Abstract
The new coronavirus SARS-CoV-2 has infected more than 14 million people worldwide so far. Brazil is currently the second leading country in number of cases of COVID-19, while São Paulo state accounts for 20% of total confirmed cases in Brazil. The aim of this study was to assess environmental and social factors influencing the spread of SARS-CoV-2 in the expanded metropolitan area of São Paulo, Brazil. Firstly, a spatial analysis was conducted to provide insights into the spread of COVID-19 within the expanded metropolitan area. Moreover, Spearman correlation test and sensitivity analysis were performed to assess social indicators and environmental conditions which possibly influence the incidence of COVID-19. Our results reveal that the spread of COVID-19 from the capital city São Paulo—its epicenter in Brazil—is directly associated with the availability of highways within the expanded metropolitan area of São Paulo. As for social aspects, COVID-19 infection rate was found to be both positively correlated with population density, and negatively correlated with social isolation rate, hence indicating that social distancing has been effective in reducing the COVID-19 transmission. Finally, COVID-19 infection rate was found to be inversely correlated with both temperature and UV radiation. Together with recent literature our study suggests that the UV radiation provided by sunlight might contribute to depletion of SARS-CoV-2 infectivity.
Keywords: Cumulative confirmed cases, Infection rate, Spatial analysis, Social indicators, Solar UV radiation, Temperature, Weather conditions
Introduction
The new coronavirus SARS-CoV-2 has infected more than 14 million people worldwide so far (Worldometers 2020), the reason why the World Health Organization (WHO) has described the situation as a pandemic (WHO 2020).
Up to date (July 17, 2020), there are 2,046,328 confirmed cases in all regions of Brazil (Brazil 2020), which is currently the second leading country in number of cases (Worldometers 2020). São Paulo state accounts for 20% of cumulative confirmed cases in Brazil, with 407,415 confirmed cases, being currently the most affected state worldwide (John Hopkins 2020), while São Paulo-SP is the city with most confirmed cases (163,624) in Brazil (SEADE 2020a). São Paulo is the largest city in Latin America, with a population of 12,252,023 people, and an expanded metropolitan area with 33,652,991 people (SEADE 2020b). On March 24, 2020, partial lockdown was ordered by São Paulo state government (São Paulo 2020a), being social isolation monitored since then (São Paulo 2020b).
One recent review has addressed the role of climate change in the emergence and re-emergence of infectious diseases worldwide, indicating that temperature is an important environmental condition determining the success of infectious agents (El-Sayed and Kamel 2020). Furthermore, several studies have investigated the impact of weather on the COVID-19 transmission, with special attention to temperature and humidity (Harmooshi et al. 2020; Liu et al. 2020; Qi et al. 2020; Şahin 2020), indicating that temperature is inversely related to COVID-19 incidence. Moreover, each 1 °C increase in temperature has been associated with decreases in daily new cases at different extents (Prata et al. 2020; Wu et al. 2020).
A few investigations have also considered social aspects potentially associated with the spread of COVID-19, such as population density, metropolitan population, intra-provincial traffic, and national lockdown, indicating that the social distancing measures have been successful in reducing new cases (Ahmadi et al. 2020; Hamidi et al. 2020; Tobías 2020).
The aim of this study was to assess environmental and social factors influencing the spread of SARS-CoV-2 in the expanded metropolitan area of São Paulo, Brazil.
Materials and methods
Seeking to understand the mechanisms of SARS-CoV-2 spread in the most affected area of Brazil, COVID-19 infection rate from March 24, 2020, to July 06, 2020, were analyzed. The infection rate (Eq. 1) defined by Ahmadi et al. (2020) was used to assess the COVID-19 spread speed.
| 1 |
Firstly, a spatial analysis was conducted using the cumulative confirmed cases of COVID-19 to provide insights into the spread of COVID-19 within the expanded metropolitan area over time. Moreover, cities in the expanded metropolitan area of São Paulo with more than 500 confirmed cases of COVID-19 were selected for statistical analyses (Spearman correlation test and sensitivity analysis) of the following social indicators which possibly influence the incidence of COVID-19 (infection rates): population (people), population density (people∙km−2), Municipal Human Development Index (MHDI), gross domestic product (R$ per capita), and average income (R$ per capita). Therefore, 59 cities were included in this analysis, accounting for a total of 29,389,922 people.
Secondly, the following criteria were used for selecting cities for statistical analyses (Spearman correlation test and sensitivity analysis) of both meteorological conditions and social isolation rate: (i) cities with more than 2000 confirmed cases of COVID-19; (ii) within the expanded metropolitan area of São Paulo; and (iii) with available meteorological data. Thus, a total of 10 cities were analyzed considering the infection rates, corresponding to a population of 18,033,600 people (Table 1).
Table 1.
Cities selected for statistical analyses of both meteorological conditions and social isolation rate, population, and cumulative confirmed cases of COVID-19 as of July 06, 2020
| City | Population | Cumulative confirmed cases | Cases per 1000 people |
|---|---|---|---|
| São Paulo | 12,252,023 | 140,231 | 11.81 |
| Campinas | 1,204,073 | 9624 | 8.19 |
| São Bernardo do Campo | 838,936 | 9174 | 11.30 |
| Guarulhos | 1,379,182 | 7747 | 5.73 |
| Sorocaba | 679,378 | 5318 | 8.07 |
| Jundiaí | 418,492 | 4236 | 10.41 |
| São José dos Campos | 721,944 | 3547 | 4.99 |
| Carapicuíba | 400,927 | 2745 | 6.96 |
| Piracicaba | 404,142 | 2643 | 6.78 |
| Barueri | 274,182 | 2324 | 8.79 |
| Total | 18,033,600 | 187,589 | 10,40 |
Daily data made available by the São Paulo State Environmental Agency (CETESB 2020) were used to assess the meteorological conditions of temperature (T, °C), relative humidity (RH, %), wind speed (WS, m s−1), and ultraviolet radiation (UV, W m−2) from March 18, 2020, to July 06, 2020. Social isolation rates (SIR, %) published on a daily basis by the São Paulo State Social Isolation Intelligent Monitoring System (São Paulo 2020b) were used to analyze the effectiveness of a social distancing measure for reducing the transmission of COVID-19. For each city, the Spearman correlation test at 95% significance level (α = 0.05) was used to assess correlation between infection rate and meteorological parameters or social isolation rate.
The partial correlation coefficient (PCC) method was applied to perform a sensitivity analysis using the infection rate as the dependent variable and meteorological conditions or social indicators as the independent variables. Data were normalized using the mean value and the standard deviation (Eq. 2), according to Zhu et al. (2020). The forward, stepwise, and backward procedures (Mollalo et al. 2020) were conducted to select the best linear regression model and to determine the regression coefficients and significant variables (p value < 0.15).
| 2 |
where X is the normalized value; x is the raw value; μ is the mean value; and σ is the standard deviation.
Results and discussion
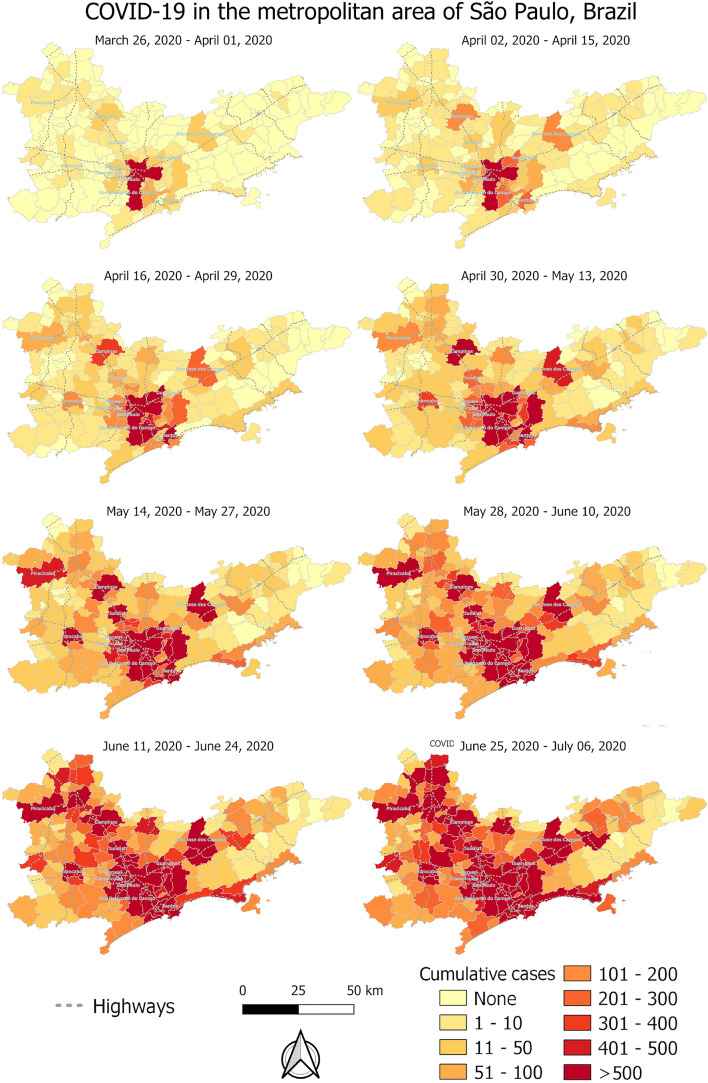
The analysis of cumulative confirmed cases in a spatial-dependent manner shows that initially (March 26, 2020), the COVID-19 transmission was mainly in the capital city São Paulo. Over the weeks, increasing transmission has been occurring in cities surrounded by highways, and by July 06, 2020, COVID-19 has spread all over the expanded metropolitan area of São Paulo (Fig. 1). Therefore, using spatial analysis, we have observed that the spread of COVID-19 from the capital city São Paulo—its epicenter in Brazil—is directly associated with the availability of highways within the expanded metropolitan area of São Paulo. Our findings are consistent with recent literature, as Hamidi et al. (2020) have reported metropolitan population as one of the most significant predictors of infection rates in the USA, due to shared transportation and interaction of people in metropolitan areas.
Fig. 1.
Evolution of the COVID-19 spread in the Expanded Metropolitan Area of São Paulo, Brazil, from March 26, 2020, to July 06, 2020
Using the Spearman correlation test, significantly positive correlations were found between infection rate and population (people), cumulative COVID-19 confirmed cases, and population density (people∙km−2) (Table 2). Similarly, Şahin (2020) reported high correlation between population and total cases in Turkey, and Ahmadi et al. (2020) found significant correlation between population density and total cases in Iran. Interestingly, Hamidi et al. (2020) have reported that at county level in the USA, population density is not significantly related to infection rate possibly because of adherence to social distancing. In low- and middle-income countries though, high population density is commonly associated with informal urban settlements, being social distancing impracticable (Wilkinson 2020).
Table 2.
Spearman correlation coefficients (ρ): infection rate vs social indicators considering 59 cities with a total of 29,389,922 people
| Social indicator | Infection rate | p value |
|---|---|---|
| Population (people) | 0.83* | 0.0000 |
| Cumulative confirmed cases | 0.99* | 0.0000 |
| Population density (people∙km−2) | 0.46* | 0.0003 |
| Municipal Human Development Index (MHDI) | 0.11 | 0.4014 |
| Gross domestic product (R$ per capita) | 0.13 | 0.3162 |
| Average income (R$ per capita) | 0.15 | 0.2675 |
R$, reais, Brazilian currency
*In italics: significant correlation at α = 0.05
The sensitivity analysis indicated the importance of the average income and the gross domestic product within the expanded metropolitan area of São Paulo, Brazil (Table 3) possibly due to higher frequency of international traveling of population living in wealthier neighborhoods.
Table 3.
Results of sensitivity analysis using the PCC method (p value < 0.15): infection rate as the dependent variable and social indicators as the independent variables
| Social indicator | Coefficient | t value | p value |
|---|---|---|---|
| Average income (R$ per capita) | − 0.00090 | − 2.5867 | 0.0126 |
| Population density (people∙km−2) | − 0.00063 | − 1.8897 | 0.0644 |
| Population (people) | 0.00625 | 1.4543 | 0.1520 |
| Gross domestic product (R$ per capita) | − 0.00052 | − 1.5856 | 0.1190 |
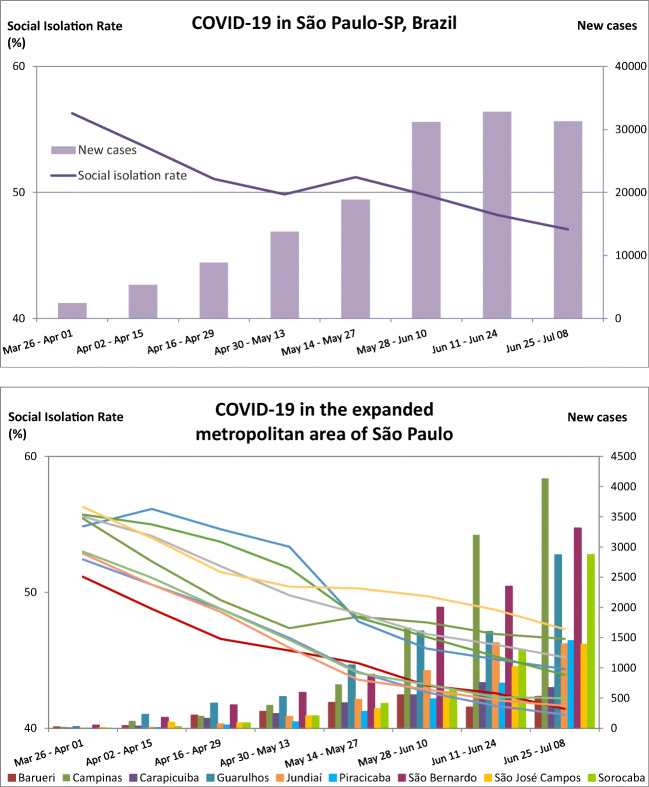
As for a different social aspect, significantly negative correlations were found between COVID-19 infection rate and social isolation rate in all analyzed cities (Table 4), thus indicating that social distancing has been effective in reducing the COVID-19 transmission within the expanded metropolitan area of São Paulo. Furthermore, using graphical analysis, we have observed a consistent trend in all analyzed cities, with increases of confirmed new cases of COVID-19 associated with decreases in social isolation rates (Fig. 2). Our results corroborate data from recent literature, as Ahmadi et al. (2020) found a significant correlation between COVID-19 cases and intra-provincial traffic in Iran.
Table 4.
Spearman correlation coefficients (ρ): infection rate vs meteorological conditions and social isolation rate in each analyzed city
| Infection rate | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SP | CPS | SBC | GUA | SOR | JND | SJC | PIR | CAR | BAR | |
| SIR3 | − 0.58* | − 0.44* | − 0.79* | − 0.83* | − 0.76* | − 0.76* | − 0.59* | − 0.73* | − 0.86* | − 0.65* |
| SIR7 | − 0.56* | − 0.47* | − 0.77* | − 0.80* | − 0.75* | − 0.74* | − 0.54* | − 0.73* | − 0.84* | − 0.63* |
| SIR14 | − 0.42* | − 0.39* | − 0.61* | − 0.62* | − 0.61* | − 0.62* | − 0.45* | − 0.63* | − 0.67* | − 0.49* |
| UV3 | − 0.55* | - | − 0.59* | − 0.51* | - | - | − 0.28* | - | - | − 0.58* |
| UV7 | − 0.65* | - | − 0.67* | − 0.59* | - | - | − 0.40* | - | - | − 0.66* |
| UV14 | − 0.65* | - | − 0.68* | − 0.50* | - | - | − 0.38* | - | - | − 0.62* |
| T3 | − 0.30* | − 0.59* | - | − 0.29* | − 0.42* | − 0.37* | − 0.39* | − 0.49* | − 0.32* | − 0.28* |
| T7 | − 0.29* | − 0.63* | - | − 0.29* | − 0.45* | − 0.38* | − 0.42* | − 0.55* | − 0.33* | − 0.28* |
| T14 | − 0.33* | − 0.67* | - | − 0.33* | − 0.50* | − 0.42* | − 0.48* | − 0.62* | − 0.36* | − 0.33* |
| RH3 | 0.14 | - | - | - | − 0.03 | 0.01 | − 0.08 | 0.26* | − 0.11 | − 0.11 |
| RH7 | 0.07 | - | - | - | − 0.01 | 0.10 | − 0.03 | 0.34* | − 0.04 | − 0.04 |
| RH14 | − 0.13 | - | - | - | − 0.12 | 0.00 | − 0.04 | 0.27* | − 0.12 | − 0.12 |
| WS3 | − 0.16 | − 0.35* | − 0.19 | 0.07 | - | − 0.24* | − 0.44* | 0.04 | − 0.21* | − 0.14 |
| WS7 | − 0.26* | − 0.41* | − 0.30* | 0.03 | - | − 0.32* | − 0.52* | 0.06 | − 0.30* | − 0.24* |
| WS14 | − 0.32* | 0.50* | − 0.41* | − 0.04 | - | − 0.41* | − 0.55* | − 0.13 | − 0.36* | − 0.31* |
SP, São Paulo; CPS, Campinas; SBC, São Bernardo do Campo; GUA, Guarulhos; SOR, Sorocaba; JND, Jundiaí; SJC, São José dos Campos; PIR, Piracicaba; CAR, Carapicuíba; BAR, Barueri; SIR, social isolation rate; UV, ultraviolet radiation; T, temperature; RH, relative humidity; WS, wind speed; 3, 3 days previous to case reports; 7, 7 days previous to case reports; 14, 14 days previous to case reports
- indicates data not available
*In italics: significant correlation at α = 0.05
Fig. 2.
Confirmed new cases of COVID-19 associated with decreases in social isolation rates over time in the capital city São Paulo and in nine cities within the expanded metropolitan area of São Paulo
Using the Spearman correlation test, significantly negative correlations were found between COVID-19 infection rate and UV radiation in all cities with available UV data (5 out of 9 analyzed cities) (Table 4); furthermore, the sensitivity analysis pointed out UV radiation as a significant variable (Table 5). These findings are consistent with recent literature; for example, Ahmadi et al. (2020) have found the lowest COVID-19 infection rates in provinces with high solar radiation. Furthermore, Schuit et al. (2020) have demonstrated that the influenza virus in aerosols decays more rapidly under simulated sunlight than under dark conditions, and concluded that their results are in accordance with epidemiological data reporting sunlight levels to be inversely correlated to influenza transmission. More importantly, Sagripanti and Lytle (2020) have recently predicted the inactivation of SARS-CoV-2 by solar UVB in densely populated cities in the world. The authors have estimated that during the winter season in the city of São Paulo, a 41-min exposure to sunlight around solar noon would be required to achieve 90% inactivation of SARS-CoV-2 virus, while a 13-min exposure to sunlight around solar noon could achieve 99% inactivation during the summer season. Therefore, recent literature corroborates our finding that the UV radiation provided by sunlight potentially reduces the infectivity of SARS-CoV-2.
Table 5.
Results of sensitivity analysis using the PCC method (p value < 0.15): infection rate as the dependent variable and meteorological conditions and social isolation rate as the independent variables
| Coefficient | t value | p value | |
|---|---|---|---|
| SIR3 | − 0.3478 | − 10.81 | 6.45 × 10−24 |
| SIR7 | − 0.0746 | − 1.45 | 0.14795 |
| SIR14 | − 0.0849 | − 2.22 | 0.02697 |
| UV3 | − 0.1468 | − 4.73 | 3.20 × 10−6 |
| UV7 | − 0.1984 | − 6.26 | 1.02 × 10−9 |
| UV14 | − 0.1847 | − 5.92 | 7.33 × 10−9 |
| WS14 | − 0.0757 | − 2.59 | 0.00988 |
SIR, social isolation rate; UV, ultraviolet radiation; WS, wind speed; 3, 3 days previous to case reports; 7, 7 days previous to case reports; 14, 14 days previous to case reports
Significantly negative correlations were also found between COVID-19 infection rate and temperature of three, 7 or 14 days previous to case reports in all cities with available temperature data (9 out of 10 analyzed cities) (Table 4), thus suggesting that increases in temperature contribute to decreases in COVID-19 transmission in the expanded metropolitan area of São Paulo. Several studies in recent literature have also indicated that temperature is inversely related to COVID-19 incidence (Liu et al. 2020; Prata et al. 2020; Qi et al. 2020; Şahin 2020; Wu et al. 2020). More importantly, some authors have reported that the infection ability of SARS-CoV-2 decreases with temperature increases, and thus, COVID-19 prevention and control are expected to be more effective at warmer weather, being the molecular mechanism thoroughly described elsewhere (He et al. 2020).
Significant negative correlations were also found between COVID-19 infection rate and wind speed 14 days before case reports in 7 out of 9 analyzed cities (Table 4), and the sensitivity analysis pointed out wind speed 14 days before case reports as a significant variable (Table 5). Likewise, Ahmadi et al. (2020) have reported significant inverse correlation between infection rate and wind speed in Iran.
Conclusions
Our results reveal that the spread of COVID-19 within the expanded metropolitan area of São Paulo, Brazil, is influenced by the availability of highways. As for social aspects, COVID-19 infection rate was found to be both positively correlated with population density (ρ = 0.46), and negatively correlated with social isolation rate (ρ varying from − 0.39 to − 0.86), hence, indicating that social distancing has been effective in reducing the COVID-19 transmission. Overall, our results show that the COVID-19 transmission within the expanded metropolitan area of São Paulo is inversely correlated with both temperature (ρ varying from − 0.28 to − 0.67) and UV radiation (ρ varying from − 0.28 to − 0.68). Together with recent literature, our study suggests that the UV radiation provided by sunlight potentially contributes to depletion of SARS-CoV-2 infectivity.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Liane Yuri Kondo Nakada, Email: lnakada@unicamp.br.
Rodrigo Custodio Urban, Email: rodrigo.urban@puc-campinas.edu.br.
References
- Ahmadi M, Sharifi A, Dorosti S, Ghoushchi SF, Ghanbari N. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci Total Environ. 2020;729:138705. doi: 10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brazil (2020) Ministry of Health – COVID19 – Coronavirus Panel. https://covid.saude.gov.br/. Accessed 10 July 2020
- CETESB – São Paulo State Environmental Agency (2020). QUALAR: air quality information system. https://qualar.cetesb.sp.gov.br/qualar/home.do. Accessed 22 Apr 2020
- El-Sayed A, Kamel M. Climatic changes and their role in emergence and re-emergence of diseases. Environ Sci Pollut Res. 2020;27:22336–22352. doi: 10.1007/s11356-020-08896-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamidi S, Sabouri S, Ewing R (2020) Does density aggravate the COVID-19 pandemic? J Am Plan Assoc 1–15. 10.1080/01944363.2020.1777891
- Harmooshi NN, Shirbandi K, Rahim F. Environmental concern regarding the effect of humidity and temperature on 2019-nCoV survival: fact or fiction. Environ Sci Pollut Res. 2020;27:36027–36036. doi: 10.1007/s11356-020-09733-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He J, Tao H, Yan Y, Huang SY, Xiao Y. Molecular mechanism of evolution and human infection with SARS-CoV-2. Viruses. 2020;12:428. doi: 10.3390/v12040428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John Hopkins University & Medicine (2020) Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html Accessed 18 July 2020
- Liu J, Zhou J, Yao J, Zhang X, Li L, Xu X, He X, Wang B, Fu S, Niu T, Yan J, Shi Y, Ren X, Niu J, Zhu W, Li S, Luo B, Zhang K. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci Total Environ. 2020;726:138513. doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollalo A, Vahedi B, Rivera KM. GIS-based spatial modeling of COVID-19 incidence rate in the continental United States. Sci Total Environ. 2020;728:138884. doi: 10.1016/j.scitotenv.2020.138884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata DN, Rodrigues W, Bermejo PH. Temperature significantly changes COVID-19 transmission in (sub)tropical cities of Brazil. Sci Total Environ. 2020;729:138862. doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H, Xiao S, Shi R, Ward MP, Chen Y, Tu W, Su Q, Wang W, Wang X, Zhang Z. COVID-19 transmission in Mainland China is associated with temperature and humidity: a time-series analysis. Sci Total Environ. 2020;728:138778. doi: 10.1016/j.scitotenv.2020.138778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagripanti J-L, Lytle CD. Estimated inactivation of coronaviruses by solar radiation with special reference to COVID-19. Photochem Photobiol. 2020;96:731–737. doi: 10.1111/php.13293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Şahin M. Impact of weather on COVID-19 pandemic in Turkey. Sci Total Environ. 2020;728:138810. doi: 10.1016/j.scitotenv.2020.138810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- São Paulo (2020a) São Paulo state–Decreto n. 64.881, de 22 de Março de 2020. https://www.al.sp.gov.br/norma/193361. Accessed 21 April 2020
- São Paulo (2020b) São Paulo state–social isolation intelligent monitoring system. https://www.saopaulo.sp.gov.br/coronavirus/isolamento/. Accessed 07 July 2020
- Schuit M, Gardner S, Wood S, Bower K, Williams G, Freeburger D, Dabisch P. The influence of simulated sunlight on the inactivation of Influenza Virus in aerosols. J Infect Dis. 2020;221:372–378. doi: 10.1093/infdis/jiz582. [DOI] [PubMed] [Google Scholar]
- SEADE (2020a) Coronavirus. https://www.seade.gov.br/coronavirus/. Accessed 07 July 2020
- SEADE (2020b) IMP https://www.imp.seade.gov.br. Accessed 07 July 2020
- Tobías A. Evaluation of the lockdowns for the SARS-CoV-2 epidemic in Italy and Spain after one month follow up. Sci Total Environ. 2020;725:138539. doi: 10.1016/j.scitotenv.2020.138539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO – World Health Organization (2020) WHO Director-General’s opening remarks at the media briefing on COVID19 - 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19%2D%2D-11-march-2020. Accessed 25 Apr 2020
- Wilkinson A (2020) Local response in health emergencies: key considerations for addressing the COVID-19 pandemic in informal urban settlements. Environ Urban:095624782092284. 10.1177/0956247820922843 [DOI] [PMC free article] [PubMed]
- Worldometers (2020) Coronavirus. https://www.worldometers.info/coronavirus/. Accessed 30 Apr 2020
- Wu Y, Jing W, Liu J, Ma Q, Yuan J, Wang Y, Du M, Liu M. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci Total Environ. 2020;729:139051. doi: 10.1016/j.scitotenv.2020.139051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu L, Liu X, Huang H, Avellán-Llaguno RD, Lazo MML, Gaggero A, Rifo RS, Patiño L, Valencia-Avellan M, Diringer B, Huang Q, Zhu Y-G. Meteorological impact on the COVID-19 pandemic: a study across eight severely affected regions in South America. Sci Total Environ. 2020;744:140881. doi: 10.1016/j.scitotenv.2020.140881. [DOI] [PMC free article] [PubMed] [Google Scholar]