Abstract
Background
The present study is a prospective observational single arm clinical investigation, with parallel bench test interrogation, aimed at investigating the technical feasibility, safety and clinical outcomes with the cone flare crush modified-T (CFCT) bifurcation stenting technique. Bifurcation percutaneous coronary intervention (PCI) remains an area of ongoing procedural evolution. More widely applicable and reproducible techniques are required.
Methods
From April 2018 until March 2019, 20 consecutive patients underwent bifurcation PCI using the CFCT technique with a Pt-Cr everolimus drug-eluting stent with a bioresorbable polymer. Exercise stress echocardiography was performed at 12-month follow-up. The primary outcome was a composite of cardiac related mortality, myocardial infarction, target lesion/vessel revascularization and stroke. Safety secondary endpoints included bleeding, all-cause mortality and stent thrombosis.
Results
All patients underwent a successful CFCT bifurcation procedure with no complications to 30-day follow-up. One patient met the primary endpoint requiring target lesion revascularization at 9 months for stable angina. There were no other primary or secondary outcome events in the cohort. There were no strokes, deaths, stent thrombosis or myocardial infarction during the follow-up period. The mean CCS score improved from 2.25 to 0.25 (p < 0.0001). Optical coherence tomography (OCT) and bench test findings indicated optimal side branch ostial coverage and minimal redundant strut material crowding the neo-carina.
Conclusions
The CFCT technique appears to be a safe, efficacious and feasible strategy for managing coronary artery bifurcation disease. Expanded and randomized datasets with longer term follow-up are required to further explore confirm this feasibility data. (ANZCTR ID: ACTRN12618001145291).
Keywords: Percutaneous Coronary Intervention (PCI), Stenting technique (STEC), Drug Eluting Stent (DES)
Abbreviations: ACS, Acute coronary syndrome; ACT, Activated clotting time; AHA, American Heart Association; ARC, Academic Research Consortium; BARC, British Academic Research Consortium; CABG, Coronary artery bypass grafting; CCS, Canadian Cardiovascular Society; CFCT, Cone Flare Crush Modified-T; CFI, Cone Flare Inflation; DAPT, Dual antiplatelet therapy; DES, Drug Eluting Stent; DMV, Distal main vessel; DSE, Dobutamine stress echocardiography; ESE, Exercise stress echocardiography; ISKB, Intermediary simultaneous kissing balloon; ISR, In stent restenosis; LAD, Left anterior descending artery; LCx, Left circumflex artery; LMCA, Left main coronary artery; MACCE, Major adverse cardiac and cerebrovascular event; MI, Myocardial infarct; MRA, Mechanical rotational atherectomy; MV, Main Vessel; NSTEMI, Non-ST elevation Myocardial Infarction; NYHA, New York heart association; OCT, Optical coherence tomography; PCI, Percutaneous Coronary Intervention; PMV, Proximal main vessel; POT, Proximal Optimisation Technique; PUKBI, Penultimate kissing balloon inflation; QCA, Quantitative Coronary Angiography; RBP, Rated Burst Pressure; SB, Side Branch; SEM, Standard Error of the mean; ST, Stent thrombosis; STEMI, ST elevation Myocardial Infarction; SYNTAX, Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery; TLR, Target Lesion Revascularisation; TVR, Target Vessel Revascularisation; UAP, Unstable angina pectoris
1. Introduction
Bifurcation percutaneous coronary intervention (PCI) remains an area of ongoing procedural evolution and active research [1]. Multiple bifurcation strategies have been studied however bifurcation PCI continues to be heterogeneously managed with approaches that vary between operators, institutions and geographies. Dedicated two-limb pre-fabricated bifurcation stents have not been established to be adequately efficacious and are not widely available commercially [2], [3]. Numerous provisional and upfront two-stent approaches have been assessed in registry and clinical trial settings with variable results [4], [5], [6], [7], [8], [9], [10], [11]. Clinical outcome data suggests that a single stent provisional side-branch technique, outside of the left main bifurcation setting, should be the preferred approach [12], [13], [14]. Countervailing this, an a priori two-stent technique is frequently employed because of concern around the risk of irretrievable side-branch loss or the clinical significance of the side branch disease itself [15], [16], [17], [18]. The strategy employed varies depending on operator preference, anatomical considerations and relative vessel sizes [8], [19]. The cone flare crush modified-T (CFCT) bifurcation technique is a modified double kiss double-crush (DK-Crush) strategy and has been adopted by some operators as a default strategy where an upfront two-stent approach is deemed necessary [20]. The technique offers the potential for greater predictability for side-branch re-access for kissing balloon inflations (with less stent material in the peri-bifurcation region) and is potentially applicable to all bifurcation angles.(5) This study is a prospective observational single arm cohort investigation to examine the safety, technical feasibility and clinical outcomes with the implementation of the CFCT technique. The clinical data is complemented by intravascular imaging and bench test findings [21].
2. Methods
2.1. Study population
The CFCT study is a prospective investigator initiated single arm registry of twenty consecutive patients planned to undergo an upfront two-stent bifurcation stenting strategy utilizing a resorbable polymer third generation drug eluting stent (DES) with a platinum-chromium (Pt-Cr) based platform design (SYNERGY, Boston Scientific Inc, Marlborough, MA, USA). The study was approved by the relevant institutional human research and ethics committee (HREC) and all patients provided informed consent in-line with the Declaration of Helsinki and in accordance with the guidelines of the American Physiological Society [22]. The study was registered with the Australian and New Zealand Clinical Trial Registry (ANZCTR ID number, ACTRN12618001145291). Clinical, demographic and procedural data was collected prospectively and entered into a central database as per the study protocol. Data collection was assisted by interrogation of the electronic medical record (EMR) system in place at our institution (Cerner Inc, Kansas, MO, USA). For each patient the Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX) score was calculated [23]. Angiographic variables assessed included lesion location and bifurcation type (Medina classification), presence of calcification and American Heart Association (AHA) lesion grade [24], [25]. Procedural time, contrast load and fluoroscopy doses were collected in addition to the number of stents, stent lengths and diameters.
Consecutive patients over the age of 18 at our institution who were planned to undergo a CFCT bifurcation technique using a Pt-Cr everolimus DES with a bioresorbable polymer in a non-emergent setting were eligible for enrollment. Patients were excluded if they were unable to take dual antiplatelet therapy, were undergoing primary PCI for STEMI (or rescue PCI for failed fibrinolysis), or did not have capacity to provide informed consent.
2.2. Description of the CFCT technique
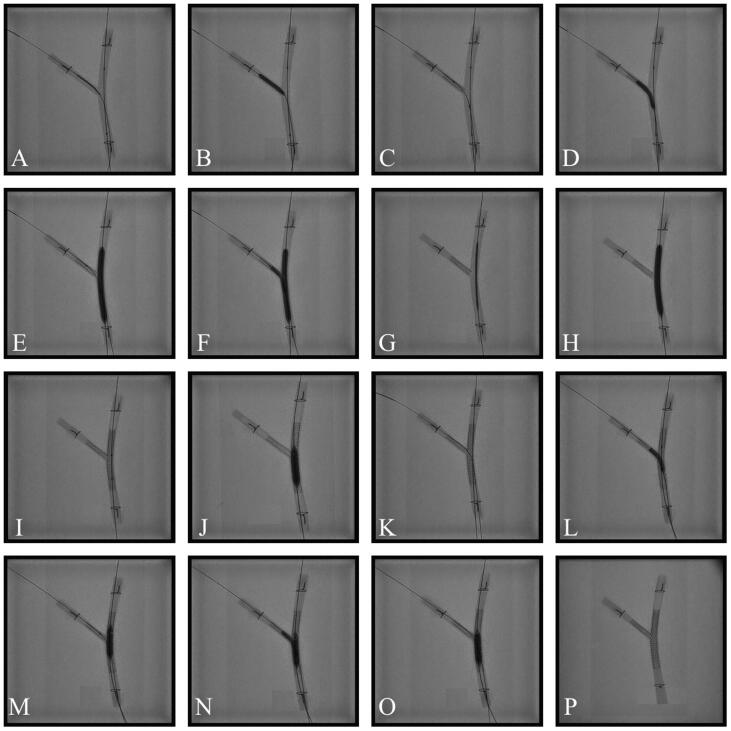
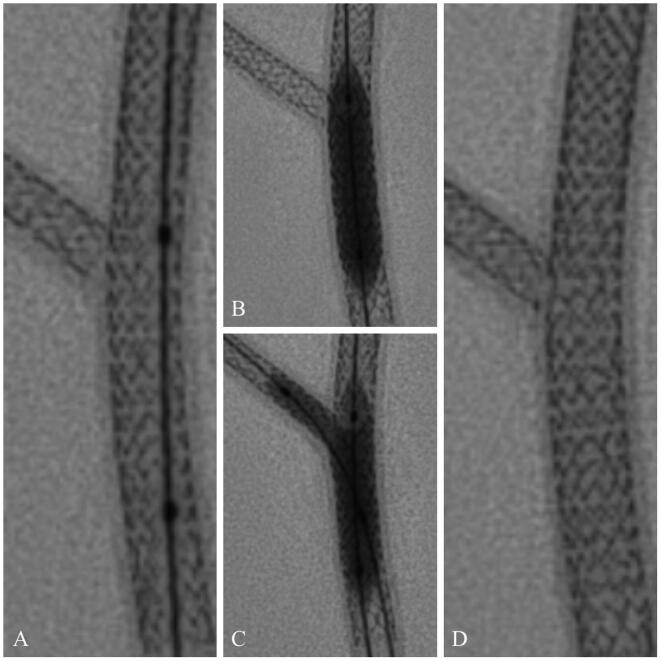
The original form of the CFCT technique was initially described by Rajdev et al. [20]. The modified version of this technique involves the following steps (and is displayed in Fig. 1):
-
1.
Stenting of the side-branch (SB) is performed first (with pre-dilatation if required) with an iso-sized semi-compliant balloon in the main vessel (MV) sized to the vessel distal to the bifurcation.
-
2.
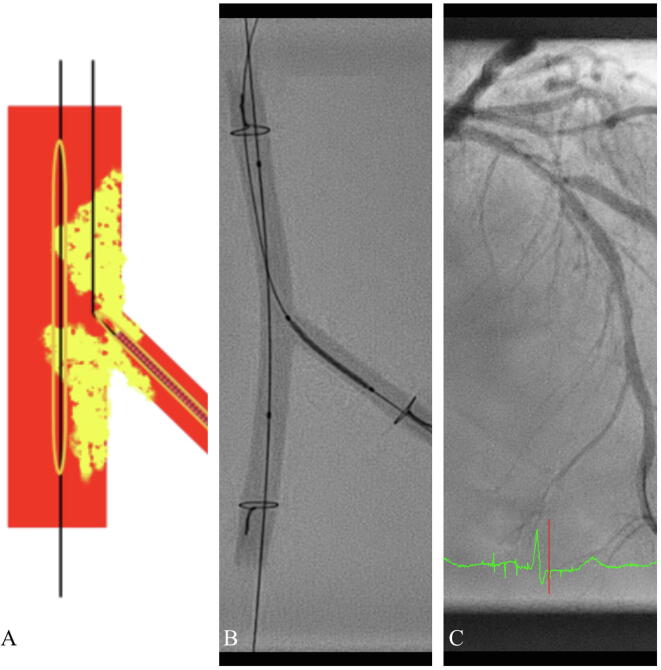
Side-branch (SB) ostial stent placement is positioned so that the proximal end of the stent extends back to the SB-ostium distal vertex only (as shown in Fig. 2) and is deployed at nominal pressure.
-
3.
The stent balloon is then pulled back 50 – 70 per cent of its length and inflated for the ‘cone flare’ inflation to rated burst pressure (RBP). Following SB balloon deflation, the MV semi-compliant balloon is then inflated to between nominal and RBP, at operator discretion, and an intermediary simultaneous kissing balloon (ISKB) inflation is performed to between 6 and 8 atm.
-
4.
The SB wire and stent balloon are then removed. The MV balloon is then ‘jogged’ backward and forward to predict ease of MV stent passage with any resistance leading to further MV inflations before MV balloon removal.
-
5.
The MV balloon is then removed and the main vessel stent positioned and deployed at a pressure at operator discretion (usually between nominal and RBP).
-
6.
Murasato optimal proximal optimization technique (POT) is then performed on the MV stent, using an iso-sized (to the vessel proximal to the bifurcation) non-compliant balloon, prior to re-wiring of the SB [26]. The SB is re-accessed and a balloon iso-sized to the SB stent is positioned across the ostium of the SB. Sequential inflations are then performed in the SB and MV followed by a penultimate kissing balloon inflation (PUKBI) to 6 – 8 atm. A final POT inflation is then performed in the MV.
-
7.
Optical coherence tomography (OCT) is then performed on the MV and SB to document stent expansion and apposition [27].
Fig. 1.
(A) Optimal SB stent positioning. (B) SB stent deployment. (C) Balloon retracted for flare. (D) Flare inflation. (E) Crush inflation. (F) First KB inflation. (G) MV stent positioning with side branch wire removed. (H) MV stent deployment. (I) Murasato POT positioning. (J) Initial POT. (K) SB rewired. (L) Post-dilatation of SB. (M) Post dilatation of MV. (N) Penultimate KB inflation. (O) Final POT. (P) Final result.
Fig. 2.
(A) Illustration. (B) Bench test. (C) Angiographic appearance.
2.3. Study outcomes
The primary outcome was a composite outcome of cardiac related mortality, non-fatal myocardial infarction (MI), target lesion or target vessel revascularization (TLR/TVR) and stroke at 12 months. Secondary endpoints included the individual components of the primary outcomes in addition to safety outcomes of bleeding (BARC 2–5), all-cause mortality and Academic Research Consortium (ARC) defined stent thrombosis (ST) [28], [29]. Peri-procedural MI was defined as per contemporary PCI studies but also in accordance with ARC recommendations [29], [30], [31]. Symptom data was also recorded using the Canadian Cardiovascular Society (CCS) score for angina at baseline and follow-up reviews [32]. Quantitative coronary angiography (QCA) data was recorded pre and post-PCI. Data was analyzed using descriptive statistics with findings expressed as mean ± standard error of the mean (SEM) unless other specified. Data comparisons were done with Student’s T test for continuous variables and Pearson’s chi-squared test for categorical variables with SPSS Version 26 (SPSS Institute Inc, Chicago, IL, USA).
2.4. Follow up
Follow-up data was obtained during outpatient clinic visits (in person or via telehealth link) at 1, 6 and 12 months. All patients underwent an exercise stress echocardiogram (ESE) at 12-month follow-up on guideline mandated medical therapy including beta-blockade with invasive coronary angiography for all patients who had a result suggestive of inducible ischemia (but not for submaximal or equivocal studies without definite ischaemic features). Patients who could not exercise due to mobility or other issues underwent a dobutamine stress echocardiogram (DSE).
2.5. Bench testing Methods
Bench testing was performed employing consensus principles [33]. Two pre-fabricated separate bifurcation models representing narrow and wide bifurcation angles (30° and 70° respectively) were used (Terumo Inc, Tokyo, Japan). They both consisted of clear polyurethane tubing affixed to a transparent PerspexTM plate via stainless-steel ties. The 30° model had 4.0 mm proximal MV (PMV), 3.0 mm distal MV (DMV) and 3.0 mm SB lumens. The 70° model had 3.5 mm PMV and DMV lumen with a 2.5 mm SB lumen.
The models were bathed in water on our catheter laboratory table and fluoroscopic images were taken with a Philips Allura Clarity imaging system (Koninklijke Philips NV, Amsterdam, Netherlands). A Balance Middle Weight 0.014″ Elite wire (Abbott, Chicago, IL, USA) was used in the MV and a PT2 Light Support 0.014″ wire (Boston Scientific Corporation, Marlborough, MA, USA) in the SB. CFCT was performed in the sequence described above. The testing was performed with a 4.0 × 38 mm SYNERGY DES for the MV and a 2.5 × 12 mm SYNERGY DES in SB for both models. The stepwise sequence of the bench model is shown in the image panel in Fig. 1.
2.6. Funding source and role of sponsor
The CFCT study is an investigator-initiated prospective registry. An institutional grant to cover registry costs was provided by Boston Scientific Corporation (Marlborough, MA, USA). Terumo Corporation (Tokyo, Japan) provided pre-fabricated bench-testing models. The study structure, design and subsequent manuscript were prepared by the listed investigators. The study sponsor was given the opportunity to review the completed manuscript. All final decisions about manuscript content were made by the authors.
3. Results
3.1. Baseline characteristics
The baseline characteristics are reported in Table 1. The mean age was 64.84 ± 2.23 years with 25% of female gender. Cardiac risk factors included hypertension and dyslipidemia in 12 patients (60%) and diabetes in 6 (30%). 14 patients had a history of current or prior smoking. Remote prior MI had occurred in 5 (25%) patients with 2 (10%) having undergone remote prior PCI. PCI was performed for acute coronary syndrome (ACS) in 45% of patients (NSTEMI n = 8, UAP n = 1). Most patients were taking statin therapy prior to PCI (90%) and all were loaded with DAPT prior to the PCI procedure.
Table 1.
Baseline clinical characteristics of study participants.
| Clinical characteristics | |
|---|---|
| Number of patients | 20 |
| Mean age (years) | 64.85 (±2.23) |
| Mean BMI (kg/m2) | 28.5 (±1) |
| Male | 15 (75%) |
| Diabetic | 6 (30%) |
| Smoker | 19 (95%) |
| Hypertension | 12 (60%) |
| Dyslipidemia | 12 (60%) |
| Previous PCI | 2 (10%) |
| Cr Clearance (ml/min) | 67.5 ± 10.8 |
| Periprocedural LVEF (%) | 54% ± 1.9 |
| Baseline CCS | 2.25 ± 0.38 |
| Baseline NYHA | 1.2 ± 0.52 |
| Indication | |
| NSTEMI | 8 (40%) |
| Unstable Angina | 1 (5%) |
| Stable Angina | 11 (55%) |
| Medications | |
| DOAC/VKA | 4 (20%) |
| Aspirin | 18 (90%) |
| Clopidogrel | 16 (80%) |
| Prasugrel | 4 (20%) |
| ACE Inhibitor/ARB | 16 (80%) |
| Statin | 20 (100%) |
| Beta blocker | 14 (70%) |
Abbreviations: BMI, body mass index; Cr, creatinine; PCI, percutaneous Coronary Intervention; CCS, Canadian Cardiovascular Society angina grade; NYHA, New York Heart Association functional score; DOAC, direct oral anticoagulant; LVEF, left ventricular ejection fraction; NSTEMI, Non ST segment elevation myocardial infarction; VKA, Vitamin K antagonist; ACE, Angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker. Data are shown as mean ± standard error of the mean or as n (%).
3.2. Procedural characteristics
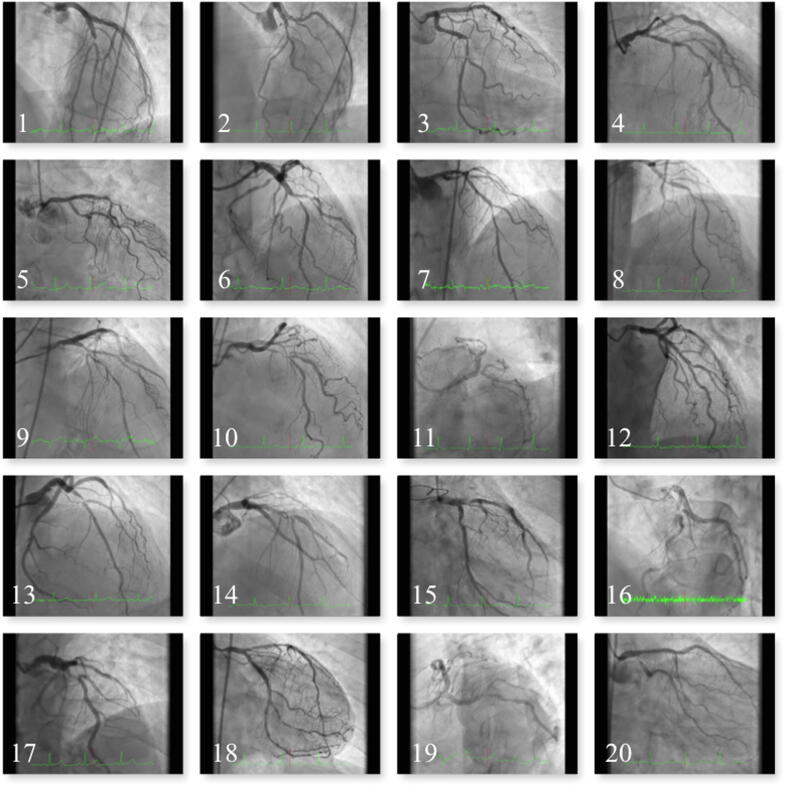
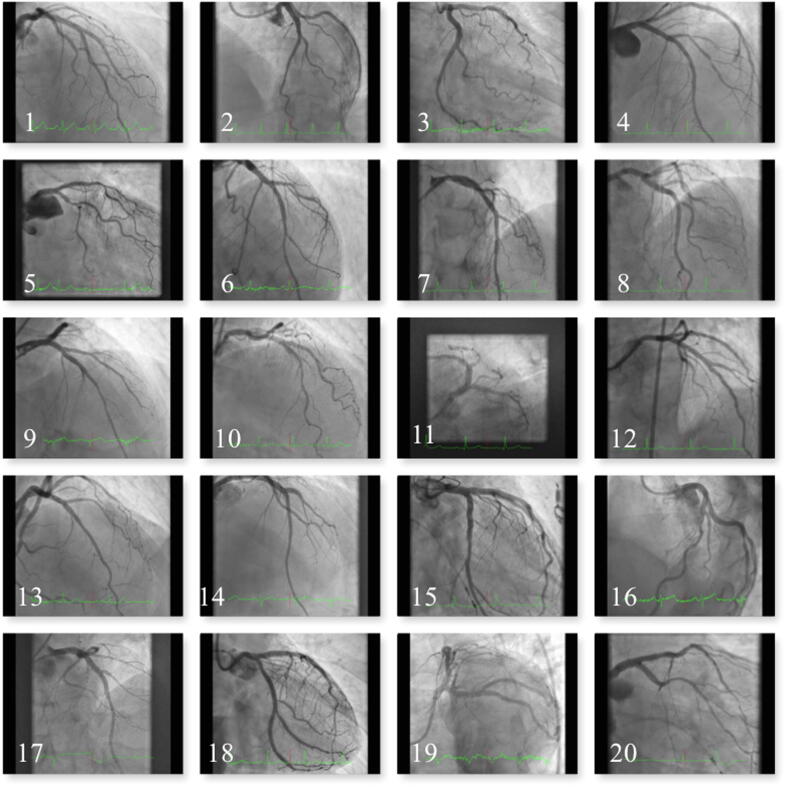
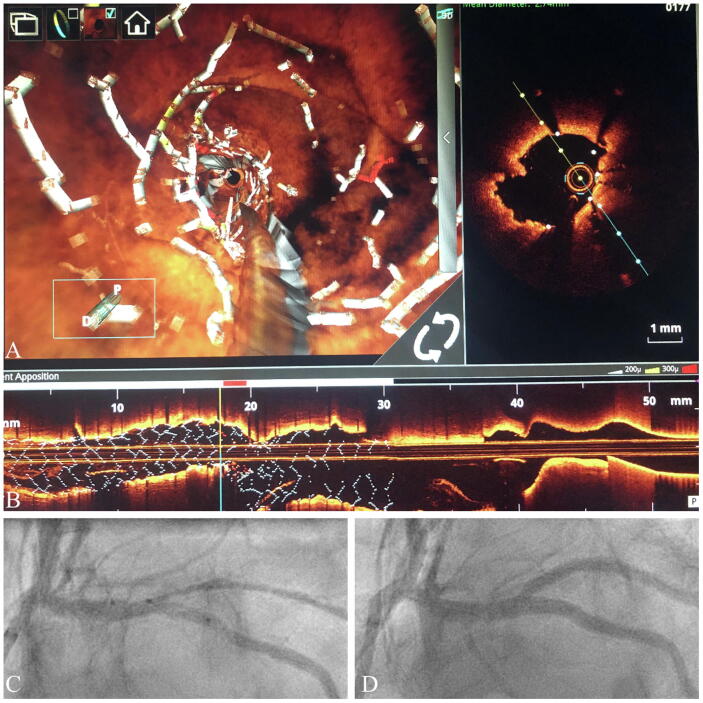
Procedural characteristics are shown in Table 2. The mean fluoroscopy time was 35 min. The median SYNTAX score was 27.9 ± 2.73. Medina 1,1,1 bifurcation disease made up 70% (n = 14) of the cohort. LAD/diagonal bifurcation disease accounted for 70% of cases (n = 14) while 10% were located in the distal LMCA (n = 2). Mechanical rotational atherectomy (MRA) was performed in 15% (n = 3) patients. The average number of stents was 2.35 ± 0.1. Penultimate kissing balloon inflations (PUKBI) were achieved in all patients (with a final POT inflation following this in all cases). Fig. 3, Fig. 4 are panels that display the pre and post-PCI angiographic appearances for all patients. OCT was performed at the conclusion of all cases to confirm adequate stent apposition and expansion (Fig. 5, Fig. 6 display representative OCT findings). All procedures were performed with intraprocedural unfractionated heparin (target ACT 250 – 300) with no use of glycoprotein IIb-IIIa inhibitors or bivalirudin. QCA data is presented in Table 3.
Table 2.
Procedural and lesion characteristics of study participants.
| SYNTAX score | |
|---|---|
| Mean Baseline SYNTAX score | 27.87 ± 2.73 |
| SYNTAX 0–22 | 7 (35%) |
| SYNTAX 22–32 | 7 (35%) |
| SYNTAX > 32 | 6 (30%) |
| Location of Bifurcation | |
| Left Main | 4 (20%) |
| LAD | 13 (65%) |
| LCx | 3 (15%) |
| Medina | |
| 1,1,1 | 15 (75%) |
| 1,0,1 | 1 (5%) |
| 0,1,1 | 4 (20%) |
| Calcified vessel | 10 (50%) |
| TIMI Flow Grade | |
| TIMI 1 | 0 |
| TIMI 2 | 0 |
| TIMI 3 | 20 (100%) |
| Procedure Characteristics | |
| Radial Access | 14 (70%) |
| Rotablation | 5 (25%) |
| 7F guide | 18 (90%) |
| 6F guide | 2 (10%) |
| Multivessel PCI | 2 (10%) |
| Procedural time (mins) | 102.8 (±7.23) |
| Fluroscopy time (mins) | 35 ± 1.97 |
| Contrast volume (mls) | 335.6 ± 22.11 |
| Mean number of stents | 2.35 ± 0.1 |
| Penultimate kissing balloon inflation | 20 (100%) |
| Murasato final POT | 20 (100%) |
| Main Vessel | |
| Mean stent length | 29.4 ± 1.94 |
| Mean stent diameter | 3.4 ± 0.09 |
| Side Branch | |
| Mean stent length | 17.9 ± 2.22 |
| Mean stent diameter | 2.9 ± 0.13 |
Abbreviations: SYNTAX, SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery; LAD, left anterior descending artery; LCx, left circumflex artery; F, French size; PCI, percutaneous coronary intervention; POT, Proximal optimisation technique; TIMI, Thrombolysis in Myocardial Infarction. Data are shown as mean ± standard error of the mean or as n (%).
Fig. 3.
Study subjects labelled 1 through to 20.
Fig. 4.
Study subjects labelled 1 through to 20.
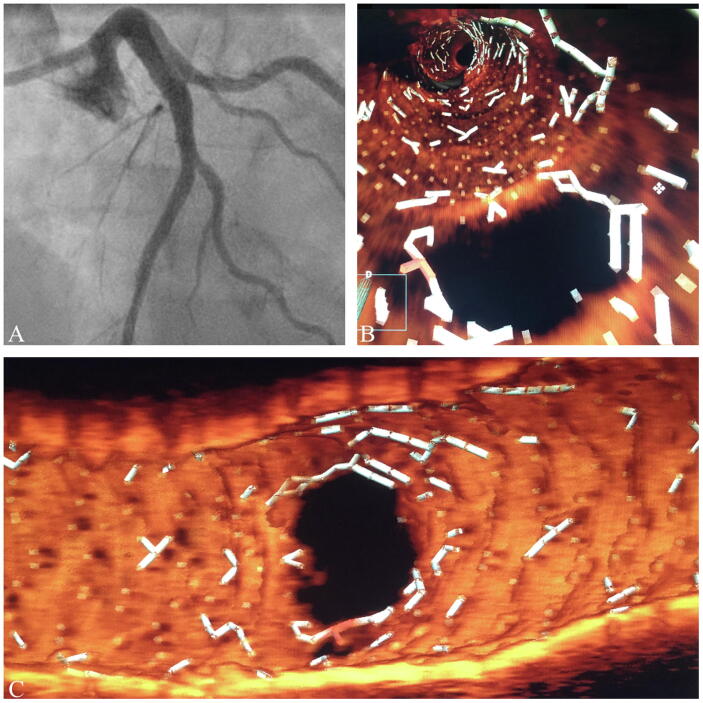
Fig. 5.
(A) Angiographic appearance. (B) St Jude OPTIS OCT 3D Flythrough image. (C) St Jude OPTIS OCT Carina View.
Fig. 6.
(A) St Jude OPTIS OCT 3D Flythrough image of main vessel stent showing minimal disruption at neo-carina. (B) St Jude OPTIS OCT Rendered Stent demonstrating main vessel struts covering proximal carina after final POT. (C) Angiographic image of vessel pre-PCI. (D) Angiographic image of vessel post-PCI.
Table 3.
Quantitative coronary angiography findings.
| Proximal MV | Baseline | Post PCI | p value |
|---|---|---|---|
| Reference diameter (mm) | 3.75 ± 0.8 | 4.40 ± 0.64 | <0.0001 |
| Minimal luminal diameter (mm) | 1.22 ± 0.8 | 3.38 ± 0.70 | <0.0001 |
| Diameter stenosis (%) | 63 ± 24 | 19 ± 8 | <0.0001 |
| Distal MV | |||
| Reference diameter (mm) | 3.17 ± 0.70 | 3.69 ± 0.51 | 0.001 |
| Minimal luminal diameter (mm) | 1.25 ± 0.83 | 2.94 ± 0.53 | <0.0001 |
| Diameter stenosis (%) | 62 ± 24 | 17 ± 5 | <0.0001 |
| SB | |||
| Reference diameter (mm) | 2.73 ± 0.51 | 3.02 ± 0.62 | 0.15 |
| Minimal luminal diameter (mm) | 1.08 ± 0.64 | 2.4 ± 0.51 | <0.0001 |
| Diameter stenosis (%) | 57 ± 25 | 15 ± 6 | <0.0001 |
| Bifurcation angle (degrees) | 54 ± 20 | ||
Abbreviations: MV, main vessel; SB, side-branch; PCI, Percutaneous coronary intervention. Data are shown as mean ± standard error of the mean.
3.3. Clinical outcomes
Complete follow-up data for all patients was available to 12 months with no loss to follow-up. One patient engaged in clinical follow-up but declined to undergo a 12-month ESE owing to living in a regional area without easy access to testing facilities but was well (CCS 0/NYHA I) with no symptoms suggestive of myocardial ischemia. Clinical data is shown in Table 2. One patient met the primary endpoint requiring TLR at 9 months (patient 15 in the image panel shown in Fig. 3, Fig. 4). The patient had undergone distal LMCA into LAD and Cx MRA facilitated bifurcation CFCT PCI after having been turned down for CABG owing to significant comorbidities. Owing to bulky calcium, his initial procedure was performed with a 2.0 Rotablator burr (Boston Scientific, Marlborough, MA, USA) for preparation of the LMCA, LAD and LCx. This patient re-presented with recurrent angina and an abnormal ESE with repeat angiography showing severe ISR of the left circumflex artery ostium and moderate ISR of the LMCA. The patient was treated with repeat bifurcation stenting utilizing the CFCT technique. There were no other primary or secondary outcome events in the study cohort. There were no strokes and no deaths during the follow-up period. The mean CCS score improved from 2.25 to 0.25 (p=<0.0001). QCA also demonstrated satisfactory findings with significant reductions in percentage stenosis for both the SB and MV (see Table 3). An additional patient presented more than 12 months post PCI with indeterminate symptoms and underwent coronary angiography that demonstrated moderate to severe stenosis in the proximal to ostial portion of the side-branch stent and was managed medically given satisfactory symptomatic control on medical therapy. There were no cases of possible, probable or definite stent thrombosis.
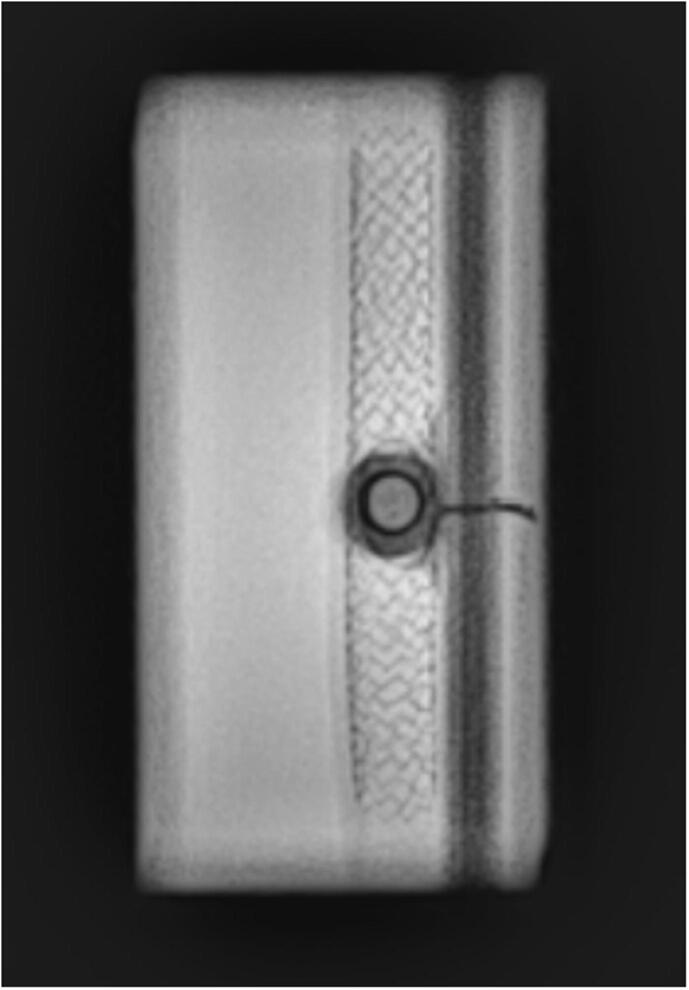
3.4. Bench testing findings
The bench test demonstrated satisfactory ostial morphology on fluoroscopic and photographic assessment. Stent coverage was satisfactory without peri-bifurcation metallic crowding and no evidence of geographic miss around the carina (Fig. 1, Fig. 7). End-on fluoroscopy demonstrated circular expansion of the SB ostium (Fig. 8).
Fig. 7.
(A) Bench test revealing naked proximal carina and optimal positioning of POT balloon. (B) POT inflation. (C) Kissing inflation. (D) Final result (following further final POT inflation).
Fig. 8.
End-on fluroscopic view coaxial with the long access of the side-branch stent demonstrating unobstructed circular ostium and absence of stent-strut crowding or deformation.
4. Discussion
4.1. General discussion
The data presented demonstrates the potential role for the CFCT technique in the treatment of coronary bifurcation disease. Bifurcation management represents an ongoing area of evolution and debate owing to sub-optimal outcomes when compared with the management of non-bifurcation disease and as a result has no universally accepted single technical solution [1]. The data from this cohort suggests that the CFCT strategy is a potentially reproducible method that minimizes strut material in the peri-bifurcation region and maximizes the ability for SB re-entry to facilitate a penultimate kissing balloon inflation (PUKBI). Bench testing and OCT findings indicate that the CFCT technique results in satisfactory coverage of the side-branch ostium. The technique emphasizes the role of optimal POT balloon inflation to cause carinal modification and to utilize extrusion of the peri-SB-ostial MV strut to facilitate proximal SB ostial coverage [26].
The CFCT technique appears to be a safe strategy and potentially holds promise as an additional tool in the armamentarium of contemporary bifurcation techniques. The findings also indicate the technical feasibility and suitability of this approach when using an everolimus-eluting bioresorbable polymer abluminal coated Pt-Cr DES (SYNERGY, Boston Scientific, Marlborough, MA, USA). The clinical data is supported by the above described bench testing findings with this platform. The complete resorption of polymer (poly-DL-lactide-coglycolide {PLGA]) with this platform within approximately 16 weeks and reduced levels of vessel inflammation may be particularly well suited to the bifurcation setting [34].
The twelve-month major adverse cardiac and cerebrovascular event (MACCE) rate in the present study was 5% owing to a single patient with symptom driven TLR for TLF. The DKCRUSH III study reported a 12-month MACCE of 6.2% in the DK-crush arm and 16.3% in the culotte arm with TLR of 2.4% and 6.7% respectively [4]. The findings are also comparable to the DKCRUSH V study where TLR was 5% in the DK-crush arm [35]. The current study findings appear to be in keeping with the original work on the initial iteration of the CFCT technique presented by Radjev et al. [20]. There were no instances of stent thrombosis, procedure related mortality or 12 mortality in the present study.
The technique is reproducible with potentially greater predictability for SB re-crossing and PUKBI (prior to final POT inflation) than other techniques [26]. It is postulated that SB re-access for the PUKBI is enhanced by the cone-flare inflation (CFI) prior to the intermediary KB step. The CFI step also serves to ensure apposition of the side branch stent to the ostium and acts as a high-pressure post inflation in the event that it is not possible to deliver a non-compliant balloon through the jailed stent. In the present cohort PUKBI was achieved in all patients and compares favorably with reported rates of 75 – 90% of patients in the DK Crush literature [12], [36]. Utilization the initial iteration of the technique Rajdev et al also found a higher success rate re-crossing side branches with shorter time taken compared with conventional crush stenting [20]. Sixty to seventy per cent of in-stent restenosis in bifurcation stent strategies is reported to occur at the neo-carina [4], [37]. The CFCT technique minimizes stent struts at the carina through precise positioning of the proximal edge of the SB stent level with, but not beyond, the distal vertex of the SB ostium. The CFCT technique then relies on the Murasato POT to push main vessel stent struts into the proximal vertex of the SB-ostium rather than having two or three layers of stent struts with significant strut deformation in this region (see Fig. 1, Fig. 2, Fig. 3) [26], [38]. Accurate positioning of the ostial SB stent is therefore a crucial part of the CFCT technique. Precise positioning of the stent so that the distal vertex of the SB ostium is level but not beyond will result in adequate final SB ostial coverage at the proximal vertex following Murasato optimal POT and PUKBI (Fig. 1). The dichotomy of either complete ostial coverage with DK-crush or culotte versus none with provisional SB management may be better addressed by the middle ground that the CFCT strategy represents.
4.2. Study limitations
The present study has several limitations. The first is the observational (albeit prospective) nature of the study with a relatively small sample size. The small sample size itself is in keeping with other technical feasibility studies in the bifurcation field [39], [40]. The purpose of this was to attain data and outcomes in an organized, systematic, prospective way regarding current practice of a technique with limited published findings, but with growing adoption. The study is also limited by the absence of a randomized study design with a comparator arm. Furthermore, the procedures were performed by relatively high-volume individual PCI operators (150–200+ PCI cases per year) and this may limit applicability to lower volume operators. Countervailing this, a strength of the CFCT technique is its relative predictability and safety. The study would also have been enhanced by routine angiography with intravascular imaging at 12 months on all patients (rather than clinically driven) but this would not have been appropriate given the observational nature of the registry and that routine angiography is not used to check stent patency.
4.3. Conclusion
The CFCT technique for bifurcation coronary artery stenosis appears to be safe and feasible with satisfactory clinical outcomes at 12 months in this prospective cohort. Expanded datasets to confirm this feasibility data will include angiographic and OCT follow-up, and subsequent randomized controlled data.
Declaration of Competing Interest
The cost of the registry was funded by an institutional grant from Boston Scientific Incorporated. ACC is a clinical proctor for Abbott and Edwards Lifesciences and has received advisory board and or consulting fees from Boston Scientific, Medtronic and Abbott. SGW is a clinical proctor for Abbott and Edwards Lifesciences and has received research grant support from Abbott and Biotronik. AI is a clinical proctor for Edwards Lifesciences. SVC is a clinical proctor for Abbott. The remaining authors have nothing to disclose.
References
- 1.Lassen J.F., Holm N.R., Banning A., Burzotta F., Lefevre T., Chieffo A. Percutaneous coronary intervention for coronary bifurcation disease: 11th consensus document from the European Bifurcation Club. EuroIntervention. 2016;12(1):38–46. doi: 10.4244/EIJV12I1A7. [DOI] [PubMed] [Google Scholar]
- 2.Genereux P., Kumsars I., Lesiak M., Kini A., Fontos G., Slagboom T. A randomized trial of a dedicated bifurcation stent versus provisional stenting in the treatment of coronary bifurcation lesions. J. Am. Coll. Cardiol. 2015;65(6):533–543. doi: 10.1016/j.jacc.2014.11.031. [DOI] [PubMed] [Google Scholar]
- 3.Gil R.J., Bil J., Grundeken M.J., Kern A., Inigo Garcia L.A., Vassilev D. Regular drug-eluting stents versus the dedicated coronary bifurcation sirolimus-eluting BiOSS LIM (R) stent: the randomised, multicentre, open-label, controlled POLBOS II trial. EuroIntervention. 2016;12(11):e1404–e1412. doi: 10.4244/EIJY15M11_11. [DOI] [PubMed] [Google Scholar]
- 4.Chen S.L., Xu B., Han Y.L., Sheiban I., Zhang J.J., Ye F. Comparison of double kissing crush versus Culotte stenting for unprotected distal left main bifurcation lesions: results from a multicenter, randomized, prospective DKCRUSH-III study. J. Am. Coll. Cardiol. 2013;61(14):1482–1488. doi: 10.1016/j.jacc.2013.01.023. [DOI] [PubMed] [Google Scholar]
- 5.Rigatelli G., Dell'Avvocata F., Zuin M., Vassiliev D., Mazza A., Dinh H.D. Complex coronary bifurcation revascularization by means of very minimal crushing and ultrathin biodegradable polymer DES: Feasibility and 1-year outcomes of the “Nano-crush” technique. Cardiovasc. Revasc. Med. 2017;18(1):22–27. doi: 10.1016/j.carrev.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 6.Erglis A., Kumsars I., Niemela M., Kervinen K., Maeng M., Lassen J.F. Randomized comparison of coronary bifurcation stenting with the crush versus the culotte technique using sirolimus eluting stents: the Nordic stent technique study. Circ. Cardiovasc. Interv. 2009;2(1):27–34. doi: 10.1161/CIRCINTERVENTIONS.108.804658. [DOI] [PubMed] [Google Scholar]
- 7.Zheng X.W., Zhao D.H., Peng H.Y., Fan Q., Ma Q., Xu Z.Y. Randomized comparison of the crush versus the culotte stenting for coronary artery bifurcation lesions. Chin. Med. J. (Engl). 2016;129(5):505–510. doi: 10.4103/0366-6999.176997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Louvard Y., Thomas M., Dzavik V., Hildick-Smith D., Galassi A.R., Pan M. Classification of coronary artery bifurcation lesions and treatments: time for a consensus! Catheterization Cardiovasc. Intervent. 2008;71(2):175–183. doi: 10.1002/ccd.21314. [DOI] [PubMed] [Google Scholar]
- 9.Zhang D., He Y., Yan R., Yin D., Feng L., Xu B. A novel technique for coronary bifurcation intervention: Double rewire crush technique and its clinical outcomes after 2 years of follow-up. Catheterization Cardiovasc. Intervent. 2019;93(S1):851–858. doi: 10.1002/ccd.28066. [DOI] [PubMed] [Google Scholar]
- 10.Colombo A., Stankovic G., Orlic D., Corvaja N., Liistro F., Airoldi F. Modified T-stenting technique with crushing for bifurcation lesions: immediate results and 30-day outcome. Catheterization Cardiovasc. Intervent. 2003;60(2):145–151. doi: 10.1002/ccd.10622. [DOI] [PubMed] [Google Scholar]
- 11.Crimi G., Mandurino-Mirizzi A., Gritti V., Scotti V., Strozzi C., De Silvestri A. Percutaneous coronary intervention techniques for bifurcation disease: a network meta-analysis reveals superiority of double kissing crush. Can. J. Cardiol. 2019 doi: 10.1016/j.cjca.2019.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Colombo A., Bramucci E., Saccà S., Violini R., Lettieri C., Zanini R. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations. Circulation. 2009;119(1):71–78. doi: 10.1161/CIRCULATIONAHA.108.808402. [DOI] [PubMed] [Google Scholar]
- 13.Behan M.W., Holm N.R., Curzen N.P., Erglis A., Stables R.H., de Belder A.J. Simple or complex stenting for bifurcation coronary lesions clinical perspective. Circulation: Cardiovasc. Intervent. 2011;4(1):57–64. doi: 10.1161/CIRCINTERVENTIONS.110.958512. [DOI] [PubMed] [Google Scholar]
- 14.Chen X., Li X., Zhang J.-J., Han Y., Kan J., Chen L. 3-Year outcomes of the DKCRUSH-V trial comparing DK crush with provisional stenting for left main bifurcation lesions. JACC: Cardiovasc. Intervent. 2019;12(19):1927–1937. doi: 10.1016/j.jcin.2019.04.056. [DOI] [PubMed] [Google Scholar]
- 15.Latib A., Colombo A. Bifurcation disease: what do we know, what should we do? JACC: Cardiovasc. Intervent. 2008;1(3):218–226. doi: 10.1016/j.jcin.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 16.Colleran R., Byrne R.A., Kastrati A. Bifurcation intervention with a two-stent strategy: can one size fit all? Eur. Soc. Cardiol. 2016 doi: 10.1093/eurheartj/ehw440. [DOI] [PubMed] [Google Scholar]
- 17.Dou K., Zhang D., Xu B., Yang Y., Yin D., Qiao S. An angiographic tool for risk prediction of side branch occlusion in coronary bifurcation intervention: the RESOLVE score system (Risk prEdiction of Side branch OccLusion in coronary bifurcation interVEntion) JACC: Cardiovasc. Intervent. 2015;8(1 Part A):39–46. doi: 10.1016/j.jcin.2014.08.011. [DOI] [PubMed] [Google Scholar]
- 18.Hahn J.-Y., Chun W.J., Kim J.-H., Song Y.B., Oh J.H., Koo B.-K. Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: results from the COBIS II Registry (COronary BIfurcation Stenting) J. Am. Coll. Cardiol. 2013;62(18):1654–1659. doi: 10.1016/j.jacc.2013.07.041. [DOI] [PubMed] [Google Scholar]
- 19.Sawaya F.J., Lefèvre T., Chevalier B., Garot P., Hovasse T., Morice M.-C. Contemporary approach to coronary bifurcation lesion treatment. JACC: Cardiovasc. Intervent. 2016;9(18):1861–1878. doi: 10.1016/j.jcin.2016.06.056. [DOI] [PubMed] [Google Scholar]
- 20.Rajdev S., Suarez A., Modi K.A., Brott B.C., Aqel R.A., Misra V.K. “Cone Crush”, a variant of modified T-Stenting technique for coronary bifurcation lesions: bench testing, clinical feasibility, and in-hospital outcomes. J. Am. Coll. Cardiol. 2007;49(S9) 6B-B. [Google Scholar]
- 21.Darlington A.M., Balouch M.A., Shroff A.R. Optimization of coronary bifurcation intervention using intravascular imaging. Curr. Cardiovasc. Imaging Rep. 2019;12(7):26. [Google Scholar]
- 22.Association W.M. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull. World Health Organ. 2001;79(4):373. [PMC free article] [PubMed] [Google Scholar]
- 23.Sianos G., Morel M.-A., Kappetein A.P., Morice M.-C., Colombo A., Dawkins K. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1(2):219–227. [PubMed] [Google Scholar]
- 24.Ellis S.G., Vandormael M.G., Cowley M.J., DiSciascio G., Deligonul U., Topol E.J. Coronary morphologic and clinical determinants of procedural outcome with angioplasty for multivessel coronary disease. Implications for patient selection. Multivessel Angioplasty Prognosis Study Group. Circulation. 1990;82(4):1193–1202. doi: 10.1161/01.cir.82.4.1193. [DOI] [PubMed] [Google Scholar]
- 25.Medina A., Suárez de Lezo J., Pan M. A new classification of coronary bifurcation lesions. Revista Española de Cardiología (English Edition) 2006;59(2):183. [PubMed] [Google Scholar]
- 26.Murasato Y., Mori T., Okamura T., Nagoshi R., Fujimura T., Yamawaki M. Efficacy of the proximal optimization technique on crossover stenting in coronary bifurcation lesions in the 3D-OCT bifurcation registry. Int. J. Cardiovasc. Imaging. 2019;35(6):981–990. doi: 10.1007/s10554-019-01581-1. [DOI] [PubMed] [Google Scholar]
- 27.Tearney G.J., Regar E., Akasaka T., Adriaenssens T., Barlis P., Bezerra H.G. Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: a report from the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation. J. Am. Coll. Cardiol. 2012;59(12):1058–1072. doi: 10.1016/j.jacc.2011.09.079. [DOI] [PubMed] [Google Scholar]
- 28.Mehran R., Rao S.V., Bhatt D.L., Gibson C.M., Caixeta A., Eikelboom J. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123(23):2736–2747. doi: 10.1161/CIRCULATIONAHA.110.009449. [DOI] [PubMed] [Google Scholar]
- 29.Garcia-Garcia H.M., McFadden E.P., Farb A., Mehran R., Stone G.W., Spertus J. Standardized end point definitions for coronary intervention trials: the Academic Research Consortium-2 consensus document. Eur. Heart J. 2018;39(23):2192–2207. doi: 10.1093/eurheartj/ehy223. [DOI] [PubMed] [Google Scholar]
- 30.Stone G.W., Sabik J.F., Serruys P.W., Simonton C.A., Généreux P., Puskas J. Everolimus-eluting stents or bypass surgery for left main coronary artery disease. N. Engl. J. Med. 2016;375(23):2223–2235. doi: 10.1056/NEJMoa1610227. [DOI] [PubMed] [Google Scholar]
- 31.Mäkikallio T., Holm N.R., Lindsay M., Spence M.S., Erglis A., Menown I.B. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. The Lancet. 2016;388(10061):2743–2752. doi: 10.1016/S0140-6736(16)32052-9. [DOI] [PubMed] [Google Scholar]
- 32.Hemingway H., Fitzpatrick N.K., Gnani S., Feder G., Walker N., Crook A.M. Prospective validity of measuring angina severity with Canadian Cardiovascular Society class: the ACRE study. Can. J. Cardiol. 2004;20(3):305–309. [PubMed] [Google Scholar]
- 33.Ormiston J.A., Kassab G., Finet G., Chatzizisis Y.S., Foin N., Mickley T.J. Bench testing and coronary artery bifurcations: a consensus document from the European Bifurcation Club. EuroIntervention. 2018;13(15):e1794–e1803. doi: 10.4244/EIJ-D-17-00270. [DOI] [PubMed] [Google Scholar]
- 34.Wilson G.J., Marks A., Berg K.J., Eppihimer M., Sushkova N., Hawley S.P. The SYNERGY biodegradable polymer everolimus eluting coronary stent: porcine vascular compatibility and polymer safety study. Catheterization Cardiovasc. Intervent. 2015;86(6):E247–E257. doi: 10.1002/ccd.25993. [DOI] [PubMed] [Google Scholar]
- 35.Chen S.-L., Zhang J.-J., Han Y., Kan J., Chen L., Qiu C. Double kissing crush versus provisional stenting for left main distal bifurcation lesions: DKCRUSH-V randomized trial. J. Am. Coll. Cardiol. 2017;70(21):2605–2617. doi: 10.1016/j.jacc.2017.09.1066. [DOI] [PubMed] [Google Scholar]
- 36.Kervinen K., Niemela M., Romppanen H., Erglis A., Kumsars I., Maeng M. Clinical outcome after crush versus culotte stenting of coronary artery bifurcation lesions: the Nordic Stent Technique Study 36-month follow-up results. JACC Cardiovasc, Interv. 2013;6(11):1160–1165. doi: 10.1016/j.jcin.2013.06.009. [DOI] [PubMed] [Google Scholar]
- 37.Takagi K., Ielasi A., Shannon J., Latib A., Godino C., Davidavicius G. Clinical and procedural predictors of suboptimal outcome after the treatment of drug-eluting stent restenosis in the unprotected distal left main stem: the Milan and New-Tokyo (MITO) registry. Circ. Cardiovasc. Interv. 2012;5(4):491–498. doi: 10.1161/CIRCINTERVENTIONS.111.964874. [DOI] [PubMed] [Google Scholar]
- 38.Hoye A. The proximal optimisation technique for intervention of coronary bifurcations. Intervent. Cardiol. Rev. 2017;12(2):110. doi: 10.15420/icr.2017:11:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Worthley S., Hendriks R., Worthley M., Whelan A., Walters D.L., Whitbourn R. Paclitaxel-eluting balloon and everolimus-eluting stent for provisional stenting of coronary bifurcations: 12-month results of the multicenter BIOLUX-I study. Cardiovasc. Revascul. Med. 2015;16(7):413–417. doi: 10.1016/j.carrev.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 40.Çaylı M., Şahin D.Y., Elbasan Z., Gür M., Çağlıyan C.E., Kıvrak A. Modified flower petal technique: a new technique for the treatment of Medina type 1.1. 1 coronary bifurcation lesions. JACC: Cardiovasc. Intervent. 2013;6(5):516–522. doi: 10.1016/j.jcin.2012.12.130. [DOI] [PubMed] [Google Scholar]