Abstract
Background and Purpose
The effect of the integrated program comprising cognitive training, art therapy, and music therapy has not been extensively studied in patients with Alzheimer's disease (AD). The present study investigated the effect of integrated cognitive intervention therapy on cognition, and activity of daily life (ADL), and mood in patients with mild to moderate AD.
Methods
In this study, the data of 59 patients who met the National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer disease and Related Disorders Association (NINCDS-ADRDS) criteria of probable AD among those who registered at the Centenarian's Good Memory Program in Goyang from September 2014 to August 2019 were collected. We statistically analyzed the scores of Korean version of a Mini-Mental Status Examination (K-MMSE), Korean Dementia Screening Questionnaire-Cognition (KDSQ-C), Geriatric Depression Scale (GDS), Beck Anxiety Inventory (BAI), and Seoul-Instrumental Activities of Daily Living (S-IADL) of the same patients before and after the use of integrated cognitive intervention therapy.
Results
K-MMSE slightly increased from 18.7±4.5 to 19.7±5.0 (p<0.001) and KDSQ-C improved from 14.5±7.6 before therapy to 12.6±7.2 after therapy (p=0.001). Mean S-IADL score improved from 17.6±7.6 before therapy to 15.7±9.5 after therapy (p<0.001). Additionally, mean GDS score before the therapy was 5.6±3.5 that improved to 4.2±3.0 after the therapy (p<0.001). Mean BAI score decreased from 8.4±10.3 before therapy to 5.9±8.4 after therapy (p=0.001).
Conclusions
In conclusion, this study demonstrated the possibility that the use of an integrated cognitive therapy improved cognition, ADL, and mood (depression and anxiety) in patients with mild to moderate ADs.
Keywords: Alzheimer's Disease, Art Therapy, Music Therapy
INTRODUCTION
Generally speaking Alzheimer's disease (AD), which is the most common cause of dementia, is growing burden in an aging society.1 In addition to cognitive decline and impairment of activity of daily life (ADL), depression (>50%)2 and anxiety (up to 70%)3 are also common comorbidities in AD that are associated with behavioral and psychological symptoms of dementia (BPSD) in elderly populations affected by this disease.
In fact, pharmacological and non-pharmacological strategies are the two most popular treatment options for AD. Pharmacological treatments such as acetylcholinesterase inhibitors and N-methyl-D-aspartate (NMDA) receptor antagonist are the widely used medications for treating AD.4 However, these medications cannot reverse impaired cognition and provide weak beneficial effects on BPSD and ADL. Similarly, benzodiazepines and antipsychotics not only have limited effects on BPSD, but also have some identified adverse effects among elderly patients with AD.5,6 Therefore, a good supplementary option for these patients can be the use of non-pharmacological treatments such as cognitive training, art therapy, and music therapy.7,8,9,10,11,12,13 These treatments may aid in controlling behavioral and functional concerns and provide beneficial effects concerning cognitive functions, without the participants having to endure any side effects from the treatment.
Our group had reported that music therapy of Centenarian's Good Memory Program improved mood and ADL in patients with noted identified cognitive decline.14 The previous studies on art or music therapy as reviewed usually focused on how the therapies affect the mood, but the effect on cognitive function was rarely measured.7,9,10,15 In addition, the effect of cognitive training has been controversial as noted in previous studies.16 Furthermore, although most of the studies have usually reported the effect of either cognitive training, art therapy, or music therapy, few studies have reported the effect of the integrative therapy, which can be synergistically effective. We developed the integrated program comprising cognitive training, art therapy, and music therapy that is being conducted at the Centenarian's Good Memory School for several years. This study investigated the effect of this integrated cognitive therapeutic intervention on cognition in program participants, as well as ADL and mood in patients with mild to moderate AD.
METHODS
Participants
We collected the data of 93 patients registered under the Centenarian's Good Memory Program in Goyang, Republic of Korea, from September 2014 to August 2019. All of the patients underwent a detailed medical history taking, neurological examinations, neuroimaging (brain computed tomography [CT] or magnetic resonance imaging [MRI]), and blood and neuropsychological tests. A total of 59 patients out of the 93 met the criteria of probable AD according to the National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer disease and Related Disorders Association (NINCDS-ADRDA).17 Participants were mild to moderate AD, which is a rating that corresponds to 0.5–2 in the Korean version of Clinical Dementia Rating (CDR), and these participants were included in the study.
Among the 59 participants, we could review 49 participants' medication history using medical records during therapy. Among the 49 participants whose medical history we were able to review, 41 were on acetylcholinesterase, and two were on NMDA antagonist. Among 11 participants who took anti-depressive medication, only three were advise to slightly increased the dose during therapy. Among the six patients who took anti-psychotics, it was noted that five maintained the same dose during therapy.
The exclusion criteria were the presence of metabolic diseases that can affect cognitive function (hyperthyroidism, vitamin B12 or folic acid deficiency, chronic renal failure, uncontrolled diabetes, and hepatic failure), consumption by a participant of more than three glasses of alcohol per day, and a history of stroke, seizure, and brain surgery. Further, patients who met the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) for psychotic or mood disorders such as schizophrenia or major depressive disorder were also excluded.9 This study was approved by the Institutional Review Board (IRB) of the Myongji Hospital and the study was performed in accordance with the approved protocols and guidelines. The requirement of informed consent was waived by the IRB of the Myongji Hospital, because we used retrospective de-identified data collected during the regular visits of the participants.
Integrated cognitive intervention programs
The therapy provided to the dementia patients was a non-pharmacological treatment program developed by combining cognitive and arts therapies. It was a 32-hour therapy (2 hours×16 sessions) comprising 16 hours of cognitive training, 8 hours of music therapy, and 8 hours of art therapy. In this sense, the mean number of sessions that the participants received was 14.7±1.3.
Cognitive training
To begin with, cognitive training was comprised of 16 sessions of 60 minutes each conducted over 8 weeks (twice weekly). The training consisted of 5 stages: introductory activity, brain health lifestyle education, activity briefing, main activity, and finishing activity. The introductory activity stage included welcome greetings, regards and sharing, recalling previous activities, and determining today's date, day, and weather. In the brain health lifestyle education stage, we investigated the “My Day” diary and brain health lifestyle as was written by the participants in their cognitive health notebook. The Department of Health and Human Services has recommended to teach healthy and bad lifestyles according to the dementia prevention guidelines 3.3.3. In the activity briefing stage, patients were informed regarding the purpose and method of the sessions, stating goals and expected effects, and were encouraged to be motivated to complete all sessions.
The main activity stage was comprised of activities for strengthening memory and management function and for increasing attention, concentration, and space-time, perception, concept formation and reasoning, composition, language, and computational abilities. Training information papers with fully explained cognitive training methods were provided to the participants and the methods on how to use the training were demonstrated. The program was selected such that the participant could have fun and interest, and help was provided if required by the participant. Initially, an easy level program was conducted for all participants. Then, the level was gradually increased to an appropriate level, and finally, a slightly difficult program was executed to match the difficulty level of the program and to develop interest and a sense of achievement and confidence among the patients. The memory was trained to strengthen the storage and withdrawal stages, which was a memory strategy that could be specifically developed and applied in the daily life of the participants. Attention training was focused on the activities of reading colors, finding the wrong or same picture, finding the models or letters in the same order, and memorizing the color and position of shapes. Activities for concept formation and reasoning comprised finding a common ground among objects and classifying them and finding similarities in categorization. The management function training involved finding the maze, drawing the same figure, matching the shapes and puzzles, constructing a symmetrical drawing, arranging the matches, and inferring a plan and three-dimensional figures. Activities for strengthening language ability included the use of a word search, word quiz, and participating in story making. In this section, the cognitive training aimed to maintain and enhance daily living performance and to maintain and enhance cognitive function by area.
All the activities concluded with an appreciation for participating in this session and next session guidance for upcoming sessions. During the cognitive training, the participants understood and talked about the strengths and deficiencies of their cognitive functions and support was provided for the difficulties, depression, and anxiety in daily life due to the noted cognitive decline as experienced by the participants.
Art therapy
The art therapy program comprised one 60-minute session per week that was conducted for the duration of 8 weeks. Art therapy was conducted structurally, focusing on reminiscence therapy that stimulates the memories of the participants. Each session program consisted of three phases: introductory activity, main activity, and finishing activity. The introduction activity was 10 minutes, and with regard to the greetings, it was possible to introduce it to the activity with a time to structurally recall information through questions related to session topics. In addition, the art media used in these sessions was explored and the use and method of using art materials was taught to the participants in order that the patients could access the activities smoothly. In the next 40-minute activity, the artist had to recall previous episodes through art activities, with a focus on strengthening concentration and helping the activity of coordination of vision and perception of the patients. The finishing activity was a 10-minute activity that involved appreciating the finished work and providing the title to it for participants to appreciate it, share their feelings, and experience a sense of accomplishment and positive emotions at the conclusion of the session. The whole program was divided into early, mid-term, and late activities that involved recalling stages from childhood to present. In the early activities, seniors were asked to recall the play they had enjoyed in childhood, and to make a detailed note of what was there was made. In the mid-term activities, the topic of adult life was composed. The Cheongsa Chorong Lantern used at the wedding ceremony were used to remind the participants of their marriage and after they recalled their motives and present life, they went on to work on art. In the latter period was a time available to recall the past life of the participants, using the natural media related to the season of the present life. In the last activity, participants made an album by printing photos of their works and activities performed during the therapy. These photos were sorted in the order of sessions, attached to the albums in sequence, and described on the speech bubble stickers to stimulate memories and preserve them for enjoyment and appreciation over a long-term timeframe.
Music therapy
The music therapy program was comprised one 60-minute session per week that was conducted for a total of 8 weeks. This program involved active music activities split into three phases: introductory activity, main activity, and finishing activity. The introductory activities consisted of providing opportunities for the participants to listen to hello songs and to play simple games. The Hello Song was a folk song written by a music therapist, created to announce the beginning of the program and to help build group intimacy among all participants. This activity consisted of therapeutic singing and instrumental performance. In this activity, folk songs, popular songs, arts songs, and nursery rhymes that were most preferred by Korean elderly individuals were used. First, in the therapeutic song singing activity, the participants had time to listen to or sing all of the prepared songs together, to share feelings, and discuss the meaning of the lyrics. Afterwards, each section was divided into groups and solos, and each group member sang in solo and proceeded in a solo-tutti structure performed in chorus. In addition, therapeutic singing included the creation of song lyrics by group members.
In the activity of instrumental, participants were expected to improvise on the rhythm. After presenting a variety of rhythmic instruments, participants selected their favorite instrument and tried to add their interpretation of the music as well as improvise on the rhythm presented to them on the therapist’s piano. Once the participant became accustomed to playing the instrument, the participants recognized their role in the solo-tutti structure and structured themselves to express themselves when performing along with other group members. In this activity, playing melody instruments such as colored handbells by looking at color scores was attempted by participants at that time.
These performances aided in developing the eye-hand coordination, an aesthetic sense of achievement, and helped the participants to gain confidence in task performance by playing acoustic instruments in their own-developed performances.
The finishing activity consisted of determining the activities performed under music therapy, briefly allowing the participants an opportunity for sharing their feelings, and letting them participate in singing the folk song “Jindo Arirang.” The participants responded to the therapist's question, “Well done, well done, what did you do well?” and the structured song. These “call & response” structure folk songs were structurally recognized by the participants as marking the end of the song.
Cognitive assessment and neuropsychological tests
Through this process, the Seoul Neuropsychological Screening Battery (SNSB), which is a structured cognitive function assessment tool for evaluating each domain of the cognitive function,18 was used as a basic examination. In this section, the Korean version of the Mini-Mental Status Examination (K-MMSE)18 and CDR were performed when the conduction of a detailed neuropsychological examination was difficult to complete. Additionally, a Korean Dementia Screening Questionnaire-Cognition (KDSQ-C)19 was administered to the patients to evaluate the cognitive function of the participants. Before and after patients underwent the integrated cognitive intervention therapy, Short Form of Geriatric Depression Scale (GDS),20 Beck Anxiety Inventory (BAI),21 and Seoul-Instrumental Activities of Daily Living (S-IADL)22 were used to assess the emotions and activities of daily living of each of the patients. The cut-off values were as follows: Short Form of GDS, 8 out of 15; BAI, 22 out of 63; S-IADL, 8 out of 45; and KDSQ-C, 6 out of 15. The follow-up cognitive assessment was done within 4 months of the study. In particular, the mean interval between baseline and follow-up was 2.2±0.8 months.
Statistical analysis
As observed, the change of cognition, ADL, and mood before and after the integrated cognitive intervention therapy was analyzed in the same patients by using a Wilcoxon signed rank test. Here it is noted that p≤0.05 indicated a statistical significance in this case. All analyses were performed using PASW Statistics 23 software (SPSS Inc., Chicago, IL, USA).
RESULTS
Among 59 participants, it was noted that 53 had mild AD with a CDR score of 0.5–1 and 6 had moderate AD with a CDR score of 2. The mean age of participants was 77.2±7.1 years, 72.9% of the participants were women, and the mean years of education were 7.2±4.2 years. Notably, the baseline K-MMSE score of the participants was 18.7±4.5 (Table 1).
Table 1. Demographic characteristics of participants.
| Demographic characteristics | Values | |
|---|---|---|
| No. of participants | 59 | |
| Age (yr) | 77.2±7.1 | |
| Female | 43 (72.9) | |
| Education (yr) | 7.2±4.2 | |
| Hypertension | 30 (50.8) | |
| Diabetes | 14 (23.7) | |
| Dyslipidemia | 12 (20.3) | |
| Medication | ||
| Acetylcholinesterase inhibitor | 41/49 (83.7) | |
| NMDA receptor antagonist | 2/49 (4.1) | |
| Anti-depressive medication | 11/49 (22.4) | |
| Anti-psychotics | 5/49 (10.2) | |
Data are shown as number (%) and continuous variables are presented as means±standard deviation.
NMDA: N-methyl-D-aspartic acid.
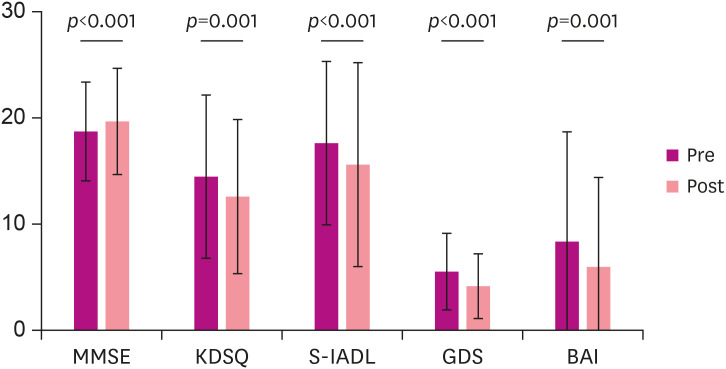
To begin with, the general cognitive assessment using K-MMSE improved from 18.7±4.5 before therapy to 19.7±5 after therapy (p<0.001), and the KDSQ-C improved from 14.5±7.6 before therapy to 12.6±7.2 after therapy. In addition, notable improvement in S-IADL scores was observed, from 17.6±7.6 before therapy to 15.7±9.5 after therapy (p<0.001). The GDS score before the integrated cognitive intervention therapy was 5.6±3.5, and that improved to 4.2±3.0 after the therapy (p<0.001). In this section, the number of patients with a GDS short form score indicating depression before therapy were 13 (22%), and that score decreased to 8 (13.6%) after the utilization of therapy. In this context, the BAI score decreased from 8.4±10.3 before therapy to 5.9±8.4 after therapy (p=0.001). Likewise, the number of patients with significant anxiety based on BAI were 6 (10.2%) before therapy and those evaluated after therapy were shown at 3 (5.1%) (Table 2 and Fig. 1).
Table 2. Comparison of cognitive scales between pre- and post-therapy.
| Tests | Pre-therapy | Post-therapy | p-value |
|---|---|---|---|
| K-MMSE | 18.7±4.5 | 19.7±5.0 | <0.001 |
| KDSQ-C | 14.5±7.6 | 12.6±7.2 | 0.001 |
| S-IADL | 17.6±7.6 | 15.7±9.5 | <0.001 |
| GDS, short form | 5.6±3.5 | 4.2±3.0 | <0.001 |
| BAI | 8.4±10.3 | 5.9±8.4 | 0.001 |
The continuous variables are shown in mean±standard deviation.
K-MMSE: Korean version of Mini Mental Status Examination, KDSQ-C: Korean version of Dementia Screening Questionnaire-Cognition, S-IADL: Seoul-Instrumental Activity of Daily Life, GDS: Geriatric Depression Scale, BAI: Beck Anxiety Inventory.
Fig. 1. Comparison of neuropsychological examination result between pre- and post-therapy.
Each neuropsychological scale improved after integrated cognitive intervention therapy. The Wilcoxon rank test was performed for comparing pre- and post-therapy scores. Where noted p indicates p-value for the Wilcoxon rank test.
K-MMSE: Korean version of Mini Mental Status Examination, KDSQ-C: Korean version of Dementia Screening Questionnaire-Cognition, S-IADL: Seoul-Instrumental Activity of Daily Life, GDS: Geriatric Depression Scale, BAI: Beck Anxiety Inventory.
In summary, the comparison between pre and post therapy scores of K-MMSE, KDSQ-C, S-IADL, GDS, and BAI indicated a significant improvement in cognitive functions, ADL, and patient mood after the implementation of the integrated cognitive intervention program.
DISCUSSION
The present study demonstrated the possibility of improvement in cognitive function, ADL, and mood of patients with probable AD, meeting the NINCDS-ADRDA criteria, who underwent integrated cognitive intervention therapy at the Centenarian's Good Memory School. Recently, large scale randomized controlled trials are investigating the effect of integrated programs that include an evaluation of the relationship between the assessment of vascular risk factors, diet, and exercise and provide cognitive training to participants with normal cognition or mild cognitive impairment (MCI).23,24,25 We developed an integrated program focused on cognitive training, art therapy, and music therapy, which was customized for patients with mild to moderate AD, considering where they were in their social and clinical conditions. Our findings suggested that this therapy is a beneficial tool that helps improve cognition, ADL, and can be seen to elevate the mood of the patients with mild to moderate AD.
Our study showed the cognitive outcome was improved after integrative cognitive therapy, although the effect of non-pharmacological treatment on cognition has been limited and controversial in previous studies.16 Consequently, the K-MMSE score was significantly improved after the use of the intervention. Because the practice effect of repeated cognitive tests might partly be different, we double-checked the subjective change of the cognitive function to identified caregivers using KDSQ-C. In these terms, the KDSQ-C score was also noted as being significantly higher than the baseline score. Considering that the existing pharmacological treatment cannot block the progress of AD and that the effect of integrative cognitive therapy has not been comprehensively studied, the improvement of cognitive function with integrative therapy in this study is revealed to be a noteworthy characteristic and result at this time.
Although the effect of non-pharmacological treatment on ADL function has not been studied comprehensively, our study demonstrated that the S-IADL score of patients was significantly improved after the therapy. If the integrative cognitive intervention can aid patients with AD to maintain a more beneficial ADL function, then it would aid these patients to independently perform ADL and delay the potential for the development of severe dementia, which is a serious burden to the caregiver and society on patients with that disease or to people exhibiting that condition. This is a noteworthy result because it adds evidence of the effect of non-pharmacological therapy on ADL function as existing the pharmacological treatment has only limited effect on ADL. Similar to studies on non-pharmacological interventions, the present study demonstrated that integrated cognitive intervention therapy including art and music therapies alleviated depression and anxiety in patients with mild to moderate AD. Art and music therapy can be applicable as a useful patient therapy regardless of education level, learning ability or cognitive status. Therefore, art and music therapies may more effective than utilizing the only cognitive training in clinically advanced patients who lack learning ability, or with less educated patients who are not familiar with written language. In addition, art and music therapies provide a chance to participate in social interaction among AD patients, who may be suffering from the experience of social isolation. Furthermore, drugs such as benzodiazepine6 or antipsychotics may have a harmful effect on the cognitive function of older AD patients. An effective integrated cognitive intervention therapy may reduce the necessity of having to utilize a prescription of benzodiazepine and antipsychotics in the older patient population demographic.
The strength of our study was that it demonstrated the possibility that the well-programmed integrated cognitive intervention therapy at the Centenarian's Good Memory School significantly improves cognitive function, ADL, and mood in patients with mild to moderate AD. However, we note that our study had some limitations. We did not use an amyloid biomarker to diagnose AD, and for this reason a certain degree of diagnostic uncertainty remains unclear at this time. Additionally, our study did not have a control group who did not take integrated cognitive intervention therapy for the same period; hence, the strength of the evidence is limited. Therefore, a randomized clinical trial investigating the long-term effect of integrated cognitive intervention therapy is warranted on the merits of these results. In addition, a future study should be followed to demonstrate that the domain integrative therapy (art+music+cognitive training) is more effective than the use of single or double domain interventions in these identified cases.
Nevertheless, our findings are noteworthy because they demonstrated the possibility that the integrated cognitive intervention therapy significantly improved cognitive function, ADL and mood in patients with mild to moderate AD, although a previous large-scale clinical trial on a non-pharmacological therapy had indicated the result of only a small effect size in MCI or general population at high risks in these cases.
In conclusion, this study demonstrated the possibility that the integrated cognitive program improved cognition, ADL, and mood in patients with mild to moderate AD. Further, this study suggested that the integrative cognitive program may be a viable supplementary treatment to be given along with an approved pharmacological therapy.
Footnotes
Funding: This research was supported by a grant of the Korea Health Technology R&D project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HI19C1132) and by the faculty grant of Myongji Hospital (2020-04-020).
Conflict of Interest: The authors have no financial conflicts of interest.
Author Contributions: Conceptualization: Jung YH, Lee S, Kim WJ, Lee JH, Kim MJ, Han HJ; Data curation: Jung YH, Lee S, Kim WJ, Lee JH, Kim MJ, Han HJ; Formal analysis: Jung YH; Investigation: Jung YH; Methodology: Jung YH, Lee S, Han HJ; Supervision: Lee S, Han HJ; Validation: Jung YH, Lee S, Kim WJ, Lee JH, Han HJ; Visualization: Jung YH; Writing - original draft: Jung YH, Lee S, Lee JH, and Han HJ; Writing - review & editing: Jung YH, Lee S, Lee JH, and Han HJ.
References
- 1.Wimo A, Guerchet M, Ali GC, Wu YT, Prina AM, Winblad B, et al. The worldwide costs of dementia 2015 and comparisons with 2010. Alzheimers Dement. 2017;13:1–7. doi: 10.1016/j.jalz.2016.07.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lyketsos CG, Olin J. Depression in Alzheimer's disease: overview and treatment. Biol Psychiatry. 2002;52:243–252. doi: 10.1016/s0006-3223(02)01348-3. [DOI] [PubMed] [Google Scholar]
- 3.Ferretti L, McCurry SM, Logsdon R, Gibbons L, Teri L. Anxiety and Alzheimer's disease. J Geriatr Psychiatry Neurol. 2001;14:52–58. doi: 10.1177/089198870101400111. [DOI] [PubMed] [Google Scholar]
- 4.Bianchetti A, Ranieri P, Margiotta A, Trabucchi M. Pharmacological treatment of Alzheimer's disease. Aging Clin Exp Res. 2006;18:158–162. doi: 10.1007/BF03327433. [DOI] [PubMed] [Google Scholar]
- 5.Schneider LS, Tariot PN, Dagerman KS, Davis SM, Hsiao JK, Ismail MS, et al. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer's disease. N Engl J Med. 2006;355:1525–1538. doi: 10.1056/NEJMoa061240. [DOI] [PubMed] [Google Scholar]
- 6.Tannenbaum C, Martin P, Tamblyn R, Benedetti A, Ahmed S. Reduction of inappropriate benzodiazepine prescriptions among older adults through direct patient education: the EMPOWER cluster randomized trial. JAMA Intern Med. 2014;174:890–898. doi: 10.1001/jamainternmed.2014.949. [DOI] [PubMed] [Google Scholar]
- 7.Chancellor B, Duncan A, Chatterjee A. Art therapy for Alzheimer's disease and other dementias. J Alzheimers Dis. 2014;39:1–11. doi: 10.3233/JAD-131295. [DOI] [PubMed] [Google Scholar]
- 8.Im ML, Lee JI. Effects of art and music therapy on depression and cognitive function of the elderly. Technol Health Care. 2014;22:453–458. doi: 10.3233/THC-140803. [DOI] [PubMed] [Google Scholar]
- 9.Choi AN, Lee MS, Cheong KJ, Lee JS. Effects of group music intervention on behavioral and psychological symptoms in patients with dementia: a pilot-controlled trial. Int J Neurosci. 2009;119:471–481. doi: 10.1080/00207450802328136. [DOI] [PubMed] [Google Scholar]
- 10.Suzuki M, Kanamori M, Watanabe M, Nagasawa S, Kojima E, Ooshiro H, et al. Behavioral and endocrinological evaluation of music therapy for elderly patients with dementia. Nurs Health Sci. 2004;6:11–18. doi: 10.1111/j.1442-2018.2003.00168.x. [DOI] [PubMed] [Google Scholar]
- 11.Vink AC, Zuidersma M, Boersma F, de Jonge P, Zuidema SU, Slaets JP. The effect of music therapy compared with general recreational activities in reducing agitation in people with dementia: a randomised controlled trial. Int J Geriatr Psychiatry. 2013;28:1031–1038. doi: 10.1002/gps.3924. [DOI] [PubMed] [Google Scholar]
- 12.Wall M, Duffy A. The effects of music therapy for older people with dementia. Br J Nurs. 2010;19:108–113. doi: 10.12968/bjon.2010.19.2.46295. [DOI] [PubMed] [Google Scholar]
- 13.Zhang Y, Cai J, An L, Hui F, Ren T, Ma H, et al. Does music therapy enhance behavioral and cognitive function in elderly dementia patients? A systematic review and meta-analysis. Ageing Res Rev. 2017;35:1–11. doi: 10.1016/j.arr.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 14.Han HJ, Son SJ, Ha J, Lee JH, Kim S, Lee SY. The effect of group musical therapy on depression and activities on daily living in patients with cognitive decline. Dement Neurocogn Disord. 2014;13:107–111. [Google Scholar]
- 15.Rusted J, Sheppard L, Waller D. A multi-centre randomized control group trial on the use of art therapy for older people with dementia. Group Anal. 2006;39:517–536. [Google Scholar]
- 16.Carrion C, Folkvord F, Anastasiadou D, Aymerich M. Cognitive therapy for dementia patients: a systematic review. Dement Geriatr Cogn Disord. 2018;46:1–26. doi: 10.1159/000490851. [DOI] [PubMed] [Google Scholar]
- 17.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 18.Kang SH, Park YH, Lee D, Kim JP, Chin J, Ahn Y, et al. The cortical neuroanatomy related to specific neuropsychological deficits in Alzheimer's continuum. Dement Neurocogn Disord. 2019;18:77–95. doi: 10.12779/dnd.2019.18.3.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang DW, Cho B, Chey JY, Kim SY, Kim BS. The development and validation of Korean dementia Screening questionnaire (KDSQ) J Korean Neurol Assoc. 2002;20:135–141. [Google Scholar]
- 20.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982-1983;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 21.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 22.Ku HM, Kim JH, Kwon EJ, Kim SH, Lee HS, Ko HJ, et al. A study on the reliability and validity of Seoul-Instrumental Activities of Daily Living (S-IADL) J Korean Neuropsychiatr Assoc. 2004;43:189–199. [Google Scholar]
- 23.A longitudinal follow-up of 550 mild cognitive impairment patients: evidence for large conversion to dementia rates and detection of major risk factors involved. J Alzheimers Dis. 2015;43:335. doi: 10.3233/JAD-159000. [DOI] [PubMed] [Google Scholar]
- 24.Yaffe K, Barnes DE, Rosenberg D, Dublin S, Kaup AR, Ludman EJ, et al. Systematic Multi-Domain Alzheimer's Risk Reduction Trial (SMARRT): study protocol. J Alzheimers Dis. 2019;70:S207–S220. doi: 10.3233/JAD-180634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Train the Brain Consortium. Randomized trial on the effects of a combined physical/cognitive training in aged MCI subjects: the Train the Brain study. Sci Rep. 2017;7:39471. doi: 10.1038/srep39471. [DOI] [PMC free article] [PubMed] [Google Scholar]