Abstract
Background
The coronavirus disease 2019 pandemic has greatly increased the frequency of disinfecting surfaces in public places, causing a strain on the ability to obtain disinfectant solutions. An alternative is to use plain alcohols (EtOH and IPA) or sodium hypochlorite (SH).
Aim
To determine the efficacy of various concentrations of EtOH, IPA and SH on a human coronavirus (HCoV) dried on to surfaces using short contact times.
Methods
High concentrations of infectious HCoV were dried on to porcelain and ceramic tiles, then treated with various concentrations of the alcohols for contact times of 15 s, 30 s and 1 min. Three concentrations of SH were also tested. Reductions in titres were measured using the tissue culture infectious dose 50 assay.
Findings
Concentrations of EtOH and IPA from 62% to 80% were very efficient at inactivating high concentrations of HCoV dried on to tile surfaces, even with a 15-s contact time. Concentrations of 95% dehydrated the virus, allowing infectious virus to survive. The dilutions of SH recommended by the Centers for Disease Control and Prevention (1/10 and 1/50) were efficient at inactivating high concentrations of HCoV dried on to tile surfaces, whereas a 1/100 dilution had substantially lower activity.
Conclusions
Multiple concentrations of EtOH, IPA and SH efficiently inactivated infectious HCoV on hard surfaces, typical of those found in public places. Often no remaining infectious HCoV could be detected.
Keywords: Human coronavirus, COVID-19, Ethanol, Isopropanol, Sodium hypochlorite
Introduction
With the rapid spread of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) around the world, there has been a concomitant rapid increase in the need for effective sanitizers/disinfectants. With the major method of transmission being through aerosolized respiratory droplets, and virus remaining viable on surfaces for hours or even days [[1], [2], [3]], there is a constant need to disinfect surfaces properly. Healthcare institutes, businesses and homes quickly found themselves in need of reagents to disinfect surfaces, and the need to disinfect surfaces more frequently resulted in product shortages. To increase awareness of potentially effective surface disinfectant products for use against the possible presence of SARS-CoV-2 on surfaces, the Environmental Protection Agency (EPA) provided a list of ‘Disinfectants for use against SARS-CoV-2’ [4]. Under their guidelines, EPA allows a manufacturer to provide data which show that their product(s) is (are) potentially effective against harder-to-inactivate viruses. After receiving approval from EPA, the manufacturers can market claims for use against SARS-CoV-2. While this list can potentially provide important information to users, it has several shortcomings. First, for many of the disinfectants on the list, it is difficult, if not impossible, to obtain the experimental protocols used to determine the effectiveness of the disinfectant. Second, the US Food and Drug Administration, EPA, and the Department of Health and Human Services all require that standards for meeting efficacy data requirements include testing virucidal effects on a carrier (surface), as opposed to a suspension assay [[5], [6], [7]]. Third, the surface or carrier test also requires the drying of virus on to the carrier in the presence of a protein ‘soil’, and the virus is subsequently recovered and assayed for infectivity [[5], [6], [7]]. Fourth, many of the contact times reported on EPA's list are not realistic for practical use. A contact time >1 min is often not pragmatic under normal situations in healthcare institutes, business or homes. It is also questionable if the viruses used to make these claims are really harder-to-inactivate viruses. This list was developed to provide necessary guidance at the beginning of the present pandemic. For that early need, it was an important aid. However, the list was meant to be a stop gap until more evidence-based studies could be completed.
In the absence of readily available disinfectants, many public places have found that the only products available in the necessary quantities are common alcohols – ethanol (EtOH) and isopropyl alcohol (IPA) – without additives. This study investigated the efficacy of these two basic disinfectants, which are relatively easy to obtain, and are relatively safe for use in public areas. Various concentrations of these two alcohols, commonly used in disinfectants and sanitizers, were tested. To satisfy the requirements of hard surfaces as carriers, ceramic and porcelain tiles that are commonly found in public places were tested. All assays were performed in the presence of a ‘soil’, bovine serum albumin (BSA). For all of the assays, high titre stocks of human coronavirus 229e (HCoV-229e) were used as a surrogate for SARS-CoV-2. While there are clear differences in the pathology of these viruses, they are from the same family of viruses, have very similar structures, and both are human respiratory pathogens. In a dried state, SARS-1 has been shown to survive for up to 9 days, whereas HCoV-229e only survived for up to 6 days [8]; however, comparison between disinfectants were not undertaken. Using the surrogate enabled the authors to rapidly test and provide science-based answers in the search for an effective surface disinfectant, using contact times that better reflect real-life situations.
Methods
Cell lines, cell culture and virus
Huh7 cells were grown in Dulbecco Modified Eagle's Medium (DMEM) supplemented with 10% fetal bovine serum (FBS) (DMEM10) and 100 U/mL pen/strep, and the cells were grown in 5% CO2 at 37°C. Infectious stocks of HCoV 229e were prepared by seeding T75 flasks with 7 × 106 Huh7 cells, which were incubated overnight. The following day, the media was changed to DMEM with 2% FBS (DMEM2), and cells were infected with virus using a multiplicity of infection of 0.01. The infected flasks were incubated in 5% CO2 at 35°C for 2 days. On the second day, the flasks were frozen at -80°C for at least 1 h, then thawed in a 37°C water bath, taking care to remove them from the water bath before they were completely thawed. Thawing was completed at room temperature. The cell suspensions were transferred to a 15-mL polypropylene tube and sonicated on ice in a cup sonicator at 100 W peak envelope power, with three bursts of 20 s each. The lysates were clarified by centrifugation at 3000 rpm for 10 min at 4°C, and the supernatant was poured into a fresh 15-mL tube. Virus solutions were aliquoted into eight 0.5-mL portions, and several smaller aliquots were frozen for long-term storage at -80°C. One of the smaller aliquots was used to determine the titre of the stock using the tissue culture infectious dose 50 (TCID50) assay.
TCID50 assay
Huh7 cells were harvested, counted and resuspended in DMEM2 to a concentration of 1.5 × 106 cells/mL. Next, 100 μL of the cell suspension was added to each well of the 96-well plate. Plates were incubated overnight in 5% CO2 at 37°C. Serial 10-fold dilutions of virus were added to each column of wells containing cells. An extra row of mock-infected cells was included across the bottom as controls. The plates were incubated in 5% CO2 at 35°C for 3 days. On the third day, the wells were examined for the presence of cytopathic effects (CPE), and TCID50 was calculated using the Reed–Muench method [9], based on the number of wells positive for CPE at each dilution.
Disinfectant testing
The disinfectants used in the study were EtOH (Thermo Fisher Scientific, Waltham, MA, USA), IPA (Sigma-Aldrich, St Louis, MO, USA), glutaraldehyde (GTA) (Cidex and Cidexplus; Advanced Sterilization Products, Irvine, CA, USA), ortho-phthalaldehyde (OPA) (Cidex OPA; Advanced Sterilization Products) and sodium hypochlorite (SH) (Activate; Deardorff Fitzsimmons Corp., Merlin, OR, USA). Each disinfectant was prepared according to the manufacturer's recommendations and stated dilution immediately before testing.
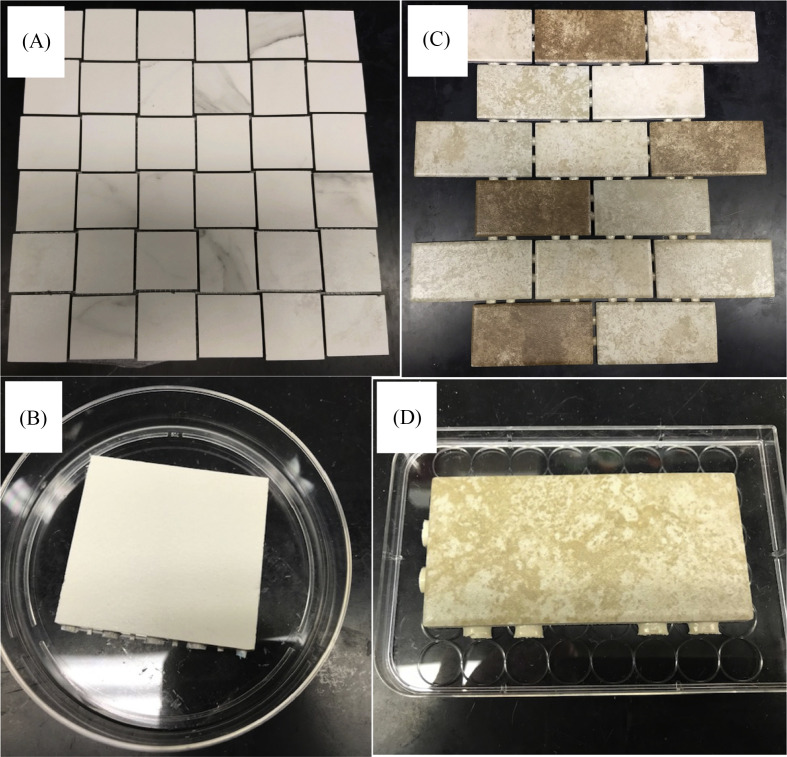
Porcelain and ceramic tiles were purchased from a local building supply company and used as carriers for the disinfection assays (Figure 1 ). Carriers were soaked in 10% hydrogen peroxide for 15 min, neutralized in sterile water containing 200 U/mL of catalase for 10 min, and rinsed in sterile water for 10 min before being dried in a sterile Petri dish [10,11]. Two hundred microlitres of an organic load or soil of 5% BSA was added to the virus suspension, and 200 μL of this virus solution was spread on to a single carrier side with a sterile pipette tip. The inoculated carriers were allowed to dry in a laminar flow cabinet for 30 min. Immediately after drying, 1 mL of each liquid disinfectant was added to the surface of the carrier, covering the entire area containing the dried virus. Carriers were then incubated at room temperature for contact times of 15 s, 30 s and 1 min. Virus was subsequently scraped off the carrier into a 15-mL Amicon Ultra centrifugal filter (100,000 MW cut-off) and 2 mL of neutralizer was added to the filters immediately. The filters were centrifuged at 4000 rpm for 10 min, washed four times with DMEM2, and centrifuged again at 4000 rpm for 10 min. The virus-containing eluents were then assayed for infectivity using the TCID50 method. At least four replicate assays were performed for each disinfectant and contact time. Controls for virus recovery after drying on a carrier were included for each set of assays performed. No significant decrease (<0.5 log10) in infectious virus was observed due to drying the virus on either type of tile. Neutralizers used were DMEM2 for EtOH and IPA, and 7% glycine for SH, GTA and OPA.
Figure 1.
Common tiles used in public places. Tiles were separated into individual pieces and used as carriers for the disinfectant testing. (A,B) Porcelain tiles. (C,D) Ceramic tiles.
Results
Table I shows that, in general, both EtOH and IPA were highly effective at inactivating HCoV. EtOH concentrations of 62%, 70%, 75% and 80%, and IPA concentrations of 70%, 75% and 80% were able to produce >4 log10 inactivation of HCoV, and in some cases, no remaining infectious virus could be detected. More than 99.99% reduction of infectious virus was observed at all contact times, including the shortest time of 15 s. In many instances, it was not possible to detect any residual infectious virus (Table I). However, in a few cases with contact times of 15 s or 30 s, some of the replicates reached only a 3 log10 reduction (Table I), although this level still means that >99.9% of the infectious virus was destroyed. Interestingly, at the highest concentrations tested (95% EtOH and 95% IPA), significant reductions in virus inactivation were observed, with some contact times producing <2 log10 reduction of infectious virus.
Table I.
Effectiveness of disinfectants against human coronavirus 229e after different contact times
| Disinfectant | Carrier | Log10 decrease contact time 1 min |
Log10 decrease contact time 30 s |
Log10 decrease contact time 15 s |
|---|---|---|---|---|
| 62% EtOH | Porcelain | >4 log10a | >4 log10a | >4 log10a |
| 62% EtOH | Ceramic | >4 log10a | >4 log10 | >4 log10a |
| 70% ETOH | Porcelain | >4 log10a | >4 log10a | >4 log10a |
| 70% ETOH | Ceramic | >4 log10a | >4 log10a | >4 log10 |
| 75% ETOH | Porcelain | >4 log10 | >4 log10a | >4 log10a |
| 75% ETOH | Ceramic | >4 log10a | >4 log10a | >3 to >4 log10 |
| 80% ETOH | Porcelain | >4 log10a | ≥4 log10 | >4 log10 |
| 80% ETOH | Ceramic | >4 log10a | >4 log10 | >4 log10 |
| 95% ETOH | Porcelain | >1 but <2 log10 | >2 but <3 log10 | >2 but <3 log10 |
| 95% ETOH | Ceramic | >1 but <2 log10 | >1 but <2 log10 | <1 to <2 log10 |
| 70% IPA | Porcelain | >4 log10a | >4 log10a | >4 log10a |
| 70% IPA | Ceramic | >4 log10a | >3 to >4 log10 | >4 log10a |
| 75% IPA | Porcelain | >4 log10a | >4 log10a | >4 log10a |
| 75% IPA | Ceramic | >4 log10a | >4 log10 | >3 to >4 log10 |
| 80% IPA | Porcelain | >4 log10 | >4 log10a | >4 log10 |
| 80% IPA | Ceramic | >4 log10a | >4 log10a | >4 log10a |
| 95% IPA | Porcelain | >3 but <4 log10 | >3 but <4 log10 | >4 log10 |
| 95% IPA | Ceramic | >1 but <2 log10 | >1 to >2 log10 | ≥3 to >4 log10 |
| 0.525% SH | Porcelain | >4 log10a | >4 log10a | >4 log10a |
| 0.525% SH | Ceramic | >4 log10a | >4 log10a | >4 log10a |
| 0.0525% SH | Porcelain | >2 but <3 log10 | >2 to <3 log10 | >1 to <2 log10 |
| 0.0525% SH | Ceramic | >1 to <2 log10 | >1 to <2 log10 | >1 to <3 log10 |
| 0.1% SH | Porcelain | ND | ND | ND |
| 0.1% SH | Ceramic | >4 log10a | >4 log10a | >4 log10a |
| GTA | Porcelain | >4 log10a | >4 log10a | >4 log10a |
| GTA | Ceramic | >4 log10a | >4 log10a | >4 log10a |
EtOH, ethanol; IPA, isopropanol; GTA, glutaraldehyde; ND, not done; OPA, ortho-phthalaldehyde; SH, sodium hypochlorite.
No detection of remaining infectious virus.
Due to the authors' previous experience testing bleach (SH) [[10], [11], [12], [13]], and the potential for people to have it available for use to disinfect surfaces, the decision was made to include SH in these evaluations. Common concentrations of bleach purchased by the general public contain between 5% and 6% SH, and it is recommended to be used at a dilution of 1/10 to 1/100. In this study, 5.25% SH diluted 1/10 (∼0.525%) was used, as the authors have done previously as a positive virucidal control [10,11,13]. As expected, 0.525% SH was highly effective at inactivating HCoV, producing >4 log10 decrease in infectious virus. No signs of remaining infectivity were observed for any of the contact times (Table I). As there are recommendations to use bleach at 1/50 and 1/100 dilutions for sanitizing surfaces [14,15], the authors also tested the 1/100 dilution (∼0.0525% SH), and found a significant decrease in its ability to inactivate HCoV (Table I). Sometimes, the inactivation was <2 log10 decrease. A 1/50 dilution (∼0.1% SH) was also tested (Table I), and the efficacy of 0.1% SH was similar to that of 0.525% SH, both producing >4 log10 decrease in infectivity with contact times of 30 s and 15 s. With both 0.525% and 0.1% SH, there was no evidence of any remaining infectious virus (Table I).
Due to its prominent role for the last several decades as a hospital sterilant, GTA was also tested. As expected, GTA proved to be highly effective at inactivating HCoV, producing >4 log10 decrease in infectious virus at all contact times (Table I).
Discussion
In the midst of a pandemic, the supply chain may not be able to provide traditional disinfectants at sufficient speed to meet needs. Basic alcohols (EtOH and IPA) are likely easy solutions to fill unmet needs. Clear evidence-based answers to important questions of contact times, effect of carrier types, and the influence of soil contamination on disinfectants used on a new infectious organism are minimal or non-existent. The aim of this study was to create a more real-world situation to evaluate the efficacy of available disinfecting agents. In situations such as the present pandemic, these may be the only products available during times of shortage. This study used a wide range of concentrations, porcelain and ceramic tile carriers (common surfaces in public places), contamination with organic soil, and short contact times that represent real-world practices in disinfecting public spaces. The study found that EtOH and IPA at concentrations ranging from 62% to 80% are highly effective at inactivating HCoV on tile surfaces, even with contact times as low as 15 s. While there were slight differences between the two carriers, both were able to inactivate >99.99% or 99.9% of the virus. Noteworthy differences were observed when 95% EtOH or 95% IPA was used. It is likely that a minimum concentration of water is required to catalyse microbial penetration, allowing these agents to perform their destructive effects optimally. Higher concentrations of alcohol may dehydrate the virus, allowing significant levels to remain viable [16,17]. Therefore, the adage that ‘more is better’ is not necessarily true for alcohols. As many public spaces have bleach on hand, this was also tested at three recommended concentrations [14,15]. Concentrations of 0.525% and 0.1% inactivated ≥99.99% of the virus within short contact times. However, 0.0525% SH was much less effective at inactivating the virus.
Several studies have reported the efficacy of various disinfectants in inactivating CoVs, including animal [18,19] and human [[1], [2], [3], [4], [5], [6], [7], [8], [9], [10]] CoVs. These studies are discussed in a 2020 review [11]. The majority of these studies did not use the carrier method of drying the virus on to a solid surface. It has been shown recently that HCoV can remain infectious in aerosols for hours and on surfaces for days [12], demonstrating the importance of testing the efficacy of a disinfectant in the manner in which it will be used (i.e. to disinfect solid surfaces). Of those studies that used the carrier method, some dried the virus on Petri dishes [2,13] while others used stainless steel as the carrier [1,14,15]. Similar to the use of stainless steel, this study used carriers that represented real-world situations. Porcelain and ceramic tiles are common surfaces in many public places, and require constant disinfection during a pandemic. This study found only small differences in effect, <1 log10 inactivation, between the two tile types for only a few of the disinfectant concentrations and contact times tested.
Previous studies of particular relevance to the present results used different concentrations of EtOH and IPA [[7], [8], [9],15,16]. All but one of these studies used the suspension technique, so those testing high concentrations of EtOH or IPA were unable to factor in the rapid dehydration phenomenon which is characteristic of these agents. The only study that performed testing by drying the virus on to a carrier only used 70% EtOH [15]. Results from these studies aligned well with the present results, but none covered the range of concentrations covered here, with the majority only testing a few concentrations. In addition, only one study used the carrier model. Two studies that tested bleach as a surface disinfectant showed, in agreement with the present study, that diluting SH 100-fold resulted in poor inactivation of two animal CoVs (mouse hepatitis virus and transmissible gastroenteritis virus [15]) or HCoV 229e [1]. In addition, one of these studies also tested SH diluted 50-fold, and observed a 99.9% reduction in virus titre [1], similar to the present results.
SARS-CoV-2 is the third pathogenic HCoV with significant mortality to spread in the human population in the past 20 years [17,18]. After its emergence, it spread rapidly around the world. While there is potential for other mechanisms of transmission, aerosolization and fomites are considered the most probable means. Some of the most common symptoms of COVID-19 are associated with the formation of aerosols. Persons infected but showing only mild or no symptoms can readily spread the virus by aerosols [19]. Aerosols directly and indirectly contaminate surfaces in all public places, on which the virus can stay infectious for days [12]. This resulted in persons responsible for the safety of many public places, including healthcare institutes, businesses and homes, trying to find solutions to their need to disinfect surfaces much more often. This led to rapid strain on the supply chain to provide sufficient quantities of normally used disinfectant compositions. One answer was the use of readily available agents such as common alcohols (EtOH and IPA) and diluted bleach. This study provides important information on the efficacy of these agents at different concentrations to inactivate HCoV.
Acknowledgements
The authors wish to thank Dr. Jianming Hu, Pennsylvania State University for the kind gift of the Huh7 cells.
Conflict of interest statement
None declared.
Funding sources
This study was funded, in part, by the Huck Institutes of the Life Sciences' Coronavirus Research Seed Fund.
References
- 1.Sattar S.A., Springthorpe V.S., Karim Y., Loro P. Chemical disinfection of non-porous inanimate surfaces experimentally contaminated with four human pathogenic viruses. Epidemiol Infect. 1989;102:493–505. doi: 10.1017/s0950268800030211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Omidbakhsh N., Sattar S.A. Broad-spectrum microbicidal activity, toxicologic assessment, and materials compatibility of a new generation of accelerated hydrogen peroxide-based environmental surface disinfectant. Am J Infect Control. 2006;34:251–257. doi: 10.1016/j.ajic.2005.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kariwa H., Fujii N., Takashima I. Inactivation of SARS coronavirus by means of povidone-iodine, physical conditions and chemical reagents. Dermatology. 2006;212(Suppl. 1):119–123. doi: 10.1159/000089211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wood A., Payne D. The action of three antiseptics/disinfectants against enveloped and non-enveloped viruses. J Hosp Infect. 1998;38:283–295. doi: 10.1016/S0195-6701(98)90077-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eggers M., Koburger-Janssen T., Eickmann M., Zorn J. In vitro bactericidal and virucidal efficacy of povidone-iodine gargle/mouthwash against respiratory and oral tract pathogens. Infect Dis Ther. 2018;7:249–259. doi: 10.1007/s40121-018-0200-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eggers M., Eickmann M., Zorn J. Rapid and effective virucidal activity of povidone-iodine products against Middle East respiratory syndrome coronavirus (MERS-CoV) and modified vaccinia virus Ankara (MVA) Infect Dis Ther. 2015;4:491–501. doi: 10.1007/s40121-015-0091-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kratzel A., Todt D., V'Kovski P., Steiner S, Gultom M, Thao TTN. Inactivation of severe acute respiratory syndrome Coronavirus 2 by WHO-recommended hand rub formulations and alcohols. Emerg Infect Dis. 2020;26:1592–1595. doi: 10.3201/eid2607.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rabenau H.F., Kampf G., Cinatl J., Doerr H.W. Efficacy of various disinfectants against SARS coronavirus. J Hosp Infect. 2005;61:107–111. doi: 10.1016/j.jhin.2004.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rabenau H.F., Cinatl J., Morgenstern B., Bauer G., Preiser W., Doerr H.W. Stability and inactivation of SARS coronavirus. Med Microbiol Immunol. 2005;194:1–6. doi: 10.1007/s00430-004-0219-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siddharta A., Pfaender S., Vielle N.J., Dijkman R, Friesland M, Becker B. Virucidal activity of World Health Organization-recommended formulations against enveloped viruses, including Zika, Ebola, and emerging coronaviruses. J Infect Dis. 2017;215:902–906. doi: 10.1093/infdis/jix046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104:246–251. doi: 10.1016/j.jhin.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Doremalen N., Bushmaker T., Morris D.H., Holbrook MG, Gamble A, Williamson BN. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dellanno C., Vega Q., Boesenberg D. The antiviral action of common household disinfectants and antiseptics against murine hepatitis virus, a potential surrogate for SARS coronavirus. Am J Infect Control. 2009;37:649–652. doi: 10.1016/j.ajic.2009.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goyal S.M., Chander Y., Yezli S., Otter J.A. Evaluating the virucidal efficacy of hydrogen peroxide vapour. J Hosp Infect. 2014;86:255–259. doi: 10.1016/j.jhin.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hulkower R.L., Casanova L.M., Rutala W.A., Weber D.J., Sobsey M.D. Inactivation of surrogate coronaviruses on hard surfaces by health care germicides. Am J Infect Control. 2011;39:401–407. doi: 10.1016/j.ajic.2010.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saknimit M., Inatsuki I., Sugiyama Y., Yagami K. Virucidal efficacy of physico-chemical treatments against coronaviruses and parvoviruses of laboratory animals. Jikken Dobutsu. 1988;37:341–345. doi: 10.1538/expanim1978.37.3_341. [DOI] [PubMed] [Google Scholar]
- 17.Drosten C., Gunther S., Preiser W., van der Werf S, Brodt HR, Becker S. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med. 2003;348:1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- 18.Zaki A.M., van Boheemen S., Bestebroer T.M., Osterhaus A.D., Fouchier R.A. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 19.Bai Y., Yao L., Wei T., Tian F, Jin DY, Chen L. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323:1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]