Abstract
Background and Objective
Numerous actions have been taken to control the COVID-19 pandemic and reduce their morbidity and mortality. One of the most important measures in this regard is social distancing. However, there is limited evidence on the effectiveness of social distancing on COVID-19 incidence and mortality. Thus, the current study aimed to assess the effectiveness of social distancing measures on the COVID-19 incidence and mortality in Iran.
Materials and Methods
In the current quasi-experimental study, we evaluated the daily incidence cases and the number of deaths of COVID-19 in Iran before and after the implementation of social distancing measures. The segmented regression model was used to analyze the data. We also performed the interrupted time series (ITS) analysis using Newey ordinary least squares (OLS) regression-based methods.
Results
After the implementation of social distancing, the trend of both daily new cases and deaths due to COVID-19 was decreasing [(ß = −1.70 (95% CI = [−2.30 – −1.10; P < 0.001])) and (ß = −0.07 (95% CI = [−0.10 − −0.05; P < 0.001], respectively))].
Conclusion
Social distancing along with other public health interventions could reduce the morbidity and mortality of COVID-19 to some degrees, and it seems to be crucial to control the pandemic.
Keywords: COVID-19, social distancing, Iran, mortality, incidence
Introduction
Acute respiratory coronavirus 2 (SARS-COV-2) is the cause of evolving global pandemic coronavirus disease 2019 (COVID-19).1,2 Since its emergence, COVID-19 becomes a serious global public health and economic threat. World Health Organization (WHO) has been declared as a pandemic disease on 11 March 2020.3 It was initially identified in Wuhan, China in December 2019 as a case of pneumonia . Since that, it has spread across the world and reported from almost all countries within a few months. The global total confirmed cases have exceeded 21,107,157, and it killed 785,102 people on 14 August 2020 [Worldmeter].
The first COVID-19 related death was officially reported in Iran on 19 February 2020.4 As of 11 May 2020, 278,892 confirmed total cases and 6,640 deaths occurred in Iran due to COVID-19 . According to COVID-19 morbidity statistics, Iran was ranked 11th after the United States, Brazil, India, Russia, South Africa, Peru, Mexico, Colombia, Chile, and Spain.5
The Basic Reproductive Number (R0) which indicates the average number of people infected by each infected case in a susceptible population is an essential concept in the epidemiology of infectious diseases.6 This figure for the COVID-19 epidemic is 2.8 to 3.8 based on a meta-analysis conducted on Chinese studies.7 If we consider this number to be 3.5, about 56 million people in Iran as a country with a total population of more than 83 million in the Persian Gulf region will be infected.8 Moreover, an estimate showed that about 14% of infected cases could have a severe illness, and also 6% of them could be critical cases who require special care.9 Therefore, if no serious action is taken to reduce the transmissibility of the disease, probably 8 million hospital beds and 3 million special care facilities are required to treat severe cases in Iran.
Due to the absence of vaccines or drugs for COVID-19, the only effective method to control the disease is public health measures such as social distancing. Social distance measures were implemented in late March 2020 in Iran. Social distancing means reduced movement outside the home.10 That is used to reduce contacts between people in a community.11 This measure can delay the peak of the epidemic which could give a chance to the health-care system to be more prepared to contain pandemic.9
The National Committee to Combat Corona in Iran decided to close down shopping malls and big markets, sports places, and swimming pools, parks, and museums and even mosques, holy shrines, and Friday prayers.12 These measures followed by reduced mobility within provinces of Iran. Since social distance has a profound effect on the economic and social condition of the country, assessment of its effectiveness is necessary to support decision-makers. A study in China showed that when social distancing starts with only 1-day delay, 2.41 days will be added to the containment period.13 However, there is limited evidence on the effectiveness of social distancing measures on the incidence and mortality of COVID-19 in Iran.
Studies based on data from hospitalized patients showed that the mortality rate of COVID-19 is associated with older age, male gender, and underlying diseases such as diabetes, hypertension.14–16 Local forecasts based on different scenarios are crucial to enhance or take new control measures during epidemic. Due to limited evidence on this issue, the current study aimed to investigate the effectiveness of social distancing measures on the trend of morbidity and mortality of COVID-19 in Iran.
Materials and Methods
In the current quasi-experimental study, we used daily data on confirmed cases and death of COVID-19 from Feb 20, 2020, to May 13, 2020. All used data extracted from Our World in Data website that is available at https://ourworldindata.org/coronavirus. The data converted to a proportion (per 100,000 population). Interrupted time series (ITS) model used to assess the effect of social distancing on the incidence and mortality of COVID-19. The ITS is one of the appropriate models that could assess the short- and long-term effects of one or more interventions in quasi-experimental studies. In this model, the dependent variable is measured before and after the intervention. Our data included 84 observations of the deaths and COVID-19 confirmed cases that occurred in Iran during the mentioned period. Although social distancing started formally in the fourth week of March 2020, considering the Incubation period of this infection to better evaluation of the effect of this measure, April 9, 2020, is considered as the starting time of social distancing in our analysis. Finding on the incidence of COVID-19 in the Princess Diamond cruise ship shows that deaths began two weeks after the identification of the Index case.14 Thus, it is reasonable that one examines the effects of social distancing on mortality and morbidity rates after two-week of implementation. So, deaths and cases occurred before April 9, 2020, were considered as a baseline (control period), while death and cases occurred after April 9, 2020, as an intervention period. Segmented regression model and ITS analysis using Newey ordinary least squares OLS regression-based methods were used to model the under-studied data. The Newey approach estimates the coefficients by OLS regression, but due to possible heteroskedasticity and autocorrelations the Newey–West standard errors are used to handle them. To ensure the estimation of a model that accounts for the correct autocorrelation structure, the Actest, lag (6) were used to investigate autocorrelation and selection of best lags to model estimation. Due to the presence of autocorrelation error terms at lag 1 (P < 0.001) for both incidence and death of data, the primary model adjusted with lag (1). The standard ITS regression model is as follows:
 |
Yt is the aggregated number of cases/deaths that occurred at each equally spaced time point t, Tt is the time since the beginning of the study, Xt is a categorical variable representing the intervention (pre-intervention periods 0, otherwise 1), and XtTt is an interaction term. The β0 represents the intercept. β1 is the slope of the outcome variable before the start of the intervention. β2 represents the change in the level of the outcome that occurs in the period immediately after the start of the intervention (compared with the counterfactual). β3 represents the difference between pre-intervention and post-intervention slopes of the outcome. A significant β2 indicates an immediate effect, and significant β3 indicates an effect over time.17,18 Data were analyzed using StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC (USA).
Results
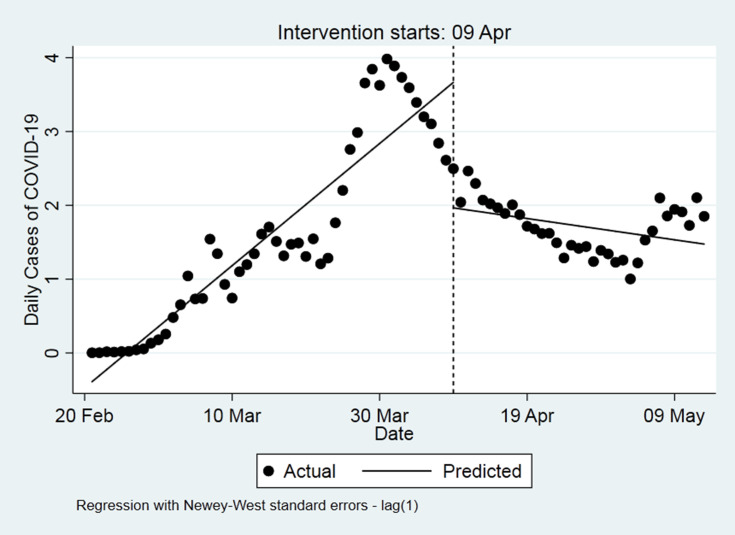
Figure 1 depicts the total number of confirmed cases and deaths of COVID-19 from February 20, 2020, to May 13, 2020. The starting point of the new cases of COVID-19 was estimated at −0.38, and the trend of new cases increase significantly every day until 9th April 2020 according to pre-intervention slope of (ß=0.08 (95% CI = [0.06–0.10]; P < 0.001)). After the intervention (social distancing) implementation the occurrence of new cases was significantly decreasing (ß = −1.70 (95% CI = [−2.30 – −1.10; P < 0.001])). The occurrence of new cases had a decreasing trend over the time after 9 April 2020 with a coefficient of −0.10 (95% CI = [−0.11– −0.07; P < 0.001])[Table 1]. Figure 2 shows the trend of COVID-19 cases occurrence before and after the implementation of social distancing in Iran. The trend of new cases of COVID-19 was increasing before the implementation of social distancing, however, after the implementation of social distancing, the occurrence of new cases is decreasing [Figure 2].
Figure 1.
The trend of deaths and new cases of COVID-19 in Iran since February 20, 2020, to May 13, 2020.
Table 1.
Estimated Coefficients of the Segmented Regression Model for New Cases (Proportion per 100,000 Population) of COVID-19 in Iran Since February 20, 2020, to May 13, 2020
| Regression with Newey-West Standard Errors Maximum Lag: 1 Number of Observation = 84 F (3, 80) = 90.78 p= 0.00001 | ||||||
|---|---|---|---|---|---|---|
| New Cases | Coefficients | Standard Error | t | P>t | [95% Confidence Interval] |
|
| Intercept | −0.38 | 0.11 | −3.40 | 0.001 | −0.61 | −0.16 |
| Pre intervention slope | 0.08 | 0.007 | 11.79 | <0.001 | 0.06 | 0.10 |
| Change in intercept | −1.70 | 0.29 | −5.70 | <0.001 | −2.30 | −1.10 |
| Change in slope (Interaction) | −0.10 | 0.01 | −9.33 | <0.001 | −0.11 | −0.07 |
| Post intervention linear trend | −0.01 | 0.008 | −1.79 | 0.07 | −0.03 | 0.001 |
Figure 2.
Segmented regression model for new cases (proportion per 100,000 population) of COVID-19 in Iran since February 20, 2020, to May 13, 2020, using the Newey-West standard errors.
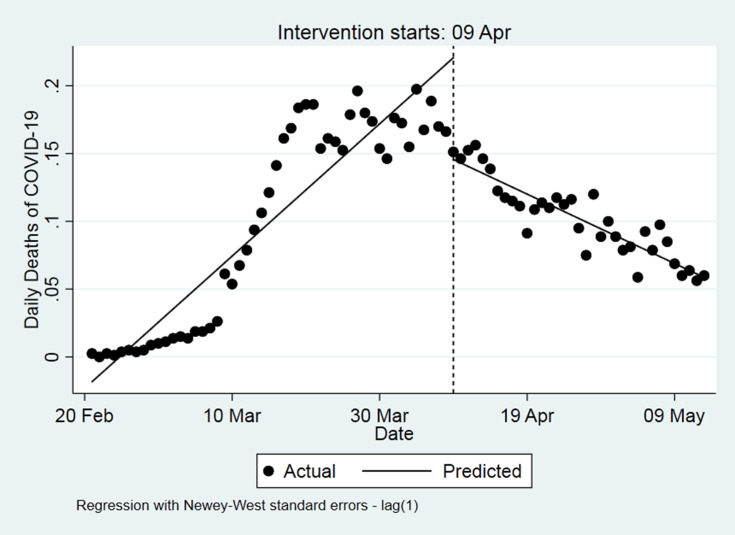
The proportion of COVID-19 deaths at the beginning of the study period is −0.01 [Table 2]. The trend of proportion of COVID-19 deaths was significantly increasing before the implementation of social distancing (9 April 2020) (ß = 0.005 (95% CI = [0.004–0.006]; P < 0.001)). The trend of COVID-19 deaths was significantly decreasing after the implementation of social distancing (ß = −0.07 (95% CI = [−0.10 – −0.05; P < 0.001])). The occurrence of new deaths had a decreasing trend over the time after 9 April 2020 with the coefficient (ß = −0.007 (95% CI = [−0.008− −0.006; P < 0.001])). Figure 3 shows the trend of deaths of COVID-19 cases before and after the implementation of social distancing. The trend of new deaths of COVID 19 was increasing before the implementation of the intervention (9 April 2020), but it was decreasing after the implementation of the intervention.
Table 2.
Estimated Coefficients of the Segmented Regression Model for Deaths (Proportion per 100,000 Population) of COVID-19 in Iran Since February 20, 2020, to May 13, 2020
| Regression with Newey-West Standard Errors Maximum Lag: 1 Number of Observation = 84 F (3, 80) = 131.18 p= 0.0000 | ||||||
|---|---|---|---|---|---|---|
| Death of COVID-19 | Coefficients | Standard Error | t | P>t | [95% Confidence Interval] |
|
| Intercept | −0.01 | 0.007 | −2.29 | 0.02 | −0.03 | −0.002 |
| Pre intervention slope | 0.005 | 0.0003 | 14.95 | <0.001 | 0.004 | 0.006 |
| Change in intercept | −0.07 | 0.01 | −5.99 | <0.001 | −0.10 | −0.05 |
| Change in slope(Interaction) | −0.007 | 0.0003 | −19.25 | <0.001 | −0.008 | −0.006 |
| Post intervention linear trend | −0.002 | 0.0002 | −11.91 | <0.001 | −0.03 | −0.002 |
Figure 3.
Segmented regression model for deaths (proportion per 100,000 population) of COVID-19 in Iran since February 20, 2020, to May 13, 2020, using the Newey-West standard errors.
Discussion
The results of the present study showed that social distancing significantly reduced the incidence and mortality of COVID-19 in Iran. Despite the increase in the number of cases before and the early days of social distancing implementation, there was a significant reduction after the implementation. However, a reduction in the occurrence of new COVID-19 cases since April 9, 2020 (after the implementation of social distancing) was steady. This finding is consistent with the incubation period of the infection.
An average estimated incubation period of COVID-19 is 5.1 days, and in most cases, the disease detected around the second week of the incubation period.19 Thus, some cases of the disease might have been infected in the days before the implementation of social distancing, and diagnosed after the implementation of the measure. Therefore, a significant reduction in the incidence of the disease was observed in 1–2 weeks after the implementation of social distancing. The present study retrospectively analyzed the data of the number of confirmed cases and COVID-19 mortality over 84 days.
The current study had some limitations. First, during the study period, some variables such as the definition of the case and accuracy of the diagnostic tests may be changed and this could affect the effectiveness of the intervention positively or negatively. Second, some variables such as the level of the population knowledge regarding COVID-19, the extent to which people have access to the health-care system, and their compliance with health principles could affect the effectiveness of social distancing. However, since data on these variables were not available, controlling their role was not possible. Third, unregistered infected individuals are likely to maintain the disease transmission cycle in families 21,20 which obscure the effectiveness of social distancing.
Despite the economic, psychological impacts of social distancing measures,22,23 its role in containing the pandemic is undeniable. However, social distancing should be implemented with caution and greater sensitivity due to its extreme effect it imposes on the socioeconomic status of a country. Therefore, social distancing and other prevention programs could prevent the mortality and morbidity of Iranians population to some degree. Other measures such as case finding, isolation and contact tracing, encourage people to use a face mask and follow the principles of personal hygiene, especially hand washing, in addition to social distancing could help fight the pandemic. A study conducted in China24 suggests that after an intense social distancing, they effectively exited their lockdown. Again in China, it has been reported that the prevention strategies based on non-pharmaceutical interventions were effective.25
Conclusion
The present study suggests that social distancing could decrease the incidence and mortality related to COVID-19. Thus, it is necessary to continue these measures, because if the government plan to reduce the social distancing measures the occurrence of the next waves of the epidemic will be inevitable.
Disclosure
The authors report that there is no conflicts of interest in this work.
References
- 1.WHO. Naming the coronavirus disease (COVID-19) and the virus that causes it. April 10, 2020. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(COVID-2019)-and-the-virus-that-causes-it. Accessed August31, 2020.
- 2.Nikpouraghdam M, Farahani AJ, Alishiri G, et al. Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in IRAN: a single center study. J Clin Virol. 2020;127:104378. doi: 10.1016/j.jcv.2020.104378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. Novel-coronavirus-2019/events-as-they-happen 2020. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Accessed March12, 2020.
- 4.Takian A, Raoofi A, Kazempour-Ardebili S. COVID-19 battle during the toughest sanctions against Iran. Lancet. 2020;395(10229):1035–1036. doi: 10.1016/S0140-6736(20)30668-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.world meters. 2020. Available from: https://www.worldometers.info/coronavirus/#countries. Accessed April10, 2020.
- 6.Alimohamadi Y, Sepandi M. Basic reproduction number: an important indicator for the future of the COVID-19 epidemic in Iran. J Mil Med. 2020;22:96–97. [Google Scholar]
- 7.Alimohamadi Y, Taghdir M, Sepandi M. The estimate of the basic reproduction number for novel coronavirus disease (COVID-19): a systematic review and meta-analysis. Korean J Prev Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.worldometers. Iran Demographics. 2020. Available from: https://www.worldometers.info/demographics/iran-demographics/. Accessed April10, 2020.
- 9.Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395:931–934. doi: 10.1016/S0140-6736(20)30567-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Afrashteh S, Alimohamadi Y, Sepandi M. The role of isolation, quarantine and social distancing in controlling the COVID-19 epidemic. J Mil Med. 2020;22:210–211. [Google Scholar]
- 11.Gharebaghi R, Heidary F. COVID-19 and Iran: swimming with hands tied! Swiss Med Wkly. 2020;150. [DOI] [PubMed] [Google Scholar]
- 12.Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20(6):669–677. doi: 10.1016/S1473-3099(20)30243-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Du Z, Xu X, Wang L, Fox SJ, Cowling BJ, Galvani AP, et al. Effects of Proactive Social Distancing on COVID-19 Outbreaks in 58 Cities, China. Emerging infectious diseases. 2020;26:2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Russell TW, Hellewell J, Jarvis CI, et al. Estimating the infection and case fatality ratio for coronavirus disease (COVID-19) using age-adjusted data from the outbreak on the Diamond Princess cruise ship, February 2020. Eurosurveillance. 2020;25:2000256. doi: 10.2807/1560-7917.ES.2020.25.12.2000256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2). Science. 2020;368(6490):489–493. doi: 10.1126/science.abb3221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qiu H, Wu J, Hong L, Luo Y, Song Q, Chen D. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect Dis. 2020;20(6):689–696. doi: 10.1016/S1473-3099(20)30198-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Piroozi B, Takian A, Moradi G, Amerzadeh M, Safari H, Faraji O. The effect of Iran’s health transformation plan on utilization of specialized outpatient visit services: an interrupted time series. Med J Islam Repub Iran. 2018;32:121. doi: 10.14196/mjiri.32.128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rashidian A, Moradi G, Takian A, et al. Effects of the health transformation plan on caesarean section rate in the Islamic Republic of Iran: an interrupted time series. East Mediterr Health J. 2019;25(4):254–261. doi: 10.26719/emhj.18.044 [DOI] [PubMed] [Google Scholar]
- 19.Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172(9):577–582. doi: 10.7326/M20-0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li R, Pei S, Chen B, Song Y, Zhang T, Yang W, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2). Science 2020;368( 6490):489–493. doi: 10.1126/science.abb3221 [DOI] [PMC free article] [PubMed]
- 21.Qiu H, Wu J, Hong L, Luo Y, Song Q, Chen D. Clinical and epidemiological features of 36 children with coronavirus disease 2019. (COVID-19) in Zhejiang, China: an observational cohort study. The Lancet Infectious Diseases; 2020;20(6):689–696. doi: 10.1016/S1473-3099(20)30198-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Monit. 2020;26:e923921. doi: 10.12659/MSM.923921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ainslie KE, Walters CE, Fu H, Bhatia S, Wang H, Xi X, et al. Evidence of initial success for China exiting COVID-19 social distancing policy after achieving containment. Wellcome Open Research 2020; 5(81):1–10. doi: 10.5281/zenodo. 3751005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lai S, Ruktanonchai NW, Zhou L, Prosper O, Luo W, Floyd JR, et al. Effect of non-pharmaceutical interventions for containing the COVID-19 outbreak in China. Nature 2020. doi: 10.1038/s41586-020-2293–x. [DOI] [PMC free article] [PubMed]