Graphical Abstract
Introduction
Clinical clerkship is facing major difficulties due to the coronavirus disease 2019 (COVID-19) pandemic. As of March 17, 2020, the Association of American Medical Colleges (AAMC) have provided guidelines suggesting that medical schools support suspending clinical rotations for medical students.1 Rose2 commented that the profound effect of COVID-19 may forever change how future physicians are educated. Due to the pandemic, medical students are not involved in patient care. Rose2 suggested that the culture of professionalism and altruism must be redefined taking into consideration even the effects of potential actions done with good intentions.
In all the medical schools (of 40 universities) in Korea, clinical clerkship is part of the curriculum for third- and fourth-year medical students, from February to December each year. The required 52-week period of clinical clerkship is regulated by the Accreditation Standards of Korean Institute of Medical Education and Evaluation (ASKIMEE).3 In mid-February 2020, all Korean medical schools suspended clinical clerkship courses due to the surge of COVID-19 patients in Daegu and Gyeongbuk, Korea. The Ministry of Education in Korea recommended to postpone the new semester until the 3rd week of March.4
Herein, we discuss our experience of teaching clinical clerkship safely from March to July 2020 at Department of Pediatrics, Gyeongsang National University Hospital and Jeonbuk National University Hospital in Korea. Primarily, for their own safety, medical students were prohibited in the respiratory clinic, the COVID-19 screening clinics, and primary community clinics. All courses except clinical clerkship continued via online as usual; clinical clerkship started on March 23, 2020. From March 2, 2020, medical students from all the regions were required to stay in their dormitories or at home. Using Self-Isolation App, the health conditions of the students such as body temperature and respiratory symptoms were monitored from March 2 to March 22, 2020. During the 5 days from March 23 to 27, 2020, faculty and medical students of all departments at hospitals had separate meetings in large classrooms.
Prior to entering the hospital, small group meetings were held in the classroom while wearing a mask and using hand sanitizers from time to time. The social accountability of health professionals was re-emphasized for patient safety. Medical students were reminded that they should take care of their own health, including maintaining social distancing at all times. These steps are unique from the past practices as these require medical students to demonstrate professionalism and altruism during the pandemic.
The guidelines for self-regulation before practicing clinical clerkship in the hospital are similar in all medical schools. All students should enter the hospital through only one gate after body temperature was checked and hands were washed. The new rules for students during hospital stay were as follows:
✓ Wear a mask.
✓ Do not go in groups of two or more when meeting a patient or patient's guidance.
✓ Wash hands frequently.
✓ Wear a nameplate with a photo ID.
During the 20 weeks of clinical clerkship, no medical student or medical staff was detected with COVID-19. All clerkships, such as patient interviews, physical examinations, bedside teaching, and skill practice, were carried out by medical students in outpatient clinics, inpatients, operation rooms, emergency rooms, and intensive care units (ICU), including neonatal ICU.
In addition, clinical skill examinations (CSE) were well conducted with standardized patients without any problems, as were the joint CSEs of universities all over the country. All third- and fourth-year medical students, professors, standardized patients (SP), and assistants participated and conducted CSEs wearing masks and ensured frequent use of hand sanitizer (Fig. 1). During CSE, a rule was enforced not to take off the mask. Therefore, oral examination was omitted or the examination findings were given to the students in cases where oral examination was required. Although a third-year medical student in Daegu was diagnosed with COVID-19 before the CSE,5 no one was infected during the CSE, in spite of close contact with SP over 30 days in a room. This is because all of them wore masks and washed hands with soap or sanitizers.
Fig. 1. Clinical performance examination. A medical student interviewing a standardized patient. Both of them wore masks.
Experiencing the real-world scenario is a key component of medical school education. It is highly recommended for the community-based curriculum for undergraduate students globally, as the communities require more support than tertiary hospitals.6,7 Most students responded that it was more interesting and accomplishing, as they can apply their knowledge and decision-making in direct contact with patients. This experience cannot be obtained from general practice in basic medicine. All the students did not reveal any discontent except for various missing patient cases.
Emerging Problems in Pediatric Clerkship
Decrease in number of pediatric patients
Pediatric clinical clerkship faces another barrier with a drastic decrease of up to 70% in pediatric patients visiting primary clinics and tertiary hospitals,8,9 even though the prevalence of flu has decreased in Korea.10 In Korea, common infectious diseases such as upper respiratory infection, hand-foot-mouth disease, and viral or bacterial pneumonia in children and adolescents, rapidly decreased,11 which may be related to suspension of classes, mask wearing, and correct and frequent hand washing. Most parents postponed the child's vaccination and routine development examination because they feared that their children might come in contact with the febrile patients in the hospital. Although this is a good approach for the chidren's health, it was problematic for educating medical students and for pediatric residents. Education of normal development or immunization is very important for pediatrics, but it was not possible to practice them at primary care.
Increase in parents' refusal to undergo medical students' examination
The reflection notes of students who finished pediatric clerkship showed the negative experience of parents' refusal or complaints about the meeting by medical students. University hospitals are tertiary hospitals; therefore, children with chronic diseases visit them or are hospitalized, and the fear of COVID-19 by parents of these children was immense. The only shortcoming is that medical students cannot experience more patients due to the pandemic of COVID-19. Therefore, during pediatric clinical clerkship, most students spent lots of their time checking for digital medical records.
Reduction of ward round with three or more medical students
As a part of social distancing, faculty's ward round with three or more medical students was not permitted. Faculty's bed-side teachings were performed with 1-2 medical students and 2-3 pediatric residents (Fig. 2). The grand rounds of the pediatric hospitalization ward, which is conducted by the entire pediatric clerkship students group, is the process in which students briefly present their patients, receive feedback, and learn while discussing with each other. This process was prohibited for the safety of hospitalized patients.
Fig. 2. Medical student examining the patient with his mother. Medical students and patient's mother wore masks.

Adaptations in Pediatric Clerkship Education
Due to the COVID-19, we had to change the schedule and curriculum of pediatric clinical clerkship, but retaining bedside teaching in the pediatric ward and NICU, the first-visit patient interview, and observation at the outpatient clinic.
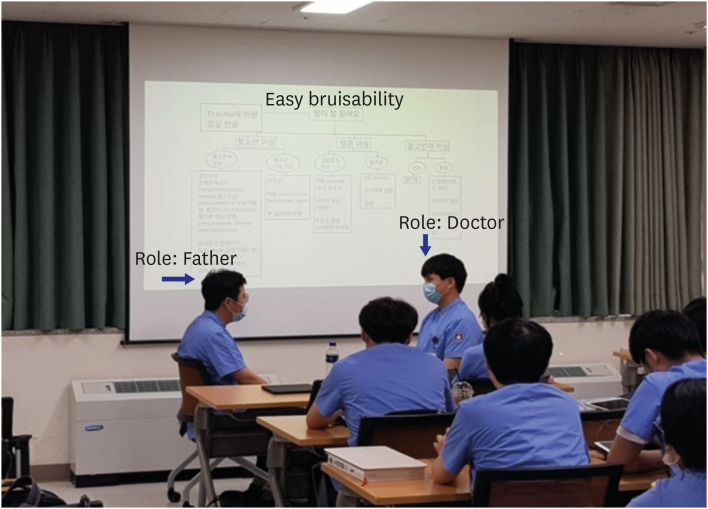
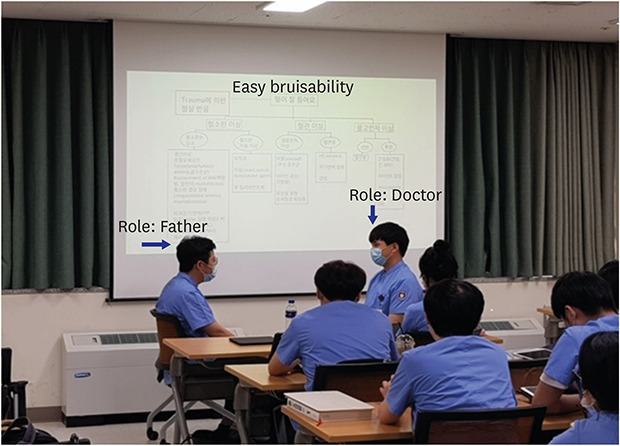
Actual patient encounter-based role play
Due to the decreased number of hospitalized pediatric patients, only one student within the student group (usually 3–4 students in a group) performed history taking and physical examination of the hospitalized patient with a guardian. Then, the student presented the patient's diagnosis and progress to the faculty. Using this real patient's present illness and laboratory findings, the student who conducted patient encounter acted as a parent, and another student acted as a doctor (Fig. 3).
Fig. 3. Role play after interview and physical examination with real patients presenting with easy bruisability. One student acted as patient's father and the second student acted as doctor. Other students observed the role play and discussed the case and role play.
Screen tests of development with an actual patient were also performed by only one student, and other students learnt via a case-based learning discussion.
Clinical performance-based role play
Vaccination appropriate for a given situation was applied and learned as a role play. We decided to teach the diseases seen in pediatrics through case-based learning, using photographs and online videos of typical cases. Skill practices such as intramuscular and subcutaneous injections were performed using the manikin. Hydration to a dehydrated infant was learnt in the simulation room. Physical examination was learnt by practicing with each other.
In the students' self-reflection notes after pediatric clerkship, the students found it more interesting and accomplishing to get to know patients' infirmities of medical history and physical examination, rather than learn typical cases through case-based learning. On the other hand, students preferred more discussions with the faculty about their own patients' medical history, physical examination, laboratory findings, and detailed feedback, compared with the previous years, along with a decreased number of patients.
Conclusion
Due to the COVID-19 pandemic, clinical practice today has changed, and social responsibility of medical students is an important factor in the continuation of their education. Detailed guidelines were provided by the schools and hospitals, and cooperation between patients and their caregivers was crucial. We should continue clinical practice in this way and hope that awareness and education on infectious diseases would be strengthened. It remains unclear if virtual patients would help or if SP, modeling, and role playing could be adopted in pediatric clinical practice. Predicting the type of disease that will be prevalent is impossible. However, doctors must be trained for better clinical performance at hospital and the community clinics. Despite the pandemic with high mortality, it is important to continue the clinical practice of medical students while taking measures to protect the patients, medical staff, and the students themselves.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Lee YM, Seo JH.
- Supervision: Lee YM, Park KD.
- Writing - original draft: Seo JH.
- Writing - review & editing: Lee YM, Park KD, Seo JH.
References
- 1.Association of American Medical College. Important guidance for medical students on clinical rotations during the coronavirus (COVID-19) outbreak. [Updated 2020]. [Accessed March 23, 2020]. http://www.aamc.org/news-insights/press-releases/important-guidance-medical-students-clinical-rotations-during-coronavirus-covid-19-outbreak.
- 2.Rose S. Medical students education in the time of COVID-19. JAMA. 2020;323(21):2131–2132. doi: 10.1001/jama.2020.5227. [DOI] [PubMed] [Google Scholar]
- 3.Korean Institute of Medical Education and Evaluation. The new standards for accredication. [Accessed June 21, 2020]. https://kimee.or.kr/en/standards/the-new-standards-for-accredication/
- 4.Ministry of Education. Briefing on new management of new coronavirus: Elementary and junior high schools opened on March 23, 2 weeks extra performance - Ministry of Education related to Corona 19. [Updated 2020]. [Accessed June 28, 2020]. https://www.moe.go.kr/boardCnts/view.do?m=020101&s=moe&page=2&boardID=339&boardSeq=79935&lev=0&opType=N.
- 5.New Daily. Daegu Keimyung University medical students, COVID-19 positive, 2020. May 30. [Updated 2020]. [Accessed August 13, 2020]. http://tk.newdaily.co.kr/site/data/html/2020/05/30/2020053000019.html.
- 6.Magzoub M, Schmidt HG. A taxonomy of community-based medical education: academic medicine. Acad Med. 2000;75(7):699–707. doi: 10.1097/00001888-200007000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Hideki W, Yasuyuki S. Learning from the curriculum of the University of Glasgow: Community-based medical education with an emphasis on general practice/primary care. Med Educ. 2011;42(6):371–374. [Google Scholar]
- 8.MEDICAL Observer. Direct hit (decreasing number of patients) of COVID-19 to pediatrics clinic, 2020 June 19. [Updated 2020]. [Accessed August 20, 2020]. http://www.monews.co.kr/news/articleView.html?idxno=211536.
- 9.Medigate News. In March, the closed pediatric clinic increased 1.8 times compared to the previous year. [Updated 2020]. [Accessed June 29, 2020]. http://www.medigatenews.com/news/3447311051.
- 10.Noh JY, Seong H, Yoon JG, Song JY, Cheong HJ, Kim WJ. Social distancing against COVID-19: Implication for the control of influenza. J Korean Med Sci. 2020;35(19):e182. doi: 10.3346/jkms.2020.35.e182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Korean Centers for Disease Control. Acute infectious disease pathogen monitoring information. 2020. July 30. [Updated 2020]. [Accessed September 9, 2020]. http://www.cdc.go.kr/npt/biz/npp/iss/hfmdcStatisticsMain.do.