families’ symptom management strategies) and healthcare professionals (medicine access, treatment efficacy, healthcare professionals’ demographics, treatment side effects, specialist support, healthcare professionals’ training, health services delivery, home care). Only one study included patients’ views.
Conclusion:
There is a need for effective communication between healthcare professionals and families, more training for healthcare professionals, improved symptom management planning including anticipatory prescribing, and urgent attention paid to the patients’ perspective.
Keywords: Child, paediatrics, palliative care, terminal care, pain management, caregivers, systematic review, meta-analysis
What is already known about the topic?
The palliative care needs of infants, children and young people differ to those of adults.
The broad spectrum of paediatric life-limiting or life-threatening conditions mean that symptoms are varied and complex to manage.
The UK National Institute for Health and Care Excellence (NICE) has emphasised pain management in paediatric palliative care as a research priority.
What this paper adds?
This is the first systematic review and meta-analysis to investigate and report on the barriers and facilitators experienced by carers and healthcare professionals when managing paediatric symptoms at end of life.
Healthcare professionals’ attitudes, treatment and its side effects, place of care and families’ own symptom management strategies all impact on family caregivers’ ability to manage symptoms.
Barriers and facilitators to symptom management for healthcare professionals include medicine access, treatment efficacy and side effects, specialist support, training and education, health services delivery and home care.
Implications for practice, theory or policy
This review provides information about ways to improve paediatric symptom management at end of life.
Effective communication between healthcare professionals and families, increased healthcare professional training and better symptom management planning are needed to improve pain and symptom management.
There is an urgent need for more research on paediatric patients’ views on end-of-life symptom management.
Introduction
It is estimated that nearly 1.2 million children worldwide require palliative care at end of life1 while nearly 50,000 infants, children and young people in the United Kingdom and 500,000 in the United States live with a life-threatening or life-limiting condition.2,3 The broad spectrum of these conditions and the differing palliative care needs of children compared to adults means that symptoms are varied and complex to manage.4 Effective symptom management differs significantly in children depending on their age, diagnosis, physiological and cognitive developmental stage and their ability to communicate and understand.5
There is a lack of research on family carers’ experiences of administering medicines for symptom and pain management in this population. Caregivers may not have the required knowledge and confidence to provide adequate symptom relief while also minimising side effects such as sedation. Fear of errors may lead to insufficient or inappropriate doses of analgesics.6 As such, parents will move children away from their preferred place of care if effective symptom relief cannot be provided.7 Healthcare professionals also describe home paediatric palliative care as ‘difficult, complex and ambiguous’8 suggesting that they may lack the skills and training required to support carers.
A clinical practice guideline from the UK National Institute for Health and Care Excellence (NICE) on end-of-life care for children was based on the findings of 20 systematic reviews.9 Four of these assessed the effectiveness of interventions for agitation, respiratory distress, seizures and pain management.9 Only the latter review found any studies that met the inclusion criteria and these involved pharmacological interventions only. Although these reviews provided essential guidance, to our knowledge, no systematic review has examined the barriers and facilitators to paediatric symptom management at end of life. NICE emphasised pain management in palliative care as a research priority and recommended further research on the factors influencing preferred place of end-of-life care, hypothesising that symptom management plays a critical role in this decision.9 A greater understanding of this could inform the design of evidence-based interventions to support more effective symptom management, thereby improving care for children and their families. The aim of this systematic review was to identify and synthesise the existing literature exploring barriers and facilitators experienced by patients, family carers and healthcare professionals when managing paediatric symptoms at end of life.
Methods
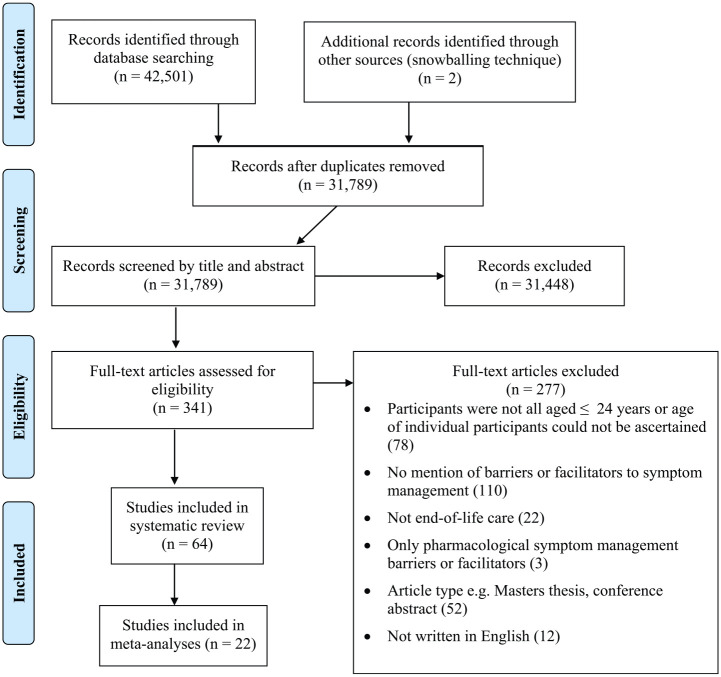
A detailed description of the searches (Supplementary File 1) and quality assessment for this systematic review is included in the published protocol10 and registered on PROSPERO (ID CRD42019124797).11 Study exclusion and inclusion criteria are shown in Table 1 and the flow diagram of the included studies is shown in Figure 1.
Table 1.
Inclusion and exclusion criteria.
| Inclusion | Exclusion | |
|---|---|---|
| Population | Views, attitudes, opinions, perceptions, beliefs or feelings of carers, healthcare professionals or patients up to the age of 24 years when managing symptoms in infants, children and young people with terminal illnesses receiving palliative care and/or at end of life. All definitions of ‘end of life’ will be included | |
| Location | Worldwide | |
| Publication type | Qualitative, quantitative and mixed-method studies | Articles written in any language other than English, masters theses, conference abstracts, reviews |
| Range of years | From the inception of each database until February 2019 |
Figure 1.
Flow of records for inclusion in the systematic review and meta-analyses of barriers and facilitators to paediatric symptom management at end of life.
Data synthesis
The majority of included studies were either qualitative, mixed-methods or involved a quantitative survey, as opposed to an intervention design. A narrative summary approach was taken as this allowed the integration of qualitative and quantitative evidence. Since qualitative data were relatively thin, a thematic synthesis approach to our narrative summary was conducted, enabling the identification and organisation of the data into prominent themes as per our protocol.10 K.G. and S.H. independently read the studies and extracted relevant findings into NVivo.12 After data familiarisation, they generated initial codes with written interpretations of quantitative data coded in the same way as qualitative data, for example, if a study reported that half of the nurses surveyed reported a lack of training in pain relief, this was coded under a theme on healthcare professionals’ training.13 The two authors discussed and compared codes and emerging themes, with successive independent re-reading of the studies and data. Over several discussions, K.G. and S.H. developed and refined common themes from the codes for patients, caregivers and healthcare professionals separately. The papers were then re-read by both reviewers to check the data fitted the codes and to check for any relevant uncoded data. There is currently no recommended approach for assessing confidence in combined qualitative and quantitative evidence.14 However, since we used an integrated design, in which quantitative data were transformed into qualitative data (themes), the GRADE-CERQual (Confidence in the Evidence from Reviews of Qualitative research)15 was used to summarise confidence in each theme.
Meta-analytic methods
A meta-analysis was chosen to synthesise and summarise the quantitative data and identify any barriers or facilitators arising from these data. The outcome for meta-analysis was the proportion of participants endorsing or reporting each specific facilitator/barrier. Data had to be available from two or more eligible studies reporting similar barriers or facilitators for meta-analyses to be conducted. For each survey item data pertaining to (1) the number of participants endorsing or reporting that barrier or facilitator and (2) the total number of valid survey responses was extracted. If data were only given in percentages, the raw values (i.e. number of participants endorsing each response) were computed. If studies divided participants into subgroups (e.g. by gender or career stage), the data were re-aggregated. The exact question asked, possible responses (where included in the original article) and raw data are provided in Supplementary File 2. Where data were available, we computed the crude unweighted mean proportion of agreement. We then used Comprehensive Meta-Analysis (CMA) version 316 to compute a pooled weighted estimate using a random-effects model since this can be used when statistical heterogeneity (I2) is present. Cochran’s Q and the I2 statistic were used to assess study heterogeneity. With Cochran’s Q, a significant result is indicative of heterogeneity. The I2 statistic describes the percentage of variability in effect estimates due to heterogeneity as opposed to sampling error.17
Results
Study selection
The titles and abstracts of 31,789 articles were reviewed by one reviewer (K.G.) and a random 20% were checked by a second reviewer (S.H.), with high inter-coder agreement (0.99 Cohen’s kappa coefficient). After discussion, 341 full-texts were read and 277 were excluded (see Figure 1 for reasons). The final review included 64 eligible studies, which included 32 quantitative studies, 18 qualitative studies and 14 mixed-methods studies (see Table 2 for study characteristics).
Table 2.
Characteristics of studies included in the systematic review.
| Study (in alphabetical order) | Aims | Participants (sample size) | Design and data collection | Date and duration | Setting and location | Data analysis methods |
|---|---|---|---|---|---|---|
| Amery18 | Map children’s palliative care around the world and survey respondents’ learning needs | Varied including healthcare professionals (251), students, managers, social workers, volunteers, academics, counsellors/psychologists, therapists (346) | Closed-question survey | 3-month period in 2010 | Online questionnaire, UK | Descriptive statistics |
| Amery and Lapwood19 | Identify and explore educational needs of children’s hospice doctors in England | UK children’s hospice doctors (35 for questionnaire, 17 for diary and interview) | Closed-question survey, diary and semi-structured interview | Not stated | Children’s hospices in the United Kingdom | Questionnaire and diary: not stated; interview: findings were discussed and crosschecked |
| Amery et al.20 | Research the children’s palliative care educational needs of healthcare professionals in Uganda | Healthcare professionals (48 for survey, 8 for survey interview and focus group) | Closed-question survey, logbook, semi-structured interview, focus group | Not stated | Hospices in Uganda, | Survey: descriptive statistics logbook, interview and focus group: thematic analysis |
| Bagatell et al.21 | Design, implement and evaluate a seminar series for paediatric residents | Paediatric residents (10 pre-test, 8 post-test) | Pre- and post-test closed-question survey | Not stated | University of Arizona, USA | Pre- and post-test comparison, descriptive statistics |
| Balkin et al.22 | Create and test a portable reference card to improve paediatric resident education | Year 1 and Year 2 paediatric residents (26) | Pre- and post-intervention closed-question survey | 6-month period in 2015 | The University of California San Francisco Benioff Children’s Hospital, USA | Pre- and post-test comparison, descriptive statistics |
| Baughcum et al.23 | Develop and evaluate a paediatric palliative care workshop for oncology fellows | Oncology fellows in a paediatric haematology/oncology fellowship programme (32) | Pre- and post- workshop closed-question survey | 1 day in November 2004 and May 2005 | Children’s Hospital in Columbus, Ohio and at the annual meeting of the American Society of Paediatric Hematology Oncology (ASPHO), Washington DC, USA | Pre- and post-test comparison, descriptive statistics |
| Bergstraesser et al.24 | Describe perceptions and needs of paediatric healthcare professionals | Paediatric healthcare professionals caring for children with palliative care needs (78) | Qualitative interview | September 2007–January 2008 and February–August 2009 | The participants’ work environments, Switzerland | Content analysis |
| Bogetz et al.25 | Examine healthcare professionals’ views on barriers to paediatric palliative care | Nurses and other paediatric specialists (275) | Online closed- and open-question survey | 2017 | Children’s hospitals within the University of California, San Francisco Health System, USA | Descriptive statistics and comparison with data from a previous study |
| Byrne et al.26 | Explore the role of parent self-efficacy related to pain management for seriously ill children and adolescents | Parents/caregivers (50) of children and adolescents expected to survive 3 years or less | Closed-question surveys | Not stated | At home or at a hospital/clinic in the USA | Descriptive statistics |
| Chen et al.27 | Evaluate the impact of training on paediatric healthcare professionals’ confidence and attitudes related to pain and symptom management for children with life-limiting or life-threatening conditions | Paediatricians and nurses who had completed a 5 hour training programme (71) | Pre- and post-training closed-question survey | Not stated | The Taichung Veterans General Hospital, Taichung City, Taiwan | Pre- and post-training comparison, descriptive statistics |
| Collins et al.28 | (1) Identify benefits and difficulties encountered by families during their child’s palliative care; (2) suggest strategies; (3) assess parents’ adjustment after their child’s death | Families (18) of children who had died receiving palliative care at home | Semi-structured interviews; closed-question survey | Not stated | Home, hospital or over the telephone, New South Wales, Australia | Not stated |
| Contro et al.29 | Obtain personal accounts of families’ experiences | Parents (68) of deceased children | Face-to-face interviews with closed- and open-questions | September 1998–March 1999 | Lucile Salter Packard Children’s Hospital (LSPCH), California, USA | Thematic analysis |
| Contro et al.30 | Conduct a staff survey on paediatric palliative care | Staff members from a children’s hospital (446) | Survey with closed-questions and 1 open-question | Not stated | Postal questionnaires, LSPCH, California, USA | Descriptive statistics and thematic analysis |
| Dangel et al.31 | (1) Measure the quality of a paediatric hospice home care programme; (2) assess parents’ needs and concerns | Parents/primary caregivers (80) of children who had died under the hospice home care | Open- and closed-question survey | Not stated | Postal questionnaire, the Warsaw Hospice for Children, Poland | Descriptive statistics |
| Davies et al.32 | Explore barriers to palliative care experienced by paediatric healthcare professionals caring for seriously ill children | Paediatric healthcare professionals (240) | Closed-question survey | January–March 2002 | Postal questionnaire, University of California, San Francisco (UCSF) Children’s Hospital, USA | Descriptive statistics |
| Dickens33 | Identify and evaluate factors associated with healthcare professionals’ confidence in delivering paediatric palliative care | Paediatric healthcare professionals with experience in paediatric palliative care (157) | Closed-question survey | 2-month period in 2005 | Emailed survey, Helen DeVos Children’s Hospital, Michigan, USA | Statistical analysis including descriptives |
| Ellis et al.34 | Describe pain management practices for children with cancer | Contact person at Canadian hospitals and clinics providing paediatric cancer treatment (26) | Closed-question survey | Not stated | Email/telephone questionnaire, Canada | Descriptive statistics |
| Fortney and Steward35 | Explore how nurses observe and manage infant symptoms at the end of life | Nurses (14) | Face-to-face exploratory qualitative interviews | Not stated | A children’s hospital in central Ohio, USA | A framework approach |
| Fowler et al.36 | Determine Children’s Oncology Group (COG) members’ comfort level in dealing with end-of-life care | Paediatric oncologist members of the COG in 2003 (623) | Closed-question survey | June 2003 | Online survey, USA | Statistics including descriptives |
| Friedrichsdorf et al.37 | Elicit parents’ perceptions of their children’s symptoms and symptom management strategies used during the last week of life | Parents of children who had died under the hospice programme | Semi-structured interview | 2004–2006 | Telephone interviews, The Barnes-Jewish Hospital Wings Paediatric Hospice Program, Missouri, USA | Categories and labels assigned to data (thematic analysis) |
| Gilmer et al.38 | Describe parental perceptions of the care of hospitalised, terminally ill children | Parents (15) of children who had died in a children’s hospital | Telephone interviews, closed- and open-question survey | Not stated | The Monroe Carell Jr Children’s Hospital, Nashville, USA | Descriptive statistics and qualitative content analysis |
| Grimley39 | Examine the knowledge, barriers and support needs of healthcare professionals providing paediatric palliative care | Healthcare professionals (225) | Survey with closed-questions and one open-question | October 2009–March 2010 | Online/paper survey, USA | Statistics including descriptives, content analysis |
| Groh et al.40 | Evaluate involvement of a specialised paediatric palliative healthcare team | Primary caregivers (40) of severely ill children | Pre- and post-intervention survey with closed- and open- questions | April 2011–June 2012 | Families’ homes, Germany | Statistics including descriptives |
| Hendricks-Ferguson41 | Identify symptoms of greatest parental concern and symptom management strategies at end of life | Parents (28) of children who had died under the hospice programme | Telephone interviews with open-ended questions | 2004–2006 | The Barnes-Jewish Hospital Wings Paediatric Hospice Program, Missouri, USA | Semantic content analysis |
| Hilden et al.42 | Assess attitudes, practices and challenges associated with end-of-life care of patients with cancer | Paediatric oncologist members of the American Society of Clinical Oncology (ASCO; 228) | Closed-question survey | Not stated | Postal survey to ASCO members in the United States, Canada and the United Kingdom | Statistics including descriptives |
| Houlahan et al.43 | Establish a standard of care to manage end-of-life symptoms | Inpatient oncology nurses and paediatric oncology fellows (24) | Closed-question survey | Not stated | Emailed survey, The Dana-Farber Cancer Institute/Children’s Hospital Cancer Care Program, Missouri, USA | Descriptive statistics |
| Klepping44 | Explore the case of a 16 year old with nasopharyngeal carcinoma | 16 year old with nasopharyngeal carcinoma approaching end of life (1) | Case study | Not stated | Hospice (location not stated) | Not stated |
| Kohler and Radford45 | (1) Find out how long children dying of cancer live for when they are taken home to die; (2) find out how these children die; (3) discover the problems faced by these families | Parents (19) of children dying of cancer | Semi-structured interview and a questionnaire (type not specified) | Not stated | Not stated | Not stated |
| Kolarik et al.46 | (1) Determine the extent of paediatric residents’ training, knowledge, experience, comfort and competence in paediatric palliative care; (2) learn about their views on palliative care and training | Paediatric residents (49) | Closed-question survey | September–December 2003 | The Children’s Hospital of Pittsburgh, Pennsylvania, USA | Statistics including descriptives |
| Lewis et al.47 | Explore the views of healthcare professionals on providing palliative and end-of-life care | Adult and paediatric nurses and doctors (32) | Focus groups, 1 semi-structured interview | Not stated | The Kilimanjaro Christian Medical Centre, Tanzania | Thematic analysis |
| Malcolm et al.48 | (1) Explore which rare life-limiting conditions in children present symptom challenges; (2) explore which symptoms are difficult to manage | Healthcare professionals (43), families (16) | Closed- and open-question survey | 3 weeks (not stated when) | Online questionnaire, UK | Thematic analysis |
| Mariyana et al.49 | Explore the experiences of mothers managing their children’s pain during palliative care | Mothers (8) of children with cancer receiving palliative care | Semi-structured face-to-face interview | Not stated | The Rachel House Foundation, West Jakarta and Taufan Jakarta Community, India | The Colaizzi method of analysis |
| Maynard and Lynn50 | Evaluate the effectiveness of delivering 24/7 children’s palliative care | Healthcare professionals (53), hospice professionals (60), families (26) | Closed- and open-question survey | Not stated | England (setting not stated) | Descriptive statistics, thematic analysis using a framework approach |
| McCabe et al.51 | Document the frequency and context of paediatric resident experiences with paediatric end-of-life care and their views on adequacy of training | Paediatric residents (40) | Closed-question survey | February–April 2006 | Emailed questionnaire, the Johns Hopkins Children’s Center, Maryland, USA | Statistics including descriptives |
| McCluggage and Elborn52 | Identify the symptoms that cause the most anxiety to healthcare professionals | Healthcare professionals working in UK children’s hospices (38) | Open- and closed-question survey | Not stated | Postal questionnaire, UK | Descriptive statistics |
| Meyer et al.53 | Examine perspectives and priorities of parents of children at end of life in the PICU | Parents of infants at end of life in the PICU (56) | The Parental Perspectives Questionnaire:53 closed- and open- questions | Not stated | Postal questionnaire, 3 paediatric intensive care units in Boston, USA | Descriptive statistics |
| Michelson et al.54 | Determine paediatric residents and fellows’ views, training, knowledge, experience, comfort and perceived competence in palliative care | Paediatric residents (52) and fellows (46) | Closed-question survey | Not stated | Emailed questionnaire, USA (study hospital not stated) | Statistics including descriptives |
| Monterosso et al.55 | Elicit parents’ and service providers’ views of supportive and palliative care | Service providers (n not stated) and families of children with life-threatening conditions (129) | Telephone or face-to-face survey with closed- questions (families), semi-structured interviews (families and service providers) | February 2003 and March 2005 | Western Australia (setting not stated) | Descriptive statistics and content analysis |
| Monterosso and Kristjanson56 | Determine (1) the palliative and supportive care needs of families whose children died from cancer; (2) how well these needs were met; (3) perceived barriers to service provision | Families (24) of children dying of cancer | Telephone or face-to-face semi-structured interviews, survey with closed- questions | February 2003 and March 2005 | Western Australia (setting not stated) | Descriptive statistics, thematic analysis, latent content analysis and constant comparison techniques |
| Monterosso et al.57 | Determine (1) the palliative and supportive care needs of families whose children died from cancer; (2) how well these needs were met; (3) perceived barriers to service provision | Families (69) of children who had died from cancer | Phone or face-to-face semi structured-interviews with open and closed questions | Not stated | Western Australia (setting not stated) | Statistics including descriptives |
| Naicker et al.58 | Describe the development of a palliative care package for the home care of young children | Home- and community-based care workers (28) | Photo-elicitation | Not stated | Rural areas in KwaZulu-Natal, South Africa | Thematic analysis |
| Peng et al.59 | Explore (1) neonatal nurses’ experiences of caring for dying neonates; (2) their palliative care education; (3) their educational needs | Neonatal nurses (115) | Closed-question survey | October 2011–July 2012 | 3 medical centres in the central area of Taiwan | Descriptive statistics |
| Price et al.60 | Examine healthcare professionals’ views on caring for children at end of life | Health and social care professionals (35) | Focus group interviews | November 2008–January 2009 | UK (setting not stated) | Thematic content analysis |
| Price61 | Explore bereaved parents’ experiences of providing children’s end-of-life care | Bereaved parents (25) | Face-to-face interview with open-ended questions | November 2007–September 2008 | Participants’ homes, UK | Thematic analysis followed by narrative analysis |
| Pritchard62 | Study the symptoms experienced by dying children that were of most concern to parents | Parents of children who had died from cancer (42) | Telephone interviews with open-ended questions, medical record reviews | Not stated | A paediatric cancer centre, USA | Statistics including descriptive statistics |
| Pritchard et al.63 | Identify (1) cancer-related symptoms that most concerned parents of children at end of life; (2) the care strategies that parents found helpful from healthcare professionals | Parents of children who had died from cancer (65) | Telephone interview, review of medical records | Not stated | A paediatric cancer centre, USA | Content analysis and consensus coding, descriptive statistics |
| Rapoport et al.64 | Examine the attitudes of palliative care physicians towards paediatric patients | Palliative care physicians (44) | Open- and closed-question survey | 4-month duration | The University of Toronto, Ontario, USA | Descriptive statistics, content analysis |
| Saad et al.65 | Evaluate the quality of paediatric palliative care as perceived by bereaved parents | Parents (29) of children who had died of cancer | Face-to-face interview with open- and closed- questions | September–December 2008 | Parents’ home, Lebanon | Descriptive statistics, analysis for open-ended questions not stated |
| Stein et al.66 | Assess the impact of chronic life-threatening illness on families and their perception of hospice care | Families (25) of children with chronic life-threatening illnesses | Face-to-face interview consisting of a semi-structured questionnaire and survey | Not stated | Oxfordshire, UK | Descriptive statistics; analysis of open- ended data not described |
| Szymczak et al.67 | Explore paediatric oncology providers’ views on the paediatric palliative care service | Paediatric oncology providers (16) | Semi-structured interviews with open-ended questions | Not stated | A place of the participants’ choosing the United States (state not stated) | Modified grounded theory approach |
| Tamannai et al.68 | (1) Gain a better understanding of the needs of Burkitt–Lymphoma patients and families in rural Cameroon; (2) assess their perception of the palliative care outreach programme; (3) identify issues | Children with Burkitt–Lymphoma (3), their caregivers (7) and nurses (2) | Semi-structured interviews with open-ended questions | Not stated | Interviews conducted during home visits in a rural area of Cameroon | Thematic analysis |
| Theunissen et al.69 | Examine symptoms in children with cancer and their parents during palliative care | Parents (59) of children with cancer receiving palliative care | Postal questionnaire with closed- questions, review of medical records | Not stated | The Radboud University Nijmegen Medical Centre (RUNMC), The Netherlands | Descriptive statistics |
| Thienprayoon et al.70 | Explore parental perspectives on the hospice experience | Parents (34) of children who had died of cancer | Qualitative interview with open-ended questions | Not stated | Interviews conducted at a location chosen by the parent, Children’s Medical Center Dallas, Texas, USA | Thematic content analysis |
| Ullrich et al.71 | (1) Describe fatigue as experienced by children with advanced cancer; (2) evaluate factors hypothesised to be associated with fatigue and its treatment | Parents (141) of children who had died of cancer | Telephone or face-to-face semi-structured survey – all closed- questions | 1997–2001 | The Dana-Farber Cancer Institute/Children’s Hospital Boston and the Children’s Hospitals and Clinics, St Paul and Minneapolis, USA | Statistics including descriptives |
| Van der Geest et al.72 | Explore the perspective of GPs caring for children with advanced cancer at home | GPs (91) | Open- and closed-written survey | 2013 | The Netherlands (setting not stated) | Statistics including descriptives |
| Verberne et al.73 | Provide an overview of parental caregiving | Parents (42) caring for children with life-limiting diseases | Interview with open- questions | August 2013–November 2015 | Interviews conducted at parents’ homes, Amsterdam, The Netherlands | Inductive thematic analysis |
| Vickers et al.74 | Gain understanding into parents’ experience of caring for a terminally ill child | Parents (10) of children who had died | Interview with open- questions | Not stated | Interviews conducted at parents’ homes, UK | Thematic content analysis |
| Vollenbroich et al.75 | Evaluate the perception of symptoms, treatment and their influence on palliative care as perceived by parents | Parents of children who had died due to a life-limiting disease (38) | Closed-question postal survey | June–December 2007 | The Coordination Center for Paediatric Palliative Care (CPPC) of the University of Munich, Germany | Statistics including descriptives |
| Vollenbroich et al.76 | Evaluate whether paediatric palliative home care can be improved with a paediatric palliative home care team | Parents (38) of children who had died, healthcare professionals involved in the children’s care (87) | Closed-question postal survey | June–December 2007 | The Coordination Center for Paediatric Palliative Care (CPPC) of the University of Munich, Germany | Statistics including descriptives |
| Wheeler77 | (1) Establish survey properties; (2) describe attitudes and practices of paediatric nurses regarding the care of infants and children with life-threatening conditions; (3) assess barriers to care; (4) examine differences in attitudes, practices and barriers | Paediatric nurses (343) | Closed-question survey | Not stated | A large children’s hospital, USA | Statistics including descriptives |
| Wolfe et al.78 | Determine (1) the patterns of care among children who die of cancer; (2) the symptoms, effectiveness of treatment and factors related to suffering from pain at end of life | Parents (103) of children who had died from cancer | Telephone or face-to-face interview with closed- questions, review of medical records | September 1997–1998 | Boston Children’s Hospital and the Dana-Farber Cancer Institute in Boston, USA | Statistics including descriptives |
| Yorke79 | Explore experiences of families whose child died in the paediatric intensive care unit (PICU) | Parents (23) of children who died in PICU | Semi-structured interview and closed-question survey | Not stated | PICU at the UNC Children’s Hospital, USA | Constant comparison content analysis |
| Zaal-Schuller et al.80 | Investigate (1) what parents and physicians consider important for quality of life in children with profound intellectual and multiple disabilities (PIMD); (2) how parents and physicians discuss and incorporate quality of life in end-of-life decision-making | Parents (17) of children with PIMD and physicians (11) | Semi-structured interviews with open-ended questions | Not stated | The Netherlands | Qualitative data analysis using coding |
| Zelcer et al.81 | Explore the end-of-life experience of children with brain tumours and their families | Parents (25) of deceased children with brain tumours | Focus group interview | Not stated | Interview conducted outside of hospital, the Children’s Hospital, London Health Sciences Center, Canada | Thematic analysis |
Study appraisal
The majority of the included studies were of low/moderate quality (see Supplementary File 3). Trustworthiness82 of qualitative studies was rated as high in 11, medium in 6 and low in 4 studies. Inter-coder agreement was 0.72, 0.80 and 0.25 Cohen’s kappa coefficient for the qualitative, mixed-methods and quantitative studies, respectively. Low inter-rater reliability for the quantitative studies was due to different interpretation of one question (E1) on the Quality Assessment Tool for Quantitative Studies (QATQS)83 regarding the criteria for assessing the validity of questionnaires. Once the interpretation of this item was discussed and agreed, the studies were reassessed on this item giving an overall inter-rater reliability for the QATQS of 0.90 Cohen’s kappa coefficient.
Confidence in the evidence (the themes) was assessed using the GRADE-CERQual (Supplementary File 4). For the majority of the evidence, confidence was reduced due to moderate–substantial methodological limitations (insufficient detail on data collection and analysis and validity and reliability of quantitative data collection tools).
Thematic analysis
The thematic analysis produced six key themes relating to family carers’ views and eight themes relating to healthcare professionals’ views on barriers or facilitators to symptom management. Only one included study involved children’s views. A summary is presented in Supplementary File 5.
Barriers and facilitators to symptom management reported by family carers
Giving treatment
Giving adequate medication was, unsurprisingly, seen as beneficial in improving or managing children’s symptoms.41,45,53,62,63,75,78 One study highlighted the importance of free medication for providing adequate pain control.68 In several studies, parents stated that children were not given sufficient medication or treatment therefore leading to poor symptom management (Supplementary File 5, quotation 1 (Q1)),29,30 particularly when a child’s condition deteriorated;61 he or she developed complications;61,73 or when there was a lack of available drugs licensed for children.61 Inadequate assistance with administering or managing treatment was a barrier to symptom management in two studies.55,57 Some families also felt the assessment of their child’s emotional symptoms was not properly met,50 suggesting that they were not sufficiently treated either.
Treatment side effects
Parents made decisions not to use medication aimed at treating symptoms, due to the drugs’ side effects. In one study, for example, parents turned down a doctor’s suggestion for chemotherapy as they did not want their child to be sick and miserable (Q7).62 The only study involving patient interviews included a 14 years old who had decided to stop taking oral morphine due to nausea, despite the ‘burning pain’ she experienced.68
When new symptoms appeared, parents had to decide between leaving these untreated or risking new or worsened side effects.73 One study also reported a parent’s view that healthcare professionals did not treat their child’s pain due to fear of symptoms from the medication (Q8).79 Some parents chose perceived quality of life (QoL) over pain relief, delayed the start of pain medication so their child could play, assuming that they would only sleep if treatment was given.73 However, our review also suggests that parents will expose their child to side effects if they feel this is beneficial overall. In one study, for example, a minority of parents mentioned very low QoL with little chance for improvement as a reason for starting pain relief medication that could lead to or hasten death.80
Healthcare professionals’ attitudes
Parents’ perception of symptom management is influenced by healthcare professional’s attitudes towards them and their children.29,30,41,48,61,62,66,75,78 Parents felt healthcare professionals were dismissive of symptoms such as constipation48 or did not take their concerns about inadequate pain relief seriously (Q10).29 They discuss having to convince healthcare professionals to give pain medication or other treatment.62 Lack of involvement in the child’s care (as reported by parents) by an oncologist was associated with more suffering from pain.78
Inadequate communication from healthcare professionals was also a barrier to symptom management. One study described how parents wished hospital staff had communicated sooner that pain doctors were available (Q11).30 In another, children’s pain was associated with parents’ perception of receiving conflicting information from healthcare professionals.78
In contrast, when healthcare professionals were seen as vigilant and attentive, this was perceived to have a beneficial impact on symptom management. This included anticipating the child’s needs,41,61 treating parents as active members of the child’s care team, being honest with them (Q12),29 listening to parents29 and the child (Q14),62 and placing a high priority on symptom relief.66 Several studies38,57,75 reported that advice or information from healthcare professionals facilitated symptom management. For example, a father in one study discussed how he was initially concerned that his baby would only be treated for pain; however, the paediatric palliative care team explained that other potential symptoms could be managed (Q15).75
Influence of hospice care
In several studies, families described how the hospice environment was helpful for controlling children’s pain and other symptoms.31,66,70 Families valued the emphasis on symptom relief at the hospice (as opposed to a focus on interventions to manage the child’s condition) and the staff’s experience with rare conditions and complex symptom clusters.66
However, one study conducted in the United States found that Spanish-speaking families viewed the hospice as a facilitator to symptom management (Q16); yet English-speaking families returned to hospital care due to poor symptom control.70 The authors suggest this could be due to Spanish-speaking families prioritising place of care (at home or at the hospice as opposed to the hospital) over pain control, while the English-speaking families’ main priority was pain and symptom relief. In another study, parents noted that the hospice did not know how to control the pain, but they were unable to access a hospital pain team because the child was not an inpatient.29
Care and support at home
A number of studies highlighted barriers to symptom management for children being looked after at home.28,31,65 Parents feared that their child might not receive medical treatment,31 and that symptoms would not be controlled.45,81 One study noted a parent’s fear that they would make their child worse if they accidentally gave too much medication (Q17).74 Several studies noted that parents reported a lack of information, knowledge and support around pain control and symptom management (Q20, Q21).48,55,57,68
When parents did receive information, advice or education from healthcare professionals or disease-specific organisations, this was seen to facilitate symptom management.41,48,62 In one study, the child’s suffering was not worse in children being cared for at home and receiving specialised paediatric palliative care compared to those being cared for in hospital.37 However, parents in another study emphasised that they had learnt to control their child’s symptoms ‘on their own’; yet some still struggled when their child’s disease progressed or when complications occurred.73
Other barriers to symptom management at home included a lack of access to support in the form of home visits from healthcare professionals38,49 or 24-hour support.50,56 Community nurses were viewed as facilitating symptom management by providing complex care at home such as the preparation of pain relief (Q22).56 One parent noted the importance of having a regular nurse to help with home care, who had knowledge of their child’s specific symptoms (Q23).56
Availability of resources at home also affected symptom management. Parents reported having to wait for, or locate, prescribed medication after leaving hospital or having to coordinate care from different agencies.62 In one study, children were admitted to hospital due to limited availability of equipment at home.65 In other studies, healthcare professionals supported parents by arranging the necessary equipment (Q24).56,61 In a study conducted in India, some parents noted they were not able to administer enough medication to control pain at home and they also had difficulties in using or accessing hospital services due to cost and transportation barriers.49
Caregiver mental wellbeing may also influence symptom management at home. Byrne and colleagues found that self-efficacy to manage children’s pain was negatively associated with higher parental strain and negative mood and positively associated with higher parental vigour.26 While this suggests that parental mood and strain could impact on pain management, this study cannot demonstrate causality.
Families’ symptom management strategies
Several studies reported that families carried out a number of non-pharmacological symptom management strategies. One study described how parents worked constantly to reduce, relieve or prevent symptoms.73 In another study, mothers assessed their child’s pain by asking them using a pain level tool (0–10) to determine the extent of their pain before deciding on suitable symptom management.49
Placing the child in different positions to avoid issues such as skin breakdown and pain was noted as a symptom prevention strategy (Q27)41 as were distraction techniques such as reading, singing and talking to the child41,49 and encouraging and motivating children to fight their pain.49 In India, parents used non-pharmacological treatments such as kencur (i.e., Kaempferia galanga, also known as aramotic ginger) or eucalyptus oil or massages to help eliminate their child’s pain.49 Parents felt they helped relieve their child’s symptoms by staying close to them and providing physical comfort.41,49,62 Healthcare professionals staying close to the child was also viewed as helpful by parents.62 In addition, some parents chose to keep their child out of day care to minimise the risk of infection.73 Parents described feeling overwhelmed by the decisions they had to make around preventing or reducing symptoms and balancing this with the need for the child to have ‘a life worth living’.73
Barriers and facilitators to symptom management reported by healthcare professionals
Access to medicines
A lack of access to medicines and resources was noted as a barrier to providing care in four studies (Q28).20,47,58,60 Three of these were conducted in low-income countries where medical care access is limited for economic reasons; however, one study was based in the United Kingdom.60 It was not clear whether the lack of access in this instance was financial or logistical.
Treatment efficacy
Healthcare professionals in several studies reported children experiencing pain and other symptoms.37 In some cases, this was linked to inadequate pain control59 or not addressing emotional symptoms,50 although the reasons for this were not identified. In a case review, Klepping44 describes a teenage boy whose pain was worsened by events around him (such as the presence of certain family members), which appeared to impede the effectiveness of medication.
Age and gender of healthcare professionals
Two studies found that male healthcare professionals had greater confidence or comfort in managing symptoms compared to female healthcare professionals.33,36 The authors in these studies suggested this could be due to differing perceptions of comfort36 or differences in self-reporting confidence.33 Older healthcare professionals were also more confident in managing symptoms,33 which could be linked to greater experience, self-report differences or accumulating life experiences.33 Physicians and nurses reported greater expertise in managing symptoms compared to psychosocial staff.39 The reasons for this were not described.
Treatment side effects
Healthcare professionals’ concerns about side effects of treatment can be a barrier to symptom management when decisions are made not to administer medication. In several studies, fears of addiction, sedation, respiratory depression or hastening death were identified as potential barriers to treatment (Q30).34,43,47 Balancing the need for symptom relief with the risk of these side effects was a difficult decision for some healthcare professionals.80 However, side effects were not always barriers but rather acted as facilitators to seeking alternative symptom management – one study reported a patient’s preference for the side effect (drowsiness) as opposed to being in pain.44,80
Specialist advice and support
In a number of studies, healthcare professionals stated that access to specialist support, for example, from a paediatric palliative care team, would be favourable for paediatric symptom management.24,35,54,77 In three studies, healthcare professionals had access to either a specialist paediatric palliative care team or support from other colleagues, and this was viewed as beneficial for effective symptom management.52,67,76 In one study, the involvement of a palliative care team was delayed by physicians, who were concerned about families readiness for palliative care, the association of ‘palliative’ with ‘death’ and the fear of negatively impacting the physician–family relationship.67
Healthcare professional education, training, knowledge and experience
In a number of studies, healthcare professional’s education, training, knowledge and/or experience were seen as barriers or facilitators to symptom management. Only one study appeared to indicate that the majority of healthcare professionals felt they had sufficient knowledge to manage symptoms at end of life.34 Healthcare professionals reported having inadequate training, education or support to manage symptoms in children at end of life, and that they would value further training.19–21,25,32,43,46,51,54,58,59,64,76 In one study, the barriers to obtaining the necessary education or training included a lack of opportunities, time and costs.34 Fowler et al.36 found that healthcare professionals with formal training were more likely to feel comfortable treating pain and psychological issues.
Healthcare professionals described feeling inexperienced to manage symptoms.30,39 In two studies, healthcare professionals felt this resulted from the ‘low volume’ of patients they encountered with complicated pain problems.34,39 In line with this, healthcare professionals with more experience reported greater confidence in treating pain33 and this was associated with less fatigue in children.71
A lack of experience or exposure to certain conditions meant that healthcare professionals voiced difficulties in managing rare and/or progressive conditions48 and in recognising and treating symptoms35,52 sometimes due to a lack of guidance or evidence (Q34, Q35).48 Studies found improvements in healthcare professionals’ comfort, confidence or knowledge following training or education aimed at improving end-of-life symptom management.21–23,27 In one study in Uganda, a healthcare professional noted that a myth had existed that children do not experience pain. Training had enabled the healthcare professional to appreciate that this was untrue and therefore that pain can be assessed and managed (Q36).20 Another study found that paediatric residents’ self-reported knowledge and comfort in end-of-life symptom management increased after the introduction of a Paediatric End-of-Life Care Management Reference Card.22
Delivery of health services
This theme encompasses the working practices utilised by healthcare professionals, how decisions are made and how care is planned. It includes how healthcare professionals collaborate within teams and with families. The benefits of well-planned, interdisciplinary decision-making and symptom management were reported in one study,50 whereas another identified these as areas that needed attention, along with the lack of standardisation of care and symptom control.24 In another study, general practitioners (GPs) providing home-based palliative care reported receiving insufficient information from the hospital about symptoms and difficulties during the palliative phase.72 Similarly, after a review of patient cases, Houlahan and colleagues43 identified barriers including a lack of available physicians as reported by nurses, difficulty in obtaining orders for medication and delays in obtaining medication from pharmacy.
Disagreement and conflict about treatment decisions and goals were identified as other symptom management barriers. Conflict (about treatment) between healthcare professionals and families was noted in three studies,32,35,60,77 as well as disagreement among healthcare professionals (Q37)19,35 and among families.77
Factors relating to care at home
One study conducted a survey on pain management in Canadian paediatric cancer centres.34 The authors note the difficulties encountered by healthcare professionals in these areas including a lack of infrastructure for effective and timely links between the cancer centre, community and the family. The need for parent and home care nurse education around pain assessment and management was also highlighted. In a study conducted in Tanzania,47 the hospital was reported by healthcare professionals as the best place for care due to the lack of equipment at home (Q39). In another study, adequate pain control and symptom management were noted as difficult due to lack of communication between hospital and community staff.72
Meta-analysis
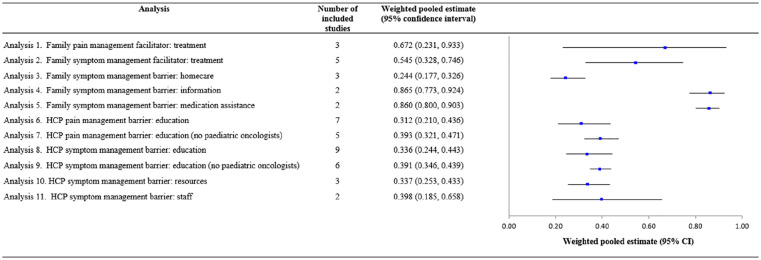
Meta-analyses were run on six barriers/facilitators, four of which corresponded to the themes developed through the thematic analysis. Forest plots are shown in Supplementary File 6, and overall effect sizes are shown in Figure 2.
Figure 2.
Overall weighted pooled estimates and 95% confidence intervals (CIs) for each analysis of barriers and facilitators to paediatric symptom management at end of life.
Squares represent the barrier/facilitator weighting with horizontal lines representing the corresponding 95% CIs.
Barriers and facilitators to symptom management reported by family carers
Three studies53,75,78 that asked families about pain management facilitators found that giving treatment (usually pharmacological though this was not always specified) was helpful. This was reported by between 27% and 84% of participants (crude unweighted mean: 0.645, 95% confidence interval (CI): 0.278–1.011). Meta-analysis (Analysis 1) yielded a pooled weighted mean of 0.672 (k = 3, n = 197, 95% CI = 0.231–0.933), with significant heterogeneity (Cochran’s Q = 53.06, df = 2, p < 0.001, I2 = 96.23). A further meta-analysis (Analysis 2) on studies that surveyed families about symptom management in general (not just pain)53,62,63,75,78 found that treatment was again reported as a facilitator (crude unweighted mean = 0.541, 95% CI = 0.342–0.739). The pooled weighted estimate was 0.545 (k = 5, n = 295, 95% CI: 0.328–0.746), with significant heterogeneity (Cochran’s Q = 47.77, df = 4, p < 0.001, I2 = 91.63).
Three studies included survey items about the effect of caring for a child at home on symptom management.28,31,65 This was reported as a barrier by between 22% and 24% of participants (crude unweighted mean: 0.238, 95% CI: 0.077–0.399). Meta-analysis (Analysis 3) yielded a pooled weighted mean of 0.244 (k = 3, n = 197, 95% CI = 0.177–0.326), without significant heterogeneity (Cochran’s Q = 0.06, df = 2, p = 0.969, I2 = 0.00).
Two studies38,57 reported that advice or information facilitated symptom management for between 86% and 93% of participants (crude unweighted mean: 0.894, 95% CI: 0.818–0.971). Meta-analysis (Analysis 4) yielded a pooled weighted mean of 0.865 (k = 2, n = 84, 95% CI = 0.773–0.924), without significant heterogeneity (Cochran’s Q = 0.63, df = 1, p = 0.428, I2 = 0.00).
A lack of assistance with administering or managing treatment was reported as a barrier to symptom management in two studies55,57 by between 84% and 87% of participants (crude unweighted mean: 0.857, 95% CI: 0.825–0.888). Meta-analysis (Analysis 5) yielded a pooled weighted mean of 0.860 (k = 2, n = 179, 95% CI = 0.800–0.903), without significant heterogeneity (Cochran’s Q = 0.36, df = 1, p = 0.547, I2 = 0.00).
Barriers and facilitators to symptom management reported by healthcare professionals
Inadequate training, education or support to manage symptoms in children at end of life was a barrier to pain management reported by between 0% and 61.9% of participants in seven studies25,30,32,36,39,42,64 (crude unweighted mean: 0.316, 95% CI: 0.131–0.450). Meta-analysis (Analysis 6) yielded a pooled weighted mean of 0.312 (k = 7, n = 2317, 95% CI = 0.210–0.436), with significant heterogeneity (Cochran’s Q = 147.410, df = 6, p < 0.0001, I2 = 95.93). Perceived lack of confidence or support was considerably lower in studies that only surveyed paediatric oncologists36,42,43 as opposed to nurses or other physicians. A further analysis was run after excluding these studies. The crude unweighted mean was 0.414 (95% CI: 0.258–0.570) and the pooled weighted estimate (Analysis 7) was 0.393 (k = 5, n = 1474, 95% CI: 0.321–0.471), with significant heterogeneity (Cochran’s Q = 30.693, df = 5, p < 0.001, I2 = 83.71).
Nine studies surveyed healthcare professionals on the extent that they lacked education, training, knowledge or experience in paediatric symptom management in general (including, but not limited to, pain) at end of life.25,30,32,36,39,42,43,64,76 Again, this was reported by between 0% and 61.9% of participants (crude unweighted mean: 0.346, 95% CI: 0.206–0.486). Meta-analysis (Analysis 8) yielded a pooled weighted mean of 0.336 (k = 9, n = 2412, 95% CI: 0.244–0.443), with significant heterogeneity (Cochran’s Q = 142.56, df = 8, p < 0.001, I2 = 94.39). After excluding studies that only surveyed paediatric oncologists,36,42,43 the crude unweighted mean was 0.411 (95% CI: 0.299–0.523) and the pooled weighted estimate (Analysis 9) was 0.391 (k = 6, n = 1561, 95% CI: 0.346–0.439), with significant heterogeneity (Cochran’s Q = 15.10, df = 5, p = 0.01, I2 = 66.89).
Three studies reported that a lack of resources (information or staff) was a barrier to symptom management43,72,77 for between 30% and 56% of participants (crude unweighted mean: 0.393, 95% CI: 0.269–0.759). Meta-analysis (Analysis 10) yielded a pooled weighted mean of 0.337 (k = 3, n = 450, 95% CI = 0.253–0.433), without significant heterogeneity (Cochran’s Q = 4.64, df = 2, p = 0.098, I2 = 56.86). A follow-up analysis (Analysis 11) on studies that included items regarding a lack of staff specifically43,77 found a crude unweighted mean of 0.430 (95% CI: 0.170–0.690) and a pooled weighted estimate of 0.398 (k = 2, n = 359, 95% CI: 0.185–0.658) with significant heterogeneity (Cochran’s Q = 4.608, df = 1, p = 0.032, I2 = 78.30).
Discussion
Main findings
This narrative synthesis and meta-analysis has uniquely identified the barriers and facilitators to paediatric symptom management at end of life. Both family carers and healthcare professionals described barriers and facilitators related to treatment efficiency and side effects, and factors relating to care at home, particularly issues around a lack of education and information. In addition, family carers described aspects of hospice care; the attentiveness of healthcare professionals; their own symptom management strategies; ease of access to medicines, assistance with medication and provision of information as affecting symptom management. Healthcare professionals emphasised support from palliative teams as a facilitator and issues relating to health service delivery as a barrier to managing symptoms. These factors link to the recent NICE guidelines,9 which recommend that healthcare professionals consider the importance of good communication with families, providing information, care planning, practical and social support, support for caregivers and appropriate service delivery.
Our review has highlighted the importance of symptom management planning in paediatric end-of-life care especially since caregivers and healthcare professionals believe that children suffer at end of life due to inadequate symptom treatment. This could be due to fear of treatment side effects, which may be based on inaccurate or outdated beliefs. In keeping with this, aside from paediatric oncologists, healthcare professionals in several studies reported that a lack of training and education prevented effective symptom management. Paediatric palliative care was only recognised as a speciality in the United Kingdom in 2009;84 yet the studies in our review date back to 1985; as such, misunderstandings related to treatments may be less prevalent today. Nonetheless, widespread implementation of paediatric palliative care is far from being attained in many countries, including the United States;85 thus, misconceptions about side effects may still hinder symptom management in many areas of the world. We recommend that clear and comprehensive symptom management plans are implemented to avoid children suffering at end of life, and that healthcare professionals involved in paediatric palliative care are given adequate training to recognise, treat and prevent symptoms including pain.
Issues around care at home were linked to poor symptom management and further indicate the need for good care planning. Caring for a child at end of life is challenging for parents,86 and our study highlights the need for more practical and social support and information to enable children to be looked after in their chosen place of care.9 Without effective pain relief, they may face unnecessary hospital admissions.7 We recommend that families are provided with information about symptom management so that they are equipped to effectively manage symptoms, including pain, when providing care for children at home. Future research could investigate what specific support or information is required to manage symptoms at home.
Our review highlights the need for good communication between healthcare professionals and families and within care teams. Some family carers felt that healthcare professionals did not respond to their concerns about symptoms, or that they received conflicting advice. Healthcare professionals also reported conflict within care teams. Delivery of palliative care services should be organised to ensure continuous care and prevent delays in access to treatment, with guidelines that enable healthcare professionals to make safe and effective decisions that put children and their families at the forefront of care. Communication training for healthcare professionals is a key component of the recommendations made by NICE9 to ensure that children and their caregivers are involved in care planning and decision-making.
Access to treatment was identified as a further potential barrier. Several studies were conducted in low-middle income countries where supply chains and prescriber difficulties may inhibit symptom management. In the United Kingdom, access to medicines for patients at home can sometimes be challenging, and we recommend that families are supported to ensure they have access to essential equipment and to the medications they require, including the provision of anticipatory prescribing.
Strengths and limitations
Our review was fairly broad in its approach and inclusive to ensure we identified as many sources of data as possible. However, due to the lack of studies specifically and properly designed to identify barriers and facilitators to paediatric symptoms management at end of life, our review has incorporated a number of studies of low quality. Some aimed to identify barriers yet did not give participants the opportunity to freely discuss these and instead presented pre-defined concepts. Other studies included decisions about treatments aimed at disease modification and/or prolonging life, rather than purely symptom management. In addition, the majority were not informed by a theoretical framework or model. Further research is required in this area, particularly regarding the views of children themselves, since only one study included patients’ perspectives.
The majority of the surveys used in the quantitative studies were devised by the researchers. This limited their comparability and the number of meta-analyses that could be performed. Differences in individual study effect sizes in the meta-analyses could be due to the varying ways in which questions were asked, especially as the exact questions and possible responses were not always listed. These findings suggest the need for a reliable, valid questionnaire assessing barriers and facilitators to paediatric symptom management at end of life.
What this study adds
Our findings are limited by the quality of studies on which this review is based; however, they highlight the importance of clear communication between clinical teams and between healthcare professionals and families. Healthcare professionals and families would benefit from increased education and training, while delivery of services needs to include social and practical support for families, anticipatory care planning and symptom management planning.
Supplemental Material
Supplemental material, Supplementary_File_1_Search_Strategy_ for A mixed-methods systematic review and meta-analysis of barriers and facilitators to paediatric symptom management at end of life by Katie Greenfield, Simone Holley, Daniel E Schoth, Emily Harrop, Richard F Howard, Julie Bayliss, Lynda Brook, Satbir S Jassal, Margaret Johnson, Ian Wong and Christina Liossi in Palliative Medicine
Supplemental material, Supplementary_File_2_Meta-analysis_raw_data for A mixed-methods systematic review and meta-analysis of barriers and facilitators to paediatric symptom management at end of life by Katie Greenfield, Simone Holley, Daniel E Schoth, Emily Harrop, Richard F Howard, Julie Bayliss, Lynda Brook, Satbir S Jassal, Margaret Johnson, Ian Wong and Christina Liossi in Palliative Medicine
Supplemental material, Supplementary_File_3_Quality_assessments_of_included_studies for A mixed-methods systematic review and meta-analysis of barriers and facilitators to paediatric symptom management at end of life by Katie Greenfield, Simone Holley, Daniel E Schoth, Emily Harrop, Richard F Howard, Julie Bayliss, Lynda Brook, Satbir S Jassal, Margaret Johnson, Ian Wong and Christina Liossi in Palliative Medicine
Supplemental material, Supplementary_File_4_Assessment_of_confidence_in_themes for A mixed-methods systematic review and meta-analysis of barriers and facilitators to paediatric symptom management at end of life by Katie Greenfield, Simone Holley, Daniel E Schoth, Emily Harrop, Richard F Howard, Julie Bayliss, Lynda Brook, Satbir S Jassal, Margaret Johnson, Ian Wong and Christina Liossi in Palliative Medicine
Supplemental material, Supplementary_File_5_Themes_developed_from_thematic_analysis for A mixed-methods systematic review and meta-analysis of barriers and facilitators to paediatric symptom management at end of life by Katie Greenfield, Simone Holley, Daniel E Schoth, Emily Harrop, Richard F Howard, Julie Bayliss, Lynda Brook, Satbir S Jassal, Margaret Johnson, Ian Wong and Christina Liossi in Palliative Medicine
Supplemental material, Supplementary_File_6_Meta-analysis_individual_forest_plots for A mixed-methods systematic review and meta-analysis of barriers and facilitators to paediatric symptom management at end of life by Katie Greenfield, Simone Holley, Daniel E Schoth, Emily Harrop, Richard F Howard, Julie Bayliss, Lynda Brook, Satbir S Jassal, Margaret Johnson, Ian Wong and Christina Liossi in Palliative Medicine
Supplemental material, Title_and_description_of_supplementary_materials for A mixed-methods systematic review and meta-analysis of barriers and facilitators to paediatric symptom management at end of life by Katie Greenfield, Simone Holley, Daniel E Schoth, Emily Harrop, Richard F Howard, Julie Bayliss, Lynda Brook, Satbir S Jassal, Margaret Johnson, Ian Wong and Christina Liossi in Palliative Medicine
Footnotes
Author contributions: E.H., R.F.H., M.J. and I.W. conceived the idea and reviewed the protocol and manuscript. C.L. conceived the idea, planned, designed, reviewed and revised the protocol, reviewed and revised the search strategy, search findings and manuscript. D.E.S. planned the searches, data extraction and statistical analysis, conducted data synthesis and reviewed and revised the protocol and manuscript. K.G. and S.H. planned and carried out the searches, data extraction, quality assessment and data synthesis and drafted and revised the protocol and manuscript. J.B., S.S.J. and L.B. provided critical insights and reviewed the study protocol and manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This study was supported by Great Ormond Street Children’s Charity and SPARKS (grant number: V5118).
ORCID iD: Christina Liossi  https://orcid.org/0000-0003-0627-6377
https://orcid.org/0000-0003-0627-6377
Supplemental material: Supplemental material for this article is available online.
References
- 1. Connor SR, Bermedo M. Global atlas of palliative care at the end of life. London: Worldwide Palliative Care Alliance and World Health Organization, 2014. [Google Scholar]
- 2. Fraser LK, Miller M, Hain R, et al. Rising national prevalence of life-limiting conditions in children in England. Pediatrics 2012; 129(4): e923–e929. [DOI] [PubMed] [Google Scholar]
- 3. International Children’s Palliative Care Network. Scale of the need, http://www.icpcn.org/information/the-need-for-childrens-palliative-care/ (accessed 7 June 2019).
- 4. Himelstein BP, Hilden JM, Boldt AM, et al. Pediatric palliative care. N Engl J Med 2004; 350: 1752–1762. [DOI] [PubMed] [Google Scholar]
- 5. Department of Health and Children. Palliative care for children with life-limiting conditions in Ireland: a national policy, https://health.gov.ie/blog/publications/palliative-care-for-children-with-life-limiting-conditions-in-ireland-a-national-policy/ (2010, accessed 13 June 2019).
- 6. Chi N-C, Demiris G, Pike KC, et al. Pain management concerns from the hospice family caregivers’ perspective. Am J Hosp Palliat Care 2018; 35(4): 601–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brombley K. Understanding the factors that influence parents as they plan and manage their child’s end of life care. In: The 3rd congress on paediatric palliative care – a global gathering, Rome, Foundazione Maruzza, 16–19 November 2016. [Google Scholar]
- 8. Castor C, Hallstrom I, Hansson H, et al. Home care services for sick children: healthcare professionals’ conceptions of challenges and facilitators. J Clin Nurs 2017; 26(17–18): 2784–2793. [DOI] [PubMed] [Google Scholar]
- 9. National Institute for Health and Care Excellence. End of life care for infants, children and young people: planning and management (NICE Guideline NG61), https://www.nice.org.uk/guidance/ng61/evidence/full-guidance-pdf-2728081261 (2016, accessed 13 June 2019). [PubMed]
- 10. Greenfield K, Holley S, Schoth D, et al. Barriers and facilitators experienced by patients, carers and healthcare professionals when managing symptoms in infants, children and young people at end-of-life: a mixed methods systematic review protocol. BMJ Open 2019; 9(7): e030566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Greenfield K, Holley S, Schoth D, et al. Systematic review of the barriers and facilitators experienced by patients, carers and healthcare professionals when managing symptoms in infants, children and young people at end-of-life CRD42019124797, http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42019124797 (2019, accessed 21 May 2019). [DOI] [PMC free article] [PubMed]
- 12. QSR International. NVivo qualitative data analysis software [computer program] (Version 12). Chadstone, VIC, Australia: QSR International Pty Ltd, 2018. [Google Scholar]
- 13. Dixon-Woods M, Agarwal S, Jones D, et al. Synthesising qualitative and quantitative evidence: a review of possible methods. J Health Serv Res Policy 2005; 10(1): 45–53. [DOI] [PubMed] [Google Scholar]
- 14. Noyes J, Booth A, Moore G, et al. Synthesising quantitative and qualitative evidence to inform guidelines on complex interventions: clarifying the purposes, designs and outlining some methods. BMJ Glob Health 2019; 4(Suppl. 1): e000893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lewin S, Glenton C, Munthe-Kaas H, et al. Using qualitative evidence in decision making for health and social interventions: an approach to assess confidence in findings from qualitative evidence syntheses (GRADE-CERQual). PLoS Med 2015; 12: e1001895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Biostat. Comprehensive meta-analysis [computer program] (Version 3). Englewood, NJ: Biostat, 2015. [Google Scholar]
- 17. Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. London: The Cochrane Collaboration, 2008. [Google Scholar]
- 18. Amery J. Mapping children’s palliative care around the world: an online survey of children’s palliative care services and professionals’ educational needs. J Palliat Med 2012; 15(6): 646–652. [DOI] [PubMed] [Google Scholar]
- 19. Amery J, Lapwood S. A study into the educational needs of children’s hospice doctors: a descriptive quantitative and qualitative survey. Palliat Med 2004; 18(8): 727–733. [DOI] [PubMed] [Google Scholar]
- 20. Amery JM, Rose CJ, Byarugaba C, et al. A study into the children’s palliative care educational needs of health professionals in Uganda. J Palliat Med 2010; 13(2): 147–153. [DOI] [PubMed] [Google Scholar]
- 21. Bagatell R, Meyer R, Herron S, et al. When children die: a seminar series for pediatric residents. Pediatrics 2002; 110(2 Pt 1): 348–353. [DOI] [PubMed] [Google Scholar]
- 22. Balkin EM, Ort K, Goldsby R, et al. Pocket reference card improves pediatric resident comfort in caring for children at end of life. J Palliat Med 2017; 20(4): 409–414. [DOI] [PubMed] [Google Scholar]
- 23. Baughcum AE, Gerhardt CA, Young-Saleme T, et al. Evaluation of a pediatric palliative care educational workshop for oncology fellows. Pediatr Blood Cancer 2007; 49: 154–159. [DOI] [PubMed] [Google Scholar]
- 24. Bergstraesser E, Inglin S, Abbruzzese R, et al. The needs of professionals in the palliative care of children and adolescents. Eur J Pediatr 2013; 172(1): 111–118. [DOI] [PubMed] [Google Scholar]
- 25. Bogetz JF, Root MC, Purser L, et al. Comparing health care provider-perceived barriers to pediatric palliative care fifteen years ago and today. J Palliat Med 2019; 22: 145–151. [DOI] [PubMed] [Google Scholar]
- 26. Byrne MW, Evan E, Goshin LS, et al. Parent self-efficacy for managing pain in seriously ill children and adolescents nearing end of life. Palliat Support Care 2011; 9(2): 137–147. [DOI] [PubMed] [Google Scholar]
- 27. Chen YC, Peng NH, Chen CH, et al. Effectiveness of pain and symptom management training for paediatric clinicians. J Res Nurs 2017; 22: 405–415. [Google Scholar]
- 28. Collins JJ, Stevens MM, Cousens P. Home care for the dying child: a parent’s perception. Aust Fam Physician 1998; 27(7): 610–614. [PubMed] [Google Scholar]
- 29. Contro N, Larson J, Scofield S, et al. Family perspectives on the quality of pediatric palliative care. Arch Pediatr Adolesc Med 2002; 156: 14–19. [DOI] [PubMed] [Google Scholar]
- 30. Contro NA, Larson J, Scofield S, et al. Hospital staff and family perspectives regarding quality of pediatric palliative care. Pediatrics 2004; 114(5): 1248–1252. [DOI] [PubMed] [Google Scholar]
- 31. Dangel T, Fowler-Kerry S, Karwacki M, et al. An evaluation of a home palliative care programme for children. Ambul Child Health 2000; 6: 101–114. [Google Scholar]
- 32. Davies B, Sehring SA, Partridge JC, et al. Barriers to palliative care for children: perceptions of pediatric health care providers. Pediatrics 2008; 121(2): 282–288. [DOI] [PubMed] [Google Scholar]
- 33. Dickens DS. Building competence in pediatric end-of-life care. J Palliat Med 2009; 12(7): 617–622. [DOI] [PubMed] [Google Scholar]
- 34. Ellis JA, McCarthy P, Hershon L, et al. Pain practices: a cross-Canada survey of pediatric oncology centers. J Pediatr Oncol Nurs 2003; 20(1): 26–35. [DOI] [PubMed] [Google Scholar]
- 35. Fortney CA, Steward DK. A qualitative study of nurse observations of symptoms in infants at end-of-life in the neonatal intensive care unit. Intensive Crit Care Nurs 2017; 40: 57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fowler K, Poehling K, Billheimer D, et al. Hospice referral practices for children with cancer: a survey of pediatric oncologists. J Clin Oncol 2006; 24(7): 1099–1104. [DOI] [PubMed] [Google Scholar]
- 37. Friedrichsdorf SJ, Postier A, Dreyfus J, et al. Improved quality of life at end of life related to home-based palliative care in children with cancer. J Palliat Med 2015; 18(2): 143–150. [DOI] [PubMed] [Google Scholar]
- 38. Gilmer MJ, Foster TL, Bell CJ, et al. Parental perceptions of care of children at end of life. Am J Hosp Palliat Care 2013; 30(1): 53–58. [DOI] [PubMed] [Google Scholar]
- 39. Grimley ME. Survey on pediatric palliative care for healthcare providers (SPPCHP): identifying knowledge, barriers, and support needs. PhD Thesis, University of Miami, Coral Gables, FL, 2011. [Google Scholar]
- 40. Groh G, Borasio GD, Nickolay C, et al. Specialized pediatric palliative home care: a prospective evaluation. J Palliat Med 2013; 16(12): 1588–1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hendricks-Ferguson V. Physical symptoms of children receiving pediatric hospice care at home during the last week of life. Oncol Nurs Forum 2008; 35(6): E108–E115. [DOI] [PubMed] [Google Scholar]
- 42. Hilden JM, Emanuel EJ, Fairclough DL, et al. Attitudes and practices among pediatric oncologists regarding end-of-life care: results of the 1998 American Society of Clinical Oncology survey. J Clin Oncol 2001; 19(1): 205–212. [DOI] [PubMed] [Google Scholar]
- 43. Houlahan KE, Branowicki PA, Mack JW, et al. Can end of life care for the pediatric patient suffering with escalating and intractable symptoms be improved. J Pediatr Oncol Nurs 2006; 23(1): 45–51. [DOI] [PubMed] [Google Scholar]
- 44. Klepping L. Total pain: a reflective case study addressing the experience of a terminally ill adolescent. Int J Palliat Nurs 2012; 18(3): 121–127. [DOI] [PubMed] [Google Scholar]
- 45. Kohler JA, Radford M. Terminal care for children dying of cancer: quantity and quality of life. Br Med J 1985; 291(6488): 115–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kolarik RC, Walker G, Arnold RM. Pediatric resident education in palliative care: a needs assessment. Pediatrics 2006; 117(6): 1949–1954. [DOI] [PubMed] [Google Scholar]
- 47. Lewis EG, Oates LL, Rogathi J, et al. ‘We never speak about death’. Healthcare professionals’ views on palliative care for inpatients in Tanzania: a qualitative study. Palliat Support Care 2018; 16(5): 566–579. [DOI] [PubMed] [Google Scholar]
- 48. Malcolm C, Forbat L, Anderson G, et al. Challenging symptom profiles of life-limiting conditions in children: a survey of care professionals and families. Palliat Med 2011; 25(4): 357–364. [DOI] [PubMed] [Google Scholar]
- 49. Mariyana R, Allenidekania A, Nurhaeni N. Parents’ voice in managing the pain of children with cancer during palliative care. Indian J Palliat Care 2018; 24(2): 156–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Maynard L, Lynn D. Innovative approach to providing 24/7 palliative care for children. Nurs Child Young People 2014; 26(6): 27–34. [DOI] [PubMed] [Google Scholar]
- 51. McCabe ME, Hunt EA, Serwint JR. Pediatric residents’ clinical and educational experiences with end-of-life care. Pediatrics 2008; 121(4): e731–E737. [DOI] [PubMed] [Google Scholar]
- 52. McCluggage H. Symptoms suffered by life-limited children that cause anxiety to UK children’s hospice staff. Int J Palliat Nurs 2006; 12(6): 254–258. [DOI] [PubMed] [Google Scholar]
- 53. Meyer EC, Burns JP, Griffith JL, et al. Parental perspectives on end-of-life care in the pediatric intensive care unit. Crit Care Med 2002; 30: 226–231. [DOI] [PubMed] [Google Scholar]
- 54. Michelson KN, Koogler T, Sullivan C, et al. Parental views on withdrawing life-sustaining therapies in critically ill children. Arch Pediatr Adolesc Med 2009; 163(11): 986–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Monterosso L, Kristjanson LJ, Aoun S, et al. Supportive and palliative care needs of families of children with life-threatening illnesses in Western Australia: evidence to guide the development of a palliative care service. Palliat Med 2007; 21(8): 689–696. [DOI] [PubMed] [Google Scholar]
- 56. Monterosso L, Kristjanson LJ. Supportive and palliative care needs of families of children who die from cancer: an Australian study. Palliat Med 2008; 22(1): 59–69. [DOI] [PubMed] [Google Scholar]
- 57. Monterosso L, Kristjanson LJ, Phillips MB. The supportive and palliative care needs of Australian families of children who die from cancer. Palliat Med 2009; 23: 526–536. [DOI] [PubMed] [Google Scholar]
- 58. Naicker SN, Richter L, Stein A, et al. Development and pilot evaluation of a home-based palliative care training and support package for young children in southern Africa. BMC Palliat Care 2016; 15: 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Peng N-H, Chen C-H, Huang L-C, et al. The educational needs of neonatal nurses regarding neonatal palliative care. Nurse Educ Today 2013; 33: 1506–1510. [DOI] [PubMed] [Google Scholar]
- 60. Price J, Jordan J, Prior L. A consensus for change: parent and professional perspectives on care for children at the end-of-life. Issues Compr Pediatr Nurs 2013; 36(1–2): 70–87. [DOI] [PubMed] [Google Scholar]
- 61. Price JE. Parents’ experiences of palliative and terminal care for children (patch). PhD Thesis, Queen’s University Belfast, Belfast: 2010. [Google Scholar]
- 62. Pritchard M. Symptoms of dying children in the last week of life. PhD Thesis, The University of Tennessee, Knoxville, TN, 2006. [Google Scholar]
- 63. Pritchard M, Burghen E, Srivastava DK, et al. Cancer-related symptoms most concerning to parents during the last week and last day of their child’s life. Pediatrics 2008; 121(5): e1301–e1309. [DOI] [PubMed] [Google Scholar]
- 64. Rapoport A, Obwanga C, Sirianni G, et al. Not just little adults: palliative care physician attitudes toward pediatric patients. J Palliat Med 2013; 16(6): 675–679. [DOI] [PubMed] [Google Scholar]
- 65. Saad R, Huijer HA, Noureddine S, et al. Bereaved parental evaluation of the quality of a palliative care program in Lebanon. Pediatr Blood Cancer 2011; 57(2): 310–316. [DOI] [PubMed] [Google Scholar]
- 66. Stein A, Forrest GC, Woolley H, et al. Life threatening illness and hospice care. Arch Dis Child 1989; 64: 697–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Szymczak JE, Schall T, Hill DL, et al. Pediatric oncology providers’ perceptions of a palliative care service: the influence of emotional esteem and emotional labor. J Pain Symptom Manage 2018; 55(5): 1260–1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Tamannai M, Kaah J, Mbah G, et al. An evaluation of a palliative care outreach programme for children with Burkitt lymphoma in rural Cameroon. Int J Palliat Nurs 2015; 21(7): 331–337. [DOI] [PubMed] [Google Scholar]
- 69. Theunissen J, Hoogerbrugge P, van Achterberg T, et al. Symptoms in the palliative phase of children with cancer. Pediatr Blood Cancer 2007; 49(2): 160–165. [DOI] [PubMed] [Google Scholar]
- 70. Thienprayoon R, Marks E, Funes M, et al. Perceptions of the pediatric hospice experience among English- and Spanish-speaking families. J Palliat Med 2016; 19(1): 30–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Ullrich CK, Dussel V, Hilden JM, et al. Fatigue in children with cancer at the end of life. J Pain Symptom Manage 2010; 40(4): 483–494. [DOI] [PubMed] [Google Scholar]
- 72. Van der Geest IM, Bindels PJ, Pluijm SM, et al. Home-based palliative care for children with incurable cancer: long-term perspectives of and impact on general practitioners. J Pain Symptom Manage 2017; 53(3): 578–587. [DOI] [PubMed] [Google Scholar]
- 73. Verberne LM, Kars MC, Schouten-van Meeteren AY, et al. Aims and tasks in parental caregiving for children receiving palliative care at home: a qualitative study. Eur J Pediatr 2017; 176(3): 343–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Vickers JL, Carlisle C. Choices and control: parental experiences in pediatric terminal home care. J Pediatr Oncol Nurs 2000; 17(1): 12–21. [DOI] [PubMed] [Google Scholar]
- 75. Vollenbroich R, Borasio GD, Duroux A, et al. Listening to parents: the role of symptom perception in pediatric palliative home care. Palliat Support Care 2016; 14(1): 13–19. [DOI] [PubMed] [Google Scholar]
- 76. Vollenbroich R, Duroux A, Grasser M, et al. Effectiveness of a pediatric palliative home care team as experienced by parents and health care professionals. J Palliat Med 2012; 15(3): 294–300. [DOI] [PubMed] [Google Scholar]
- 77. Wheeler JH. Pediatric nurses’ attitudes, practices, and barriers regarding the care of infants and children living with life-threatening conditions and their families. PhD Thesis, University of Houston, Houston, TX, 2005. [Google Scholar]
- 78. Wolfe J, Grier HE, Klar N, et al. Symptoms and suffering at the end of life in children with cancer. N Engl J Med 2000; 342: 326–333. [DOI] [PubMed] [Google Scholar]
- 79. Yorke DM. Parents’ reflections on the quality of dying and death of their children in the PICU. PhD Thesis, The University of North Carolina at Chapel Hill, Chapel Hill, NC, 2007. [Google Scholar]
- 80. Zaal-Schuller IH, Willems DL, Ewals F, et al. Considering quality of life in end-of-life decisions for severely disabled children. Res Dev Disabil 2018; 73: 67–75. [DOI] [PubMed] [Google Scholar]
- 81. Zelcer S, Cataudella D, Cairney AE, et al. Palliative care of children with brain tumors: a parental perspective. Arch Pediatr Adolesc Med 2010; 164(3): 225–230. [DOI] [PubMed] [Google Scholar]
- 82. Guba EG, Lincoln YS. Naturalistic inquiry. Newbury Park, CA: SAGE, 1985. [Google Scholar]
- 83. Effective Public Health Practice Project. Quality assessment tool for quantitative studies 1998. Hamilton, ON, Canada: Effective Public Health Practice Project. [Google Scholar]
- 84. Hain R, Heckford E, McCulloch R. Paediatric palliative medicine in the UK: past, present, future. Arch Dis Child 2012; 97(4): 381–384. [DOI] [PubMed] [Google Scholar]
- 85. Knapp C, Woodworth L, Wright M, et al. Pediatric palliative care provision around the world: a systematic review. Pediatr Blood Cancer 2011; 57(3): 361–368. [DOI] [PubMed] [Google Scholar]
- 86. Hill DL, Miller VA, Hexem KR, et al. Problems and hopes perceived by mothers, fathers and physicians of children receiving palliative care. Health Expect 2015; 18(5): 1052–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_File_1_Search_Strategy_ for A mixed-methods systematic review and meta-analysis of barriers and facilitators to paediatric symptom management at end of life by Katie Greenfield, Simone Holley, Daniel E Schoth, Emily Harrop, Richard F Howard, Julie Bayliss, Lynda Brook, Satbir S Jassal, Margaret Johnson, Ian Wong and Christina Liossi in Palliative Medicine
Supplemental material, Supplementary_File_2_Meta-analysis_raw_data for A mixed-methods systematic review and meta-analysis of barriers and facilitators to paediatric symptom management at end of life by Katie Greenfield, Simone Holley, Daniel E Schoth, Emily Harrop, Richard F Howard, Julie Bayliss, Lynda Brook, Satbir S Jassal, Margaret Johnson, Ian Wong and Christina Liossi in Palliative Medicine
Supplemental material, Supplementary_File_3_Quality_assessments_of_included_studies for A mixed-methods systematic review and meta-analysis of barriers and facilitators to paediatric symptom management at end of life by Katie Greenfield, Simone Holley, Daniel E Schoth, Emily Harrop, Richard F Howard, Julie Bayliss, Lynda Brook, Satbir S Jassal, Margaret Johnson, Ian Wong and Christina Liossi in Palliative Medicine
Supplemental material, Supplementary_File_4_Assessment_of_confidence_in_themes for A mixed-methods systematic review and meta-analysis of barriers and facilitators to paediatric symptom management at end of life by Katie Greenfield, Simone Holley, Daniel E Schoth, Emily Harrop, Richard F Howard, Julie Bayliss, Lynda Brook, Satbir S Jassal, Margaret Johnson, Ian Wong and Christina Liossi in Palliative Medicine
Supplemental material, Supplementary_File_5_Themes_developed_from_thematic_analysis for A mixed-methods systematic review and meta-analysis of barriers and facilitators to paediatric symptom management at end of life by Katie Greenfield, Simone Holley, Daniel E Schoth, Emily Harrop, Richard F Howard, Julie Bayliss, Lynda Brook, Satbir S Jassal, Margaret Johnson, Ian Wong and Christina Liossi in Palliative Medicine
Supplemental material, Supplementary_File_6_Meta-analysis_individual_forest_plots for A mixed-methods systematic review and meta-analysis of barriers and facilitators to paediatric symptom management at end of life by Katie Greenfield, Simone Holley, Daniel E Schoth, Emily Harrop, Richard F Howard, Julie Bayliss, Lynda Brook, Satbir S Jassal, Margaret Johnson, Ian Wong and Christina Liossi in Palliative Medicine
Supplemental material, Title_and_description_of_supplementary_materials for A mixed-methods systematic review and meta-analysis of barriers and facilitators to paediatric symptom management at end of life by Katie Greenfield, Simone Holley, Daniel E Schoth, Emily Harrop, Richard F Howard, Julie Bayliss, Lynda Brook, Satbir S Jassal, Margaret Johnson, Ian Wong and Christina Liossi in Palliative Medicine