Abstract
Background
South America is the current epicenter of COVID-19 pandemic. Yet, the epidemiological and clinical features of the disease have not been described in Brazil, the third most affected country in the world.
Methods
In this retrospective study, we describe the demographics, epidemiology and clinical features of the first 557 consecutive patients positive for SARS-CoV-2 living in Pernambuco state, Northeast Brazil.
Results
The first COVID-19 cases occurred in the high income population. The age of infected patients ranged from 27 days to 97 years with a median of 47 years. The ratio of males to female in the SARS-CoV-2-infected group was 0.83:1. The most common symptom was cough (74.51%), followed by fever (66.79%), dyspnea (56.01%), sore throat (28.19%) and O2 saturation <95% (24.42%). 86.44% of the lethal cases were patients older than 51 years. The median time from illness onset to diagnosis was 4.0 days (range 0–39 days) Severe patients diagnosed after 14 days of symptoms onset had higher viral load than patients with mild disease.
Conclusions
Our study provides important information about COVID-19 in the tropics and will assist physicians and health officials to face the current pandemics as SARS-CoV-2 continues to spread in the human population.
Keywords: Coronavirus disease 2019, SARS-CoV-2, Clinical characteristics, Demographics, Epidemiology, Clinics
Highlights
-
•
We describe for the first time the demographics, epidemiology and clinical of COVID-19 in Brazil. .
-
•
The first COVID-19 cases occurred in the high income population.
-
•
86.44% of the lethal cases were patients older than 51 years.
-
•
Severe patients diagnosed after 14 days of symptoms onset had higher viral load than patients with mild disease.
1. Introduction
In late December 2019, a cluster of severe pneumonia cases of unknown origin was reported in Wuhan, Hubei Province, China [1]. The disease, later named coronavirus disease 2019 (COVID-19), was caused by a novel coronavirus identified as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [2,3]. Similar to other highly pathogenic coronaviruses (CoVs -SARS-CoV and Middle East respiratory syndrome CoV (MERS-CoV), SARS-CoV-2 belongs to β genus within the Coronaviridae family and emerged from bats.
The rapid spread of SARS-CoV-2 around the world caused the World Health Organization (WHO) to declared COVID-19 as a pandemic on March 11, 2020 [4]. China was the first epicenter of pandemic, followed by Europe, the USA, and now South America. On February 26, 2020, Brazil reported the first case in Latin America in a São Paulo patient returning home after a work trip to Italy from February 9th to 21st. The patient had a mild respiratory disease characterized by coryza, dry cough, and sore throat [[5], [6], [7]]. Since then, the number of COVID-19 cases in Brazil has increased steadily and the country has become the third most affected in the world after the USA and India. Given the paucity of diagnostic tests in developing countries, the actual incidence of COVID-19 in Brazil is heavily underestimated. For instance, while the USA has done 282,114 tests per million inhabitants, Brazil has performed only 68,143 tests/million people (https://www.worldometers.info/coronavirus/). As of September 15, 2020, Brazil has confirmed 4.3 million COVID-19 cases and 132,297 deaths (https://www.worldometers.info/coronavirus/). Pernambuco is one of the most affected state in Brazil with 137.869 cases and 7914 deaths [8].
The emergence of SARS-CoV-2 caused a profound change in the global scenario and recruited public health authorities and research groups from different parts of the world to fill knowledge gaps in the biology and pathogenesis of this devastating pathogen. Although the epidemiological and clinical presentation of COVID-19 has been well documented in several countries of the Northern Hemisphere, information regarding the clinical features of COVID-19 in Latin America, especially in Brazil, remains scarce and limited. Thus, an updated analysis of cases could help to significantly improve our knowledge and consequently provide insights into COVID-19 in this region of the planet, given its unique climate, social dynamics, population genetics and political scenario [9].
Here, we describe for the first time the clinical, epidemiological and demographic features of the first 557 laboratory-confirmed COVID-19 cases in Pernambuco state, Northeast Brazil, who were diagnosed between March 12 and April 22, 2020.
2. Methods
2.1. Study design and participants involvement
A total of 557 patients living in Pernambuco state with a positive SARS-CoV-2 nucleic acid test were included in this study. Patients were considered to have confirmed COVID-19 infection if they had at least one positive RT-qPCR test for SARS-CoV-2. This study was approved by the UPE Institutional Review Board under protocol CAAE: 27607619.0.0000.5207 and was performed in accordance with relevant guidelines e regulations, including the Brazilian National Health Council (CNS) Resolution 466/2012. The requirement for informed consent study was waived based on the nature of this observational retrospective study, in which patient identifying information were kept confidential.
2.2. Data collection
Patient epidemiological information, demographic and clinical characteristics, including medical history, signs and symptoms, laboratory findings, underlying co-morbidities, and date of disease onset were obtained from electronic medical records of the Pernambuco Central Public Health Laboratory (LACEN) and analyzed. Patient outcome data were obtained from March 12 to 22 April 2020, the final date of follow-up.
2.3. Laboratory confirmation
All COVID-19 patients enrolled in this study were diagnosed according to World Health Organization interim guidance [10]. Laboratory confirmation was performed at the Pernambuco LACEN, which is one of the designated laboratories for the diagnosis of SARS-CoV-2 in this state. Nasopharyngeal and oropharyngeal swabs were collected from patients presenting respiratory signs of disease compatible with COVID-19. After sample collection, viral RNA was extracted using the ReliaPrep Viral TNA Miniprep System Kit (Promega, Madison, WI, USA), according to the manufacturers’ instructions and the RNA was used for RT-qPCR following the protocol for SARS-CoV-2 detection established by Corman and coworkers [11].
2.4. Spatial analysis
Spatial analysis were done by georeferencing only the addresses of individuals residing in Recife (n = 306), capital of the State of Pernambuco and city with the largest number of confirmed cases of COVID-19 at the time of this analysis. For that, the QGIS software (https://qgis.org/en/site/) was used to plot home addresses and the Kernel Density Estimation method was applied to identify the neighborhoods with the highest concentration of COVID-19 cases. We also calculated the incidence of infection in the neighborhoods and that concentration of cases were displayed on a heat map. The location of the georeferenced addresses was produced on a scale of 1:215,000, which means that on the map, the location of the addresses presents an error of approximately 0.4 mm (40 m on the real scale). Therefore, the addresses of individuals are located in an area of approximately 2500 m2. As Recife is an urbanized city, ethical concerns are not applicable because it is not possible to verify the exact location of each residence. The cartographic base used was acquired in shapefile format at the website of the Brazilian Institute of Geography and Statistics (IBGE) in the Geocentric Reference System for the Americas (SIRGAS) 2000. In addition, we built a graduated map with information on the income of households in the neighborhoods from the city of Recife and we classified the neighborhoods based on the amount of minimum wages received to correlate the distribution of COVID-19 cases within the different ranges of household income of the studied population. We used data on minimum wages and average monthly nominal income per household from the last Brazilian census (http://censo2010.ibge.gov.br/).
2.5. Statistical analysis
Microsoft Office Excel (version 2010) was used to build a database with patient's information. Data process and analysis were made using the GraphPad Prism version 6.0 for Windows (GraphPad Software, La Jolla, CA, USA). Continuous variables were expressed as medians and interquartile ranges, as appropriate. Categorical variables were summarized as counts and percentages. A chi-square test was used to investigate the level of association among variables. Statistically significant differences were defined as p < 0.05.
3. Results
3.1. Study population
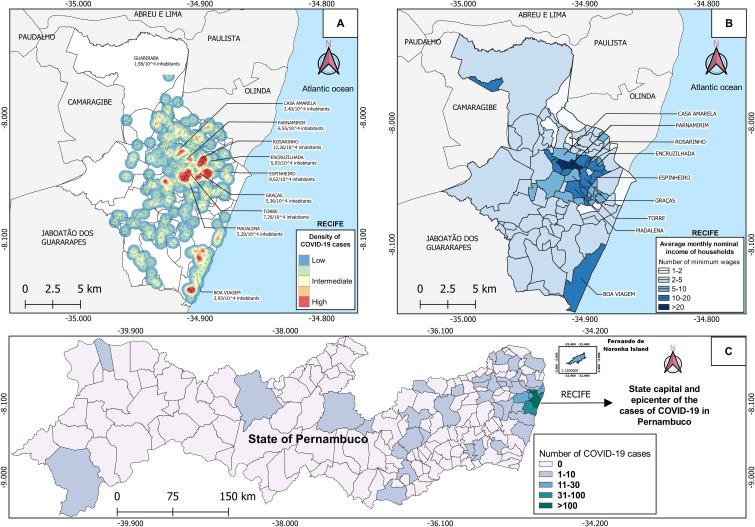
From 12 March to April 22, 2020, a total of 2772 suspected cases-1616 females (58.30%) and 1156 males (41.70%) - were collected and tested for SARS-CoV-2 at the Pernambuco LACEN by RT-qPCR. From total cases, 557 (20.09%) were positive for SARS-COV-2. These were the first COVID-19 cases reported in the state. Fig. 1 illustrates the epidemic distribution in Pernambuco state. The highest number of cases (n = 304, 54.58%) occurred in the city of Recife, capital of Pernambuco, followed by the metropolitan cities Jaboatão dos Guararapes (n = 43, 7.72%), Olinda (n = 43, 7.72%), Paulista (n = 30, 5.39%), São Lourenço da Mata (n = 23, 4.13%), and Camaragibe (n = 16, 2.87%).
Fig. 1.
Spatial analysis of COVID-19 cases in Pernambuco state, Brazil. Fig. 1A shows the spatial distribution of COVID-19 cases in Recife, Pernambuco capital as heat map. The Kernel Density Estimate was used to show the areas with the highest concentration of cases associated with the incidence of the disease in some neighborhoods. Fig. 1B shows a graduated map with information on the average nominal monthly household income converted into the amount of minimum wages. Fig. 1C shows the cities with COVID-19 positive cases in the State of Pernambuco.
3.2. Spatial analysis
The first 304 cases of COVID-19 in Recife were georeferenced using the Kernal Density Estimate. The highest case numbers were concentrated in the neighborhoods of Casa Amarela, Parnamirim, Rosarinho, Encruzilhada, Espinheiro, Graças, Torre, Madalena, and Boa Viagem (Fig. 1A). The Rosarinho neighborhood had the highest incidence of COVID-19 (12.26/104 inhabitants) and also had the highest number of cases per square kilometer (20/km2), while the Guabiraba neighborhood had the lowest incidence (1.58/104 inhabitants) and a lower number of cases per square kilometer (0.02/km2). Regarding the distribution of COVID-19 cases in the different household income ranges (Fig. 1B), we found that SARS-CoV-2 infections occurred in neighborhoods with greater purchasing power. Of the nine neighborhoods highlighted on the heat map, seven had households with earnings greater than 10 minimum wages, demonstrating that the first COVID-19 cases in Pernambuco target the high income population.
3.3. Cumulative number of COVID-19 cases
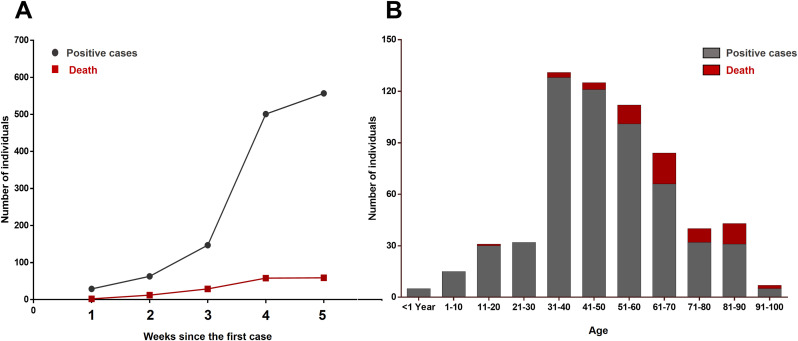
Fig. 2A presents the cumulative number of COVID-19 cases recorded weekly. The first positive case for SARS-CoV-2 in the state of Pernambuco was notified on March 12, 2010. During the first week, 29 (5.20%) cases and 2 (3.38%) deaths were registered. The fourth week (from 7 to 14 April) registered the greatest increase in the number of cases and deaths. A total of 354 (63.55%) cases and 29 (49.15%) deaths were recorded in that period, which corresponded to 501 (89.94%%) accumulated positive cases and 58 (98.30%) deaths.
Fig. 2.
Epidemiological features of COVID-19 patients (n = 557) in Pernambuco, Brazil. A) Cumulative number of COVID-19 infected and deceased patients recorded weekly since the first diagnostic. B) Age distribution in COVID-19 lethal and non-lethal cases.
3.4. Patient epidemiological features
The age of SARS-CoV-2 infected patients ranged from 27 days to 97 years with a mean of 48.57 years and a median of 47 (interquartile range [IQR], 32 to 68). The ratio of males to female in the SARS-CoV-2-infected group was 0.83:1 (45.42% males/54.58% females; chi-square test, p = 0.46), showing a slight higher incidence in females than males. The highest number of cases occurred in patients aged 31–40 years old (n = 128, 22.98%), followed by the 41–50 years age group (n = 121, 21.72%), and the group embracing patients from 51 to 60 years old (n = 101, 18.13%). During the study period, a total of 59 deaths occurred. Among these, 51 (86.44%) were patients older than 51 years. Although the incidence was more elevated in females, the number of deaths tended to be higher in males (55.93% versus 44.06%), despite the difference not reaching statistical significance (chi-square test, p = 0.87). The mean age of deceased patients was 66.06 years and the median was 65 (interquartile range, 51.5–82.5). The highest mortality rate was observed in patients in the 61–70 years age group (n = 18, 30.50%), followed by the 51 to 60 age group (n = 11, 18.64%) (Fig. 2 B).
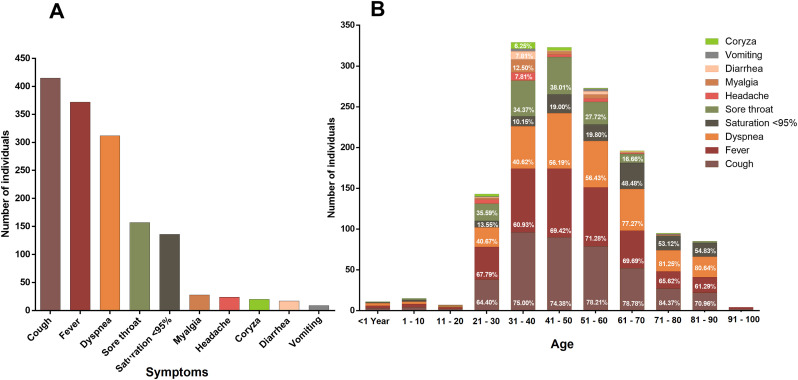
3.5. Clinical features
Fig. 3A summarizes the main symptoms presented at the time of patient notification. The most common symptom was cough (n = 415, 74.51%), followed by fever (n = 372, 66.79%), dyspnea (n = 312, 56.01%), sore throat (n = 157, 28.19%) and O2 saturation <95% (N = 136, 24.42%). Some patients also presented myalgia (n = 28, 5.03%), headache (n = 24, 4.31%), running nose (n = 20, 3.59%), diarrhea (n = 17, 3.05%), and vomiting (n = 9, 1.62%). Fig. 3 B shows the symptoms according to age groups. The most prevalent symptom in patients aged less than 20 years old were fever, cough and dyspnea. In addition to these symptoms, sore throat, myalgia, headache, diarrhea, vomiting and runny nose were more common in people aged over 20 years old. The highest rate of patients with saturation <95% was found in individuals aged over 61 years. The average time from the symptoms onset to notification date was 4.85 days while among deceased patients this number was 4.52 days.
Fig. 3.
Clinical features of COVID-19 patients (n = 557) in Pernambuco, Brazil. A) Main symptoms presented at the time of patient notification. B) Symptoms distribution according to the age group.
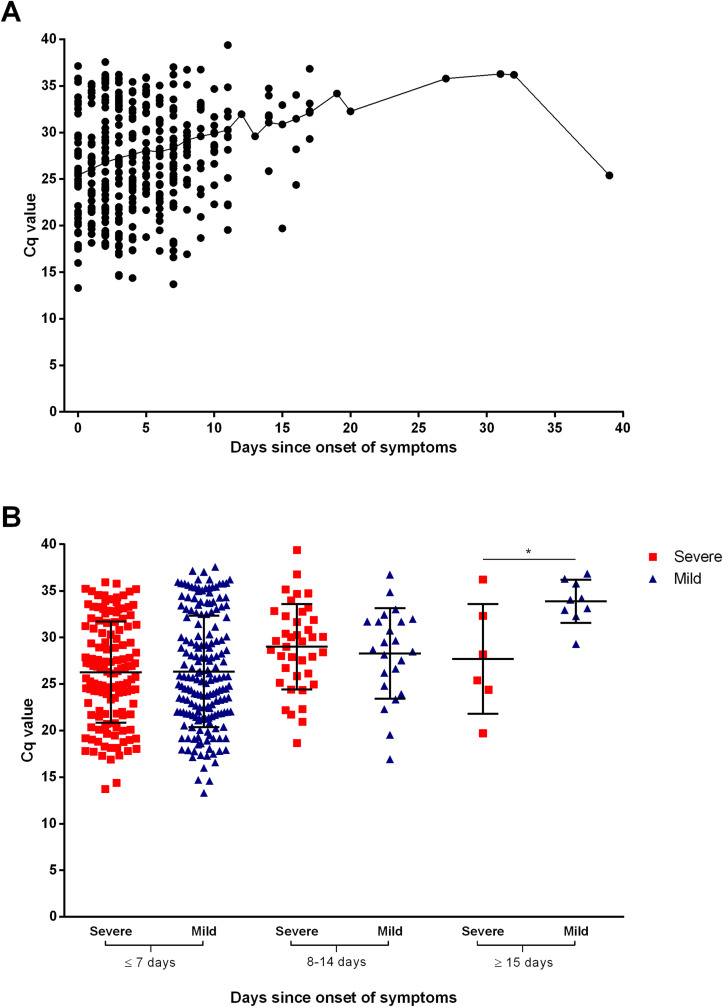
3.6. Virus shedding patterns at the time of SARS-CoV-2 diagnosis
We next sought to investigate the virus shedding pattern in patients at the time of diagnosis. Information on the quantitation cycle (Cq) was available for 388 patients. The Cq value was used to estimate the viral load of patient's nasopharyngeal specimens, in which lower Cq values indicate higher amount of virus. The median Cq of the patients was 26.3 (SD = 5,7) and ranged from 13.3 to 39.3. To evaluate SARS-CoV-2 shedding patterns in this cohort, the data were further stratified according to the day of symptoms onset at the time of sampling. The median time from illness onset to diagnosis was 4.0 days (SD = 4,7), with a range of 0–39 days (Fig. 4 A). We then compared the viral load of severe cases (patients that were admitted to ICU and the ones that have died) with mild cases at different days since symptoms onset (Fig. 4B). There was no statistically significant difference in viral load at the time of diagnosis of patients with mild or severe COVID-19 up to 14 days of symptoms onset. However, patients with severe disease diagnosed after 14 days of symptoms onset had higher viral load than patients with mild disease (p = 0.0218).
Fig. 4.
Virus shedding patterns at the time of diagnosis.
A) Viral load in nasopharyngeal swabs according to the date of symptoms onset. B) Viral load in severe and mild patients according to the date of symptoms onset. *p <
0.05.
3.7. Clinical evolution and associated comorbidities
The clinical evolution of patients reported up to the date of notification (April 22nd, 2020) indicated that 50.63% (282/557) were in self-isolation, 26.93% (150/557) were in general hospital wards, 5.38% (30/557) required intensive care unit (ICU) care, 6.46% (36/557) fully recovered from the disease and 10.59% (59/557) of the patients evolved to death (Table 1 ).
Table 1.
Epidemiological features of COVID-19 patients (n = 557) in Pernambuco, Brazil.
| Age | <1 year N = 5 (%) |
1–10 N = 6 (%) |
11–20 N = 3 (%) |
21–30 N = 59 (%) |
31–40 N = 128 (%) |
41–50 N = 121 (%) |
51–60 N = 101 (%) |
61–70 N = 66 (%) |
71–80 N = 32 (%) |
81–90 N = 31 (%) |
91–100 N = 5 (%) |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Total | |||||||||||
| Female | 304 (54.58) | 1 (20.00) | 3 (50.00) | 2 (66.66) | 35 (59.32) | 77 (60.15) | 60 (49.59) | 53 (52.48) | 34 (51.52) | 18 (56.25) | 18 (58.06) | 3 (60.00) |
| Male | 253 (45.42) | 4 (80.00) | 3 (50.00) | 1 (33.34) | 24 (40.68) | 51 (39.85) | 61 (50.41) | 48 (47.52) | 32 (48.48) | 14 (43.75) | 13 (41.94) | 2 (40.00) |
| Evolution | Total | |||||||||||
| Self-isolation | 282 (50.63) | 3 (60.00) | 2 (33.33) | 1 (33.33) | 48 (81.35) | 88 (68.75) | 70 (57.85) | 50 (49.50) | 10 (15.15) | 5 (15.62) | 4 (12.90) | 1 (20.00) |
| Hospital wards | 150 (26.93) | 2 (40.00) | 4 (66.66) | – | 6 (10.17) | 24 (18.75) | 39 (32.23) | 24 (23.76) | 27 (40.91) | 14 (43.75) | 10 (32.26) | – |
| ICU | 30 (5.38) | – | – | – | 2 (3.38) | 1 (0.78) | 3 (2.48) | 8 (7.92) | 6 (9.09) | 4 (12.50) | 5 (16.13) | 1 (20.00) |
| Death | 59 (10.59) | – | – | 1 (33.33) | – | 3 (2.34) | 4 (3.31) | 11 (10.89) | 18 (27.27) | 8 (25.00) | 12 (38.71) | 2 (40.00) |
| Recovered | 36 (6.46) | – | – | 1 (33.33) | 3 (5.08) | 12 (9.36) | 5 (4.13) | 8 (7.92) | 5 (7.58) | 1 (3.13) | – | 1 (40.00) |
Numbers between parentheses indicate percentage of patients in each age group.
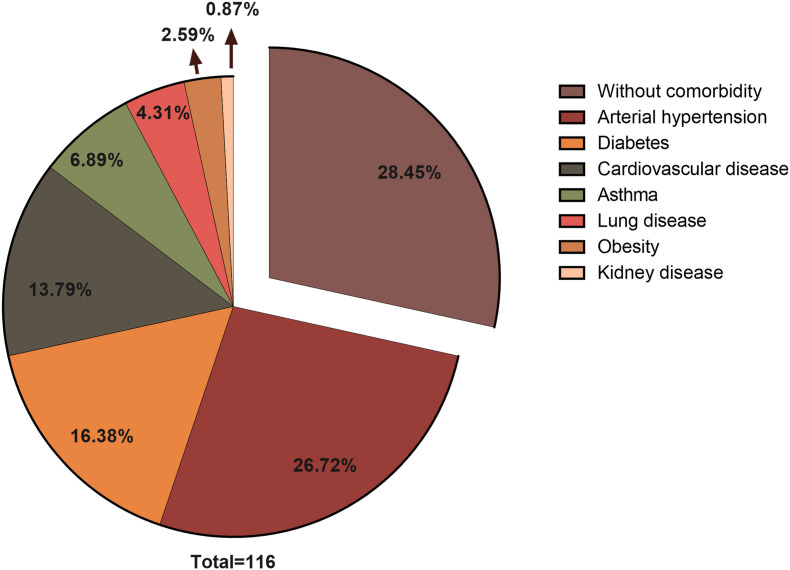
Information on comorbidities was available to 116 patients. A total of 72.27% of the patients reported comorbidities. The most common comorbidity was arterial hypertension (26.72%), followed by diabetes mellitus (16.38%), cardiovascular diseases (13.79%), asthma (6.89%), lung disease (4.31%), obesity (2.59%), and kidney disease (0.87%) (Fig. 5 ).
Fig. 5.
Clinical comorbidities in COVID-19 positive patients.
4. Discussion
Brazil remains the third most affected country after the USA and India. After its initial detection on February 26, 2020, SARS-CoV-2 has spread to all its 26 states and the federal district. Yet, the epidemiological and clinical profile of COVID-19 in Brazil has not been reported in the literature. Here, we described for the first time the epidemiological and clinical characteristics of the first 557 consecutive patients diagnosed with SARS-CoV-2 in the state of Pernambuco between 12 March and April 22, 2020. The first patients diagnosed with SARS-CoV-2 in Pernambuco were an elderly couple (71-year-old man and 66-year-old woman) returning from Rome, Italy on 29 February and whose diagnostic was confirmed on 12 March. The couple lived in the Boa Viagem, a high-income neighborhood located in the southern region of the city (Fig. 1). This couple had returned from a trip to Italy and sought medical treatment on March 5, 2020, when Italy already had 3858 confirmed cases of COVID-19 (WHO). On March 17, Pernambuco reported local transmission of SARS-CoV-2 for the first time and since then the number of new cases has increased steadily first in the metropolitan area and then spreading to inland cities. The state capital, Recife had the highest number of COVID-19 cases in the study period. As shown in Fig. 1B, the first SARS-CoV-2 cases were concentrated in neighborhoods with a higher nominal monthly household income, such as the Rosarinho, Espinheiro, and Boa Viagem neighborhoods that had average earnings above 10 Brazilian minimum wages. Our data is in agreement with a study done in Rio de Janeiro, Brazil in which the highest rates of COVID-19 were observed in the wealthiest regions [12].
Despite the epidemiological evidence and the first detection of SARS-CoV-2 in the Boa Viagem neighborhood with subsequent spread mainly to high income neighborhoods, it is not possible to say with certainty that SARS-CoV-2 infections in Pernambuco started from these places. For that, robust phylogeography analyses based on SARS-CoV-2 genomic sequences from these patients would be necessary to definitely understand the its transmission dynamics and associate it with clinical and epidemiological data. Nevertheless, individuals with high household income are more likely to take costly international trips and are therefore expose themselves to the risk of acquiring an infection overseas. In fact, the index COVID-19 case in Brazil was diagnosed in São Paulo in patient returning from a trip from Italy. Phylogenetic analyses of the first patients in São Paulo coupled with travel history information confirmed multiple independent importations from Italy and local spread during the initial stage of SARS-CoV-2 transmission in the country [13]. Our results highlights the importance of emerging diseases strengthening programs and preventing people who have traveled to different locations in the world from returning to their countries without undergoing quarantine and testing upon return to their home country.
The median age of the patients included in this study was 47 years (IQR 32 to 68), ranging from 27 days to 97 years. However, the median age of deceased patients was 65 years. In our study, only 14 cases (2,51% of total) were reported in patients aged less the 20 years, whereas a large proportion of cases (44,70% of total) were in patients aged 31–50 years old. Lethal cases in this cohort were concentrated in patients older than 51 years, which accounted for 86.44% of total deaths. Our data is in agreement with a study conducted by Guan et al. where the median age of SARS-CoV-2 infected patients was 47 years (IQR: 35 to 58) and only 0.9% of patients were under 15 years old [14]. In another study carried out in China, the most affected patients were in the 50–59 years age group, whereas fatal cases were concentrated in the 70–79 years group [15].
In our study, a higher proportion of women sought medical attention upon suspecting of a respiratory disease (58.30% females and 41.70% males) and SARS-CoV-2 positivity was higher in female (54.58%) than males (45.42%). The data is in agreement with 102,646 cases of COVID-19 cases reported in Canada to date, in which 56% occurred in females [16]. This sex discrepancy in our studyt might be due to lifestyle behavior in which women are more likely to seek medical care at the first signs of disease than men. The COVID-19 lethality in this study showed a higher tendency in males than females (55.93% versus 44.06%), although it not reached statistical significance. In general, the men to women ratio of COVID-19 prevalence is the same, but men with COVID-19 tend have higher risk of developing the severe forms of the disease and die from it [17,18].
We found that cough, fever and dyspnea were the most common symptoms. The main symptoms showed in our study were also reported by others [[19], [20], [21], [22]]. Wan et al., 2020 demonstrated that fever (88.9%) and cough (76.5%) were also the most common symptoms, however, dyspnea was present in only 13.3% of patients [23]. Gastrointestinal manifestations were less prevalent. Lower frequency of gastrointestinal symptoms is also shown in other studies [14,20].
The virus shedding pattern in patients at the time of diagnosis was investigated in this study. Our data demonstrated that the median time from symptoms onset to viral RNA shedding was 4 days, ranging from 0 to 39 days. This data is in agreement with a study in Wuhan in which the longest duration of viral shedding in survivors was 37 days [21]. Comparison of the SARS-CoV-2 load of severe cases with mild cases at different days since symptoms onset did not find a statistically significant difference up to 14 days of symptoms onset, but lately diagnosed patients (after 14 days) had higher viral load than patients with mild disease (p = 0.0218). Recently, Liu and co-workers studied the viral dynamics in mild and severe cases of COVID-19 and found that patients with severe disease had about 60 times higher viral load than that of mild cases [24], irrespective of the day of symptoms onset.
In this cohort, 10.59% of the patients died from COVID-19. The high case-fatality rate may be overestimated in this cohort may be due scarcity of testing in Brazil compared to developed countries. For instance, Brazil has performed only 68,143 tests per million people, whereas this rate in developed countries is over 100 thousand per million inhabitants. As of September 15, 2020, the case-fatality rate of COVID-19 is about 3.15%, with 936,651 deaths and 29,648,872 confirmed cases worldwide (https://www.worldometers.info/coronavirus/). A significant proportion of cases (72.27%) in this cohort reported comorbidities and arterial hypertension was the most common condition associated with COVID-19 infection followed by diabetes mellitus. Our findings is in accordance with a study investigating the first 1000 consecutive patients in New York [25] and also in other regions of the world [26].
5. Conclusion
SARS-CoV-2 continues to spread in Brazil causing unprecedented challenges to the country's health system. Herein, we described the epidemiological and clinical manifestations of the first 557 successive COVID-19 patients in Pernambuco state, Northeast Brazil. Our study provided important information about the demographics, clinics and epidemiology of COVID-19 in the tropical world and will assist physicians and health officials to face the current pandemics and be better prepared to counteract future incursions of highly transmissible respiratory pathogens in the human population.
CRediT authorship contribution statement
Jurandy Júnior Ferraz de Magalhães: Study design, Data collection, Data analysis, Writing - original draft, Writing - review & editing. Renata Pessoa Germano Mendes: Study design, Data analysis, Writing - original draft, Writing - review & editing. Caroline Targino Alves da Silva: Study design, Data analysis, Writing - original draft, Writing - review & editing. Severino Jefferson Ribeiro da Silva: Study design, Data analysis, Writing - original draft, Writing - review & editing. Klarissa Miranda Guarines: Study design, Data analysis, Writing - original draft, Writing - review & editing. Lindomar Pena: Study design, Data analysis, Writing - original draft, Writing - review & editing, Supervision, Funding acquisition, Others for the Pernambuco COVID-19 Research Group: Data collection, Data analysis, Writing - review & editing.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgments
C.T.A.S. and S.J.R.d.S are supported by a Master's and doctoral fellowships sponsored by the Foundation for Science and Technology of Pernambuco(Facepe)-Brazil, respectively. R.P.G.M is recipient of a Master's fellowship sponsored by CAPES-Brazil. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. We would like to express our sincere gratitude and appreciation to the Pernambuco State Health Secretary Dr. André Longo de Araújo Melo, the Executive Secretary of Health Surveillance Dr. Luciana Caroline Albuquerque, and their staff at the Pernambuco State Health Department for their contribution for the diagnosis of Covid-19 and providing the clinical epidemiological data of individuals affected by SARS-CoV-2 in Pernambuco. Dr. Pena is supported by grants from the International Development Research Centre (IDRC)-Canada (Project ID 109434) and the Fiocruz Inova Program.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.tmaid.2020.101884.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO . 2020. Coronavirus disease 2019 (COVID-19) - situation report - 51.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10 [Google Scholar]
- 5.PAHO . 2020. Brasil confirma primeiro caso de infecção pelo novo coronavírus.https://www.paho.org/bra/index.php?option=com_content&view=article&id=6113:brasil-confirma-primeiro-caso-de-infeccao-pelo-novo-coronavirus&Itemid=812 [Google Scholar]
- 6.Rodriguez-Morales A.J., Gallego V., Escalera-Antezana J.P., Mendez C.A., Zambrano L.I., Franco-Paredes C. COVID-19 in Latin America: the implications of the first confirmed case in Brazil. Trav Med Infect Dis. 2020;35:101613. doi: 10.1016/j.tmaid.2020.101613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Freitas E.S.R., Pitzurra R. What are the factors influencing the COVID-19 outbreak in Latin America? Trav Med Infect Dis. 2020;35:101667. doi: 10.1016/j.tmaid.2020.101667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pernambuco S.H.D. State Health Department; Pernambuco: 2020. Boletim epidemiológico COVID-19. Recife.http://portal.saude.pe.gov.br/boletim-epidemiologico-covid-19 [Google Scholar]
- 9.The Lancet COVID-19 in Brazil: "so what? Lancet. 2020;395(10235):1461. doi: 10.1016/S0140-6736(20)31095-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO . 2020. Clinical management of severe acute respiratory infection when COVID-19 is suspected.https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected [Google Scholar]
- 11.Corman V.M., Landt O., Kaiser M., Molenkamp R., Meijer A., Chu D.K.W. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rafael R., Neto M., Depret D., Gil A., Fonseca M., Souza-Santos R. Effect of income on the cumulative incidence of COVID-19: an ecological study. Rev Latino-Am Enferm. 2020;28:11. doi: 10.1590/1518-8345.4475.3344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jesus J.G., Sacchi C., Candido D.D.S. vol. 62. Revista do Instituto de Medicina Tropical de Sao Paulo; 2020. p. e30. (Importation and early local transmission of COVID-19 in Brazil, 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Canada Go . 2020. Coronavirus disease 2019 (COVID-19): epidemiology update 2020.https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html [Google Scholar]
- 17.Gebhard C., Regitz-Zagrosek V., Neuhauser H.K., Morgan R., Klein S.L. Impact of sex and gender on COVID-19 outcomes in Europe. Biol Sex Differ. 2020;11(1):29. doi: 10.1186/s13293-020-00304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jin J.M., Bai P., He W. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health. 2020;8:152. doi: 10.3389/fpubh.2020.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in wuhan, China. J Am Med Assoc. 2020 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang J.J., Dong X., Cao Y.Y., Yuan Y.D., Yang Y.B., Yan Y.Q. Allergy; 2020. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. [DOI] [PubMed] [Google Scholar]
- 23.Wan S., Xiang Y., Fang W., Zheng Y., Li B., Hu Y. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J Med Virol. 2020 doi: 10.1002/jmv.25783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu Y., Yan L.M., Wan L. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect Dis. 2020;20(6):656–657. doi: 10.1016/S1473-3099(20)30232-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Argenziano M.G., Bruce S.L., Slater C.L., Tiao J.R., Baldwin M.R., Barr R.G. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ. 2020;369:m1996. doi: 10.1136/bmj.m1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gold M.S., Sehayek D., Gabrielli S., Zhang X., McCusker C., Ben-Shoshan M. COVID-19 and comorbidities: a systematic review and meta-analysis. Postgrad Med. 2020 doi: 10.1080/00325481.2020.1786964. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.