HIGHLIGHTS
-
•
This study reports the mortality risk due to coronavirus disease 2019 (COVID-19) in elderly patients with mental disorders.
-
•
Comparing characteristics between two groups: patients with and without mental disorders suggested that the mental disorder group had more risk factors for COVID-19.
-
•
This study suggests that elderly patients with comorbid conditions and those taking psychiatric medications might be at a higher risk of COVID-19.
Key Words: Elderly, mental disorder, COVID-19, mortality
Abstract
Objective
This study aimed to investigate the different clinical characteristics among elderly coronavirus disease 2019 (COVID-19) patients with and without mental disorders in South Korea and determine if these characteristics have an association with underlying mental disorders causing mortality.
Method
A population-based comparative cohort study was conducted using the national claims database. Individuals aged ≥65 years with confirmed COVID-19 between January 1, 2020 and April 10, 2020 were assessed. The endpoints for evaluating mortality for all participants were death, 21 days after diagnosis, or April 10, 2020. The risk of mortality associated with mental disorders was estimated using Cox hazards regression.
Results
We identified 814 elderly COVID-19 patients (255 [31.3%] with mental disorder and 559 [68.7%] with nonmental disorder). Individuals with mental disorders were found more likely to be older, taking antithrombotic agents, and had diabetes, hypertension, chronic obstructive lung disease, and urinary tract infections than those without mental disorders. After propensity score stratification, our study included 781 patients in each group (236 [30.2%] with mental disorder and 545 [69.8%] with nonmental disorder). The mental disorder group showed higher mortality rates than the nonmental disorder group (12.7% [30/236] versus 6.8% [37/545]). However, compared to patients without mental disorders, the hazard ratio (HR) for mortality in elderly COVID-19 patients with mental disorders was not statistically significant (HR: 1.57, 95%CI: 0.95–2.56).
Conclusion
Although the association between mental disorders in elderly individuals and mortality in COVID-19 is unclear, this study suggests that elderly patients with comorbid conditions and those taking psychiatric medications might be at a higher risk of COVID-19.
INTRODUCTION
The recent outbreak of coronavirus disease 2019 (COVID-19) was declared a global pandemic by the World Health Organization.1 As of September 13, 2020, a total of 28,637,952 cases of laboratory-confirmed COVID-19 have been reported worldwide, of which 917,417 patients have died.2 According to emerging data, COVID-19 is particularly dangerous for elderly individuals,3 who account for the majority of deaths.4 Mental health disorders could potentially worsen the outcomes. Although there is a significant prevalence of mental health disorders in elderly individuals, especially dementia, no studies have investigated the association between mental health disorders and COVID-19 in this patient population.
Rapid transmission of COVID-19 could exacerbate the risk of mental health problems and existing psychiatric symptoms, thereby compromising daily functioning.5 Problems, particularly related to mental health in elderly individuals have been reported in the context of the COVID-19 pandemic.6 Elderly with dementia or cognitive decline have been reported to become more stressed, angry, anxious, agitated, and withdrawn during the COVID-19 outbreak.7 Moreover, COVID-19 further exacerbates the vulnerability of individuals with dementia.8 Retrospective studies during the 2003 severe acute respiratory syndrome epidemic demonstrated that suicide rates in elderly individuals had surged during that time.9 It is, therefore, important to recognize the distinctive impact of COVID-19 on mental health of elderly population.10
In South Korea, the number of elderly people has been steadily increasing, and mental health problems have become common in elderly individuals, with the prevalence of major depressive disorder being estimated at 5.37%.11 More than 100 countries outside of China, reported COVID-19 cases and out of these, South Korea was one of the first ones.12 However, only a few studies have reported the mental health of elderly individuals to be directly impacted by the COVID-19 outbreak.
In the current study, we explored the differences in clinical characteristics between elderly COVID-19 patients with and without mental disorders in South Korea. We also investigated how these characteristics were associated with underlying mental disorders leading to mortality in such patients.
METHODS
Data Source
We used the data provided by the Health Insurance Review and Assessment Service, a South Korean government-affiliated agency that reviews the accuracy of national health insurance claims.13 This database contained demographic information of the patients and the healthcare service information such as diagnoses, prescription medications, procedures, and devices. The Health Insurance Review and Assessment Service data were encoded using the Observational Medical Outcomes Partnership (OMOP) common data model (CDM) version 514 in combination with a de-identification procedure. The OMOP CDM is maintained by the Observational Health Data Sciences and Informatics network and provides tools to facilitate data analysis. The advantage of using the OMOP CDM is that the framework for observational analysis enables rapid analysis, and common analysis codes, along with standardized data, can be applied across multiple center databases without sharing patient-level data.15 , 16 This study was approved by the Ajou University Hospital Institutional Review Board (AJIRB-MED-EXP-20-077), and the requirement for informed consent was waived.
Study Design
The source population consisted of individuals aged ≥65 years with lab-confirmed COVID-19 between January 1, 2020 and April 10, 2020, with the date of diagnosis used as the index date. We excluded patients who were not continuously observed in the database at least 1 year prior to their index date. Patients were classified into two groups: a mental disorder and a nonmental disorder group, depending on whether they received a psychiatric illness diagnosis within 6 months before the index date. Furthermore, an additional analysis was conducted to compare the risk of mortality between the dementia group and the nonmental disorder group (see Supplementary Material for cohort definitions). Patients were followed up until death, 21 days after the index date, or April 10, 2020.
Statistical Analysis
We present baseline demographic and clinical characteristics (medical history, medication use, symptoms, and risk scores) as number (%) for categorical variables and mean (SD) for continuous variables. Differences between the mental disorder and the nonmental disorder group were compared using independent two-sample t-tests (for continuous variables) and χ2 tests (for categorical variables). To minimize group differences in baseline characteristics, we developed a propensity score model for both cohorts with regularized regression. Propensity scores were estimated for the following strategies: 1) without propensity scores and 2) with minimum propensity scores (age, sex, and index month). We determined equipoise using a preference score definition based on patients with a propensity score distribution between 0.25 and 0.75.17 Cox proportional hazard models were used to assess and compare the adjusted and unadjusted hazard ratios (HR) between the mental disorder and non-mental disorder groups. HR were presented at 95% confidence intervals (CI) and p values. All p values less than 0.05 were considered statistically significant. All analyses were performed using the open-source Observational Health Data Sciences and Informatics Cohort Method and survival R package.18
RESULTS
Demographic and Clinical Characteristics
A total of 814 participants were included in the study: 255 patients with and 559 patients without mental disorders, respectively. The demographic and clinical characteristics of the patients are shown in Table 1 . The mental disorder group more likely included older females with diabetes, hypertension, chronic obstructive lung disease, urinary tract infections, and osteoarthritis (Table 1). There was no significant difference between the two groups in their history of neoplasms, but the mental disorder group was more likely to have a history of antithrombotic agent use and medication for acidity related disorders (Table 1). The mental disorder group used antidepressants (31.0%), anxiolytics (31.8%), and antipsychotics (15.7%) significantly more than the non-mental disorder group. Almost half of the patients in the mental disorder group had dementia (51.8%), organic mental disorder (54.5%), depression (45.9%), or anxiety disorder (41.2%). In addition, the mental disorder group was more likely to have symptoms of fever, nausea, and vomiting (Table 1). In risk scores, Charlson comorbidity index, CHA₂DS₂-VASc score, and Diabetes Complications Severity Index were significantly higher in the mental disorder group than in the nonmental disorder group (7.4 versus 5.2, t = 7.78, df = 466.78, p <0.001; 4.9 versus 3.8, t = 8.39, df = 499.76, p <0.001; and 4.4 versus 3.2, t = 6.96, df = 476.65, p <0.001; respectively; Table 1). After propensity score stratification for age and sex, our study lost 33 patients (19 with mental disorder and 14 with nonmental disorder) and finally included 781 patients in each group (236 [30.2%] with mental disorder and 545 [69.8%] with nonmental disorder). Table 2 presents the baseline characteristics for the stratification of propensity scores for the two groups, with prestratification differences in age and sex, but no statistically significant differences after stratification.
TABLE 1.
Baseline Characteristics of Both Groups
| Characteristic | Nonmental Disorder % or Mean (SD) (n = 559) | Mental Disorder % or Mean (SD) (n = 255) | /t(df)a | p Value |
|---|---|---|---|---|
| Age | 73.7 (6.7) | 77.2 (7.5) | 6.48(448) | <0.0001 |
| Age group | 45.07(7) | <0.0001 | ||
| 65–69 | 32.9 | 18.9 | ||
| 70–74 | 24.8 | 18.1 | ||
| 75–79 | 22.3 | 24.1 | ||
| 80–84 | 12.7 | 19.6 | ||
| 85–89 | 4.7 | 14.1 | ||
| 90–94 | 2.5 | 4.1 | ||
| 95–99 | 0.2 | 0.7 | ||
| 100–104 | 0 | 0.4 | ||
| Sex: female | 48 | 57.3 | 5.49(1) | 0.0192 |
| Medical history: General | ||||
| Chronic liver disease | 6.1 | 7.5 | 0.34(1) | 0.5613 |
| Chronic obstructive lung disease | 6.6 | 11.8 | 5.48(1) | 0.0193 |
| Diabetes mellitus | 29.3 | 41.2 | 10.56(1) | 0.0012 |
| Gastroesophageal reflux disease | 29.5 | 34.9 | 2.12(1) | 0.1453 |
| Gastrointestinal hemorrhage | 2.3 | 2.7 | 0.01(1) | 0.9088 |
| Human immunodeficiency virus infection | 0.4 | 0 | 0.04(1) | 0.8468 |
| Hyperlipidemia | 53.7 | 61.2 | 3.71(1) | 0.0541 |
| Hypertensive disorder | 56.7 | 72.5 | 17.93(1) | <0.0001 |
| Lesion of liver | 4.1 | 5.5 | 0.48(1) | 0.4886 |
| Osteoarthritis | 16.6 | 23.9 | 5.59(1) | 0.018 |
| Pneumonia | 32 | 36.1 | 1.12(1) | 0.2896 |
| Psoriasis | 0.4 | 0.8 | 0.07(1) | 0.7896 |
| Renal impairment | 15.4 | 14.9 | 0.01(1) | 0.9421 |
| Rheumatoid arthritis | 2.3 | 4.3 | 1.77(1) | 0.1829 |
| Ulcerative colitis | 0.2 | 0.4 | 0.00(1) | 1.0000 |
| Urinary tract infectious disease | 6.3 | 11.4 | 5.63(1) | 0.0177 |
| Viral hepatitis C | 1.3 | 1.6 | 0.00(1) | 0.9718 |
| Visual system disorder | 42 | 41.2 | 0.02(1) | 0.8769 |
| Medical history: Psychiatric illness | ||||
| Acute stress disorder | 0.8 | |||
| Anxiety disorder | 41.2 | |||
| Bipolar disorder | 14.5 | |||
| Dementia | 51.8 | |||
| Depressive disorder | 45.9 | |||
| Insomnia | 19.2 | |||
| Organic mental disorder | 54.5 | |||
| Panic disorder | 9.4 | |||
| Psychoactive substance dependence | 0.8 | |||
| Psychoactive substance use disorder | 1.6 | |||
| Psychoactive substance-induced organic mental disorder | 1.2 | |||
| Psychosomatic factor in physical condition | 1.6 | |||
| Psychotic disorder | 12.5 | |||
| Schizophrenia | 8.2 | |||
| Medical history: Neoplasms | ||||
| Hematologic neoplasm | 1.6 | 1.2 | 0.03(1) | 0.8709 |
| Malignant lymphoma | 1.1 | 1.2 | 0.00(1) | 1.0000 |
| Malignant neoplasm of anorectum | 19 | 17.3 | 0.24(1) | 0.6274 |
| Malignant neoplastic disease | 0.7 | 0.8 | 0.00(1) | 1.0000 |
| Malignant tumor of breast | 1.4 | 3.1 | 1.83(1) | 0.1757 |
| Malignant tumor of colon | 1.6 | 2.0 | 0.00(1) | 0.9471 |
| Malignant tumor of lung | 1.6 | 1.6 | 0.00(1) | 1.0000 |
| Malignant tumor of urinary bladder | 3.9 | 2.4 | 0.89(1) | 0.3463 |
| Medication use: General | ||||
| Agents acting on the renin-angiotensin system | 31.1 | 36.1 | 1.73(1) | 0.1880 |
| Antibacterials for systemic use | 68.9 | 68.2 | 0.01(1) | 0.9200 |
| Antiinflammatory and antirheumatic products | 47.9 | 49.4 | 0.10(1) | 0.7540 |
| Antineoplastic agents | 2.1 | 2.0 | 0.00(1) | 1.0000 |
| Antipsoriatics | 1.4 | 2.0 | 0.07(1) | 0.7966 |
| Antithrombotic agents | 41 | 51.0 | 6.72(1) | 0.0095 |
| Beta blocking agents | 13.4 | 16.9 | 1.41(1) | 0.2349 |
| Calcium channel blockers | 30.1 | 36.9 | 3.41(1) | 0.0646 |
| Diuretics | 19.7 | 25.9 | 3.62(1) | 0.0571 |
| Drugs for acid related disorders | 57.8 | 71.0 | 12.38(1) | <0.0001 |
| Drugs for obstructive airway diseases | 20.9 | 22.4 | 0.13(1) | 0.7136 |
| Drugs used in diabetes | 24.2 | 23.9 | 0.00(1) | 1.0000 |
| Immunosuppressants | 2.5 | 2.7 | 0.00(1) | 1.0000 |
| Lipid modifying agents | 37 | 43.5 | 2.84(1) | 0.0919 |
| Opioids | 61.2 | 62.4 | 0.06(1) | 0.8094 |
| Medication use: Psychiatry | ||||
| Antidepressants | 3.9 | 31.0 | 115.38(1) | <0.0001 |
| Antipsychotics | 1.8 | 15.7 | 56.28(1) | <0.0001 |
| Psychostimulants, agents used for ADHD and nootropics | 7.0 | 7.8 | 0.09(1) | 0.7669 |
| Anxiolytics | 12.5 | 31.8 | 41.65(1) | <0.0001 |
| Symptoms | ||||
| Nausea and vomiting | 22.5 | 38.0 | 20.38(1) | <0.0001 |
| Fever | 34.7 | 43.1 | 4.97(1) | 0.0258 |
| Cough | 37.9 | 42.7 | 1.51(1) | 0.2195 |
| Muscle pain | 70.3 | 70.2 | 0.00(1) | 1.0000 |
| Risk scores | ||||
| CCI | 5.2 (3.4) | 7.4 (3.7) | 7.78(466.78) | <0.0001 |
| CHA₂DS₂-VASc | 3.8 (1.6) | 4.9 (1.6) | 8.39(499.76) | <0.0001 |
| DCSI | 3.2 (2.1) | 4.4 (2.2) | 6.96(476.65) | <0.0001 |
Notes:Bold type indicates statistical significance. CCI: Charlson comorbidity index; DCSI: Diabetes Complication Severity Index.
χ2 tests & t-tests were performed.
Table 2.
Comparison of Baseline Demographics Before and After Propensity Score Stratification in Both Groups
| Before Stratification |
After Stratification |
|||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | Mental Disorder % (n = 255) | Nonmental Disorder % (n = 559) | p Valuea | Mental Disorder % (n = 236) | Nonmental Disorder % (n = 545) | p Valuea | ||
| Age group | 45.07(7) | <0.0001 | 5.90(7) | 0.5509 | ||||
| 65–69 | 18.9 | 32.9 | 30.0 | 30.7 | ||||
| 70–74 | 18.1 | 24.8 | 19.2 | 19 | ||||
| 75–79 | 24.1 | 22.3 | 21.4 | 25.4 | ||||
| 80–84 | 19.6 | 12.7 | 19.5 | 18.4 | ||||
| 85–89 | 14.1 | 4.7 | 4.5 | 3 | ||||
| 90–94 | 4.1 | 2.5 | 3.9 | 3.4 | ||||
| 95–99 | 0.7 | 0.2 | 1.0 | 0.2 | ||||
| 100–104 | 0.4 | 0 | 0.5 | 0 | ||||
| Sex: female | 57.4 | 48 | 5.49(1) | 0.0192 | 51.7 | 53.9 | 0.21(1) | 0.6498 |
Bold type indicates statistical significance.
χ2 tests was performed.
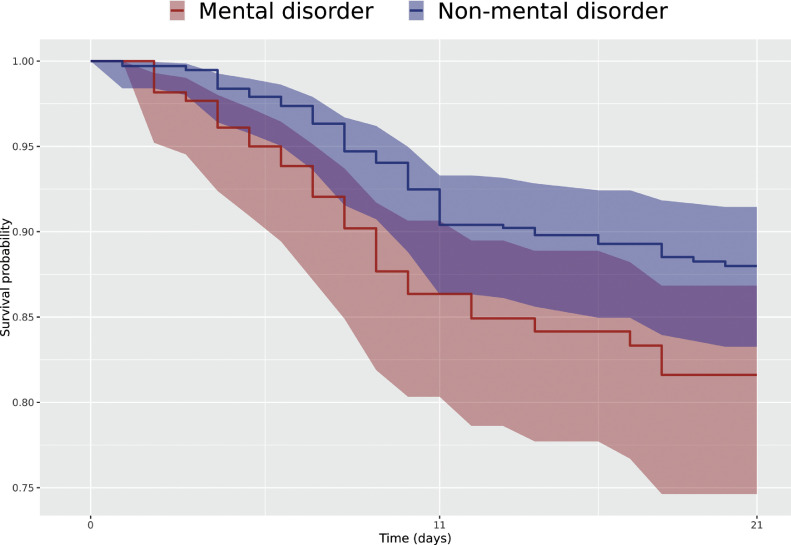
Risk of Mortality
Table 3 summarizes the number of patients, the number of postindex outcomes, person-years, incidence ratio, and HRs observed within 2 groups of interest. The prestratification HR of mortality for the mental disorder group was not statistically significant (HR: 1.38, 95%CI: 0.86–2.21, p = 0.1761). After propensity stratification for age and sex, the poststratification HR of mortality was also not statistically significant (HR: 1.57, 95%CI: 0.95–2.56, p = 0.0733) (Table 3 and Fig. 1 ).
Table 3.
Numbers of Patients, Death Counts, Incidence Rates (per 1,000 Person-Years), and Hazard Ratios for Both Groups
| Analysis | Groups | Subjects | PY | Number of Deaths | IR | Wald χ2 | HR (95%CI) | p Value |
|---|---|---|---|---|---|---|---|---|
| Without PS adjustment | Nonmental disorder | 559 | 17 | 42 | 2,343.49 | 2.29 | 1.00 (reference) | 0.1761 |
| Mental disorder | 255 | 9 | 35 | 3,879.74 | 1.38 (0.86–2.21) | |||
| PS stratification | Nonmental disorder | 545 | 17 | 37 | 2,115.57 | 2.92 | 1.00 (reference) | 0.0733 |
| Mental disorder | 236 | 8 | 30 | 3,631.92 | 1.57 (0.95–2.56) |
Notes: Degrees of freedom for Wald χ2 analyses presented in the table = 1. PY: person-years; IR: incidence ratio (per 1,000 PY); HR: hazard ratio; CI: confidence interval; PS: propensity score.
FIGURE 1.
Kaplan-Meier plot for time-to-event comparison of mortality between individuals with and without mental disorders.
CONCLUSION
To our knowledge, this study is one of the earliest reports providing evidence of the impact of COVID-19 on elderly patients with mental disorders. Our nationwide retrospective analysis shows that elderly COVID-19 patients with mental disorders in South Korea did not have a significantly higher risk of mortality than those without mental disorders and that the risk remained insignificant after adjusting for age and sex. However, co-morbid conditions including diabetes, hypertension, chronic obstructive lung disease, and urinary tract infections, which are known to be associated with mortality in patients with COVID-19 were not adjusted for in our analysis.19 , 20 Also, the use of antithrombotic agents might be not only associated with co-morbid conditions that increase mortality, but also with the reduced risk of morbidity effect in COVID-19.21 The use of antithrombotic agents with these conflicting effects was not adjusted for in our analysis. Considering this, it remains unclear whether mental disorders are associated with mortality in COVID-19.
The mental disorder group showed higher mortality rates than the nonmental disorder group, 12.7% (30 of 236) versus 6.8% (37 of 545). These findings are consistent with those of previous studies on influenza outbreaks in psychogeriatric wards. A mortality rate of 25 % has been reported for elderly patients.22 Similarly, during the first COVID-19 outbreak in South Korea, patients with mental disorders were found to have a 7% mortality rate, higher than the 1% mortality rate observed in the general population.23 However, these studies were observational rather than comparative, and no adjustments were made for various confounding factors.
In the current study, the mental disorder group was significantly older than the group without mental disorders. Increasing death rates from COVID-19 have been associated with older age in a multivariable regression model.24 The current study also found that individuals in the mental disorder group were more likely to have diabetes, hypertension, chronic obstructive lung disease, and urinary tract infections and the use of antithrombotic agents than the nonmental disorder group. Risk scores, including the Charlson comorbidity index, CHA₂DS₂-VASc score, and Diabetes Complications Severity Index were significantly higher in the mental disorder group. Previous research has found that the presence of co-morbidities is a risk factor for poor outcomes in patients with severe acute respiratory syndrome.25 Benzodiazepine use, which was recorded for 31.8% of individuals in the mental disorder group of our study, has been associated with increased influenza-related mortality.26 In addition, the mental disorder group had higher incidences of fever symptoms, nausea, and vomiting. Comparing characteristics between both groups thus suggests that the mental disorder group had more risk factors for COVID-19.
Our findings do not show a clear association between mental disorders in elderly individuals and mortality due to COVID-19. However, the mental disorder group itself showed a higher risk of COVID-19 than the non-mental disorder group. These findings are consistent with the fact that elderly individuals and those with underlying mental disorders and physical illnesses are more vulnerable to COVID-19 than the general population.27 Also, due to the nature of mental disorders, COVID-19 patients with such co-morbid disorders can face barriers in accessing timely health services, which may make treatment less effective.28 Considering that almost half of the patients in our mental disorder group had dementia and organic mental disorders, patients with cognitive decline may also fail to adhere to infection prevention measures, and their reduced activity due to negative symptoms or fear of infection can further impair their physical health and immunity.27 Actually, Brown et al. suggested increased mortality and morbidity in patients with Alzheimer's disease and related dementias.8
Strengths and Limitations
This study has several strengths. First, to the best of our knowledge, this is one of the earliest reports on mortality risk due to COVID-19 in elderly patients with mental disorders. Second, the population-based cohort design based on a nationwide database of individuals' comprehensive medical histories enhances the validity of our findings. This study has, however, some limitations. First, there might be concerns about data quality due to the common limitations of observational database research. Second, although we were able to adjust for age and sex, two important factors affecting death, we did not adjust for confounders such as hypertension and diabetes, which differed between the two cohorts. Also, we did not control for the effect of medications such as antipsychotics, which could increase the risk of metabolic syndrome. Finally, because of the limitations of the national health insurance claims data, laboratory test results were not included in this study.
In conclusion, elderly patients with mental disorders might have a higher risk when infected with COVID-19, due to their age, co-morbid conditions, and psychiatric medications. Our findings, therefore, suggest that more attention might be paid to elderly COVID-19 patients with comorbid conditions and psychiatric medications, regardless of whether they have mental disorders. Further investigations are needed to clarify the associations between mental disorders in elderly individuals and mortality due to COVID-19.
Authors Contribution
Research conception & design: Lee DY, Cho J, Son SJ, Hong CH, Rho HW; Data acquisition: Cho J, Park RW, Kim CS; Data analysis and interpretation: You SC, Lee EY; Statistical analysis: Park BH, Son SJ; Drafting of the manuscript: Lee DY, Cho J; Critical revision of the manuscript: Son SJ, Park BH, Aizenstein H, Andreescu C, Karim H.
Disclosure
The authors thank the healthcare professionals dedicated to treating COVID-19 patients in South Korea, the Ministry of Health and Welfare, and the Health Insurance Review & Assessment Service of Korea for sharing the national health insurance claims data in a prompt manner.
The authors have no disclosures to report.
This research was supported and funded by the Korean Health Industry Development Institute (grant. HI19C0094). This work was supported by the Bio Industrial Strategic Technology Development Program (20001234), funded by the Ministry of Trade, Industry & Energy, and a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health & Welfare, Republic of Korea (grant. HI16C0992).
Footnotes
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.1016/j.jagp.2020.09.016.
Appendix. SUPPLEMENTARY MATERIALS
References
- 1.Yang W, Cao Q, Qin L. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): a multi-center study in Wenzhou city, Zhejiang, China. J Infection. 2020;80:388–393. doi: 10.1016/j.jinf.2020.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Coronavirus disease 2019 (COVID-19) Wkly Epidemiol Updat. 2020:1–2. [Google Scholar]
- 3.Applegate WB, Ouslander JG. COVID-19 presents high risk to older persons. J Am Geriatr Soc. 2020;68:681. doi: 10.1111/jgs.16426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li Q, Guan X, Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang Y, Li W, Zhang Q. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e19. doi: 10.1016/S2215-0366(20)30079-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lloyd-Sherlock P, Ebrahim S, Geffen L. Bearing the brunt of covid-19: older people in low and middle income countries. BMJ. 2020;368:m1052. doi: 10.1136/bmj.m1052. [DOI] [PubMed] [Google Scholar]
- 7.Jiloha R. COVID-19 and mental health. Epidem Int. 2020;5:7–9. [Google Scholar]
- 8.Brown EE, Kumar S, Rajji TK. Anticipating and mitigating the impact of COVID-19 pandemic on Alzheimer's disease and related dementias. Am J Geriatr Psychiatry. 2020;28:712–721. doi: 10.1016/j.jagp.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yip PS, Cheung Y, Chau PH. The impact of epidemic outbreak: the case of severe acute respiratory syndrome (SARS) and suicide among older adults in Hong Kong. Crisis. 2010;31:86–92. doi: 10.1027/0227-5910/a000015. [DOI] [PubMed] [Google Scholar]
- 10.Vahia IV, Blazer DG, Smith GS. COVID-19, mental health and Aging: A need for new knowledge to bridge science and service. Am J Geriatr Psychiatry. 2020;28:695–697. doi: 10.1016/j.jagp.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park JH, Kim KW, Kim M-H. A nationwide survey on the prevalence and risk factors of late life depression in South Korea. J Affect Disord. 2012;138:34–40. doi: 10.1016/j.jad.2011.12.038. [DOI] [PubMed] [Google Scholar]
- 12.Shim E, Tariq A, Choi W. Transmission potential and severity of COVID-19 in South Korea. Int J Infect Dis. 2020;93:339–344. doi: 10.1016/j.ijid.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim J, Yoon S, Kim L-Y. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017;32:718–728. doi: 10.3346/jkms.2017.32.5.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hripcsak G, Duke JD, Shah NH. Observational Health Data Sciences and Informatics (OHDSI): opportunities for observational researchers. Stud Health Technol Inform. 2015;216:574–578. [PMC free article] [PubMed] [Google Scholar]
- 15.Suchard MA, Schuemie MJ, Krumholz HM. Comprehensive comparative effectiveness and safety of first-line antihypertensive drug classes: a systematic, multinational, large-scale analysis. Lancet. 2019;394:1816–1826. doi: 10.1016/S0140-6736(19)32317-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hripcsak G, Suchard MA, Shea S. Comparison of cardiovascular and safety outcomes of chlorthalidone vs hydrochlorothiazide to treat hypertension. JAMA Intern Med. 2020;180:542–551. doi: 10.1001/jamainternmed.2019.7454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walker AM, Patrick AR, Lauer MS. A tool for assessing the feasibility of comparative effectiveness research. Comp Eff Res. 2013;3:11–20. [Google Scholar]
- 18.Cohort Method: New-user cohort method with large scale propensity and outcome models. Martijn J: Observational Health Data Sciences and Informatics (OHDSI) network; 2014. Available at: https://github.com/ohdsi/cohortmethod. Accessed March 25, 2020
- 19.Jin J-M, Bai P, He W. Gender differences in patients with COVID-19: Focus on severity and mortality. Front Public Health. 2020;8:152. doi: 10.3389/fpubh.2020.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheng Y, Luo R, Wang K. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97:829–838. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paranjpe I, Fuster V, Lala A. Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19. J Am Coll Cardiol. 2020;76:122. doi: 10.1016/j.jacc.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sayers G, Igoe D, Carr M. High morbidity and mortality associated with an outbreak of influenza A (H3N2) in a psycho-geriatric facility. Epidemiol Infect. 2013;141:357–365. doi: 10.1017/S0950268812000659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Wide Web Domestic Occurrence Status [KCDC COVID-19 Web site]. 2020. Available at:http://ncov.mohw.go.kr/bdBoardList_Real.do?brdId=1&brdGubun=11&ncvContSeq=&contSeq=&board_id=&gubun=Accessed 21 March, 2020
- 24.Zhou F, Yu T, Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chan K, Zheng J, Mok Y. SARS: prognosis, outcome and sequelae. Respirology. 2003;8:S36–S40. doi: 10.1046/j.1440-1843.2003.00522.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nakafero G, Sanders RD, Nguyen‐Van‐Tam JS. The association between benzodiazepines and influenza‐like illness‐related pneumonia and mortality: a survival analysis using UK Primary Care data. Pharmacoepidemiol Drug Saf. 2016;25:1263–1273. doi: 10.1002/pds.4028. [DOI] [PubMed] [Google Scholar]
- 27.Kim S-W, Su K-P. Using psychoneuroimmunity against COVID-19. Brain Behav Immun. 2020;87:4–5. doi: 10.1016/j.bbi.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yao H, Chen J-H, Xu Y-F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7:e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.