Abstract
In patients with severe or critical Coronavirus disease 2019 (COVID-19) manifestations, a thromboinflammatory syndrome, with diffuse microvascular thrombosis, is increasingly evident as the final step of pro-inflammatory cytokines storm. Actually, no proven effective therapies for novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection exist. Preliminary observations on anticoagulant therapy appear to be associated with better outcomes in moderate and severe COVID-19 patients with signs of coagulopathy and in those requiring mechanical ventilation. The pathophysiology underlying the prothrombotic state elicited by SARS-CoV-2 outlines possible protective mechanisms of antithrombotic therapy (in primis anticoagulants) for this viral illness. The indications for antiplatelet/anticoagulant use (prevention, prophylaxis, therapy) are guided by the clinical context and the COVID-19 severity. We provide a practical approach on antithrombotic therapy management for COVID-19 patients from a multidisciplinary point of view.
Keywords: Anticoagulants, Antiplatelet, Antithrombotic therapy, Coronavirus, COVID-19, Thromboinflammatory syndrome
Highlights
-
•
An endothelial thromboinflammatory syndrome is involved in severe COVID-19 manifestations.
-
•
A pathophysiological rationale (anti-inflammatory and direct antiviral effects) motivates the use of antithrombotic therapy
-
•
Anticoagulant therapy is associated with better outcomes in case of coagulopathy and mechanical ventilation.
-
•
A potential role for antithrombotic therapy in COVID-19 prevention and treatment needs further investigation.
1. Introduction
Coronavirus disease 2019 (COVID-19) is a pandemic infectious disease caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The clinical presentation ranges between mild-to-moderate illness (~80% of cases) to severe (~15%) or critical (~5%) conditions [1,2]. The pathogenic pathways of SARS-CoV2 are not fully understood yet. In patients with disease progression, COVID-19 meets the criteria for acute respiratory distress syndrome (ARDS) with hyperimmune host reaction [2,3]. The mechanism of lung damage can be primarily explained by initial virus-induced direct damage involving both type I and type II pneumocytes [4] and alveolar endothelial cells [5,6], followed by uncontrolled severe inflammatory reaction and microvascular pulmonary thrombosis [7,8]. After managing more than 800 cases of severe pneumonia and more than 120 invasively ventilated patients in our Hospital [9,10], we suggested the pathophysiological hypothesis of the thromboinflammatory syndrome, as recently reported with the acronym MicroCLOTS (microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome) [11]. Although SARS-COV-2 has tropism for ACE2-expressing epithelial cells of the respiratory tract, other co-receptors are probably involved in viral entry, and patients with severe COVID-19 have symptoms of systemic hyperinflammation and endothelial damage with microvascular thrombosis also involving the microvascular bed of the heart [12], kidneys, brain [13] and other organs [14]. As this infection is novel, no proven effective therapies for COVID-19 currently exist, and tremendous efforts are made to identify a specific escalation therapy according to the clinical presentation. SARS-CoV-19 is a betacoronavirus, as are severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). Drugs such as remdesivir, lopinavir-ritonavir, interferon, hydroxychloroquine and corticosteroids, have been used in patients with COVID-19, and before against SARS or MERS, showing controversial efficacy. Actually, medical therapies to prevent the effects of the coagulopathy observed in these patients have been suggested for COVID-19 [15]. Preliminary data on anticoagulant therapy appear to be associated with better outcomes in moderate and severe COVID-19 patients with signs of coagulopathy (elevated D-dimer and fibrinogen and low anti-thrombin levels) [16,17], and in those requiring mechanical ventilation [18].
Such treatment can improve the coagulation dysfunction and also exert anti-inflammatory effects by reducing IL-6 and increasing the relative count of lymphocytes [19].
We highlight the pathophysiology underlying the prothrombotic state elicited by SARS-CoV-2 infection, present the proper studies investigating antithrombotic therapy in several virus infections, and focus on possible protective mechanisms of antithrombotic therapy (in primis anticoagulants) for COVID-19 treatment and need for future studies.
2. Rationale and evidence for potential benefit of anticoagulant therapy
There is evidence that hospitalized COVID-19 patients often suffer from an important infection-related coagulopathy and from elevated risks of microvascular thrombosis [1,14,17,20]. Anticoagulants may have positive effects here, reducing the burden of thrombotic disease and the hyperactivity of coagulation, and may also hold beneficial direct anti-inflammatory effects against sepsis and the development of ARDS. It is known that heparins, including unfractionated heparin (UFH) and low-molecular-weight heparin (LMWH), have several non-anticoagulant properties, and can exert anti-inflammatory effects. Indeed heparins block P-selectin, the cross-talk of platelets and neutrophils [21], inhibit neutrophil response and NETosis [22] and reduce the release of IL-1β, IL-6, E-selectin and ICAM-1 [23,24]. The cytokines and especially the interleukin (IL) family, are known to play an important role in inflammation and have direct effect on the plasma molecules, on erythrocytes and platelets. Hypercoagulability and impaired fibrinolysis are usually the trademarks of several inflammatory conditions. It was reported that IL-1β, IL-6 and IL-8 could cause hypercoagulation, leading to scattered fibrin clots [25]. Patients with severe COVID-19 had higher levels of IL-6, suggesting that the hypercoagulation status of COVID-19 patients may be related to the elevated levels of cytokines [[26], [27], [28]]. In addition to the anti-coagulant and anti-inflammatory properties, other mechanisms can explain the favourable effect of heparins on COVID-19 patients (Fig. 1 ). In fact, they are under investigation for potential use as direct antiviral agents due to their inhibitory effects on pathogen adhesion to cell surfaces. The direct antiviral effect of heparins involves the heparan sulfate, a family of polysaccharides, ubiquitous components of the cell surface and extracellular matrix of all animals [29]. Heparan sulfate has been known to work as the initial point of contact between target cells and several human viruses (i.e., herpesviruses, influenza A virus, hepatitis C virus, human immunodeficiency virus, dengue) [[30], [31], [32], [33], [34]], including the SARS-CoV-2 [35]. Heparins have been shown to efficiently compete with heparan sulfate and by that attenuate viral attachment and cell infection.
Fig. 1.
Mechanisms of anti-inflammatory effects of anticoagulant (left) and antiplatelet (right) therapies in patients with COVID-19.
COX = cyclooxygenase; HSPG = heparan sulfate proteoglycan; MMPs = matrix metalloproteinases; NF-kb = nuclear factor kappa-light-chain-enhancer of activated B cells; SARS-COV-2 = severe acute respiratory syndrome coronavirus 2; TNF = Tumor necrosis factor.
Moreover, SARS-CoV2 is characterized by the presence of several Spike (S) proteins projecting from the virion surface. Each S protein is formed by two subunits (S1 and S2). The S1 subunit features the receptor binding domain that interacts with the main host cell receptor, angiotensin-converting enzyme 2 (ACE2) receptor. Recently, it was reported that the SARS-CoV-2 S1 receptor binding domain is bound by heparin and that, upon binding, a significant structural change is induced, providing forthright evidence for a direct antiviral effect of LMWH in patients with COVID-19 [35].
These mechanisms are not the only ones! The S1-ACE-2 binding is only the first step of infection. The entrance of the SARS-CoV-2 into the human cell needs the cleavage of S1-S2 subunits to expose S2 for adhesion to cell membrane [36,37]. The cellular proteases, cell surface transmembrane protease/serine (TMPRSS) proteases, including cathepsins, factor Xa, furin, trypsin (most of them inhibited by heparin [38]) have been shown to proteolytically process the spike protein. In particular, the factor Xa has been shown to facilitate the activation of SARS-CoV entry into the cells [39]. Therefore, combining this knowledge with mechanisms of action of UFH and LMWH, which are all inhibitors of several proteases like factor Xa, thrombin, furin and cathepsin-L [40], we hypothesize that this can be another direct mechanism of heparins to avoid cellular entrance of SARS-CoV2.
3. Is there a rationale also for antiplatelet therapy?
Until today, unlike anticoagulant therapy, no clinical observations were reported regarding possible protective or therapeutic effects of antiplatelet therapy in COVID-19. Notwithstanding, a pathophysiological rationale for theoretical benefits exists. SARS-CoV-2 infects the endothelial cells using the ACE-2 receptors, which are widely expressed on vascular beds of different organs (kidney, heart, brain, intestine and liver) [12,13]. Post-mortem histology revealed typical lymphocytic endotheliitis as a direct consequence of SARS-CoV-2 infection, which led to diffuse endothelial inflammation and dysfunction [5]. The endothelial dysfunction favours a shift of the haemostatic balance towards procoagulant state, triggering platelet adhesion and aggregation [41] and thereby initiating a thromboinflammatory process (Fig. 1). In several tissue injury models during virus infection (influenza A virus, Dengue, HIV-1, SARS), unsuppressed platelet activation drives a destructive inflammation [42]. Activated platelets release considerable proinflammatory molecules (cytokines, chemokines, high mobility group box 1, metalloproteinases and P-selectin), which enhance neutrophil rolling, adhesion and recruitment and NETosis [43]. In addition, the physical interaction between activated platelets and neutrophils further contributes to neutrophil retention and activation, extracellular matrix proteins degradation and further endothelium activation and thrombin generation [[43], [44], [45], [46], [47], [48], [49]]. Moreover, in a high inflammatory scenario, like in COVID-19, the increase of plasmatic concentration of TNF-alpha could contribute to platelet activation and the expression of a highly thrombotic phenotype of platelets since this stimulus induce the expression of biologically active tissue factor on platelet surface [50].
In animal models, platelet activation promoted influenza A virus pathogenesis by sustaining severe inflammatory response in the respiratory system. Activating protease-activated receptor 4 (a platelet receptor for thrombin that is crucial for platelet activation) exacerbated influenza-induced acute lung injury and death mostly at late postinfection time points. In contrast, treatment with Eptifibatide (specific antagonist of glycoprotein IIb/IIIa), antagonists of protease-activated receptor 4, and Clopidogrel (inhibitors of the adenosine diphosphate receptors P2Y1 and P2Y12) showed protective effects for severe lung injury (inhibition neutrophil recruitment into inflamed lungs) and lethal infections induced by several influenza strains [51]. These results are consistent with other studies showing that aspirin blocks influenza A virus propagation via nuclear factor-kB inhibition [52], and diminishes immune activation in HIV-1 patients [53,54].
Recurrent outbreaks that cause severe infections in humans (influenza A virus subtypes, SARS, MERS etc.) have raised concerns regarding therapeutic strategies available for these pathogens. Current treatments that target viral proteins have a number of disadvantages, including the rapid development of resistant virus variants (especially for RNA virus) [55,56]. Targeting the host rather than the virus with drugs regulating thromboinflammation can be a potential strategy for new therapeutics of recurrent outbreaks. Therefore, there is a rationale behind trying specific therapies to stabilise the endothelium and platelets during viral replication, especially with antiplatelet therapy as well as with anti-inflammatory (corticosteroids) and anti-cytokine drugs (ie. tocilizumab, anakinra, reparixin, canakinumab, interleukin-1β inhibitor, and interferon-β1) [[57], [58], [59]].
During the actual pandemic of COVID-19, in the absence of validate therapies and overwhelming disease, in several hospitals, many physicians have been attempting novel therapies in order to mitigate the disease. The attempt to apply new therapeutic strategies comes from the awareness that it will take a long time before scientific studies can validate specific therapies in the face of an urgent need to save patients' lives. Even the chloroquine and the hydroxychloroquine (antimalarial drugs) were empirically utilized to treat patients mostly with mild or moderate symptoms [60], and have demonstrated in-vitro efficacy against COVID-19 by an as yet not fully understood mechanism [61,62]. Preclinical studies have suggested that hydroxychloroquine has antiplatelet properties possibly through the interaction with arachidonic acid (AA) pathway (downstream to thromboxane A2 production) and the reduction of fibrinogen levels [63,64].
Further explorations are required to determine the degree of platelet activation that is present in COVID-19 patients. In addition, it will be useful to investigate on preventive role of chronic antiplatelet therapy (single or double) on degree of viremia and disease manifestation.
4. Antithrombotic therapy for COVID-19 patients
At the moment, there is no solid scientific evidence on antithrombotic treatment for COVID-19 and further prospective investigations are warranted. Table 1 shows the peculiarities of every anticoagulant or antiplatelet agent regarding the protective role for COVID-19, the clinical setting, and the presence of drug-drug interactions. Antiplatelets share the same benefits deriving from the inhibition of NF-kB and the platelets inactivation. However, P2Y12-inhibitors and cilostazol need caution when used with drugs that interact with CYP3A4. Among the anticoagulants, heparins have less drug-drug interactions and more pathophysiological protective mechanisms if compared to Vitamin K antagonists and direct oral anticoagulants.
Table 1.
Antiplatelet and Anticoagulant agents use for COVID-19.
| Protective mechanism for COVID-19 | Clinical setting | Drug-Drug interactions | |
|---|---|---|---|
| Antiplatelet Agents | |||
| Aspirin |
|
CAD | – |
| Clopidogrel | Stroke | ||
| CAD | Not coadminister or consider dose-reduction with Lopinavir/Ritonavir (−| CYP3A4) | ||
| Ticagrelor |
|
Stroke | |
| Prasugrel | PAD | ||
| Cilostazol | ACS | Not coadminister or consider dose-reduction with Lopinavir/Ritonavir (−| CYP3A4) | |
| ACS | Administer with caution if concomitant use of Lopinavir/Ritonavir (−| CYP3A4) | ||
| PAD | Max dose 50 mg bid if concomitant use of Lopinavir/Ritonavir (−| CYP3A4) | ||
| Anticoagulants | |||
| Heparins (LMWH, UFH) |
|
AF | – |
|
VTE | ||
|
ACS | ||
| Stroke | |||
|
Prosthetic heart valve | ||
| |||
| Vitamin K Antagonists | VTE prophylaxis | AF | Increased dose: Lopinavir/Ritonavir, Ribavirin. |
| –| microvascular thrombosis | VTE | ||
| ACS | |||
| Stroke | Decreased dose: Interferon, Azithromycin, Methylprednisolone. | ||
| Prosthetic heart valve | |||
| Dabigatran | VTE prophylaxis | AF | – |
| –| microvascular thrombosis | VTE | ||
| ACS | |||
| Apixaban | VTE prophylaxis | AF | 50% dose (avoid if initial dose 2.5 mg bid) with Lopinavir/Ritonavir (−| CYP3A4, P-gp) |
| –| microvascular thrombosis | VTE | ||
| ACS | |||
| Rivaroxaban | VTE prophylaxis | AF | Do not coadminister with Lopinavir/Ritonavir (−| CYP3A4, P-gp) |
| –| microvascular thrombosis | VTE | ||
| ACS | |||
| Edoxaban | VTE prophylaxis | AF | Do not coadminister with Lopinavir/Ritonavir (−| CYP3A4, P-gp) |
| –| microvascular thrombosis | VTE | VTE: 30 mg daily in case of concomitant use of Azithromycin (−| P-gp) | |
| ACS | |||
ACS = acute coronary syndrome; AF = atrial fibrillation; CAD = coronary artery disease; HSPG = heparan sulfate proteoglycan; LMWH = low-molecular-weight heparin; MMPs = matrix metalloproteinases; NF-kb = nuclear factor kappa-light-chain-enhancer of activated B cells; PAD = peripheral artery disease; UFH = unfractioned heparin; VTE = venous thromboembolism.
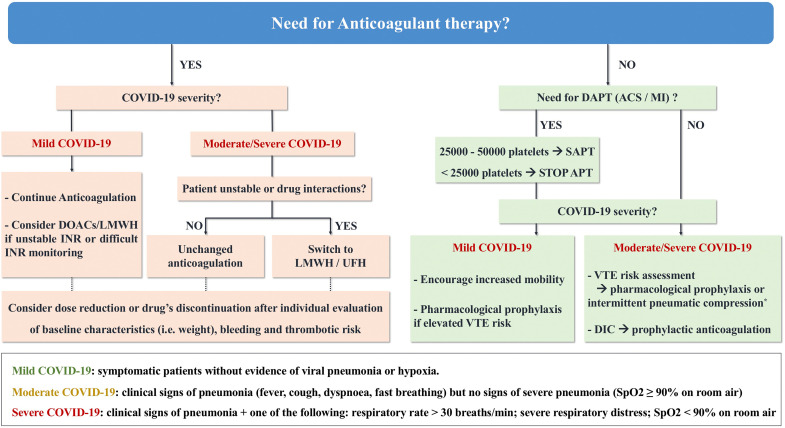
Herein, the authors propose a practical approach for the management of antithrombotic therapy for COVID-19 patients (Fig. 2 ).
Fig. 2.
Algorithm on antithrombotic therapy in patients with COVID-19.
ACS = acute coronary syndrome; APT = antiplatelet therapy; DAPT = dual antiplatelet therapy; DIC = disseminated intravascular coagulation; DOACs = direct oral anticoagulants; INR = international normalized ratio; LMWH = low-molecular-weight heparin; MI = myocardial infarction; SAPT = single antiplatelet therapy; UFH = unfractionated heparin; VTE = venous thromboembolism.
⁎If pharmacological prophylaxis is contraindicated.
Since there are no solid evidences for the prescription of antiplatelets in the absence of other indications, our recommendations are aimed at those who already make use of these drugs [65]. For safety reasons a reduction of the platelet count should guide towards a de-escalation therapy: a single antiplatelet agent should be used when platelets range between 25,000 and 50,000, whereas the antiplatelet therapy should be discontinued when platelets are below 25,000.
Two other decisional cross points of the algorithm are represented by the need for anticoagulation and the severity of COVID-19 infection. In case of no baseline anticoagulation:
-
-
increased mobility should be encouraged or pharmacological prophylaxis (if elevated venous thromboembolism risk) should be prescribed for mild COVID-19 [66];
-
-
VTE risk assessment should precede the adoption of pharmacological prophylaxis or intermittent pneumatic compression in moderate/severe COVID-19 [67]; when these forms are complicated by disseminated intravascular coagulation a prophylactic anticoagulation is needed [16].
When there is a clinical condition (i.e. atrial fibrillation, deep venous thrombosis/pulmonary embolism, prosthetic valve) that represents an indication for anticoagulation:
-
-
in patients with mild COVID-19, the usual therapy should be continued; direct oral anticoagulants or LMWH may be considered in case of unstable INR or difficulties in monitoring this parameter (i.e. quarantine, limited access to peripheral laboratories).
-
-
in moderate/severe COVID-19 manifestations anticoagulation therapy may be switched to LMWH or UFH in the presence of clinical deterioration, haemodynamic instability or drug-drug interactions.
In any case, individual evaluation of baseline characteristics (i.e. weight), bleeding and thrombotic risk should be considered for antithrombotic dose reduction or drug's discontinuation.
5. Conclusions
The rapidly expanding knowledge regarding SARS-CoV-2 virology provides a significant number of potential drug targets. The hypothesis of widespread and progressive endothelial thromboinflammatory syndrome involving patients with more severe COVID-19 manifestations needs additional confirmation. At the same time, the role of antithrombotic therapy (with anticoagulants and/or antiplatelet drugs) demands further evaluation in the context of large observational studies and randomized clinical trials. A theoretical benefit could exist in terms of COVID-19 prevention, favouring mild or asymptomatic manifestations of infectious disease, and in terms of treatment of patients with more severe or critical COVID-19 manifestation. Among all, heparins play a crucial role: they have direct antiviral activity, help prevent venous thromboembolism and have therapeutic use against disseminated intravascular coagulation and pulmonary microvascular thrombosis. However, this strategy needs to be weighed against the risk of bleeding and therefore should be individualized; it could be particularly relevant for patients with cardiovascular disease, which are more “vulnerable” because affected by pre-existing endothelial dysfunction due to hypertension, diabetes and obesity, and at higher risk of adverse outcomes in COVID-19 [68].
Twitter handles
@GodinoCosmo; @AndreaScotti21; @giovannilandoni; @SRAnesthesiaICU; @MyUniSR; @SanRaffaeleMI.
Funding
None.
Disclosures
No conflicts of interest to disclose.
References
- 1.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H., Wu Y., Zhang L., Yu Z., Fang M., Yu T., Wang Y., Pan S., Zou X., Yuan S., Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 2020;2600:1–7. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan W., Ni Z., Hu Y., Liang W., Ou C., He J., Liu L., Shan H., Lei C., Hui D.S.C., Du B., Li L., Zeng G., Yuen K.-Y., Chen R., Tang C., Wang T., Chen P., Xiang J., Li S., Wang J., Liang Z., Peng Y., Wei L., Liu Y., Hu Y., Peng P., Wang J., Liu J., Chen Z., Li G., Zheng Z., Qiu S., Luo J., Ye C., Zhu S., Zhong N. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020:1–13. doi: 10.1056/nejmoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Herold T., Jurinovic V., Arnreich C., Hellmuth J.C., Bergwelt-Baildon M., Klein M., Weinberger T. Level of IL-6 predicts respiratory failure in hospitalized symptomatic COVID-19 patients. MedRxiv. 2020 doi: 10.1101/2020.04.01.20047381. [DOI] [Google Scholar]
- 4.Rockx B., Kuiken T., Herfst S., Bestebroer T., Lamers M.M., Oude Munnink B.B., de Meulder D., van Amerongen G., van den Brand J., Okba N.M.A., Schipper D., van Run P., Leijten L., Sikkema R., Verschoor E., Verstrepen B., Bogers W., Langermans J., Drosten C., Fentener van Vlissingen M., Fouchier R., de Swart R., Koopmans M., Haagmans B.L. Comparative pathogenesis of COVID-19, MERS, and SARS in a nonhuman primate model. Science. 2020;7314 doi: 10.1126/science.abb7314. eabb7314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Varga Z., Flammer A.J., Steiger P., Haberecker M., Andermatt R., Zinkernagel A.S., Mehra M.R., Schuepbach R.A., Ruschitzka F., Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;6736:19–20. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang D., Han Z., Oppenheim J.J. Alarmins and immunity. Immunol. Rev. 2017;280:41–56. doi: 10.1111/imr.12577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giani M., Seminati D., Lucchini A., Foti G., Pagni F. Exuberant plasmocytosis in bronchoalveolar lavage specimen of the first patient requiring extracorporeal membrane oxygenation for SARS-CoV-2 in Europe. J. Thorac. Oncol. 2020 doi: 10.1016/j.jtho.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monteleone G., Sarzi-Puttini P., Ardizzone S. Preventing COVID-19-induced pneumonia with anti-cytokine therapy. Lancet Rheumatol. 2020:483–504. doi: 10.1016/S2665-9913(20)30092-8. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zangrillo A., Beretta L., Silvani P., Colombo S., Scandroglio A.M., Dell’Acqua A., Fominskiy E., Landoni G., Monti G., Azzolini M.L., Monaco F., Oriani A., Belleti A., Sartorelli M., Pallanch O., Saleh O., Sartini C., Nardelli P., Lombardi G., Morselli F., Scquizzato T., Frontera A., Ruggeri A., Scotti R., Assanelli A., Dagna L., Rovere-Querini P., Castagna A., Scarpellini P., Di Napoli D., Ambrosio A., Ciceri F., Tresoldi M. Fast reshaping of intensive care unit facilities in a large metropolitan hospital in Milan, Italy: facing the COVID-19 pandemic emergency. Crit. Care Resusc. 2020;22(2):91–94. doi: 10.51893/2020.2.pov1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zangrillo A., Beretta L., Scandroglio M., Monti G., Fominskiy E., Colombo S., Morselli F., Belletti A., Silvani P., Crivellari M., Monaco F., Azzolini M., Reineke R., Nardelli P., Sartorelli M., Votta C., Ruggeri A., Ciceri F., Cobelli F., Tresoldi M. Characteristics, treatment, outcomes and cause of death of invasively ventilated patients with COVID-19 ARDS in Milan, Italy. Crit. Care Resusc. J. Australas. Acad. Crit. Care Med. 2020;22(3):200–211. doi: 10.1016/S1441-2772(23)00387-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ciceri F., Beretta L., Scandroglio A.M., Colombo S., Landoni G., Ruggeri A., Peccatori J., Angelo A.D., De Cobelli F., Rovere-querini P., Tresoldi M., Dagna L., Zangrillo A. Microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS): an atypical acute respiratory distress syndrome working hypothesis. Crit. Care Resusc. 2020;22(2):95–97. doi: 10.51893/2020.2.pov2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zheng Y.Y., Ma Y.T., Zhang J.Y., Xie X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020 doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mao L., Wang M., Chen S., He Q., Chang J., Hong C., Zhou Y., Wang D., Miao X., Hu Y., Li Y., Jin H., Hu B. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China:a retrospective case series study. SSRN Electron. J. 2020 doi: 10.2139/ssrn.3544840. [DOI] [Google Scholar]
- 14.Tan C.W., Low J.G.H., Wong W.H., Chua Y.Y., Goh S.L., Ng H.J. Critically Ill COVID-19 infected patients exhibit increased clot waveform analysis parameters consistent with hypercoagulability. Am. J. Hematol. 2020 doi: 10.1002/ajh.25822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M., Arbous M.S., Gommers D.A.M.P.J., Kant K.M., Kaptein F.H.J., van Paassen J., Stals M.A.M., Huisman M.V., Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb. Res. 2020 doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tang N., Bai H., Chen X., Gong J., Li D., Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J. Thromb. Haemost. 2020 doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paranjpe I., Fuster V., Lala A., Russak A., Glicksberg B.S., Levin M.A., Charney A.W., Narula J., Fayad Z.A., Bagiella E., Zhao S., Nadkarni G.N. Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19. J. Am. Coll. Cardiol. 2020 doi: 10.1016/j.jacc.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shi C., Wang C., Wang H., Yang C., Cai F.E.I., Zeng F., Cheng F., Liu Y., Zhou T., Deng B.I.N., Li J., Zhang Y.U. The potential of low molecular weight heparin to mitigate cytokine storm in severe covid-19 patients: a retrospective clinical study. MedRxiv. 2020 doi: 10.1101/2020.03.28.20046144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Magro C., Mulvey J.J., Berlin D., Nuovo G., Salvatore S., Harp J., Baxter-Stoltzfus A., Laurence J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl. Res. 2020 doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maugeri N., De Gaetano G., Barbanti M., Donati M.B., Cerletti C. Prevention of platelet-polymorphonuclear leukocyte interactions: new clues to the antithrombotic properties of parnaparin, a low molecular weight heparin. Haematologica. 2005;90:833–839. [PubMed] [Google Scholar]
- 22.Manfredi A.A., Rovere-Querini P., D’Angelo A., Maugeri N. Low molecular weight heparins prevent the induction of autophagy of activated neutrophils and the formation of neutrophil extracellular traps. Pharmacol. Res. 2017;123:146–156. doi: 10.1016/j.phrs.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 23.Qian Y., Xie H., Tian R., Yu K., Wang R. Efficacy of low molecular weight heparin in patients with acute exacerbation of chronic obstructive pulmonary disease receiving ventilatory support. COPD J. Chronic Obstr. Pulm. Dis. 2014;11:171–176. doi: 10.3109/15412555.2013.831062. [DOI] [PubMed] [Google Scholar]
- 24.Li X., Zheng Z., Li X., Ma X. Unfractionated heparin inhibits lipopolysaccharide-induced inflammatory response through blocking p38 MAPK and NF-κB activation on endothelial cell. Cytokine. 2012;60:114–121. doi: 10.1016/j.cyto.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 25.Bester J., Matshailwe C., Pretorius E. Simultaneous presence of hypercoagulation and increased clot lysis time due to IL-1β IL-6 and IL-8. Cytokine. 2018;110:237–242. doi: 10.1016/j.cyto.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 26.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L., Wei Y., Li H., Wu X., Xu J., Tu S., Zhang Y., Chen H., Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Z., Yang B., Li Q., Wen L., Zhang R. Clinical features of 69 cases with Coronavirus disease 2019 in Wuhan, China. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Esko J.D., Lindahl U. Molecular diversity of heparan sulfate. J. Clin. Invest. 2001;108:169–173. doi: 10.1172/jci13530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Trybala E., Liljeqvist J.-A., Svennerholm B., Bergstrom T. Herpes simplex virus types 1 and 2 differ in their interaction with heparan sulfate. J. Virol. 2000;74:9106–9114. doi: 10.1128/jvi.74.19.9106-9114.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vicenzi E., Canducci F., Pinna D., Mancini N., Carletti S., Lazzarin A., Bordignon C., Poli G., Clementi M. Coronaviridae and SARS-associated coronavirus strain HSR1. Emerg. Infect. Dis. 2004;10:413–418. doi: 10.3201/eid1003.030683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vicenzi E., Pagani I., Ghezzi S., Taylor S.L., Rudd T.R., Lima M.A., Skidmore M.A., Yates E.A. Subverting the mechanisms of cell death: Flavivirus manipulation of host cell responses to infection. Biochem. Soc. Trans. 2018;46:609–617. doi: 10.1042/BST20170399. [DOI] [PubMed] [Google Scholar]
- 33.Skidmore M., Kajaste-Rudnitski A., Wells N., Guimond S., Rudd T., Yates E., Vicenzi E. Inhibition of influenza H5N1 invasion by modified heparin derivatives. Medchemcomm. 2015;6:640–646. [Google Scholar]
- 34.Simon A.Y., Sutherland M.R., Pryzdial E.L.G. Dengue virus binding and replication by platelets. Blood. 2015;126:378–385. doi: 10.1182/blood-2014-09-598029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mycroft-West C.J., Su D., Elli S., Guimond S.E., Miller G.J., Turnbull J.E., Yates E.A., Guerrini M., Fernig D.G., de Lima M.A., Skidmore M.A. The 2019 coronavirus (SARS-CoV-2) surface protein (Spike) S1 receptor binding domain undergoes conformational change upon heparin binding. BioRxiv. 2020 doi: 10.1101/2020.02.29.971093. [DOI] [Google Scholar]
- 36.Hirano T., Murakami M. COVID-19: a new virus, but a familiar receptor and cytokine release syndrome. Immunity. 2020:3–5. doi: 10.1016/j.immuni.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Millet J.K., Whittaker G.R. Host cell proteases: critical determinants of coronavirus tropism and pathogenesis. Virus Res. 2015;202:120–134. doi: 10.1016/j.virusres.2014.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Evangelista V., Piccardoni P., Maugeri N., De Gaetano G., Cerletti C. Inhibition by heparin of platelet activation induced by neutrophil-derived cathepsin G. Eur. J. Pharmacol. 1992;216:401–405. doi: 10.1016/0014-2999(92)90437-9. [DOI] [PubMed] [Google Scholar]
- 39.Du L., Kao R.Y., Zhou Y., He Y., Zhao G., Wong C., Jiang S., Yuen K.Y., Jin D.Y., Zheng B.J. Cleavage of spike protein of SARS coronavirus by protease factor Xa is associated with viral infectivity. Biochem. Biophys. Res. Commun. 2007;359:174–179. doi: 10.1016/j.bbrc.2007.05.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Higgins W.J., Fox D.M., Kowalski P.S., Nielsen J.E., Worrall D.M. Heparin enhances serpin inhibition of the cysteine protease cathepsin L. J. Biol. Chem. 2010;285:3722–3729. doi: 10.1074/jbc.M109.037358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yau J.W., Teoh H., Verma S. Endothelial cell control of thrombosis. BMC Cardiovasc. Disord. 2015;15:1–11. doi: 10.1186/s12872-015-0124-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Henn V., Slupsky J.R., Gräfe M., Anagnostopoulos I., Förster R., Müller-Berghaus G., Kroczek R.A. CD40 ligand on activated platelets triggers an inflammatory reaction of endothelial cells. Nature. 1998;391:591–594. doi: 10.1038/35393. [DOI] [PubMed] [Google Scholar]
- 43.Manfredi A.A., Ramirez G.A., Rovere-Querini P., Maugeri N. The neutrophil’s choice: Phagocytose vs make neutrophil extracellular traps. Front. Immunol. 2018;9:288. doi: 10.3389/fimmu.2018.00288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen R.F., Chang J.C., Yeh W.T., Lee C.H., Liu J.W., Eng H.L., Yang K.D. Role of vascular cell adhesion molecules and leukocyte apoptosis in the lymphopenia and thrombocytopenia of patients with severe acute respiratory syndrome (SARS) Microbes Infect. 2006;8:122–127. doi: 10.1016/j.micinf.2005.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hottz E.D., Medeiros-de-Moraes I.M., Vieira-de-Abreu A., de Assis E.F., Vals-de-Souza R., Castro-Faria-Neto H.C., Weyrich A.S., Zimmerman G.A., Bozza F.A., Bozza P.T. Platelet activation and apoptosis modulate monocyte inflammatory responses in dengue. J. Immunol. 2014;193:1864–1872. doi: 10.4049/jimmunol.1400091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Diacovo T.G., Roth S.J., Buccola J.M., Bainton D.F., Springer T.A. Neutrophil rolling, arrest, and transmigration across activated, surface-adherent platelets via sequential action of P-selectin and the β2- integrin CD11b/CD18. Blood. 1996;88:146–157. doi: 10.1182/blood.v88.1.146.bloodjournal881146. [DOI] [PubMed] [Google Scholar]
- 47.Mayadas T.N., Johnson R.C., Rayburn H., Hynes R.O., Wagner D.D. Leukocyte rolling and extravasation are severely compromised in P selectin-deficient mice. Cell. 1993;74:541–554. doi: 10.1016/0092-8674(93)80055-J. [DOI] [PubMed] [Google Scholar]
- 48.Zarbock A., Polanowska-Grabowska R.K., Ley K. Platelet-neutrophil-interactions: linking hemostasis and inflammation. Blood Rev. 2007;21:99–111. doi: 10.1016/j.blre.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 49.Evangelista V., Pamuklar Z., Piccoli A., Manarini S., Dell’Elba G., Pecce R., Martelli N., Federico L., Rojas M., Berton G., Lowell C.A., Totani L., Smyth S.S. Src family kinases mediate neutrophil adhesion to adherent platelets. Blood. 2007;109:2461–2469. doi: 10.1182/blood-2006-06-029082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Manfredi A.A., Baldini M., Camera M., Baldissera E., Brambilla M., Peretti G., Maseri A., Rovere-Querini P., Tremoli E., Sabbadini M.G., Maugeri N. Anti-TNFα agents curb platelet activation in patients with rheumatoid arthritis. Ann. Rheum. Dis. 2016;75:1511–1520. doi: 10.1136/annrheumdis-2015-208442. [DOI] [PubMed] [Google Scholar]
- 51.Lê V.B., Schneider J.G., Boergeling Y., Berri F., Ducatez M., Guerin J.L., Adrian I., Errazuriz-Cerda E., Frasquilho S., Antunes L., Lina B., Bordet J.C., Jandrot-Perrus M., Ludwig S., Riteau B.A. Platelet activation and aggregation promote lung inflammation and influenza virus pathogenesis. Am. J. Respir. Crit. Care Med. 2015;191:804–819. doi: 10.1164/rccm.201406-1031OC. [DOI] [PubMed] [Google Scholar]
- 52.Mazur I., Wurzer W.J., Ehrhardt C., Pleschka S., Puthavathana P., Silberzahn T., Wolff T., Planz O., Ludwig S. Acetylsalicylic acid (ASA) blocks influenza virus propagation via its NF-κB-inhibiting activity. Cell. Microbiol. 2007;9:1683–1694. doi: 10.1111/j.1462-5822.2007.00902.x. [DOI] [PubMed] [Google Scholar]
- 53.O’Brien M., Montenont E., Hu L., Nardi M.A., Valdes V., Merolla M., Gettenberg G., Cavanagh K., Aberg J.A., Bhardwaj N., Berger J.S. Aspirin attenuates platelet activation and immune activation in HIV-1-infected subjects on antiretroviral therapy: a pilot study. J. Acquir. Immune Defic. Syndr. 2013;63:280–288. doi: 10.1097/QAI.0b013e31828a292c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Triant V.A. HIV infection and coronary heart disease: an intersection of epidemics. J. Infect. Dis. 2012;205:355–361. doi: 10.1093/infdis/jis195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Song M.S., Baek Y.H., Kim E.H., Park S.J., Kim S., Lim G.J., Il Kwon H., Pascua P.N.Q., Decano A.G., Lee B.J., Il Kim Y., Webby R.J., Choi Y.K. Increased virulence of neuraminidase inhibitorresistant pandemic H1N1 virus in mice: potential emergence of drug-resistant and virulent variants. Virulence. 2013;4:37–41. doi: 10.4161/viru.25952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Butler J., Hooper K.A., Petrie S., Lee R., Maurer-Stroh S., Reh L., Guarnaccia T., Baas C., Xue L., Vitesnik S., Leang S.K., McVernon J., Kelso A., Barr I.G., McCaw J.M., Bloom J.D., Hurt A.C. Estimating the fitness advantage conferred by permissive neuraminidase mutations in recent oseltamivir-resistant A(H1N1)pdm09 influenza viruses. PLoS Pathog. 2014;10 doi: 10.1371/journal.ppat.1004065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zumla A., Hui D.S., Azhar E.I., Memish Z.A., Maeurer M. Reducing mortality from 2019-nCoV: host-directed therapies should be an option. Lancet. 2020;395:e35–e36. doi: 10.1016/S0140-6736(20)30305-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sallard E., Lescure F.-X., Yazdanpanah Y., Mentre F., Peiffer-Smadja N. Type 1 interferons as a potential treatment against COVID-19. Antivir. Res. 2020;104791 doi: 10.1016/j.antiviral.2020.104791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cavalli G., De Luca G., Campochiaro C., Della-Torre E., Ripa M., Canetti D., Oltolini C., Castiglioni B., Din C. Tassan, Boffini N., Tomelleri A., Farina N., Ruggeri A., Rovere-Querini P., Di Lucca G., Martinenghi S., Scotti R., Tresoldi M., Ciceri F., Landoni G., Zangrillo A., Scarpellini P., Dagna L. Interleukin-1 blockade with high-dose anakinra in patients with COVID-19, acute respiratory distress syndrome, and hyperinflammation: a retrospective cohort study. Lancet Rheumatol. 2020;0 doi: 10.1016/S2665-9913(20)30127-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Piva S., Filippini M., Turla F., Cattaneo S., Margola A., De Fulviis S., Nardiello I., Beretta A., Ferrari L., Trotta R., Erbici G., Focà E., Castelli F., Rasulo F., Lanspa M.J., Latronico N. Clinical presentation and initial management critically ill patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in Brescia, Italy. J. Crit. Care. 2020;58:29–33. doi: 10.1016/j.jcrc.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Touret F., de Lamballerie X. Of chloroquine and COVID-19. Antivir. Res. 2020;177:104762. doi: 10.1016/j.antiviral.2020.104762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yao X., Ye F., Zhang M., Cui C., Huang B., Niu P., Zhao L., Dong E., Song C., Zhan S., Lu R., Li H., Liu D., Clinical D., Liu D., Tan W., Liu D., Clinical D. In vitro antiviral activity and projection of optimized dosing design of hydroxychloroquine for the treatment of severe acute respiratory syndrome main point: hydroxychloroquine was found to be more potent than chloroquine at inhibiting SARS-CoV-2 in vit. Clin. Infect. Dis. 2020;2:1–25. doi: 10.1093/cid/ciaa237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Achuthan S., Ahluwalia J., Shafiq N., Bhalla A., Pareek A., Chandurkar N., Malhotra S. Hydroxychloroquine’s efficacy as an antiplatelet agent study in healthy volunteers: A proof of concept study. J. Cardiovasc. Pharmacol. Ther. 2015;20:174–180. doi: 10.1177/1074248414546324. [DOI] [PubMed] [Google Scholar]
- 64.Janc̈inová V., Nosál R., Petriková M. On the inhibitory effect of chloroquine on blood platelet aggregation. Thromb. Res. 1994;74:495–504. doi: 10.1016/0049-3848(94)90270-4. [DOI] [PubMed] [Google Scholar]
- 65.Valgimigli M., Bueno H., Byrne R.A., Collet J.P., Costa F., Jeppsson A., Kastrati A., Kolh P., Mauri L., Montalescot G., Neumann F.J., Petricevic M., Roffi M., Steg P.G., Zamorano J.L., Levine G.N., Badimon L., Vranckx P., Agewall S., Andreotti F., Antman E., Barbato E., Bassand J.P., Bugiardini R., Cikirikcioglu M., Cuisset T., De Bonis M., Delgado V., Fitzsimons D., Galiè N., Gilard M., Hamm C.W., Ibanez B., James S., Knuuti J., Landmesser U., Leclercq C., Lettino M., Lip G., Piepoli M.F., Pierard L., Schwerzmann M., Sechtem U., Simpson I.A., Uva M.S., Stabile E., Storey R.F., Tendera M., Van De Werf F., Verheugt F., Aboyans V., Windecker S., Coca A., Coman I.M., Dean V., Delgado V., Gaemperli O., Hindricks G., Iung B., Jüni P., Katus H.A., Lancellotti P., McDonagh T., Ponikowski P., Richter Di J., Shlyakhto E., Roithinger F.X., Aliyev F., Stelmashok V., Desmet W., Postadzhiyan A., Georghiou G.P., Motovska Z., Grove E.L., Marandi T., Kiviniemi T., Kedev S., Massberg S., Alexopoulos Di, Kiss R.G., Gudmundsdottir I.J., McFadden E.P., Lev E., De Luca L., Sugraliyev A., Haliti E., Mirrakhimov E., Latkovskis G., Petrauskiene B., Huijnen S., Magri C.J., Cherradi R., Ten Berg J.M., Eritsland J., Budaj A., Aguiar C.T., Duplyakov D., Zavatta M., Antonijevic N.M., Fras Z., Montoliu A.T., Varenhorst C., Tsakiris Di, Addad F., Aydogdu S., Parkhomenko A., Kinnaird T. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS. Eur. Heart J. 2018;39:213–254. doi: 10.1093/eurheartj/ehx419. [DOI] [PubMed] [Google Scholar]
- 66.Thachil J., Tang N., Gando S., Falanga A., Cattaneo M., Levi M., Clark C., Iba T. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J. Thromb. Haemost. 2020;18:1023–1026. doi: 10.1111/jth.14810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ho K.M., Tan J.A. Stratified meta-analysis of intermittent pneumatic compression of the lower limbs to prevent venous thromboembolism in hospitalized patients. Circulation. 2013;128:1003–1020. doi: 10.1161/CIRCULATIONAHA.113.002690. [DOI] [PubMed] [Google Scholar]
- 68.Mehra M.R., Desai S.S., Kuy S., Henry T.D., Patel A.N. Cardiovascular disease, drug therapy, and mortality in covid-19. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2007621. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]