Abstract
Background
Overdose deaths from synthetic opioids (e.g., fentanyl) increased 10-fold in the United States from 2013 to 2018, despite such opioids being rare in illicit drug markets west of the Mississippi River. Public health professionals have feared a “fentanyl breakthrough” in western U.S. drug markets could further accelerate overdose mortality. We evaluated the number and nature of western U.S. fentanyl deaths using the most recent data available.
Methods
We systematically searched jurisdictions west of the Mississippi River for publicly available data on fentanyl-related deaths since 2018, the most recent Centers for Disease Control and Prevention (CDC) statistics. Using mortality data from 2019 and 2020, we identified changes in fentanyl-related mortality rate and proportion of fatal heroin-, stimulant, and prescription pill overdoses involving fentanyl.
Results
Seven jurisdictions had publicly available fentanyl death data through December 2019 or later: Arizona; California; Denver County, CO; Harris County, TX; King County, WA; Los Angeles County, CA; and Dallas-Fort Worth, TX (Denton, Johnson, Parker, and Tarrant counties). All reported increased fentanyl deaths over the study period. Their collective contribution to national synthetic narcotics mortality increased 371 % from 2017 to 2019. Available 2020 data shows a 63 % growth in fentanyl-mortality over 2019. Fentanyl-involvement in heroin, stimulant, and prescription pill deaths has substantially grown.
Discussion
Fentanyl has spread westward, increasing deaths in the short-term and threatening to dramatically worsen the nation’s already severe opioid epidemic in the long-term. Increasing the standard dose of naloxone, expanding Medicaid, improving coverage of addiction treatment, and public health educational campaigns should be prioritized.
Keywords: Fentanyl, Overdose, Surveillance, Mortality, Stimulants, Heroin, Methamphetamine, Cocaine, Synthetic opioids
1. Introduction
Over the past quarter century, the U.S. has experienced a “triple wave” epidemic of opioid addiction and overdose (Ciccarone, 2019). Prescription opioid deaths began rising in the late 1990s. Heroin markets revived and began claiming lives starting around 2007, followed about five years later by surging deaths from fentanyl and other synthetic opioids. Since 2013, deaths involving synthetic opioids – mainly fentanyl and its analogues – have increased ten-fold in the United States, with over 31,000 deaths nationwide in 2018 (Drug Enforcement Administration and Control Division, 2001; Hedegaard et al., 2019; O’Donnell et al., 2018; Spencer et al., 2019; Wilson et al., 2020). Fentanyl and other synthetic opioids present new challenges due to their potency, potential for many analogs, and ease of production and distribution relative to heroin (Pardo et al., 2019).
Remarkably, excess fentanyl mortality has shifted national statistics despite fentanyl-penetration of illicit drug markets being largely confined to the Eastern U.S. (Pardo et al., 2019; Zoorob, 2019). In 2018, the 28 states east of the Mississippi River accounted for 88 % of synthetic opioid overdose deaths (Centers for Disease Control and Prevention, 2020). As recently as summer 2019, drug seizure and mortality data suggested that illicitly manufactured fentanyl remained almost entirely concentrated east of the Mississippi River, raising hopes that this deadly drug would not gain a national foothold (Hedegaard et al., 2019; Pardo et al., 2019; Zoorob, 2019). The spread of deadly drugs across illicit markets is by no means inevitable. Estonia, for example, has had a fentanyl-dominated illicit opioid market for two decades, whereas Finland, just a short ferry ride away, does not (Pardo et al., 2019; Uuskula et al., 2019), even though over 23,000 people make this crossing daily (Silm et al., 2020). Though our analysis focuses on the U.S., there are implications for any region where local drug markets have historically varied despite reasonable mobility between populations. Sometimes cultural norms, market dynamics, and law enforcement manage to constrain a particularly deadly drug to one region. If this were achieved in the U.S., it would lessen the national death toll.
However, research published in 2020 indicates that fentanyl has become nearly ubiquitous in heroin samples (as well as to a lesser extent in cocaine and methamphetamine) gathered just across U.S. borders both in Northwestern Mexico (Fleiz et al., 2020) and Western Canada (British Columbia Coroner’s Association, 2020). News reports of increasing fentanyl overdoses in late 2019 and early 2020 in various U.S. jurisdictions west of the Mississippi River raise further concern (KPIX, 2020; Elyaderani, 2020; Greenson, 2020; Healy, 2019; Hernandez, 2020; Hays Post, 2019), as do reports indicating that the illicit fentanyl trade has been only minimally affected by the novel coronavirus (COVID-19) pandemic (Sanchez and Eldeib, 2020; United Nations Office on Drugs and Crime, 2020). Given how fentanyl has so dramatically worsened the U.S. overdose death rate while only being pervasive in part of the country, its national spread could make the epidemic significantly worse.
As of August 2020, the Centers for Disease Control and Prevention (CDC)’s most current provisional national synthetic opioid overdose mortality estimates cover December 2019 (U.S. Department of Health and Human Services (HHS), 2020), yet the most recent available state- and county-level statistics only reach through December 2018 (Wilson et al., 2020). The substantial lag in availability of state and county-level mortality data hampers surveillance of regional emerging drugs trends and reduces the ability of public health and safety officials to respond rapidly.
To investigate whether fentanyl may have recently penetrated drug markets west of the Mississippi River, we synthesized mortality data from local and state health departments and medical examiner offices. We primarily report changes in population-level rate of fentanyl mortality in the time since the most recently available CDC data. We additionally utilized this data to investigate changes in fentanyl involvement in heroin-, methamphetamine-, cocaine-, and pill- (e.g., prescription opioids, benzodiazepines, 3,4-methylenedioxymethamphetamine (MDMA)) deaths.
2. Methods
We used recent data from national, state, and county sources to investigate potential changes in fentanyl-involved deaths west of the Mississippi. The primary outcome was longitudinal changes in fentanyl-involved deaths per 100,000 population in each jurisdiction. Study data comprised mortality records from Arizona (January 2017 – June 2020); California (January 2017 – December 2019); Denver County, Colorado (January 2018 – March 2020); King County, Washington (January 2017 – June 2020); Harris County, Texas (June 2019 – April 2020); Dallas-Fort Worth metro area, Texas (January 2017 – June 2020). Because Los Angeles County had more recent data available than the rest of California, we present the longitudinal trend for Los Angeles alongside the statewide trend. As a supplemental analysis, we examined county-level fentanyl data through December 2019 for the rest of California’s counties.
The secondary outcome was proportion of deaths related to other drugs (methamphetamine, cocaine, heroin, prescription opioids, benzodiazepines, MDMA) that also involved fentanyl. This was assessed using individual-level death records from San Diego County, California (January 2015 – June 2019); Harris County, Texas (June 2019; Dec 2019 – April 2020); Dallas-Fort Worth metro area, Texas (January 2015 – June 2020); Maricopa County, Arizona (January – March 2020). Los Angeles County, California had both individual (January 2019; December 2019 – April 2020) and aggregate historical (January 2017 – December 2018) records.
Owing to the fragmented nature of immediately available state and local health jurisdiction data, the data collection strategy was as systematic as possible to collect what are ultimately unsystematic results. The tradeoff of results obtained this way is that variation in time frame and level of detail is compensated for by greater immediacy and specificity relative to national data currently available from the CDC (U.S. Department of Health and Human Services (HHS), 2020; Wilson et al., 2020).
2.1. Data sources
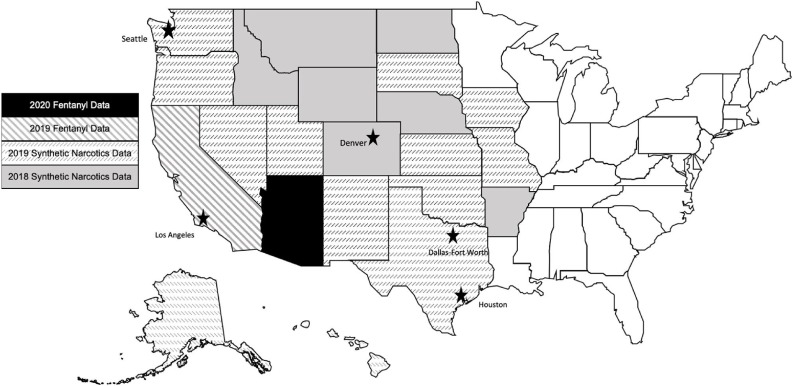
Data were included from the 22 states that are entirely west of the Mississippi River (Alaska, Arkansas, Arizona, California, Colorado, Hawaii, Idaho, Iowa, Kansas, Missouri, Montana, North Dakota, Nebraska, New Mexico, Nevada, Oklahoma, Oregon, South Dakota, Texas, Utah, Washington, Wyoming). For each state, we searched the state and county health department websites for 1) overdose surveillance data that reported fentanyl-involved deaths 2) public medical examiner data. We identified states and counties that reported fentanyl-involved mortality from 2019 or later (Fig. 1 ).
Fig. 1.
Most recently available fentanyl or synthetic opioid mortality data for jurisdictions west of the Mississippi River.
We searched each state’s health department website for a state-level opioid dashboard. Two states – Arizona and California – report fentanyl-involved overdoses through state dashboards. At the time of writing, Arizona reported fatal fentanyl overdoses through June 2020 and California reported state- and county-level fatal fentanyl overdoses through December 2019 (Arizona Department of Health Services, 2020; California Department of Public Health, 2020). For 2019 and earlier, we focus on statewide data for California; however, because county-level data were available we examined it as a supplementary analysis. Local health department websites were identified from the National Association of County Health Officials directory (National Association of County and City Health Officials, 2020) and cross-checked with the state’s public health department website. For each state, we also searched for jurisdictions with publicly available online medical examiner case data.
In addition to the two states, our review of state and local health departments identified six counties and one metro area that provided either a public report of total fentanyl-involved deaths in 2019 or 2020 or individual-level medical examiner data necessary to create such reports. Individual death records were available from Los Angeles County, CA (Los Angeles County Medical Examiner-Coroner, 2020); San Diego County, CA (San Diego County, 2020); Denver County, Co (Denver Department of Public Health and Environment Office of the Medical Examiner, 2020); Harris County, TX (Houston metro area) (Harris County Institute of Forensic Sciences, 2020); Dallas-Fort Worth, TX (comprised of four counties) (Tarrant County, 2020); Maricopa County, AZ (Maricopa County Office of the Medical Examiner, 2020).
San Diego and Dallas-Fort Worth had publicly available exportable individual death records over multiple years, which allowed us to efficiently measure changes in fentanyl-involved deaths over time. Denver County provided an aggregate file for 2019′s drug-related deaths and a count of deaths in January – March 2020. For jurisdictions with publicly available individual death records via online portal (Los Angeles, Harris County), we manually reviewed all medical examiner case records from December 2019 through April 2020, and the earliest available month from 2019 as a comparison for the drug combination analysis. We reviewed 3499 individual records from Los Angeles County and 2298 in Harris County. Because Maricopa County is located within a state that provided statewide monthly counts of fentanyl overdoses but not individual-level drug combinations, we reviewed January-March 2020 (1393 individual records) in order to capture drug combinations. We included death records where fentanyl, fentanyl analogs, methamphetamine, cocaine, amphetamines, heroin, or pills (semi-synthetic opioids, benzodiazepines, 3,4-methylenedioxymethamphetamine) were indicated in any of the cause or contributory fields. We did not distinguish by manner of death (i.e., intentional versus unintentional) owing to challenges of determining intent post-mortem and substantial overlap between these categories (Bohnert and Ilgen, 2019; Gray et al., 2014).
To investigate change in these jurisdictions’ contribution to national synthetic opioid overdose mortality, we extracted multiple cause of death data from 2018 and earlier through the CDC’s Wide-ranging Online Data for Epidemiologic Research multiple cause mortality file (Wilson et al., 2020). We extracted deaths that included International Classification of Diseases 10th Edition Code T40.4, “other synthetic narcotics,” a category that includes fentanyl and its analogues along with tramadol, meperidine and tapentadol, among others, but excludes methadone (World Health Organization, 2004). Provisional national data through December 2019 was obtained through the CDC’s Vital Statistics Rapid Release online portal (U.S. Department of Health and Human Services (HHS), 2020).
2.2. Statistical methods
To compare across locations with widely varying populations, annual rate per 100,000 population in each jurisdiction was calculated based on the number of fentanyl-involved deaths and population estimates from U.S. Census Bureau Quick Facts (U.S. Census Bureau, 2020). When an entire year’s data were not available, the annual rate was imputed based on the average of the year’s available months. We calculated the proportion of synthetic opioid overdose deaths that the reviewed jurisdictions contributed to the national total in 2017 and 2018 using CDC mortality data. We estimated the 2019 contribution using the national total from CDC provisional mortality data. For jurisdictions with 2020 data available, we estimated projected 2020 fentanyl overdose mortality by calculating what the annual rate would be if the same average monthly count was observed the rest of the year.
Finally, to contextualize the longitudinal results nationally, we present two different three-year lagged rates. The first is pooled annual population-adjusted rate across all eastern jurisdictions. This includes the District of Columbia and the 28 states that are entirely or partly (Minnesota & Louisiana) east of the Mississippi River. The second is pooled annual population-adjusted rate of jurisdictions that had the top 10 highest per capita synthetic narcotic mortality in 2018.
2.3. Ethics
This study was designated as exempt from oversight by the Stanford University School of Medicine Institutional Review Board as it involved only publicly available data.
3. Results
3.1. Longitudinal changes in fentanyl-involved mortality
The review of states and counties identified seven jurisdictions – which comprised 17.6 % of the U.S. population in 2019 - with fentanyl death data more recent than the CDC data. Increases in fentanyl-involved mortality since the CDC’s most recently released data were observed in all jurisdictions, which included two states (Arizona, California), one metro area (Dallas-Fort Worth, TX, including Tarrant, Denton, Parker, and Johnson Counties), and three counties: Denver County, CO; Harris County, TX; King County, WA (Table 1 ). Los Angeles is the only California county reporting data from 2020. Hence, longitudinal data from Los Angeles could be reported alongside the statewide data but is not double-counted when calculating the other six jurisdictions’ change in mortality from 2017 to 2019. Only jurisdictions with 2020 data (Arizona and Los Angeles, King, Denver, Harris counties and Dallas-Fort Worth) are included in calculation of preliminary changes from 2019 to 2020.
Table 1.
Number of annual fentanyl-involved deaths by jurisdiction.
| Jurisdiction | Most recent data | 2019 Population | 2017 |
2018 |
2019 |
2020 (Projected) |
Annual change |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Rate/100,000 pop | n | Rate/100,000 pop. | n | Rate/100,000 pop. | n | Rate/100,000 pop. | 2017−18 | 2018−19 | 2019−20 (Projected) | |||
| Arizona (statewide) | Jun. 2020 | 7,278,717 | 239 | 3.4 (3.0, 6.4) | 648 | 9.0 (8.3, 17.4) | 1192 | 16.4 (15.4, 31.8) | 1798 | 24.7 (26.3, 48.3) | 171 % | 84 % | 34 % |
| California (statewide) | Dec. 2019 | 39,512,223 | 431 | 1.1 (1.0, 2.1) | 786 | 2.0 (1.8, 3.8) | 1513 | 3.8 (3.6, 7.5) | -- | -- | 82 % | 92 % | -- |
| Los Angeles County, CA | Apr. 2020 | 10,039,107 | 117 | 1.2 (0.9, 2.1) | 201 | 2.0 (1.7, 3.7) | 390 | 3.9 (3.5, 7.4) | 783 | 7.8 (7.3, 15.1) | 72 % | 94 % | 101 % |
| Denver County, CO | Mar. 2020 | 727,211 | 18 | 1.4* | 17 | 2.4* (1.2, 3.6) | 53 | 7.3 (5.3, 12.6) | 45 | 6.2 (4.4, 10.6) | −6% | 212 % | −15% |
| King County, WA | Jun. 2020 | 2,252,782 | 33 | 1.5 (1.0, 2.4) | 66 | 2.9 (2.2, 5.2) | 112 | 6.0 (4.1, 9.0) | 174 | 7.7 (6.6, 14.3) | 100 % | 70 % | 55 % |
| Harris County, TX | Apr.2020 | 4,713,325 | 59 | 1.3 (0.9, 2.2) | 97 | 2.1 (1.7, 3.7) | 102 | 2.2 (1.7, 3.9) | 153 | 3.2 (2.7, 5.9) | 64 % | 5% | 50 % |
| Dallas/Fort-Worth, TX | Jun. 2020 | 3,308,417 | 19 | 0.6* | 10 | 0.3* | 16 | 0.5* | 80 | 2.4 (1.9, 4.3) | −47% | 60 % | 400 % |
| Pooled (excluding Los Angeles) | -- | 57,792,675 | 799 | 1.4 (1.3, 2.7) | 1624 | 2.8 (2.8, 5.6) | 2988 | 5.2 (5.2, 10.3) | -- | -- | 103 % | 84 % | -- |
| Pooled (excluding California) | -- | 28,319,559 | 485 | 1.7 (1.6., 3.3) | 1039 | 3.7 (3.7, 7.3) | 1865 | 6.6 (6.6., 13.2) | 3033 | 10.7 (10.7, 21.4) | 114 % | 79 % | 63 % |
Rate is calculated based on fewer than 20 cases and is thus unreliable. Projected rates for 2020 and projected change since 2019 are calculated by annualizing available data - i.e., if a jurisdiction had data through March 2020, then the to-date rate is four times the first quarter deaths divided by latest available population estimate at time of writing (July 2019).
In 2017, fentanyl deaths across the six jurisdictions (799) contributed 2.8 % of the national synthetic opioid overdose mortality (28,453). In 2018, the six jurisdictions had 1624 fentanyl deaths, which was 5.2 % of the national count (31,327). In 2019, these jurisdictions had an estimated 2003 fentanyl deaths, which was equivalent to 8.2 % of the provisional national synthetic opioid overdose mortality for 2019 (36,509) (Table 1). Among the six jurisdictions with data from 2019 and 2020, the fentanyl-involved mortality rate had increased 63 % in 2020 over 2019, with steepest increases in the Dallas-Fort Worth area (400 %), and Los Angeles (101 %), King (55 %), and Harris (50 %) Counties.
Among jurisdictions west of the Mississippi River with available data, the highest annual fentanyl-related deaths per 100,000 population were observed in Arizona in January-June 2020 (24.7, 95 % CI 26.3, 48.3); Los Angeles County, CA in January-April 2020 (7.6, 95 % CI 7.1, 14.7); King County, WA in January-March 2020 (7.5, 95 % CI 6.3, 13.8); and Denver County, CO in 2019 (7.3, 95 % CI 5.3, 12.6) (Table 1).
In Texas, rates varied considerably between major cities. Harris County had a fentanyl death rate of 3.7 (95 % CI, 3.2, 6.9) per 100,000 in early 2020. In the Dallas-Fort Worth area, the fentanyl-involved death rate increased substantially from 2019 to the first half of 2020, but remained the lowest among jurisdictions with 2020 data.
Fentanyl deaths in California rose moderately statewide through 2019, but several counties had more dramatic increases. Most notably San Francisco had 189 fentanyl-involved deaths in 2019, for a rate of 21.3, 95 % CI 18.4, 24.5, per 100,000 population. The next highest 2019 rates among California’s 58 counties were Mendocino with 9 deaths (10.2, 95 % CI 4.8, 19.3) and Sonoma with 40 deaths (8.5, 95 % CI 5.7, 10.8) (Supplemental Table 1). Twenty-three California counties reported three or fewer fentanyl deaths between 2017 through 2019, with 10 reporting zero each year. These 23 rural counties included 3.3 % of the state’s 2019 population.
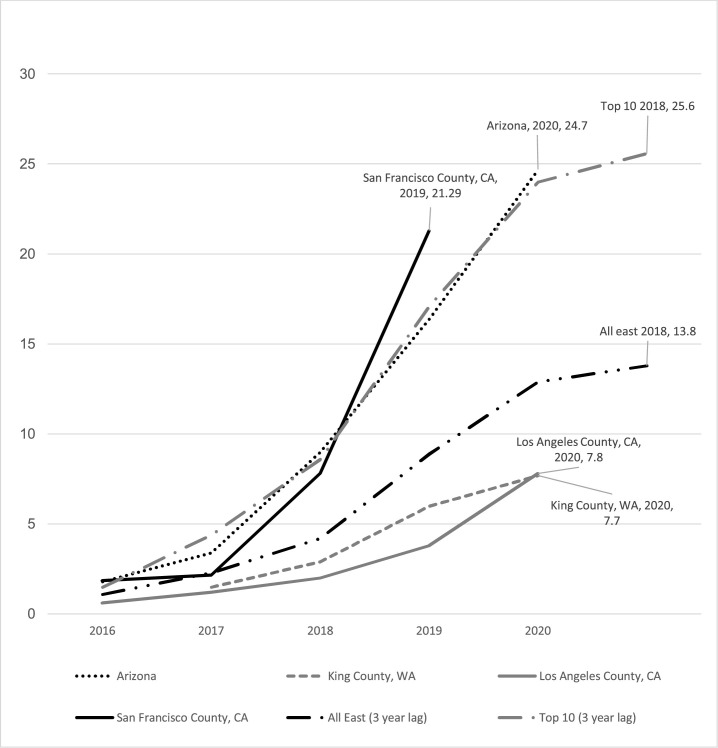
To illustrate the data in the context of the broader U.S. opioid crisis, we plotted lagged mortality rates of eastern U.S. states with high synthetic narcotic mortality alongside jurisdictions in the current study with rising fentanyl-involved mortality (Fig. 2 ). San Francisco from 2016 through 2019 had a more steeply increasing slope than the pooled average for the top 10 synthetic narcotics mortality from 2013 to 2018, and Arizona’s from 2016 through 2020 was on par. Los Angeles and King counties’ curves are rising at a slower pace but are not far off from the lagged curve for all eastern U.S. jurisdictions.
Fig. 2.
“All east” is the three-year lagged pooled synthetic narcotic mortality rate across all states that lie entirely east of the Mississippi River, as well Minnesota, Louisiana, and the District of Columbia. “Top 10″ is the three-year lagged pooled synthetic narcotic mortality across 10 jurisdictions with highest population-adjusted synthetic narcotics mortality rate in 2018 (Delaware, West Virginia, Maryland, New Hampshire, Massachusetts, New Jersey, Ohio, District of Columbia, Connecticut, Rhode Island).
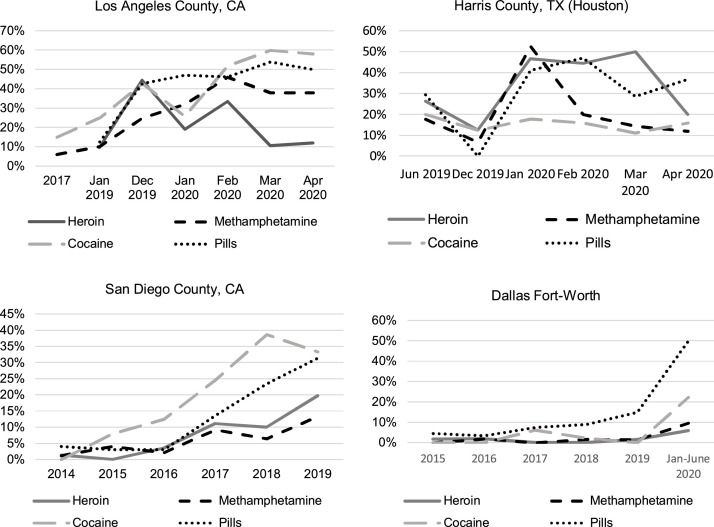
3.2. Individual-level drug combinations
We examined drug combinations using the subset of longitudinal records that were available as individual medical records. San Diego County medical examiner data (available through June 2019, separately from the rest of California’s aggregate data) provided the longest time horizon to examine fentanyl’s co-involvement in deaths related to other substances. Proportion of heroin-related deaths in San Diego County with fentanyl grew from 0% in 2014 to 20 % in the first half of 2019 (Fig. 3 ). Similarly, fentanyl was implicated in no cocaine deaths in 2014, in 39 % of cocaine deaths in 2018, and in 33 % of cocaine deaths in the first half of 2019. Los Angeles County’s 2017 comparison data differ in including toxicology results for all deaths, including those where a substance was present but not a cause of death, whereas the 2019 and 2020 data we collected includes only drugs listed as a cause of death (National Drug Early Warning System, 2018). That said, the same pattern was evident: from 2017 to April 2020, the prevalence of fentanyl grew from 15 % to nearly 60 % of cocaine deaths and from 6% to nearly 40 % of methamphetamine deaths.
Fig. 3.
Fentanyl includes fentanyl and fentanyl analogs. Heroin includes heroin and morphine. Pills include semi-synthetic opioids –i.e., oxycodone, hydrocodone, hydromorphone, oxymorphone – benzodiazepines, 3,4-methylenedioxy-methamphetamine (MDMA)).
In Harris County, the proportion of other drug-related deaths with fentanyl varied over time, whereas in Dallas-Fort Worth the proportions increased but remained lower than the other cities overall, with the percentage of heroin-related deaths also involving fentanyl never surpassing 6%.
From January - March 2020, fentanyl was implicated in 57 % (n = 276) of 485 drug-related deaths in Maricopa, AZ, including 56 % (n = 22) of cocaine-related deaths, 41 % (n = 62) of methamphetamine-related deaths, and 33 % (n = 14) of heroin-related deaths. In 2019 in Denver, CO, 23 % (n = 53) of all drug-related deaths involved fentanyl, as did 12 % of both methamphetamine (n = 9) and cocaine-related (n = 5) deaths. In 2019, only 6% (n = 6) of heroin-related deaths in Denver involved fentanyl.
The review of county health department websites identified reports of counterfeit pressed pills (e.g., oxycodone or alprazolam) containing fentanyl (Alaska Department of Public Safety, 2020; KPIX CBS SF Bay Area, 2020.; Johnson, 2020; Pittenger, 2020; Hays Post, 2019; Santa Clara County Public Health, 2019) as well as reports of heroin laced with fentanyl (Elyaderani, 2020; Montana Department of Public Health and Human Services, 2019). Although alprazolam was implicated in a relatively low number of overdoses, the proportion that also had fentanyl was typically high. Across all cities with data available for 2020, 77 (53 %) of 146 alprazolam deaths also involved fentanyl.
We illustrated fentanyl’s involvement in other fatal overdoses in markets with substantial fentanyl penetration and 2020 data (Maricopa County, AZ; Los Angeles County, CA; and Harris County, TX) (Table 2 ). There were 1270 fatal overdoses that included one or more of the following categories: fentanyl (fentanyl or fentanyl analogs), heroin (heroin or morphine), pills (semi-synthetic opioids, benzodiazepines, or 3,4-methylenedioxymethamphetamine), or stimulants (methamphetamine, cocaine, amphetamines). Deaths were more likely to be related to fentanyl than stimulants, heroin, or pills in Maricopa County; whereas stimulants were the most common category in the other jurisdictions. In all jurisdictions, overlap between fentanyl and the other categories was substantial.
Table 2.
Drug combinations in fatal overdoses in three jurisdictions west of the Mississippi River in 2020, n = 1,270.
| Los Angeles |
Harris |
Maricopa |
Dallas-Fort Worth |
Total |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Jan - Apr 2020 | Jan-Apr 2020 | Jan-Mar 2020 | Jan-Jun 2020 | |||||||
| Fentanyl | 261 | 49% | 68 | 34 % | 239 | 67% | 40 | 32% | 608 | 48% |
| Stimulants | 366 | 69% | 148 | 74% | 166 | 46% | 79 | 63 % | 759 | 60 % |
| Heroin | 93 | 18% | 87 | 43 % | 36 | 10 % | 34 | 27% | 250 | 20 % |
| Pills | 57 | 11 % | 75 | 37% | 50 | 14% | 18 | 14% | 200 | 16 % |
| Combinations | ||||||||||
| Fentanyl only | 89 | 17% | 9 | 4% | 140 | 39 % | 23 | 18% | 261 | 21 % |
| Stimulants only | 174 | 33 % | 94 | 47 % | 76 | 21 % | 47 | 37% | 391 | 31 % |
| Fentanyl & stimulants | 128 | 24% | 9 | 4% | 61 | 17% | 7 | 6% | 205 | 16 % |
| Fentanyl & heroin | 8 | 2% | 3 | 1% | 5 | 1% | 0 | 0% | 16 | 1% |
| Fentanyl & pills | 15 | 3% | 6 | 3% | 18 | 5% | 4 | 3% | 43 | 3% |
| Fentanyl, stimulants, and heroin | 8 | 2% | 6 | 3% | 7 | 2% | 1 | 1% | 22 | 2% |
| Fentanyl, heroin, stimulants, and pills | 2 | 0% | 8 | 4% | 0 | 0% | 1 | 1% | 11 | 1% |
| Fentanyl, stimulants, and pills | 9 | 2% | 6 | 3% | 7 | 2% | 4 | 3% | 26 | 2% |
| Fentanyl, heroin, and pills | 2 | 0% | 4 | 2% | 1 | 0% | 0 | 0% | 7 | 1% |
| Heroin only | 26 | 5% | 2 | 1% | 8 | 2% | 12 | 10 % | 48 | 4% |
| Heroin and stimulants | 39 | 7% | 18 | 9% | 12 | 3% | 18 | 14% | 87 | 7% |
| Pills only | 17 | 3% | 10 | 5% | 18 | 5% | 7 | 6% | 52 | 4% |
| Pills and heroin | 6 | 1% | 5 | 2% | 3 | 1% | 1 | 1% | 15 | 1% |
| Pills and stimulants | 4 | 1% | 7 | 3% | 2 | 1% | 0 | 0% | 13 | 1% |
| Stimulants, heroin, and pills | 2 | 0% | 14 | 7% | 1 | 0% | 1 | 1% | 18 | 1% |
| Total | 529 | 100 % | 201 | 100 % | 359 | 100 % | 126 | 100 % | 1270 | 100 % |
Note: Fatal overdoses that involve one or more of the following are included: fentanyl (fentanyl or fentanyl analogs), heroin (heroin or morphine), pills (semi-synthetic opioids, benzodiazepines, or 3,4-methylenedioxymethamphetamine), or stimulants (methamphetamine, cocaine, amphetamines).
4. Discussion
We report a marked increase in the rate of fentanyl-related deaths west of the Mississippi River in every jurisdiction where such data were available. Moreover, these deaths involved a wide array of other substances. Over the time period included, we observed increases in the proportion of both heroin and stimulant (methamphetamine and cocaine) fatal overdoses that also involved fentanyl. This suggests increasing, worrisome penetration of western U.S. illicit opioid and stimulant markets by fentanyl, alongside rising rates of stimulant overdoses generally (Hoots et al., 2020). These changes are not yet reflected in CDC data and hence have not, to our knowledge, come to policymakers’ attention. Enhancing awareness of fentanyl’s deadly spread is urgent, because it can stimulate a rapid response before this growing public health crisis worsens.
The share of U.S. synthetic opioid overdose mortality attributable to the Western jurisdictions from which we gathered data more than tripled from 2017 to 2019, even as the national synthetic opioid overdose mortality grew. Furthermore, increases from 2019 into early 2020 in Arizona, Los Angeles, Seattle, and Houston suggest that growth may continue. Overlaying the rates with synthetic narcotic mortality rates from states east of the Mississippi suggest that San Francisco in 2019 and Arizona in 2020 are about three years behind on similar trajectories as states with highest synthetic narcotic mortalities in 2018. Meanwhile, Los Angeles and King Counties follow curves similar to that of pooled synthetic narcotic mortality across all eastern states at a three to four-year lag. These comparisons suggest that public health and safety officials have a narrow time window in which to prevent major increases in mortality that would happen if current western state trajectories follow their east coast counterparts.
2018 saw the first drop in overall drug overdose mortality in 40 years, but the spread of fentanyl appears to have already reversed that. Provisional data for 2019 show 50,042 opioid-involved deaths nationally, up from 47,096 in 2018 (U.S. Department of Health and Human Services (HHS), 2020). Of these, 36,509 involve synthetic opioids, an absolute increase of 4984 deaths (16 %) over the previous year. Continuing to monitor the CDC data is important, but they appear at such a lag that public health and safety officials cannot afford to wait until that data are available to take action necessary to prevent more deaths. In July 2020, The New York Times published an analysis of the provisional CDC data and more recent medical examiner data in which they reported fentanyl had spread westward (Katz et al., 2020). The Times analysis, which included state and local mortality data through March 2020, also found increases in overdose mortality in the early days of the COVID-19 pandemic’s growth in the U.S. Our work corroborates both of these key findings, and slightly extends the time horizon. Together our analyses provide evidence that U.S. overdose deaths were rising before the COVID-19 pandemic and have increased even more during the pandemic and resulting social and economic disruption.
The results have several important policy and practice implications. In markets where fentanyl has fully penetrated the heroin supply, fentanyl test strips – which currently provide information only about absence or presence of fentanyl and not relative concentration – may not provide useful information. Instead, the most accurate public health message would be to communicate that any drug sold as heroin is almost certainly largely or entirely fentanyl. In contrast, because of dealer and user market differentiation as well as high-level illicit production dynamics, fentanyl testing strips may still be useful for cocaine and methamphetamine users as the penetration of fentanyl in those drugs may never be total. Similarly, test strips may be useful for pills obtained without a prescription, as fentanyl has been widely but not universally observed in counterfeit pressed pills sold to resemble oxycodone, alprazolam, and other prescription medications.
The increasing prevalence of fentanyl in the form of lookalike pharmaceutical pills appears to be contributing to the deaths observed in the data (Alaska Department of Public Safety, 2020; County of San Luis Obispo Public Health Department, 2019; County of Santa Cruz Health Services Agency, 2019; Hays Post, 2019; Tori et al., 2020). The unfortunate history of scare-mongering in drug prevention messages (e.g., in mass media) now co-exists with a present reality in which "one pill can kill" warnings could be accurate. Public health departments, media, and schools, have a responsibility to broadcast this change in a fashion that neither overstates nor understates the risks posed.
Most of the recommendations to deal with fentanyl have already been made to deal with the prescription opioid and heroin addiction (Humphreys and Pollack, 2020; Office of the Surgeon General, 2016). But all of them now have an added urgency, particularly ensuring that all public and private insurers cover treatment, that Medicaid is expanded in those states that have not done so (e.g., Texas), and that all FDA-approved medications for opioid use disorder are available in specialty and non-specialty health care settings, including correctional facilities. This would also be a propitious time to expand U.S. research on medication options for opioid use disorder with evidence of effectiveness in other countries, such as hydromorphone, slow-release oral morphine, and injectable methadone. Increasing the standard dose of naloxone is also warranted because overdoses involving synthetic opioids like fentanyl and fentanyl analogues often require more naloxone to reverse (Frank and Pollack, 2017; Moe et al., 2020). Efforts to curtail benzodiazepine overprescribing and Internet sales of high-potency benzodiazepines may also be helpful, given that these drugs are often present in opioid overdoses and may be combined with fentanyl in counterfeit pills unbeknownst to users (Blumenberg et al., 2020; Kriikku et al., 2020; Lembke et al., 2018; Papsun et al., 2020; Sun et al., 2017).
The stark differences between immediate and even two-year-old surveillance data point to the need to implement innovative methods to track emerging drug trends. Rapid surveillance using wastewater is one option (Endo et al., 2020). A recently published study used oral swabs taken as part of routine healthcare in Boston, Massachusetts from 2014 through 2019 to identify increasing rates of methamphetamine detection both alone and with fentanyl (Wakeman et al., 2020). As we demonstrate, medical examiner case reports can be a rich source of data, but few are readily available and aggregating them is time-intensive.
4.1. Limitations
Jurisdictional differences in reporting – including time period, outcome (fatal only vs. all fentanyl overdoses), drug category (synthetic opioids generally vs. fentanyl specifically) – make comparisons challenging. Changes within jurisdiction of data availability may add imprecision to results. For example, Los Angeles had 2017 drug combination data for all medical examiner cases with positive toxicology results, even if the cause of death was not drug-related. However, the individual records that comprise the 2019 and 2020 Los Angeles data only contain information on drugs implicated in death.
Using mortality data inherently underestimates the total number of fentanyl overdoses, since non-fatal overdoses are not systematically captured in any jurisdiction. Mortality data could simultaneously overestimate the degree of penetration of fentanyl into the supply of other drugs, if stimulants or heroin that contain fentanyl are more likely to result in a fatal overdose compared to the same drugs without fentanyl. Due to variation in medical examiner investigation time, some records were pending as of this writing: 66 (2%) in Los Angeles County, 29 (1%) in Harris County, and 47 (3%) in Maricopa County. As these cases are resolved, the number of deaths attributed to fentanyl will likely increase. Because jurisdictions with high numbers of fentanyl-involved deaths may be more likely to report aggregate number of fentanyl deaths, selection bias is possible; however, we do not expect this to be a factor in jurisdictions with publicly available individual-level records because these reporting mechanisms are not fentanyl-specific.
Our projections for 2020 where available are simplified; they show what the year-end death rate would be if the rate observed in the available 2020 data continues for the rest of the year. With a few exceptions, the rate of fentanyl deaths in each jurisdiction has grown over time; therefore, this strategy likely underestimates the true death toll. Because Harris County only retains online records for 12 months, we estimated the 2019 rate by taking six times sum of June and December deaths, which could overestimate the 2019 deaths by more heavily weighting later months. However, the counts observed in January through March 2020 show substantial increases that suggest any overestimation would not likely change the interpretation of results.
5. Conclusions
As evidenced by mortality data from as recently as the first half of 2020, fentanyl is not only meaningfully present west of the Mississippi River, but is spreading rapidly in nearly all jurisdictions with timely data. If public health officials do not react strongly and quickly, a significant exacerbation of the U.S. opioid epidemic could follow. Similar vigilance is warranted in other regions where spread of a deadly synthetic opioid is not a foregone conclusion. Lessons learned in this large country with major state-to-state variations in demographics, political, and historical drug-use trends may be particularly relevant in the urgent effort to prevent the opioid overdose crisis from being exported around the world.
Role of funding source
Nothing declared.
CRediT authorship contribution statement
Chelsea L. Shover: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing - original draft. Titilola O. Falasinnu: Data curation, Formal analysis, Methodology, Writing - review & editing. Candice L. Dwyer: Data curation, Project administration, Writing - review & editing. Nayelie Benitez Santos: Data curation, Writing - review & editing. Nicole J. Cunningham: Data curation, Writing - review & editing. Rohan B. Freedman: Data curation, Writing - review & editing. Noel A. Vest: Data curation, Writing - review & editing. Keith Humphreys: Conceptualization, Methodology, Supervision, Writing - review & editing.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgments
We thank Jonathan P. Caulkins and Bryce Pardo for reviewing a draft and providing helpful comments. CLS, TOF, and NV were supported by National Institute on Drug Abuse T32 DA035165. KH was supported by grants from the U.S. Veterans Health Administration. CLS and KH were supported by the Wu Tsai Neurosciences Institute. The funders had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the authors’ employers.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.drugalcdep.2020.108314.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Alaska Department of Public Safety . 2020. Fentanyl Disguised As Oxycodone Pills Found in Alaska. [Google Scholar]
- Arizona Department of Health Services . 2020. Arizona Department of Health Services | Opioid Epidemic. [Google Scholar]
- Blumenberg A., Hughes A., Reckers A., Ellison R., Gerona R. Flualprazolam: report of an outbreak of a new psychoactive substance in adolescents. Pediatrics. 2020;146 doi: 10.1542/peds.2019-2953. [DOI] [PubMed] [Google Scholar]
- Bohnert A.S.B., Ilgen M.A. Understanding links among opioid use, overdose, and suicide. N. Engl. J. Med. 2019;380:71–79. doi: 10.1056/NEJMra1802148. [DOI] [PubMed] [Google Scholar]
- British Columbia Coroner’s Association . 2020. Illicit Drug Toxicity Deaths in BC January 1. 2010 – March 31, 2020. <accessed on Aug. 12, 2020>. [Google Scholar]
- California Department of Public Health . 2020. California Opioid Overdose Surveillance Dashboard [WWW Document]https://skylab.cdph.ca.gov/ODdash/ URL. [Google Scholar]
- Centers for Disease Control and Prevention . 2020. Wide-ranging Online Data for Epidemiologic Research [WWW Document] <accessed on Aug. 9, 2020>. [Google Scholar]
- Ciccarone D. The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int. J. Drug Policy. 2019 doi: 10.1016/j.drugpo.2019.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- County of San Luis Obispo Public Health Department . 2019. Public Health Dept Warns Residents of Alarming Increase in Deaths From Fentanyl Overdose. [Google Scholar]
- County of Santa Cruz Health Services Agency . 2019. Opioid Overdoses from Fake Pills. [Google Scholar]
- Denver Department of Public Health & Environment Office of the Medical Examiner . 2020. Drug-Related Deaths in the City & County of Denver. [Google Scholar]
- Drug Enforcement Administration U., Control Division D. 2001. National Forensic Laboratory Information System: NFLIS-Drug 2019 Midyear Report. [Google Scholar]
- Elyaderani P. KOMO News; 2020. Health Officials Suspect Dangerous Batch of Heroin Circulating Through Oregon. [Google Scholar]
- Endo N., Ghaeli N., Duvallet C., Foppe K., Erickson T.B., Matus M., Chai P.R. Rapid assessment of opioid exposure and treatment in cities through robotic collection and chemical analysis of wastewater. J. Med. Toxicol. 2020;16:195–203. doi: 10.1007/s13181-019-00756-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleiz C., Arredondo J., Chavez A., Pacheco L., Segovia L.A., Villatoro J.A., Cruz S.L., Medina-Mora M.E., de la Fuente J.R. Fentanyl is used in Mexico’s northern border: current challenges for drug health policies. Addiction. 2020;115:778–781. doi: 10.1111/add.14934. [DOI] [PubMed] [Google Scholar]
- Frank R.G., Pollack H.A. Addressing the fentanyl threat to public health. N. Engl. J. Med. 2017;376:605–607. doi: 10.1056/NEJMp1615145. [DOI] [PubMed] [Google Scholar]
- Gray D., Coon H., McGlade E., Callor W.B., Byrd J., Viskochil J., Bakian A., Yurgelun-Todd D., Grey T., McMahon W.M. Comparative analysis of suicide, accidental, and undetermined cause of death classification. Suicide Life. Threat. Behav. 2014;44:304–316. doi: 10.1111/sltb.12079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenson T. Third Wave: fentanyl washed into Humboldt County in 2019 with deadly consequences. North Coast J. 2020 [Google Scholar]
- Harris County Institute of Forensic Sciences . 2020. Case Status. [WWW Document]https://ifs.harriscountytx.gov/Pages/CaseStatus.aspx URL. [Google Scholar]
- Hays Post . 2019. Kan. Sheriff Issues Warning on Fentanyl-laced Oxycodone. [Google Scholar]
- Healy M. Los Angeles Times; 2019. New Drug Overdose Data Capture Earliest Days of Fentanyl’s Deadly Westward Expansion. [Google Scholar]
- Hedegaard H., Bastian B., Trinidad J., Spencer M., Warner M. 2019. Regional Differences in the Drugs Most Frequently Involved in Drug Overdose Deaths: United States; p. 2017. [PubMed] [Google Scholar]
- Hernandez E.L. 2020. Fatal Drug Overdoses Involving Fentanyl Tripled in Denver Between 2018 and 2019. Denverite. [Google Scholar]
- Hoots B., Vivolo-Kantor A., Seth P. The rise in non-fatal and fatal overdoses involving stimulants with and without opioids in the United States. Addiction. 2020;115:946–958. doi: 10.1111/add.14878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys K., Pollack H.A. In: The Palgrave Handbook of American Mental Health Policy. Goldman H.H., Frank R.G., Morrissey J.P., editors. Springer International Publishing, Cham; 2020. How should the United States respond to the opioid addiction and overdose epidemic? pp. 259–295. [DOI] [Google Scholar]
- Johnson K. KVRR Local News; 2020. Grand Forks Police Investigate Drug Death. [Google Scholar]
- Katz J., Goodnough A., Sanger-Katz M. New York Times; 2020. In Shadow of Pandemic, U.S. Drug Overdose Deaths Resurge to Record.https://www.nytimes.com/interactive/2020/07/15/upshot/drug-overdose-deaths.html [WWW Document] URL.<accessed on Sept 6, 2020>. [Google Scholar]
- KPIX CBS SF Bay Area . 2020. Fentanyl Overdose Calls Spiking in Santa Clara County; Murder Charges in Teen’s Death – CBS San Francisco. [Google Scholar]
- Kriikku P., Rasanen I., Ojanperä I., Thelander G., Kronstrand R., Vikingsson S. Femoral blood concentrations of flualprazolam in 33 postmortem cases. Forensic Sci. Int. 2020;307 doi: 10.1016/j.forsciint.2019.110101. [DOI] [PubMed] [Google Scholar]
- Lembke A., Papac J., Humphreys K. Our other prescription drug problem. N. Engl. J. Med. 2018;378:693–695. doi: 10.1056/NEJMp1715050. [DOI] [PubMed] [Google Scholar]
- Los Angeles County Medical Examiner-Coroner . 2020. Case Search [WWW Document]https://mec.lacounty.gov/case-search/ URL <accessed on Aug. 9, 2020>. [Google Scholar]
- Maricopa County Office of the Medical Examiner . 2020. Maricopa County, AZ OME CASE STATUS [WWW Document]https://omecasestatus.maricopa.gov/ URL <accessed on Aug. 9, 2020>. [Google Scholar]
- Moe J., Godwin J., Purssell R., O’Sullivan F., Hau J.P., Purssell E., Curran J., Doyle-Waters M.M., Brasher P.M.A., Buxton J.A., Hohl C.M. Naloxone dosing in the era of ultra-potent opioid overdoses: a systematic review. CJEM. 2020;22:178–186. doi: 10.1017/cem.2019.471. [DOI] [PubMed] [Google Scholar]
- Montana Department of Public Health & Human Services . 2019. Increase in Fentanyl-related Overdose and Fatalities. [Google Scholar]
- National Association of County and City Health Officials . 2020. Directory of Local Health Departments - NACCHO [WWW Document]https://www.naccho.org/membership/lhd-directory URL <accessed on May 1, 2020>. [Google Scholar]
- O’Donnell J., Gladden R.M., Mattson C.L., Kariisa M. Notes from the Field: overdose Deaths with Carfentanil and other fentanyl analogs detected — 10 states, July 2016–june 2017. MMWR Morb. Mortal. Wkly. Rep. 2018 doi: 10.15585/mmwr.mm6727a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the Surgeon General . HHS; Washington, D.C: 2016. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. [PubMed] [Google Scholar]
- Papsun D.M., Krotulski A.J., Homan J., Temporal K.D.H., Logan B.K. Flualprazolam blood concentrations in 197 forensic investigation cases. J. Anal. Toxicol. 2020 doi: 10.1093/jat/bkaa070. [DOI] [PubMed] [Google Scholar]
- Pardo B., Taylor J., Caulkins J.P., Kilmer B., Reuter P., Stein B.D. RAND Corporation; Santa Monica, CA: 2019. The Future of Fentanyl and Other Synthetic Opioids. [Google Scholar]
- Pittenger T. KSAL; 2020. Kansans Urged to Beware of Fentanyl. [Google Scholar]
- San Diego County . 2020. Medical Examiner Cases [WWW Document]https://data.sandiegocounty.gov/Safety/Medical-Examiner-Cases/jkvb-n4p7 URL <accessed on Jun 29, 2020>. [Google Scholar]
- Santa Clara County Public Health . 2019. Fake Pills That Contain Deadly Fentanyl. [Google Scholar]
- Silm S., Jauhiainen J.S., Raun J., Tiru M. Temporary population mobilities between Estonia and Finland based on mobile phone data and the emergence of a cross-border region. Eur. Plan. Stud. 2020 doi: 10.1080/09654313.2020.1774514. [DOI] [Google Scholar]
- Spencer M.R., Warner M., Bastian B.A., Trinidad J.P., Hedegaard H. Drug overdose deaths involving fentanyl, 2011-2016. Natl. Vital Stat. Rep. 2019 [PubMed] [Google Scholar]
- Sun E.C., Dixit A., Humphreys K., Darnall B.D., Baker L.C., Mackey S. Association between concurrent use of prescription opioids and benzodiazepines and overdose: retrospective analysis. BMJ. 2017;356:j760. doi: 10.1136/bmj.j760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarrant County . 2020. Medical Examiner’s Case Records [WWW Document]https://mepublic.tarrantcounty.com/ URL <accessed on Aug. 9, 2020>. [Google Scholar]
- Tori M.E., Larochelle M.R., Naimi T.S. Alcohol or benzodiazepine Co-involvement with opioid overdose deaths in the United States, 1999-2017. JAMA Netw. Open. 2020;3:e202361. doi: 10.1001/jamanetworkopen.2020.2361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau . 2020. Quick Facts [WWW Document]https://www.census.gov/quickfacts/ URL <accessed on Aug. 9, 2020>. [Google Scholar]
- U.S. Department of Health and Human Services (HHS) 2020. VSRR Provisional Drug Overdose Death Counts. <accessed on Aug. 9, 2020>. [Google Scholar]
- Uuskula A., Jarlais D.D., Vorobjov S. The fentanyl epidemic in Estonia: opportunities for a comprehensive public health response. Lancet Psychiatry. 2019;6:985. doi: 10.1016/s2215-0366(19)30436-5. [DOI] [PubMed] [Google Scholar]
- Wakeman S., Flood J., Ciccarone D. Rise in presence of methamphetamine in oral fluid toxicology tests among outpatients in a large healthcare setting in the northeast. J. Addict. Med. Publish Ah. 2020 doi: 10.1097/adm.0000000000000695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson N., Kariisa M., Seth P., Smith Hth, Davis N.L. Drug and opioid-involved overdose deaths - United States, 2017-2018. MMWR Morb. Mortal. Wkly. Rep. 2020;69:290–297. doi: 10.15585/mmwr.mm6911a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2004. ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth Revision. [Google Scholar]
- Zoorob M. Fentanyl shock: the changing geography of overdose in the United States. Int. J. Drug Policy. 2019;70:40–46. doi: 10.1016/j.drugpo.2019.04.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.