Abstract
With growing antipathy toward conventional prescription drugs due to the fear of adverse events, the general and patient populations have been increasingly using complementary and alternative medications (CAMs) for managing acute and chronic diseases. The general misconception is that natural herbal-based preparations are devoid of toxicity, and hence short- and long-term use remain justified among people as well as the CAM practitioners who prescribe these medicines. In this regard, Ayurvedic herbal medications have become one of the most utilized in the East, specifically the Indian sub-continent, with increasing use in the West. Recent well-performed observational studies have confirmed the hepatotoxic potential of Ayurvedic drugs. Toxicity stems from direct effects or from indirect effects through herbal metabolites, unknown herb-herb and herb-drug interactions, adulteration of Ayurvedic drugs with other prescription medicines, and contamination due to poor manufacturing practices. In this exhaustive review, we present details on their hepatotoxic potential, discuss the mechanisms, clinical presentation, liver histology and patient outcomes of certain commonly used Ayurvedic herbs which will serve as a knowledge bank for physicians caring for liver disease patients, to support early identification and treatment of those who present with CAM-induced liver injury.
Keywords: Ayurveda, Complementary and alternative medicines, Drug induced liver injury, Herb induced liver injury, Chronic liver disease, AYUSH system
Core Tip: Ayurvedic herbal medications (AHM) can cause liver injury ranging from an asymptomatic elevation of liver enzymes to cirrhosis and portal hypertension. Patients who develop AHM-related liver injury have a history of consumption of complex polyherbal formulations. In most cases, identification of the offending hepatotoxic agent is difficult due to the number and complexity of herbs involved. However, multiple observational studies, quality case series, and well-performed case studies have demonstrated the hepatotoxic potential associated with certain herbs used in Ayurvedic practice. The commonly utilized and over-the-counter available Indian herbs or their extracts, such as Ashwagandha, Aloe vera, Guggul, Puncture vine, Turmeric, Gotu-kola, Bakuchi, Senna, Noni, Malabar tamarind, and Gurmar have been associated with various types of liver injury ranging from acute self-limiting hepatitis, chronic hepatitis, prolonged cholestasis, hepatic sinusoidal obstruction syndrome, cirrhosis, and portal hypertension and can present clinically as acute severe liver injury, acute liver failure, acute decompensation of cirrhosis or acute on chronic liver failure. Physician knowledge regarding regional and local complementary and alternative practices among the general and patient population is essential in identifying those who develop complications of liver disease secondary to herbal hepatotoxicity, to make optimal treatment decisions, and for early prognostication.
INTRODUCTION
Ayurveda, an ancient traditional system of medicine, originated in the Indian sub-continent. According to Ayurvedic principles, the Universe is composed of five elements, namely, Vayu (Air), Jala (Water), Aakash (Space or ether), Prithvi (Earth) and Teja (Fire) that form the three elemental humors of the human body in varying combinations - the Vata dosha, Pitta dosha, and Kapha dosha, collectively called the “Tridoshas” that, along with five sub-categories for each of the primary doshas are thought to control all of the essential physiological functions of the human body. Even though practitioners of Ayurveda believe it to be a complete system of medicine, Ayurvedic science lacks the rigorous and ideal scientific approach required for disease diagnosis and treatment. This is underscored by the fact that prospective, well-designed, good quality controlled trials are deficient in the current literature concerning Ayurvedic practice[1]. In contrast, integrative approaches toward practices in Traditional Chinese Medicine (TCM) has been exemplary, improving our understanding of beneficial active components in Chinese herbs which have been ultimately utilized in the management of lethal and resource burdening diseases such as malaria. Ayurvedic herbal medicines (AHM) are broadly divided into non-proprietary or classical and proprietary drugs. In the former, manufacturing methodology follows principles and guidelines as per approved classical texts of Ayurveda (such as Charak Samhita or Susrut Samhita); while in the latter, private drug manufacturers decide on the content, composition and preparatory methods involved in the preparation of the AHM (examples include Himalaya® Liv 52™ or Charak® Livomyn™ syrup). Das et al[2] in a study from North-East India, found that unknown herbal medications were a significant cause of mortality among patients with acute liver failure (ALF). Similarly, Udayakumar et al[3] demonstrated that traditional indigenous herbal medications prescribed by South-Indian Tamil healers led to ALF with high mortality in affected patients[3]. In a large single-center series from South-India, Devarbhavi et al[4] found that Indian Ayurvedic medicines caused drug-induced liver injury (DILI) in 1.3% of patients in whom almost half of those affected died due to progressive liver failure. In a pioneering study, Philips et al[5] addressed clinical outcomes and analyzed component toxicology of AHMs causing severe DILI. In this study, patients were prescribed AHMs mainly for non-specific gastrointestinal symptoms. The overall mortality was approximately 19% and most of the formulations were unlabelled polyherbals, with high levels of arsenic and mercury which were significantly associated with death on follow-up[5]. The same authors showed that among cirrhosis patients consuming AHMs, 35.7% presented with severe DILI leading to acute on chronic liver failure (ACLF) with an overall mortality of 53%. In this series, the most common culprit leading to AHM-DILI were unlabelled polyherbal preparations followed by proprietary Ayurvedic drugs[6]. A recent multicentre study spearheaded by the Asian-Pacific Association for the Study of Liver (APASL) demonstrated that ACLF in Asia-Pacific countries was predominantly due to CAMs (in approximately 72% of patients) inclusive of Ayurvedic herbals and herbal and dietary supplements[4]. Components implicated in DILI related to Ayurvedic medicines are difficult to ascertain due to mislabelling or un-labelling of the product, presence of potentially toxic adulterants or contaminants, and importantly, the complex polyherbal nature of preparations. In this context, a precise knowledge regarding certain potentially hepatotoxic herbs is of utmost importance for the clinician while dealing with patients with AHM-related DILI. In this review, we discuss exhaustively from current literature, the hepatotoxicity of common Indian Ayurvedic herbs that are utilized in pure form or as mixtures; explore pertinent clinical presentations and outcomes with real-life patient examples and summarize to provide future directions on Ayurvedic herbs-related DILI.
AYURVEDIC HERBS WITH POTENTIAL HEPATOTOXICITY
Withania somnifera (Ashwagandha)
Ashwagandha is a herbal extract derived from the roots of Withania somnifera, an evergreen shrub endemic to India and Southeast Asia, commonly known as the Indian ginseng or winter cherry. It is claimed to have neuroprotective and anti-inflammatory properties and has been used to treat a variety of symptoms and diseases ranging from fatigue, stress, epilepsy and arthritis to cancer chemoprevention. Some Ayurvedic practitioners and drug manufacturers proclaim that Ashwagandha has “anti-aging” properties. Multiple studies performed on small animal-models and published in anecdotal journals have alleged a “liver safe” profile[7,8]. Apart from a few randomized clinical trials with small patient numbers but with penurious methodology, and short follow-up, there have been no rigorously performed, scientifically sound, prospective studies confirming the efficacy and safety of Ashwagandha in the current literature[9]. The bioactive compounds identified in Ashwagandha include steroidal lactone triterpenoids (called withanolides), alkaloids such as cuscohygrine, and anahygrine, flavonoids, phytosteroids and coagulins. The terpenoid Withaferin A is purported to have hepatoprotective properties. The first report of possible Ashwagandha-related DILI was from Japan. Inagaki et al[10] described a 20-year-old man with anxiety disorder who used twice the recommended dose of Ashwagandha bought online in combination with multiple antianxiety drugs. The pattern of DILI was of ”highly possible” cholestatic type as per the Digestive Diseases Week – Japan 2004 (DDW-J) diagnostic criteria. The liver biopsy showed severe intrahepatic cholestasis with extensive canalicular bile plugs. The patient recovered uneventfully within 2 mo after treatment with ursodeoxycholic acid, phenobarbitone, and withdrawal of the offending drug. A drug-induced lymphocyte stimulation test revealed reactivity and drug interactions between Ashwagandha, propranolol, and alprazolam[10]. Björnsson et al[11] reported on a series of patients from Iceland and the United States Drug-Induced Liver Injury Network (DILIN) with liver injury due to Ashwagandha. The authors described five patients, mostly males with a mean age of 43 years, who developed cholestatic jaundice after consuming a herbal supplement ranging from 2 to 12 wk. Liver injury was cholestatic or mixed type and liver biopsy showed severe cholestatic hepatitis. The clinical course was prolonged, ranging from 5 to 20 wk and normalization took up to 5 mo. None of the patients developed liver failure. Chemical analysis using liquid chromatography coupled to quadrupole time-of-flight mass spectrometry on the retrieved products confirmed the presence of Ashwagandha, the absence of other toxic compounds or the presence of potentially hepatotoxic conventional drugs. In one patient, the additional consumption of Rhodiola rosea (golden root or roseroot) was suspected to have caused a herb-herb interaction resulting in the liver injury[11]. Ashwagandha-containing herbal medications can result in severe cholestatic liver injury, which may be prolonged, but self-liming without the development of chronic DILI or ALF (Figure 1).
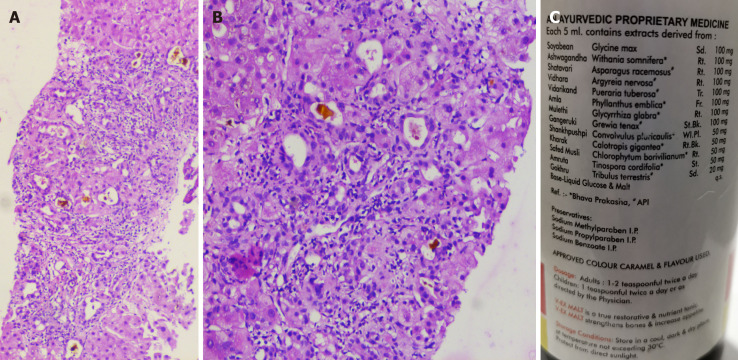
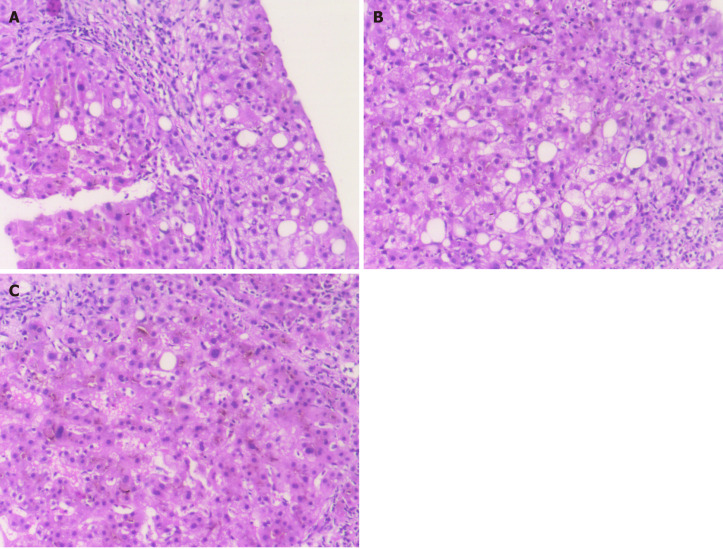
Figure 1.
Liver histopathology of acute liver injury in a patient ingesting Ashwagandha. A and B: Percutaneous liver biopsy revealed severe canalicular cholestasis along with moderate portal inflammation [A, hematoxylin and eosin stain (H&E), 40 × and B, H&E stain, 400 ×)]; C: The polyherbal formulation containing Ashwagandha, retrieved from the patient is shown in C. The patient had an uneventful course with resolution of symptoms and normalization of liver tests at 2 mo.
Bacopa monnieri and Centella asiatica (Brahmi/Gotu Kola)
The herb Brahmi, used synonymously with Gotu Kola is extensively utilized in Ayurveda due to its seemingly beneficial effect on neurocognitive functions. Both have distinct biochemical component properties, pharmacokinetics, and pharmacodynamics, and are considered separate herbs in the ancient Ayurvedic texts. Nonetheless, both are commonly used as memory ”boosters” or cognition enhancers. Brahmi is essentially Bacopa monnieri, a perennial non-aromatic creeping herb, also called the water hyssop. The primary bioactive constituents of Brahmi include steroidal saponins called bacosides, alkaloids such as Brahmine, herpestine, and nicotine. Gotu Kola or Centella asiatica commonly called the Indian pennywort, is a perennial flowering plant that is indigenous to the Indian subcontinent and Southeast Asia. Similar to Brahmi, the bioactive components in Gotu Kola are saponin-triterpenoids, which include asiaticosides, brahmoside, and Brahminoside as well as the glycosides isothankuniside and thankuniside[12,13]. In their report on severe hepatotoxicity due to Ayurvedic herbal products, Teschke and Bahre described an older woman who developed a severe hepatocellular type of DILI after consuming multiple herbal products for 9 mo for vitiligo. All other competing causes were systematically excluded by the authors. On structured causality assessment using the Council for International Organizations of Medical Sciences (CIOMS) scale on individual products, the authors found that primary hepatotoxicity was possibly due to ”Bakuchi” tablets (score 8+), containing extracts of Psoralea corylifolia (also called babchi or purple fleabane; discussed later). However, the CIOMS score was 6+ (possible) for Brahmi tablets. Properly conducted structured studies or pharmacovigilance on organ-specific toxicity of Brahmi is deficient in current literature[14]. Gotu Kola is also implicated in contact dermatitis (due to the presence of madecassoside) and infertility due to bioactive components, isothankuniside, and thankuniside[15,16]. An Argentinian group of researchers were the first to describe a series of women in whom ingestion of Gotu Kola for weight loss for approximately one to two mo resulted in severe cholestatic hepatitis. Liver biopsy revealed acute granulomatous hepatitis, with marked necro-inflammatory activity and eosinophilic degeneration mainly in zone 3, along with a lymphoplasmacytic infiltrate in all patients, and additional features of chronic hepatitis with prolonged cholestasis and progression to cirrhosis in one patient. In the patient with chronic DILI-related cirrhosis, acute decompensation developed with repeat intake. In other patients, drug withdrawal, along with a short course of corticosteroids and ursodeoxycholic acid therapy resulted in a complete reversal of liver injury at one year follow-up. In the first patient, repeat consumption of Gotu Kola seven mo later led to recurrence of DILI with similar biopsy features to the initial biopsy. In both instances, autoantibodies were positive favouring the possibility of immune-mediated DILI[17]. In another report, Gotu Kola intake for 6 wk for acne treatment led to ALF in a 15-year old girl with complete resolution of illness after drug withdrawal[18]. Phytochemicals such as alkaloids and cyclic compounds undergo biotransformation in the liver leading to the generation of metabolites that cause direct damage to hepatocytes and cholangiocytes or generate antigens, which trigger immune-mediated liver injury. In Gotu Kola, the bioactive compounds such as asiaticoside are triterpenoids which belong to the same family of hepatotoxic saponosides found in other herbs such as germander and Chinese skullcap. These bioactive compounds induce apoptosis through alteration of cellular transport at the cell membrane level, which characteristically could result in eosinophilic degeneration and cellular necrosis seen on liver histopathology[14-17]. Brahmi or Gotu Kola related DILI presents with cholestatic granulomatous hepatitis and severe autoantibody mediated necroinflammation (Figure 2). A strong suspicion for the intake of these herbs should be considered in patients presenting with acute onset cholestatic hepatitis with autoantibodies and biopsy features of granulomatous hepatitis after excluding other causes.
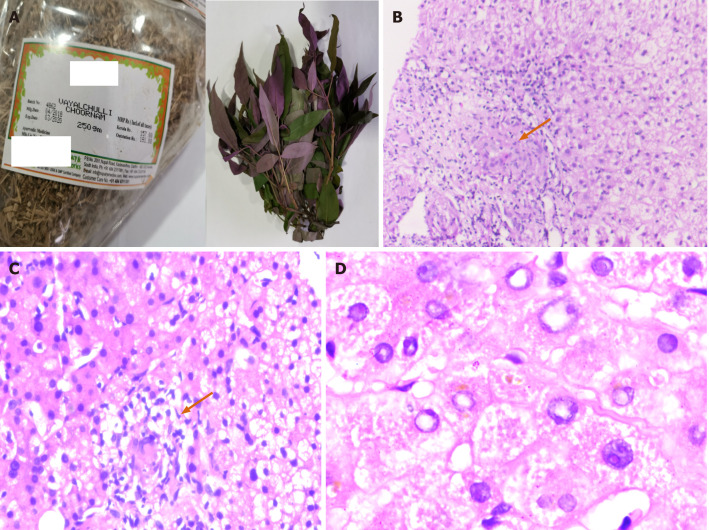
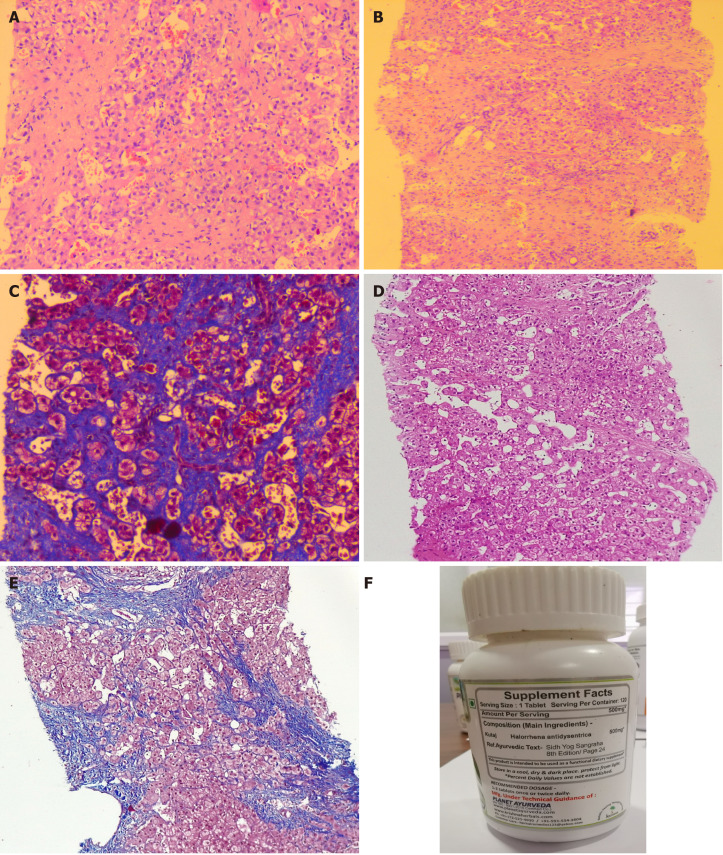
Figure 2.
Granulomatous hepatitis in a patient consuming multiple Ayurvedic herbs. The retrieved herbs implicated in acute liver injury with granulomatous hepatitis are shown in A (Hygrophila auriculate, also called the Marsh Barbel and an unknown coloured herb). Transjugular liver biopsy was performed in view of ascites in this patient. The liver histology revealed large vague as well as well-formed lobular and portal based granulomas and associated eosinophilic and lymphocytic inflammation within the sinusoids [B and C; hematoxylin and eosin (H&E), 100 × and 400 × respectively]; severe feathery degeneration of hepatocytes associated with hepatocellular cholestasis was also notable (D, H&E, 400 ×). This patient died after 6 mo follow-up due to portal hypertensive events complicated by septic shock.
Curcuma longa (Turmeric)
Turmeric and its bioactive compound curcumin are derived from the root of Curcuma longa, a perennial plant that is native to India, belonging to the ginger family. In Ayurvedic practice, it is heavily used as an anti-inflammatory and antioxidant as well as for digestive system-related symptoms and diseases such as pharyngitis, inflammatory bowel disease and fatty liver disease. Turmeric contains 3%-6% polyphenolic compounds (curcuminoids) such as curcumin, desmethoxycurcumin, and bisdemethoxycurcumin, which are responsible for its bioactivity. Turmeric is also rich in phytosteroids and bioactive compounds that have immunomodulatory properties[19,20]. Even though Ayurvedic practitioners vouch for the multisystemic beneficial effects of turmeric, a strong scientific basis for its efficacy and safety has not been proven through meticulous clinical studies. The majority of the beneficial effects of turmeric or its bioactive agents are still confined to small animal model studies without adequate translation to human diseases[21]. Lukefahr et al[22] described the case of highly probable drug-induced autoimmune hepatitis (AIH) ascribed to ingestion of turmeric dietary supplement for 10 mo in a 76-year old woman. The immunoglobulin G levels were elevated along with positive autoantibody titres for atypical perinuclear anti-neutrophil cytoplasmic antibodies and antibody to smooth muscle actin. Liver histopathology was compatible with AIH, and other causes of acute hepatitis were ruled out. After withdrawing the turmeric supplement, liver injury improved within 1 mo and returned to normal within a year and remained so at the three year follow-up[22]. Similar reports of AIH-like severe hepatitis associated with turmeric use were reported by Suhail et al[23] and Lee et al[24]. Imam et al[25] reported the case of a 78-year old female who ingested an over-the-counter curcumin supplement for dyslipidemia for 1 mo. She presented with progressive jaundice without cholestasis. The DILI was of hepatocellular type and other competing causes of acute hepatitis were ruled out. After stopping the supplement, the liver tests showed approximately 50% improvement at the end of one week and complete resolution by day 42. The authors did not review or analyse the curcumin supplement for adulterants and contaminants, and a liver biopsy was not performed given clinical improvement[25]. Luber and co-workers described two cases of curcumin-related severe hepatocellular DILI in their paper. The first patient was a woman in her early fifties with cholestatic hepatitis on Ancient Wisdom™ High Potency Turmeric (375 mg curcuminoids + 4 mg black pepper) for 1 mo before the onset of symptoms. Her liver biopsy revealed severe lobular mixed inflammation and interface hepatitis. After resolution of liver injury within 2 mo, she restarted the turmeric supplement (1125 mg curcuminoids per day) for 3 wk and presented with severe cholestatic hepatitis again. Further withdrawal resulted in complete resolution of symptoms. Analysis of the sample did not reveal any adulterants, toxins, heavy metals, or synthetic drugs. The second case was of DILI with autoantibodies in a 55-year-old male with metabolic syndrome after ingestion of turmeric-based supplements for cardiovascular health[26]. Similar biopsy findings and clinical outcome related to turmeric-induced severe liver injury was reported by Chand et al[27]. The patient developed additional features of severe myalgia, skin rash, and arthritis which resolved with normalization of liver tests after turmeric supplement withdrawal. We noted that in a middle-aged female patient with compensated hepatitis B virus-related cirrhosis, the use of turmeric capsules (1g per day for 3 wk) resulted in severe spur-cell anemia requiring blood transfusion, which resolved spontaneously on drug withdrawal, but reappeared after rechallenge (same dose for 2 wk) to resolve again after halting the turmeric supplement (Figure 3). To summarize, turmeric and its bioactive compounds have been implicated in rare but severe autoimmune hepatitis-like liver injury and rarely, severe self-limiting cholestasis with the potential to recur with drug rechallenge.
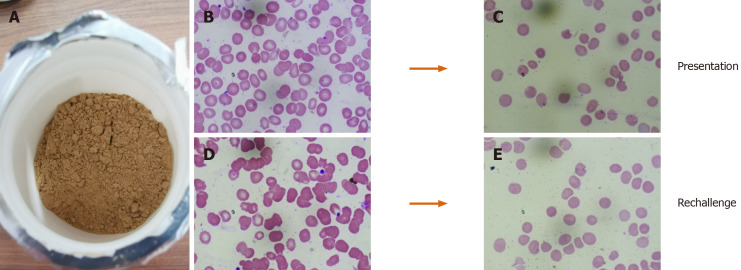
Figure 3.
Turmeric-induced spur cell anemia in a patient with compensated cirrhosis. The retrieved turmeric powder supplement is shown in A; B and C (Wright Giemsa stain, 40 ×) shows the presence of spur cells and resolution of spur cells on turmeric withdrawal. On rechallenge (D and E; Wright-Giemsa stain, 40 ×) with turmeric supplement, spur cells reappeared without the need for blood transfusion, only to resolve after withdrawing the offending agent again.
Commiphora wightii or mukul and Boswellia serrata (Guggul, Guggulu or Gugulipid)
Guggul is the gum resin procured from the white sap of various plants used in Ayurvedic practice. Two plants, Commiphora wightii (Indian bdellium or myrrh tree) and Boswellia serrata (Salai or Sallaki guggul or Shallaki from Indian olibanum or frankincense tree) are commonly utilized to prepare guggul. Guggul is considered to have beneficial effects on multiple organ systems and is used to treat symptoms ranging from leg swelling and non-specific ulcers to diseases such as inflammatory bowel disease and aggressive malignancies. The main ingredients of guggul are guggulsterone, guggulsterol, boswellic acid and an ethyl-acetate soluble fraction called guggulipid consisting of highly bioactive phytochemicals. A large number of in vitro and in vivo studies have shown that guggul and its bioactive components act on multiple molecular targets leading to anti-inflammatory, antioxidant, and anti-apoptotic activity. This has led to the use of guggul for conditions such as arthritis, in fat-burners, for dyslipidemia and cardiovascular health. However, studies on the safety and clinical efficacy of guggul or its specific bioactive components are non-existent in published literature[28]. Grieco et al[29] described the case of a 63-year-old woman who consumed an over-the-counter lipid-lowering Ayurvedic product called ”Equisterol®” (containing guggul sterol, sitosterol, chlorogenic acid, policosanol, multivitamins and red yeast rice derived monacolin) for 6 mo which was followed by the development of acute severe hepatitis. Liver biopsy revealed extensive necroinflammation with eosinophilic infiltration of hepatic lobules. Drug withdrawal and supportive care led to complete resolution of symptoms and normalization of liver tests within 10 d. The liver injury could have been due to the monacolin (with statins like activity) in red yeast, even though herb-yeast interaction was not ruled out[29]. Yellapu et al[30] described a female bodybuilder who consumed a multi-ingredient fat burner supplement leading to ALF. The supplements (Somalyz and Lipolyz, Species Nutrition, United States) contained usnic acid, L-carnitine, choline and ethanolamine, gamma-aminobutyric acid, vitamin E, green tea extract, guggulsterone Z, and guggulsterone E. She underwent cadaveric liver transplantation and was discharged uneventfully. Explant histopathology revealed massive hepatic necrosis and parenchymal collapse with a few areas of ductular regeneration. Even though various known plant-derived hepatotoxins (such as usnic acid, green tea extracts) were components of the supplement, the presence of guggul and its interactions were not ruled out. Guggul use has been implicated in the development of skin rash, diarrhea, headaches, nausea, and liver toxicity with high doses[30]. As reported by Polavarapu and co-workers, a 44-year old male developed fatigue, malaise, and jaundice after consuming a fat-burner product (Lipo-6™ containing guggulsterones and green tea extract) for 1 mo. Withdrawal of the herbal supplement resulted in complete clinical resolution after 1 mo[31]. Dalal et al[32] described a middle-aged woman who developed severe hepatocellular jaundice due to the intake of three different Ayurvedic herbal and Homeopathic medications (punarnaya mandur, extract from the Boerhavia diffusa and kanchnar guggulu, extract from Bauhinia variegate). Liver biopsy demonstrated mild portal chronic inflammation and interface activity with grade 3 bridging fibrosis, presence of ceroid-laden Kupffer cells, and conspicuous eosinophils suggestive of herbal-induced liver injury. Analysis of the retrieved herbal products and other medications did not reveal known hepatotoxic components, and the patient improved after a short follow-up[32]. Guggul and its bioactive compounds have been implicated in possible and probable DILI with hepatocellular pattern of liver damage, which is usually self-limiting. However, there have been reports of ALF requiring liver transplantation when guggul compounds have been part of multiherbal fat-burner products, a herb-herb interaction that remains unexplored (Figure 4).
Figure 4.
Guggul-related liver toxicity. The liver histopathology showed zone 3 necrosis extending to the portal region [A, hematoxylin and eosin (H&E) stain, 40 ×] with mixed neutrophilic and eosinophilic inflammation of the portal region associated with severe ductular reaction and early fibrosis (B, H&E stain, 100 ×). Associated moderate to severe canalicular cholestasis is also noted (C, H&E stain, 40 ×).
Psoralea corylifolia (Bakuchi)
Psoralea corylifolia, commonly known as purple fleabane, is a popular herb used in Ayurvedic medicine for the treatment of various skin disorders. It is a perennial plant with growth throughout the plains of the Indian continent. Seeds of the plant (known as Fructus Psoraleae, FP) are mainly used for treating leprosy (hence the Sanskrit name, ”kushtanashini” or destroyer of leprosy), psoriasis, leukoderma, and vitiligo. The monoterpenoid phenol called bakuchiol is the most important phytochemical component. Other constituents include coumarin compounds such as active psoralens, benzofuran derivatives and flavonoids[33]. A case of severe acute cholestatic hepatitis associated with FP was reported by researchers in South Korea in a post-menopausal woman consuming more than the recommended dose of the extract for osteoporosis. The liver biopsy findings were suggestive of zone 3 necrosis, cholestasis, and mixed inflammation in the lobules[34]. Three further cases of severe hepatotoxicity due to FP was reported by Cheung et al[35]. The analysis of the retrieved proprietary medicines revealed psoralens and bakuchiol[35]. In another report, Bakuchi tablets were considered the cause of severe hepatocellular type liver injury in an older woman consuming Ayurvedic medicines for vitiligo[32]. A similar case was reported by Smith et al[36], of a 52-year old female who presented with a one-week history of jaundice and severe pruritus with abdominal pain after ingesting Bakuchi seeds for vitiligo. The liver biopsy revealed centrilobular necrosis with collapse, extensive cholestasis with mixed lobular inflammation. Clinical improvement and normalization of liver chemistries were notable at 3 mo follow-up[36]. Recently, Li and colleagues described a case of severe cholestatic hepatitis leading to fatal ALF due to the consumption of Bakuchi seeds over 7 mo in a 53-year-old with vitiligo. Studies have shown multiple mechanisms for Bakuchi-related liver toxicity. The psoralen-induced inhibition of the mTOR signalling pathway, mitochondrial injury, and impairment in liver regeneration with deleterious effects on liver lipid metabolism (such as reduction of mRNA expression of CYP7A1, HMG-CoA reductase, PPARα and increased expression of BSEP) along with dose and frequency related accumulation of psoralen has been shown to promote hepatotoxicity in small animal and in vitro studies[37-39]. To summarize, prolonged use of Bakuchi is associated with severe cholestatic hepatitis, mostly related to hepatotoxic psoralen compounds and bakuchiol, that can lead to ALF and death in predisposed patients.
Cassia angustifolio (Indian Senna)
Cassia angustifolia or the Indian or Tinnevelly senna (containing tinnevellin glucosides) belong to the legume family of Fabaceae, which comprise mostly ornamental plants. Leaves and sometimes flowers and fruits of the senna plant are used in herbal teas and as laxatives in Ayurvedic and Egyptian or Alexandrian (species known as Cassia acutifolio; containing 6-hydroxymusicin glucoside) traditional medicine. Some consider senna to be a safe herbal alternative for weight loss. The major bioactive components are anthracoids (sennoside A and B), which are primarily anthraquinone glycosides[40]. Beuers et al[41] described a 26-year old nurse who presented with severe cholestatic hepatitis after consuming high doses of senna-based medicines for 1 mo (senna fruit extracts corresponding to 100 mg sennoside daily along with 10 g of folia sennae laxative herbal tea twice weekly). Her liver biopsy showed extensive necrosis around the central veins, moderate portal and lobular infiltration of lymphohistiocytes and occasional plasma cells in the absence of autoantibodies. After drug withdrawal, liver tests, and clinical symptoms normalized, only to recur after resuming senna medications after 2 mo, and improving again, after drug withdrawal. Sennosides are converted into rhein anthron in the intestine most commonly by Escherichia coli, which is then absorbed through the intestinal mucosa, glucuronidated, or sulfated and excreted through feces and urine. Rhein anthron is structurally similar to danthron, which is a well-known hepatotoxic laxative. The anthraquinones in rhubarb of which rhein anthron is a major component has been shown to be associated with liver injury[41]. A similar case was reported by Sonmez et al[42] in a 77-year old male in whom liver biopsy revealed bridging hepatocellular necrosis and canalicular cholestasis with slow but steady normalization of DILI on long-term follow-up. Seybold et al[43] reported the case of a young woman with CYP2D6*4 homozygous variant in whom, the repeated use of comparatively small quantities of senna herbal tea led to severe acute hepatitis which resolved after drug withdrawal. The authors concluded that ”poor metabolizers” of phase I hepatic detoxification were predisposed to severe liver injury due to senna[43]. Vanderperren et al[44] demonstrated that chronic ingestion of large amounts of senna fruits in the form of herbal tea led to ALF associated with acute kidney injury and severe coagulation failure in a 52-year old woman. Investigations revealed large amounts of cadmium on urine toxicology consistent with possible contamination of the herbal product with heavy metals[44]. Cadmium is a well-known cumulative nephrotoxic and hepatotoxic agent, demonstrated in multiple Ayurvedic herbal products as a contaminant or adulterant and associated with severe liver injury[4,5,45,46]. Severe hepatotoxicity leading to fatal ALF was noted in an older woman consuming Senna occidentalis (S. occidentalis) herb for constipation. S. occidentalis is a common weed that is considered highly toxic to cattle and small herbivores. Recurrent annual outbreaks of a hepato-myo-encephalopathy syndrome in children in western Uttar Pradesh in India due to S. occidentalis poisoning was also reported by Vashishtha et al[47,48]. In the absence of proper regulatory standards, oversight, and poor manufacturing practices associated with Ayurvedic medicines, contamination of classical senna preparations with similar but more toxic herbs remain a possibility for causes concerning sporadic liver injuries[49]. Portal vein thrombosis due to consumption of boiled, dried Indian senna leaves in a 42-year old woman without underlying comorbid disease or prothrombotic conditions was also reported in the literature[50]. To summarize, senna is associated with severe hepatocellular and cholestatic liver injury and possible renal injury due to the presence of anthraquinone alkaloids in predisposed patients. The clinical course is usually self-limiting with liver toxicity proven on re-challenge; however, in rare instances, fatal ALF has been reported.
Aloe barbadensis mille (aloe vera)
Aloe vera is a perineal, xerophytic, succulent, cactus-like shrub belonging to the Lily family used for centuries in traditional medicine for the management of skin diseases, wound healing; and orally as an anti-oxidant. Aloe is derived from the Arabic word ”Alloeh, ” meaning ”shining bitter substance” while ”vera” is Latin for ”true” and called by Egyptians as the ”plant of immortality. ” The aloe leaf contains glucomannans such as acemannan, the anti-inflammatory glycoprotein alprogen and multiple anthraquinones such as aloin and emodin and the plant hormones auxins and gibberellins[51]. The first report of aloe-induced acute hepatitis was published by Rabe et al[52] from Germany in 2005. In their paper, a middle-aged woman developed acute severe cholestatic jaundice after ingesting aloe supplements (500 mg tablets) for 4 wk to delay ”aging”. The liver biopsy revealed portal and lobular lymphoplasmacytic infiltrates and eosinophilic granulomas with bridging necrosis and bilirubinostasis. The liver injury and symptoms abated after stopping the aloe tablets. The authors contemplated that the liver injury was possibly due to the presence of bioactive aloe alkaloids acting on the cytochrome P450 system resulting in detoxification process interference and direct action of biotransformation end metabolites causing hepatocytotoxicity[52]. Since its original description, multiple reports, including patient series from Korea and Sweden and an extensive literature review on aloe-induced hepatitis, have been published in the literature. Liver biopsy findings in subsequent studies also featured severe hepatocyte ballooning, apoptosis, extensive cholestasis, and the presence of eosinophils predominant lobular inflammation[53,54]. Apart from hepatotoxicity, additional systemic toxicity in the form of severe intraoperative bleeding due to probable interaction between aloe plant-derived prostaglandins and sevoflurane during leg surgery in a young woman; renal failure due to over-dosing on aloe products; aloe-induced Henoch-Schonlein purpura and cathartic melanotic colon with adenomas are reported with aloe vera use[55]. Patient series of herbal and dietary supplements induced liver injury, mostly due to Herbalife® products, containing aloe-vera extracts leading to severe liver injury are also well documented in certain pharmacovigilance registries such as the Spanish DILI registry[56]. Even though in vitro and in vivo studies have demonstrated the detoxifying and hepatoprotective potential of aloe vera, well-conducted translational clinical trials in humans confirming this aspect are still lacking in published literature. Aloe-related acute decompensation of cirrhosis in a chronic hepatitis C virus patient, presenting with acute severe cholestatic jaundice, was reported by Vázquez-Fernández et al[57]. To summarize, oral aloe vera use ranging from 2 wk to 24 wk, reportedly leads to severe cholestatic hepatitis among predisposed patients as well as acute severe decompensation in patients with underlying chronic liver disease. The injury is mostly of the hypersensitive type and self-limiting but may have a prolonged morbid course (Figure 5).
Figure 5.
Aloe vera-induced liver injury in a middle-aged diabetic woman. The percutaneous liver histopathology showed porto-portal bridging necrosis [A, hematoxylin and eosin (H&E) stain, 200 ×] associated with moderate to severe ballooning of hepatocytes, hepatocyte fall out and neutrophilic satellitosis (B, H&E stain, 400 ×). Severe intrahepatic and canalicular cholestasis is also noted (C, H&E stain, 400 ×).
Morinda citrifolia (Indian mulberry or Noni juice)
Morinda citrifolia, commonly known as noni, belongs to the coffee family cultivated throughout the tropical countries. Due to its strong and pungent odor, it is also known as cheese fruit or vomit fruit. Noni-related products in the form of juice or extracts are considered by traditional medicine practitioners to benefit diseases from mouth ulcers to diabetes and HIV-AIDS even though high quality and reproducible studies demonstrating alleged clinical efficacy are non-existent in the literature. Published data on the efficacy and safety of noni juice and extracts are limited to in vivo and in vitro studies that are widely (and inaccurately) quoted by manufacturers and sellers of noni juice as strong evidence for its practical and safe use. Compositional analysis of noni demonstrated alkaloids (xeronine), polysaccharides, anthraquinones (damnacanthal, morindone), and glycosides such as citrifolinoside[58]. Austrian researchers described a 45-year-old man who consumed noni juice for 3 wk as a ”prophylactic antioxidant, ” and developed acute hepatitis. The liver biopsy revealed severe mixed inflammation of the portal tracts along with marked eosinophils, hepatocellular cholestasis in zone 3, and histiocytic infiltration of the sinusoids. Complete resolution occurred within ten days of stopping noni juice[59]. Stadlbauer et al[60] described the occurrence of ALF requiring liver transplantation in a 29-year-old man and severe acute hepatitis due to consumption of noni juice for 3-mo in an elderly woman with a self-limiting disease course in the latter. The biopsies revealed severe mixed inflammation of portal tracts and lobules along with extensive centrilobular necrosis and severe ballooning associated with mixed inflammation[60]. Nonetheless, the development of ALF in the former patient cannot be solely attributed to noni juice since multiple other potentially toxic herbal supplements such as Skullcap (a known hepatotoxic Chinese herb), and green tea extracts were also consumed during the same period. Further reports of liver injury due to noni juice have been published from Croatia, Germany, and recently the United States. In these cases, where liver biopsy was performed, the findings were similar to previously described cases – a predominant hepatocellular form of liver injury with a mixed pattern of inflammation with marked eosinophilic infiltration of portal tracts, perivenular hepatocellular zonal necrosis with hepatocellular or canalicular cholestasis. All had a self-limiting disease course with complete clinical resolution within weeks to months[61]. Manufacturers and proponents advocating the benefits of noni juice with vested business interests have been keen to publish their retaliation against published literature on noni juice-related hepatotoxicity. However, almost all of their justifications have been biased and based on anecdotal and narrative evidence especially the efficacy and safety aspects of noni juice since idiosyncratic hepatotoxicity as a possibility has never been ruled out[62]. Further to this, multiple instances of the United States Food and Drug administration serving warning letters to manufacturers for making false claims on the curative and health benefits of noni has been in the limelight recently[63]. Current literature on the hepatotoxicity of noni juice demonstrates a possible self-limiting idiosyncratic type of herb-induced liver injury, probably due to anthraquinones, presenting with a severe hepatocellular type of liver damage with a predominance of eosinophilic portal inflammation, central necrosis, and cholestasis.
Ayurvedic herbs containing pyrrolizidine alkaloids
Alkaloids belong to the group of amino acid-derived, nitrogen-bearing molecules displaying a wide range of biochemical activities. Pyrrolizidine alkaloids (PAs) are those derived from ornithine and are commonly found as esters formed by a necine base (amino alcohols) and one or more necic acids (mono- or aliphatic dicarboxylic acids). Accordingly, based on the structure of the necine base, PAs may be sorted into four groups: Retronecine-, heliotridine-, otonecine- and platynecine-types. The following plant species - Heliotropium sp., Trichodesma sp., Symphytum sp. (known as Comfrey), Senecio sp. (used in Bush teas), Eupatorium sp., Crotalaria sp. (commonly used in Indian Ayurveda), Chelidonium majus sp., and Castilleja sp. are known to be rich in PAs. In 1968, Mattocks was the first to describe the hepatotoxicity mechanism of PA, which leads to hepatic veno-occlusive disease, currently known as hepatic sinusoidal obstruction syndrome (HSOS), a condition that can lead to liver failure potentiating organ transplantation or to cirrhosis and portal hypertension[64]. PAs are transformed and activated into intermediate metabolites of which dehydropyrrolizidine alkaloids (DHPAs) are of significance. DHPA bind with groups containing sulfur, nitrogen, and oxygen present in proteins to form adducts that penetrate the nucleus and react with DNA, ultimately causing DNA cross-links and DNA-protein cross-links resulting in genotoxicity and abnormal cellular function primarily in the liver, leading to hepatocyte damage. These adducts pass to the adjacent space of Dissé as well as the sinusoidal lumen, where they injure the sinusoidal cells leading to HSOS. Apart from the liver, DHPA can also reach the pulmonary arterioles leading to secondary pulmonary hypertension and, in the long-term, congestive heart failure. Tricodesmine, a PA metabolism byproduct is neurotoxic and can cause encephalitis, vertigo, delirium and coma. The case of HSOS in a newborn of a woman who consumed herbal tea prepared from Tussilago farfara L showcasing the teratogenicity of PA is also reported[65]. The cognizance that PA-containing herbs can promote HSOS development comes from the identification of a large number of sporadic cases from Africa and the Indian subcontinent among those consuming herbal teas and ingesting traditional healer concoctions. Cross-contamination of herbal teas with PA-rich herbs leading to liver toxicity is also described. In India, consumption of honey processed (during pollen drying) using PA containing Crotalaria juncea L has been demonstrated to promote PA toxicity[66]. Figure 6 demonstrates the serial liver biopsy of a young male who developed HSOS leading to cirrhosis and portal hypertension at one year follow-up, after consuming over-the-counter capsule extracts of Holarrhena antidysenterica (pubescens) for ”indigestion” for 1 mo. H. antidysenterica contains PAs, and rats fed with extracts demonstrated liver toxicity in the form of injury to centrilobular veins, centrilobular sinusoidal hemorrhage, congestion and centrilobular and focal hepatocellular necrosis compatible with PA-induced damage[67]. Thorough knowledge of herbs promoting chronic and sub-acute liver injury, and careful assessment of herbal components in polyherbal medications is mandated by physicians treating probable cases of DILI due to Ayurvedic drugs to diagnose rare but possible causes of herbal hepatotoxicity that may progress to chronic liver disease and portal hypertension.
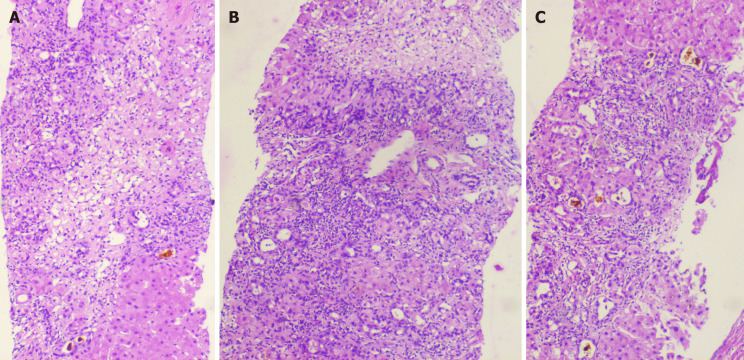
Figure 6.
Hepatic sinusoidal obstruction syndrome in a young male who consumed Holarrhena antidysenterica, known to contain pyrrolizidine alkaloids. Transjugular liver biopsy was performed in view of ascites. The liver histology showed fairly preserved portal areas with extensive sinusoidal dilatation in all zones associated with early sinusoidal and peri-sinusoidal fibrosis [A and B, hematoxylin and eosin (H&E) stain, 400 ×]; the sinusoidal fibrosis is quite evident on Masson-trichrome stain (C, 400 ×); after one year follow-up, in view of recurrence of ascites and acute variceal bleeding, a repeat liver biopsy was performed which revealed prominent sinusoidal dilatation with sinusoidal and portal fibrosis (D, H&E stain, 200 ×) and cirrhosis changes with bridging fibrosis and partial nodule formation (E, Masson-trichrome stain, 200 ×). The retrieved over-the-counter herbal supplement is shown (F).
Miscellaneous Ayurvedic Herbs
Garcinia cambogia (Malabar Tamarind): Currently known as Garcinia gummi-gutta (L) Roxb, the fruit rind is extensively used as a flavouring agent in many parts of the Indian subcontinent. In Ayurvedic medicine, it has been purported to be a safe remedy for constipation, rheumatic diseases, helminthic infestation, and as a weight-loss agent due to its appetite suppressing activity. Hydroxy-citric acid (HCA), an α-,β-dihydroxy tricarboxylic acid, is the major component present in the fruit rind, which may be responsible for the anorexic property. Garcinia fruit contains approximately 10% to 30% HCA, which reduces weight gain by inhibiting adenosine triphosphate (ATP)-citrate lyase, the enzyme responsible for catalytic reactions during fatty acid synthesis. Further appetite suppression occurs through increased release of serotonin neurotransmitter that dissipates eating behaviour. Multiple small animal model studies have demonstrated the anti-diabetic, anti-obesity, hypolipidemic, anti-inflammatory, antimicrobial, anti-parasitic activity as well as hepatoprotective effects of Garcinia. However, none of these have translated into clinical practice or confirmed in randomized studies. Those endorsing the safety and efficacy of Garcinia uphold their beliefs on the basis of low quality studies[68]. A randomized double-blind controlled trial on Garcinia failed to show significant change in fat mass and body weight compared to placebo, while a recent meta-analysis demonstrated an uncertain overall effect on long-term weight[69,70]. A total of 24 case reports and 8 case series reporting adverse events among 66 patients after Garcinia extract consumption was published in the literature. Of these, 17 studies out of 32 describe cases of acute liver injury, liver failure, and hepatotoxicity, observed among 50 patients consuming pure Garcinia or supplement mixtures. The latency period lasted from a few days to one year with continued ingestion in some patients. Two patients died, eight required liver transplantation, while one developed chronic DILI leading to cirrhosis[71,72]. Hepatotoxic adulterants and contaminants such as high levels of chromium, cadmium, and thallium in marketed Garcinia supplements leading to acute liver injury have been reported in the literature[73]. Garcinia cambogia has been implicated in acute self-limiting hepatitis, as well as ALF requiring liver transplantation and progression to cirrhosis. Furthermore, poor manufacturing practices resulting in adulteration and contamination of proprietary Garcinia supplements add to the hepatotoxic potential of Garcinia independently or synergistically.
Gymnema sylvestre (Cow plant or ”Gurmar”): Known as the ”sugar destroyer, ” this perennial woody climbing herb belonging to the milk-weed family is commonly used for treating diabetes mellitus. The most important phytochemical constituents include triterpene saponins, which are collectively called gymnemic acids, the polypeptide gurmarin, and the alkaloid conduritol. Gymnemic acid type A is the most potent hypoglycemic component, highly concentrated in the shoot tips and least in the seeds. Some of the alkaloids and saponins also act as appetite suppressants. Shiyovich et al[74] described the case of a 60-year-old female who developed severe acute hepatitis after consuming ”gurmar tea” for diabetes for one week. The work-up for other competing causes of acute hepatitis was non-contributory. The liver histopathology revealed lobular disarray with severe necroinflammatory changes in the hepatic lobules, marked ductular proliferation, and neutrophilic infiltration of portal areas. A short course of corticosteroids and ”gurmar” withdrawal resulted in complete resolution of symptoms[74]. Gymnema is also one of the components of the well-described hepatotoxic herbal and dietary weight loss supplement, Hydroxycut®[75]. Physicians caring for patients with DILI and patients with diabetes mellitus opting for additional alternative therapies must be made aware of the potential liver-damaging effects of herbs such as Gymnema (Figure 7).
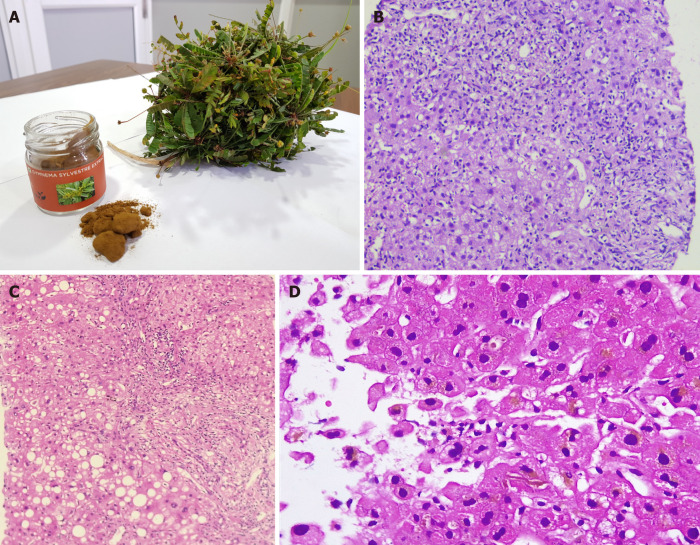
Figure 7.
Acute cholestatic hepatitis due to Gymnema sylvestre (gurmar or sugar destroyer) herb. The retrieved herbal supplement and an unknown herb is shown in A. Liver biopsy revealed moderate to severe neutrophil predominant interface hepatitis [B, hematoxylin and eosin (H&E) stain, 200 ×]; micro and macrovesicular steatosis, lobular inflammation and severe ductular reaction (C, H&E stain, 200 ×) and intrahepatic cholestasis with eosinophilic degeneration of hepatocytes (D, H&E stain, 400 ×).
Tribulus terrestis (”Gokshura” / Goat’s head / Devil’s weed or Puncture vine): Tribulus terrestris (TT), a tap-rooted herb belonging to the caltrop family, is native to regions with a tropical climate. It is known to be a noxious weed with a woody prickly fruit. Its use in Ayurveda for impotence and sexual disorders, and its use as a dietary supplement among bodybuilders and athletes, stems from the belief that it increases testosterone level, has anabolic steroid properties, and improves muscle strength – efficacy that lacks scientific proof through quality studies. The main biologically active phytochemicals in TT are steroidal saponins (mainly protodioscin, prototribestan, and dioscin), flavonoids, Harman alkaloids and lignan amides. TT ingestion is known to produce tribulosis (renal and liver injury) associated with the accumulation of phylloerythrin and beta-carboline alkaloids in the blood of cattle. It also causes staggers (neuromuscular ataxia) and geeldikkop (cholestatic liver injury and bile cast nephropathy) in sheep[76]. Talasaz et al[77] described a 28-year-old man who, after ingesting ”Tribulus Water, ” developed severe liver (transaminases > 40 times the upper limit of normal) and kidney dysfunction, and seizures leading to hypertensive crisis and advanced azotemia due to acute renal tubular dysfunction requiring haemodialysis. After a stormy 2 wk hospital course, both liver and renal parameters improved, and the patient was discharged[75]. Similarly, Ryan et al[78] described a young, healthy male who ingested TT herbal tablets for a few months as part of body-building, who presented with severe jaundice and pruritus, followed by acute renal failure with bile-casts in the renal tubules on histopathology evaluation. A percutaneous liver biopsy showed only severe cholestasis, well-preserved hepatic lobules without inflammation supporting evidence for cholestasis-induced renal damage in the patient, possibly due to TT use[78]. These reports shed light on the role of herb-induced non-serious liver injury, such as bland cholestasis indirectly leading to severe extrahepatic organ failure.
Valeriana officinalis (Valerian): Valerian is an herbal root extract form of Valeriana officinalis, a perennial flowering plant growing in Europe and Asia. The name is derived from the Latin verb ”valere” meaning ”strong, healthy.” Valerian is known to contain multiple bioactive phytochemicals such as actinidine alkaloid, valerianine, valerene and, gamma-aminobutyric acid. It is used as an anxiolytic and sedative in Ayurvedic medicine. Potential mechanisms for sedation are not yet fully identified as phytochemicals such as valeric acid, and other root-specific components did not demonstrate sedative properties in experimental models. It is believed that valerenic acid by acting on the 5-HT5A serotonin receptor modulates the sleep-wake cycle. The doubtful use of valerian as a sedative is underscored by a report on overdose in which the patient presented with mild symptoms that resolved within 24 h after consuming 20 times the recommended dose[79,80]. Valproic acid is a derivative of valeric acid. A small number of case reports have showcased hepatotoxicity associated with valerian. MacGregor et al[81] were the first to report on the potential hepatotoxic effects of valerian in 1989 in a series of four patients, all of whom consumed over-the-counter sleeping pills that also included other herbs. The presence of Chinese skullcap was thought to be the major inciting agent in these patients, but caution was advised against using valerian-based herbal combinations[81]. Cohen et al[82] described a young woman who developed self-limiting severe acute cholestatic jaundice after consuming capsules of valerian root extract 300 mg twice daily for 3 mo in the absence of other competing causes. Vassiliadis et al[83] described a 50-year-old woman with valerian extracts and tea consumption for 3 wk, after which she developed acute hepatitis. The liver biopsy showed mild portal fibrosis, lymphocytic, and eosinophilic inflammation of portal tracts, inflammatory changes of the small bile duct with ductular reaction and necrosis in the perivenular zone. Liver injury resolved after 10 mo on conservative management[83]. In a study on herb-induced liver injury in the Berlin Case-Control Surveillance program, possible causality for valerian-induced DILI was notable in five (four females) patients. The liver injury was hepatocellular and cholestatic in type, and two patients developed jaundice. In two patients, biopsy revealed extensive necrosis while in one, it was perivenular (zone III) in nature, with all showing severe lobular and portal-based mixed type of inflammation. The disease course was self-limiting with symptom resolution and improvement of liver dysfunction on follow-up[84]. In Figure 8 we illustrate the baseline and follow-up liver histopathology of a young woman who developed severe acute cholestatic hepatitis that progressed to chronic DILI and chronic liver disease at 6 mo follow-up, after consuming Indian valerian (Valeriana wallichi) root extract (Tagara®, The Himalaya Drug Company) for three to seven days. A summary of all discussed Ayurvedic herbs and their hepatotoxic details is shown in Table 1.
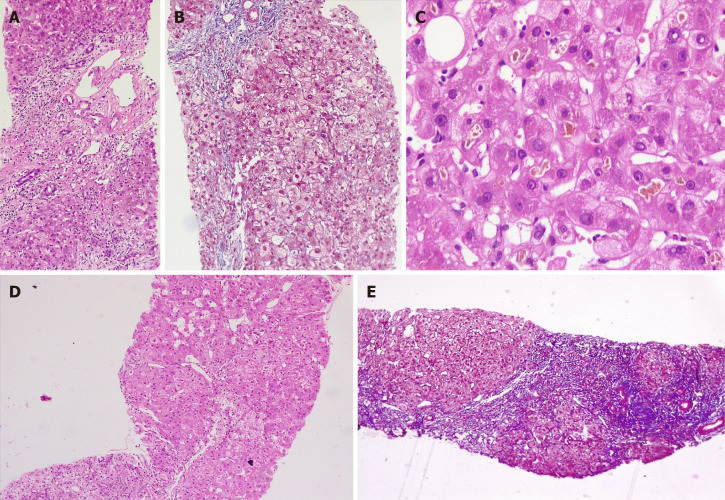
Figure 8.
Development of acute severe cholestatic hepatitis leading to chronic herb-induced liver injury resulting in cirrhosis in a young female, after ingestion of Valerian (Tagara®). Percutaneous liver biopsy performed in August 2019 (A-C) revealed portal and periportal necrosis with mixed lobular inflammation [A, hematoxylin and eosin (H&E) stain, 100 ×], pale blue staining in the regions of necrosis and hepatocyte loss is notable on Masson-trichrome staining (B, 200 ×); hepatocellular and canalicular cholestasis is notable (C, H&E, 400 ×); on follow-up, liver biopsy showed progression of fibrosis with vague hepatocyte nodule formation (D, H&E, 200 ×) with central to central and central to portal bridging fibrosis suggestive of cirrhosis and nodule formation on Masson-trichrome stain (E, 100 ×).
Table 1.
A summary of all Ayurvedic herbs implicated in liver injury with potential mechanisms of toxicity, liver injury pattern, histopathology patterns and clinical outcomes
| Ayurvedic herb | Author/study /country | Pattern of liver injury (hepatocellular, cholestatic or mixed type) | Liver biopsy features | Suspected potential toxic component (s) | Clinical outcomes and comments |
| Withania somnifera (Ashwagandha) | Inagaki et al[10]/report/Japan | Cholestatic type | Intrahepatic cholestasis, canalicular bile plugs | Unclassified triterpenoids | Resolved, survived |
| Björnsson et al[11]/series (n = 5)/Iceland and United States | Cholestatic and mixed type | Cholestatic hepatitis | Resolved, survived | ||
| Bacopa monnieri, Centella asiatica (Brahmi or Gotu-kola) | Teschke et al[14]/report/Germany | Hepatocellular type | Not performed | Saponin triterpenoids. phytoglycosides, autoantibody or immune-mediated | Resolved, survived. However, multiple other associated herbals used |
| Jorge et al[17]/series (n = 3)/Argentina | Mixed type | Granulomatous cholestatic hepatitis | One patient progressed to cirrhosis and acute decompensation on repeat herb intake; in another, complete resolution noted | ||
| Dantuluri et al[18]/report/United Kingdom | Hepatocellular type | Not performed | Acute liver failure, spontaneous resolution, survived | ||
| Curcuma longa (Turmeric) | Lukefahr et al[22]/ report/United States | Hepatocellular type | Autoimmune hepatitis | Immunomodulatory polyphenolic compounds, drug triggered autoantibodies related liver injury | Complete resolution |
| Suhail et al[23]/report/United States | Hepatocellular type | Acute panlobular hepatitis with early parenchymal collapse | Complete resolution in 3 wk | ||
| Lee et al[24]/report/United States | Hepatocellular type | Autoimmune hepatitis with additional eosinophilic and neutrophilic interface hepatitis | Complete resolution | ||
| Imam et al[25]/report/United States | Hepatocellular type | Not performed | Complete resolution | ||
| Luber et al[26]/two patient report/Australia | Mixed type in first case and hepatocellular type in second patient | Biopsy performed in first case showed mixed lobular inflammation and severe interface hepatitis; biopsy not performed in case two | Complete resolution in both patients, autoantibodies positive in second patient | ||
| Chand et al[27]/report/Australia | Hepatocellular type | Acute hepatitis with mixed inflammatory infiltrate of lobules and interface hepatitis with focal necrosis and mild cholestasis | Complete resolution, no autoantibodies noted, but high immunoglobulin G was remarkable | ||
| Guggul / Guggulipids (as part of polyherbal formulations and weight loss supplements) | Grieco et al[29]/report/Italy | Hepatocellular type | Necroinflammation with lobular eosinophilic inflammation | Guggul sterols associated herb-herb and herb-drug interaction; no direct hepatotoxicity described | Complete resolution |
| Yellapu et al[30]/report/United States | Hepatocellular type | Massive hepatic necrosis | Acute liver failure necessitating cadaveric liver transplantation | ||
| Polavarappu et al[31]/report/United States | Hepatocellular type | Not performed | Spontaneous resolution on drug withdrawal | ||
| Dalal et al[32]/report/United States | Hepatocellular type | Mixed portal inflammation, interface hepatitis, eosinophilic lobular inflammation with ceroid laden macrophages | Spontaneous resolution on drug withdrawal | ||
| Psoralea corylifolia (Bakuchi, Babchi seeds) | Nam et al[34]/report/South Korea | Mixed type | Zone 3 necrosis, cholestasis and severe mixed inflammatory infiltration of lobules | Terpenoids like bakuchiol and coumarinoids | Complete clinical resolution |
| Cheung et al[35]/series (n = 3)/ | Hepatocellular type | Not performed | All three patients had uneventful recovery after drug withdrawal | ||
| Smith et al[36]/report/United Kingdom | Hepatocellular type | Cholestatic acute hepatitis | Clinical resolution on drug withdrawal | ||
| Cassia angustifolio (Indian Senna) | Beuers et al[41]/report/Germany | Mixed type | Perivenular necrosis, lymphohistiocytic portal and lobular inflammation | Anthracoid sennoside and rhein anthron metabolites | Complete resolution, recurrence on rechallenge |
| Sonmez et al[42]/report/Turkey | Mixed type | Bridging hepatocellular necrosis and canalicular cholestasis | Complete resolution | ||
| Seybold et al[43]/report/Germany | Hepatocellular type | Not performed | Complete resolution | ||
| Vanderperren et al[44]/Belgium | Hepatocellular type | Not performed | High amounts of cadmium on toxicology evaluation | Acute liver failure with renal failure, resolved on aggressive supportive care | |
| Aloe vera | Rabe et al[52]/report/Germany | Cholestatic type | Portal and lobular lymphoplasmacytic inflammation, eosinophilic granulomas, bridging necrosis and bilirubinostasis | Aloe alkaloids, anthraquinones | Complete resolution on herbal drug withdrawal |
| Parlati et al[53]/report and review series (n = 9)/France | Hepatocellular type | All patients had portal and lobular inflammation with neutrophils and lymphoplasmacytes along with granulomas, acidophil bodies, ballooning of hepatocytes, extensive bridging necrosis and bilirubinostasis | All cases had clinical resolution of symptoms, no acute liver failure and no chronicity noted on follow up | ||
| Manso et al[56]/series on Herbalife® products/Spain | Hepatocellular type | Cholestatic hepatitis | Complete resolution after supplement withdrawal | ||
| Vázquez-Fernández et al[57]/report/Spain | Cholestatic type | Cholestatic hepatitis with lymphocyte predominant portal inflammation | Acute decompensation of cirrhosis (underlying HCV related infection); outcome not reported | ||
| Morinda citrifolia (Noni juice) | Millonig et al[59]/report/Austria | Hepatocellular type | Severe mixed inflammatory infiltration of portal tracts with lobular eosinophilic inflammation and hepatocellular cholestasis in zone 3 | Suspected noni anthraquinones | Complete resolution on herbal medicine withdrawal |
| Stadlbauer et al[60] / two cases report/Austria | Both cases hepatocellular type | First case, confluent necrosis, second case centrilobular necrosis and mild inflammatory infiltration in both | First patient progressed to acute liver failure and underwent successful liver transplantation; second patient had complete clinical recovery on conservative care | ||
| Yu et al[61]/report/United States | Hepatocellular type | Acute hepatitis with portal inflammation and periportal necrosis, hepatocellular cholestasis and numerous eosinophils in lobules | Paediatric case (14-year-old boy) with complete recovery on supportive care | ||
| Heliotropium sp., Trichodesma sp., Eupatorium sp., Senecia sp., Crotalaria sp. Chelidonium majus sp., Castilleja sp. Holarrhena antidysenterica | Neuman et al[66]/review series > 30 cases/Canada | Hepatocellular and mixed type | Early pathologic changes include the deposition of fibrinogen and factor VIII within the venular walls and liver sinusoids. In acute stage, haemorrhage into markedly dilated sinusoids with hepatocyte atrophy is noted, the sinusoids become denuded, parenchymal collapse is evident followed by the constriction and obliteration of small central veins by subendothelial swelling or fibrosis. The sinusoidal fibrosis and nodular regeneration may occur leading to cirrhosis and portal hypertension at later stages | Pyrrolizidine alkaloids | The acute form is rapidly fatal in 20% to 40% of patients. Adults have worse prognosis that the paediatric age group. Approximately 15% with acute disease will progress to subacute or chronic injury, and develop end-stage liver disease in a few years. |
| Garcinia cambogia (Malabar Tamarind) | Crescoli et al[71] and Kothadia et al[72]/case series review, n = 66/ | Hepatocellular type | Acute hepatitis with necroinflammation and parenchymal collapse is commonly noted on histopathology | Hydroxycitric acid and adulteration with heavy metals and other toxic ingredients | Commonly self-limiting even after a prolonged course; acute liver failure and acute on chronic liver failure leading to death described; in liver failure, transplantation has been performed to increase survival; chronic and prolonged DILI has been described leading to cirrhosis and portal hypertension |
| Gymnema sylvestre (Gurmar or sugar destroyer) | Shiyovich et al[74] and Dara et al[75]/series of patients including those consuming herbal and dietary supplements such as Hydroxycut® containing Gymnema | Mixed type | Necroinflammation of the lobules and portal regions with marked ductular proliferation and neutrophilic infiltration of the portal areas | Triterpene saponins, gymnemic acids and polyalkaloids | Usually self-limiting with complete resolution after herbal drug withdrawal |
| Tribulus Terrestis (Gokshura or Puncture vine) | Talasaz et al[77] and Ryan et al[78] /reports / Iran and United States respectively | Hepatocellular type | Not performed | Phylloerythrin and beta-carboline alkaloids are suspected toxins | Associated with seizures and acute kidney injury (mostly bile cast nephropathy); usually self-limiting and responsive to conservative care |
| Valeriana officinalis (Valerian) | MacGregor et al[81] series (n = 4) /Edinburgh | Hepatocellular type | Not performed | Suspected toxins include valerian alkaloids and sesquiterpenes | All patients had uneventful recovery after drug withdrawal and supportive care |
| Cohen et al[82]/report/United States | Cholestatic type | Not performed | |||
| Vassiliadis et al[83] /report/Greece | Hepatocellular type | Lymphocytic and eosinophilic portal inflammation with perivenular necrosis and small bile duct damage | |||
| Duoros et al[84]/series (n = 5)/Berlin | Hepatocellular and mixed type | Extensive necrosis, lobular and portal severe necroinflammation with neutrophils, lymphocytes and eosinophils |
HCV: Hepatitis C virus; DILI: Drug-induced liver injury.
CONCLUSION
Ayurvedic herb-related hepatotoxicity and liver injury can present as asymptomatic minor transaminase elevations, acute and chronic hepatitis, granulomatous hepatitis, asymptomatic to severe cholestasis, sinusoidal obstruction syndrome, acute liver failure requiring transplantation as well as progression to cirrhosis and portal hypertension. It is essential that physicians and specialists caring for patients with acute and chronic liver disease understand the small, but central role of herb-induced liver injury in a subset of patients who follow complementary and alternative medical practices and in whom an etiology of liver disease cannot be ascertained after extensive and conventional evaluation. The type of herb-induced liver injury and knowledge of its natural course is also important for treatment decisions and prognostication. Further studies that focus on the identification of beneficial and toxic components in Ayurvedic herbs, regulated curbing on the use of polyherbal formulations and educating the masses through public-industry partnerships, on the potential severe toxicity of certain herbs remain an unmet need.
Footnotes
Conflict-of-interest statement: Authors declare no conflict of interest for this article.
Manuscript source: Invited manuscript
Peer-review started: April 1, 2020
First decision: June 7, 2020
Article in press: August 15, 2020
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Nakano H S-Editor: Gong ZM L-Editor: Webster JR P-Editor: Wang LL
Contributor Information
Cyriac Abby Philips, The Liver Unit and Monarch Liver Lab, Cochin Gastroenterology Group, Ernakulam Medical Center, Kochi 682028, Kerala, India. abbyphilips@gmail.com.
Rizwan Ahamed, Gastroenterology and Advanced GI Endoscopy, Cochin Gastroenterology Group, Ernakulam Medical Center, Kochi 682028, Kerala, India.
Sasidharan Rajesh, Division of Hepatobiliary Interventional Radiology, Cochin Gastroenterology Group, Ernakulam Medical Center, Kochi 682028, Kerala, India.
Tom George, Division of Hepatobiliary Interventional Radiology, Cochin Gastroenterology Group, Ernakulam Medical Center, Kochi 682028, Kerala, India.
Meera Mohanan, Anesthesia and Critical Care, Cochin Gastroenterology Group, Ernakulam Medical Center, Kochi 682028, Kerala, India.
Philip Augustine, Gastroenterology and Advanced GI Endoscopy, Cochin Gastroenterology Group, Ernakulam Medical Center, Kochi 682028, Kerala, India.
References
- 1.Jaiswal YS, Williams LL. A glimpse of Ayurveda - The forgotten history and principles of Indian traditional medicine. J Tradit Complement Med. 2017;7:50–53. doi: 10.1016/j.jtcme.2016.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Das AK, Begum T, Kar P, Dutta A. Profile of Acute Liver Failure from North-east India and Its Differences from other Parts of the Country. Euroasian J Hepatogastroenterol. 2016;6:111–115. doi: 10.5005/jp-journals-10018-1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Udayakumar N, Subramaniam K, Umashankar L, Verghese J, Jayanthi V. Predictors of mortality in hepatic encephalopathy in acute and chronic liver disease: a preliminary observation. J Clin Gastroenterol. 2007;41:922–926. doi: 10.1097/01.mcg.0000225639.45157.ee. [DOI] [PubMed] [Google Scholar]
- 4.Devarbhavi H, Choudhury AK, Sharma MK, Maiwall R, Al Mahtab M, Rahman S, Chawla YK, Dhiman RK, Duseja A, Taneja S, Ning Q, Jia JD, Duan Z, Yu C, Eapen CE, Goel A, Tan SS, Hamid SS, Butt AS, Jafri W, Kim DJ, Hu J, Sood A, Midha V, Shukla A, Ghazinian H, Sahu MK, Treeprasertsuk S, Lee GH, Lim SG, Lesmana LA, Lesmana CR, Shah S, Kalal C, Abbas Z, Sollano JD, Prasad VGM, Payawal DA, Dokmeci AK, Rao PN, Shrestha A, Lau GK, Yuen MF, Saraswat VA, Shiha G, Yokosuka O, Kedarisetty CK, Jain P, Bhatia P, Sarin SK APASL ACLF working party. Drug-Induced Acute-on-Chronic Liver Failure in Asian Patients. Am J Gastroenterol. 2019;114:929–937. doi: 10.14309/ajg.0000000000000201. [DOI] [PubMed] [Google Scholar]
- 5.Philips CA, Paramaguru R, Joy AK, Antony KL, Augustine P. Clinical outcomes, histopathological patterns, and chemical analysis of Ayurveda and herbal medicine associated with severe liver injury-A single-center experience from southern India. Indian J Gastroenterol. 2018;37:9–17. doi: 10.1007/s12664-017-0815-8. [DOI] [PubMed] [Google Scholar]
- 6.Philips CA, Paramaguru R, Augustine P, Rajesh S, Ahamed R, George T, Padsalgi G. A Single-Center Experience on Outcomes of Complementary and Alternative Medicine Use Among Patients With Cirrhosis. Hepatol Commun. 2019;3:1001–1012. doi: 10.1002/hep4.1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patel SB, Rao NJ, Hingorani LL. Safety assessment of Withania somnifera extract standardized for Withaferin A: Acute and sub-acute toxicity study. J Ayurveda Integr Med. 2016;7:30–37. doi: 10.1016/j.jaim.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al-Awthan YS, Hezabr SM, Al-Zubairi AM, Al-Hemiri FA. Effects of aqueous extract of Withania somnifera on some liver biochemical and histopathological parameters in male guinea pigs. Pak J Biol Sci. 2014;17:504–510. doi: 10.3923/pjbs.2014.504.510. [DOI] [PubMed] [Google Scholar]
- 9.Dutta R, Khalil R, Green R, Mohapatra SS, Mohapatra S. Withania Somnifera (Ashwagandha) and Withaferin A: Potential in Integrative Oncology. Int J Mol Sci. 2019;20 doi: 10.3390/ijms20215310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Inagaki K, Mori N, Honda Y, Takaki S, Tsuji K, Chayama K. A case of drug-induced liver injury with prolonged severe intrahepatic cholestasis induced by Ashwagandha. Kanzo. 2017;58:448–454. [Google Scholar]
- 11.Björnsson HK, Björnsson ES, Avula B, Khan IA, Jonasson JG, Ghabril M, Hayashi PH, Navarro V. Ashwagandha-induced liver injury: A case series from Iceland and the US Drug-Induced Liver Injury Network. Liver Int. 2020;40:825–829. doi: 10.1111/liv.14393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chaudhari KS, Tiwari NR, Tiwari RR, Sharma RS. Neurocognitive Effect of Nootropic Drug Brahmi (Bacopa monnieri) in Alzheimer's Disease. Ann Neurosci. 2017;24:111–122. doi: 10.1159/000475900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gohil KJ, Patel JA, Gajjar AK. Pharmacological Review on Centella asiatica: A Potential Herbal Cure-all. Indian J Pharm Sci. 2010;72:546–556. doi: 10.4103/0250-474X.78519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Teschke R, Bahre R. Severe hepatotoxicity by Indian Ayurvedic herbal products: a structured causality assessment. Ann Hepatol. 2009;8:258–266. [PubMed] [Google Scholar]
- 15.Gonzalo Garijo MA, Revenga Arranz F, Bobadilla González P. Allergic contact dermatitis due to Centella asiatica: a new case. Allergol Immunopathol (Madr) 1996;24:132–134. [PubMed] [Google Scholar]
- 16.Dutta T, Basu UP. Crude extract of Centella asiatica and products derived from its glycosides as oral antifertility agents. Indian J Exp Biol. 1968;6:181–182. [PubMed] [Google Scholar]
- 17.Jorge OA, Jorge AD. Hepatotoxicity associated with the ingestion of Centella asiatica. Rev Esp Enferm Dig. 2005;97:115–124. doi: 10.4321/s1130-01082005000200006. [DOI] [PubMed] [Google Scholar]
- 18.Dantuluri S, North-Lewis P, Karthik SV. Gotu Kola induced hepatotoxicity in a child - need for caution with alternative remedies. Dig Liver Dis. 2011;43:500. doi: 10.1016/j.dld.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 19.Dosoky NS, Setzer WN. Chemical Composition and Biological Activities of Essential Oils of Curcuma Species. Nutrients. 2018;10 doi: 10.3390/nu10091196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kotha RR, Luthria DL. Curcumin: Biological, Pharmaceutical, Nutraceutical, and Analytical Aspects. Molecules. 2019;24 doi: 10.3390/molecules24162930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amalraj A, Pius A, Gopi S, Gopi S. Biological activities of curcuminoids, other biomolecules from turmeric and their derivatives - A review. J Tradit Complement Med. 2017;7:205–233. doi: 10.1016/j.jtcme.2016.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lukefahr AL, McEvoy S, Alfafara C, Funk JL. Drug-induced autoimmune hepatitis associated with turmeric dietary supplement use. BMJ Case Rep. 2018;2018 doi: 10.1136/bcr-2018-224611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suhail FK, Masood U, Sharma A, John S, Dhamoon A. Turmeric supplement induced hepatotoxicity: a rare complication of a poorly regulated substance. Clin Toxicol (Phila) 2020;58:216–217. doi: 10.1080/15563650.2019.1632882. [DOI] [PubMed] [Google Scholar]
- 24.Lee BS, Bhatia T, Charles TC, Wen R, Taira MT, Lim BS. Autoimmune hepatitis associated with turmeric consumption. ACG Case Rep J. 2020;7:e00320. doi: 10.14309/crj.0000000000000320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Imam Z, Khasawneh M, Jomaa D, Iftikhar H, Sayedahmad Z. Drug Induced Liver Injury Attributed to a Curcumin Supplement. Case Rep Gastrointest Med. 2019;2019:6029403. doi: 10.1155/2019/6029403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luber RP, Rentsch C, Lontos S, Pope JD, Aung AK, Schneider HG, Kemp W, Roberts SK, Majeed A. Turmeric induced liver injury: A report of two cases. Case Reports Hepatol. 2019;2019:6741213. doi: 10.1155/2019/6741213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chand S, Hair C, Beswick L. A rare case of turmeric-induced hepatotoxicity. Intern Med J. 2020;50:258–259. doi: 10.1111/imj.14727. [DOI] [PubMed] [Google Scholar]
- 28.Kunnumakkara AB, Banik K, Bordoloi D, Harsha C, Sailo BL, Padmavathi G, Roy NK, Gupta SC, Aggarwal BB. Googling the Guggul (Commiphora and Boswellia) for Prevention of Chronic Diseases. Front Pharmacol. 2018;9:686. doi: 10.3389/fphar.2018.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grieco A, Miele L, Pompili M, Biolato M, Vecchio FM, Grattagliano I, Gasbarrini G. Acute hepatitis caused by a natural lipid-lowering product: when "alternative" medicine is no "alternative" at all. J Hepatol. 2009;50:1273–1277. doi: 10.1016/j.jhep.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 30.Yellapu RK, Mittal V, Grewal P, Fiel M, Schiano T. Acute liver failure caused by 'fat burners' and dietary supplements: a case report and literature review. Can J Gastroenterol. 2011;25:157–160. doi: 10.1155/2011/174978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Polavarapu AD, Daoud M, Philipose J, Deeb L. Fat burner causing liver injury [Abstract] Am J Gastro. 2017;112:S1571. [Google Scholar]
- 32.Dalal KK, Holdbrook T, Peikin SR. Ayurvedic drug induced liver injury. World J Hepatol. 2017;9:1205–1209. doi: 10.4254/wjh.v9.i31.1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khushboo PS, Jadhav VM, Kadam VJ, Sathe NS. Psoralea corylifolia Linn.-"Kushtanashini". Pharmacogn Rev. 2010;4:69–76. doi: 10.4103/0973-7847.65331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nam SW, Baek JT, Lee DS, Kang SB, Ahn BM, Chung KW. A case of acute cholestatic hepatitis associated with the seeds of Psoralea corylifolia (Boh-Gol-Zhee) Clin Toxicol (Phila) 2005;43:589–591. doi: 10.1081/clt-200068863. [DOI] [PubMed] [Google Scholar]
- 35.Cheung WI, Tse ML, Ngan T, Lin J, Lee WK, Poon WT, Mak TW, Leung VK, Chau TN. Liver injury associated with the use of Fructus Psoraleae (Bol-gol-zhee or Bu-gu-zhi) and its related proprietary medicine. Clin Toxicol (Phila) 2009;47:683–685. doi: 10.1080/15563650903059136. [DOI] [PubMed] [Google Scholar]
- 36.Smith DA, MacDonald S. A rare case of acute hepatitis induced by use of Babchi seeds as an Ayurvedic remedy for vitiligo. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2013-200958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhou W, Chen X, Zhao G, Xu D, Jiang Z, Zhang L, Wang T. Psoralen Induced Liver Injury by Attenuating Liver Regenerative Capability. Front Pharmacol. 2018;9:1179. doi: 10.3389/fphar.2018.01179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li ZJ, Abulizi A, Zhao GL, Wang T, Zhou F, Jiang ZZ, Aibai S, Zhang LY. Bakuchiol Contributes to the Hepatotoxicity of Psoralea corylifolia in Rats. Phytother Res. 2017;31:1265–1272. doi: 10.1002/ptr.5851. [DOI] [PubMed] [Google Scholar]
- 39.Yang L, Yu YL, Cheng LY, Zhang PY, Zhang Y, Zhou K. The accumulation of psoralen contributes to its hepatotoxicity revealed by pharmacokinetic and toxicokinetic study after repeated administration. ACS Omega. 2020;5:7307–7315. doi: 10.1021/acsomega.9b04153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Franz G. The senna drug and its chemistry. Pharmacology. 1993;47 Suppl 1:2–6. doi: 10.1159/000139654. [DOI] [PubMed] [Google Scholar]
- 41.Beuers U, Spengler U, Pape GR. Hepatitis after chronic abuse of senna. Lancet. 1991;337:372–373. doi: 10.1016/0140-6736(91)91012-j. [DOI] [PubMed] [Google Scholar]
- 42.Sonmez A, Yilmaz MI, Mas R, Ozcan A, Celasun B, Dogru T, Taslipinar A, Kocar IH. Subacute cholestatic hepatitis likely related to the use of senna for chronic constipation. Acta Gastroenterol Belg. 2005;68:385–387. [PubMed] [Google Scholar]
- 43.Seybold U, Landauer N, Hillebrand S, Goebel FD. Senna-induced hepatitis in a poor metabolizer. Ann Intern Med. 2004;141:650–651. doi: 10.7326/0003-4819-141-8-200410190-00024. [DOI] [PubMed] [Google Scholar]
- 44.Vanderperren B, Rizzo M, Angenot L, Haufroid V, Jadoul M, Hantson P. Acute liver failure with renal impairment related to the abuse of senna anthraquinone glycosides. Ann Pharmacother. 2005;39:1353–1357. doi: 10.1345/aph.1E670. [DOI] [PubMed] [Google Scholar]
- 45.Saper RB, Phillips RS, Sehgal A, Khouri N, Davis RB, Paquin J, Thuppil V, Kales SN. Lead, mercury, and arsenic in US- and Indian-manufactured Ayurvedic medicines sold via the Internet. JAMA. 2008;300:915–923. doi: 10.1001/jama.300.8.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Goyer RA. Mechanisms of lead and cadmium nephrotoxicity. Toxicol Lett. 1989;46:153–162. doi: 10.1016/0378-4274(89)90124-0. [DOI] [PubMed] [Google Scholar]
- 47.Vashishtha VM, Kumar A, John TJ, Nayak NC. Cassia occidentalis poisoning as the probable cause of hepatomyoencephalopathy in children in western Uttar Pradesh. Indian J Med Res. 2007;125:756–762. [PubMed] [Google Scholar]
- 48.Vashishtha VM, Kumar A, John TJ, Nayak NC. Cassia occidentalis poisoning causes fatal coma in children in western Uttar Pradesh. Indian Pediatr. 2007;44:522–525. [PubMed] [Google Scholar]
- 49.Ish P, Rathi S, Singh H, Anuradha S. Senna Occidentalis Poisoning: An Uncommon Cause of Liver Failure. ACG Case Rep J. 2019;6:e00035. doi: 10.14309/crj.0000000000000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Soyuncu S, Cete Y, Nokay AE. Portal vein thrombosis related to Cassia angustifolia. Clin Toxicol (Phila) 2008;46:774–777. doi: 10.1080/15563650701682097. [DOI] [PubMed] [Google Scholar]
- 51.Surjushe A, Vasani R, Saple DG. Aloe vera: a short review. Indian J Dermatol. 2008;53:163–166. doi: 10.4103/0019-5154.44785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rabe C, Musch A, Schirmacher P, Kruis W, Hoffmann R. Acute hepatitis induced by an Aloe vera preparation: a case report. World J Gastroenterol. 2005;11:303–304. doi: 10.3748/wjg.v11.i2.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Belfrage B, Malmström R. [Several cases of liver affected by aloe vera] Lakartidningen. 2008;105:45. [PubMed] [Google Scholar]
- 54.Parlati L, Voican CS, Perlemuter K, Perlemuter G. Aloe vera-induced acute liver injury: A case report and literature review. Clin Res Hepatol Gastroenterol. 2017;41:e39–e42. doi: 10.1016/j.clinre.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 55.Guo X, Mei N. Aloe vera: A review of toxicity and adverse clinical effects. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 2016;34:77–96. doi: 10.1080/10590501.2016.1166826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Manso G, López-Rivas L, Duque JM, Salgueiro E. Spanish reports of hepatotoxicity associated with Herbalife products. J Hepatol. 2008;49:289–90; author reply 290-1. doi: 10.1016/j.jhep.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 57.Vázquez-Fernández P, Garayoa-Roca A, Añón-Rodríguez R, Cabezas-Macián M, Serra-Desfilis MÁ, Mora-Miguel F. Aloe vera: Not always so beneficial in patients with chronic liver disease. Rev Esp Enferm Dig. 2013;105:434–435. doi: 10.4321/s1130-01082013000700012. [DOI] [PubMed] [Google Scholar]
- 58.Philips RL. Cavernous transformation of the portal vein. Australas Radiol. 1988;32:239–241. doi: 10.1111/j.1440-1673.1988.tb02729.x. [DOI] [PubMed] [Google Scholar]
- 59.Millonig G, Stadlmann S, Vogel W. Herbal hepatotoxicity: acute hepatitis caused by a Noni preparation (Morinda citrifolia) Eur J Gastroenterol Hepatol. 2005;17:445–447. doi: 10.1097/00042737-200504000-00009. [DOI] [PubMed] [Google Scholar]
- 60.Stadlbauer V, Fickert P, Lackner C, Schmerlaib J, Krisper P, Trauner M, Stauber RE. Hepatotoxicity of NONI juice: report of two cases. World J Gastroenterol. 2005;11:4758–4760. doi: 10.3748/wjg.v11.i30.4758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yu EL, Sivagnanam M, Ellis L, Huang JS. Acute hepatotoxicity after ingestion of Morinda citrifolia (Noni Berry) juice in a 14-year-old boy. J Pediatr Gastroenterol Nutr. 2011;52:222–224. doi: 10.1097/MPG.0b013e3181eb69f0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.West BJ, Jensen CJ, Westendorf J. Noni juice is not hepatotoxic. World J Gastroenterol. 2006;12:3616–3619. doi: 10.3748/wjg.v12.i22.3616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hawaiian Organic Noni, LLC. Warning letter. Retrieved on 30-03-2020. Available from: https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/warning-letters/hawaiian-organic-noni-llc-540887-07182018. [Google Scholar]
- 64.Wiedenfeld H. Plants containing pyrrolizidine alkaloids: toxicity and problems. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2011;28:282–292. doi: 10.1080/19440049.2010.541288. [DOI] [PubMed] [Google Scholar]
- 65.Moreira R, Pereira DM, Valentão P, Andrade PB. Pyrrolizidine Alkaloids: Chemistry, Pharmacology, Toxicology and Food Safety. Int J Mol Sci. 2018;19 doi: 10.3390/ijms19061668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Neuman MG, Cohen L, Opris M, Nanau RM, Hyunjin J. Hepatotoxicity of Pyrrolizidine Alkaloids. J Pharm Pharm Sci. 2015;18:825–843. doi: 10.18433/j3bg7j. [DOI] [PubMed] [Google Scholar]
- 67.Arseculeratne SN, Gunatilaka AA, Panabokke RG. Studies on medicinal plants of Sri Lanka: occurrence of pyrrolizidine alkaloids and hepatotoxic properties in some traditional medicinal herbs. J Ethnopharmacol. 1981;4:159–177. doi: 10.1016/0378-8741(81)90033-7. [DOI] [PubMed] [Google Scholar]
- 68.Semwal RB, Semwal DK, Vermaak I, Viljoen A. A comprehensive scientific overview of Garcinia cambogia. Fitoterapia. 2015;102:134–148. doi: 10.1016/j.fitote.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 69.Heymsfield SB, Allison DB, Vasselli JR, Pietrobelli A, Greenfield D, Nunez C. Garcinia cambogia (hydroxycitric acid) as a potential antiobesity agent: a randomized controlled trial. JAMA. 1998;280:1596–1600. doi: 10.1001/jama.280.18.1596. [DOI] [PubMed] [Google Scholar]
- 70.Onakpoya I, Hung SK, Perry R, Wider B, Ernst E. The Use of Garcinia Extract (Hydroxycitric Acid) as a Weight loss Supplement: A Systematic Review and Meta-Analysis of Randomised Clinical Trials. J Obes. 2011;2011:509038. doi: 10.1155/2011/509038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Crescioli G, Lombardi N, Bettiol A, Marconi E, Risaliti F, Bertoni M, Menniti Ippolito F, Maggini V, Gallo E, Firenzuoli F, Vannacci A. Acute liver injury following Garcinia cambogia weight-loss supplementation: case series and literature review. Intern Emerg Med. 2018;13:857–872. doi: 10.1007/s11739-018-1880-4. [DOI] [PubMed] [Google Scholar]
- 72.Kothadia JP, Kaminski M, Samant H, Olivera-Martinez M. Hepatotoxicity Associated with Use of the Weight Loss Supplement Garcinia cambogia: A Case Report and Review of the Literature. Case Reports Hepatol. 2018;2018:6483605. doi: 10.1155/2018/6483605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Philips CA, Augustine P. Chemical Analysis of Weight Loss Herbal Supplement Safe Lean™ Associated With Acute Liver Injury - A Concern for Spurious Drug, Misbranding and Adulteration. J Clin Exp Hepatol. 2018;8:471–473. doi: 10.1016/j.jceh.2018.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shiyovich A, Sztarkier I, Nesher L. Toxic hepatitis induced by Gymnema sylvestre, a natural remedy for type 2 diabetes mellitus. Am J Med Sci. 2010;340:514–517. doi: 10.1097/MAJ.0b013e3181f41168. [DOI] [PubMed] [Google Scholar]
- 75.Dara L, Hewett J, Lim JK. Hydroxycut hepatotoxicity: a case series and review of liver toxicity from herbal weight loss supplements. World J Gastroenterol. 2008;14:6999–7004. doi: 10.3748/wjg.14.6999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Semerdjieva IB, Zheljazkov VD. Chemical constituents, biological properties, and uses of Tribulus terrestris: A review. Nat Prod Commun. 2019;14:8. [Google Scholar]
- 77.Talasaz AH, Abbasi MR, Abkhiz S, Dashti-Khavidaki S. Tribulus terrestris-induced severe nephrotoxicity in a young healthy male. Nephrol Dial Transplant. 2010;25:3792–3793. doi: 10.1093/ndt/gfq457. [DOI] [PubMed] [Google Scholar]
- 78.Ryan M, Lazar I, Nadasdy GM, Nadasdy T, Satoskar AA. Acute kidney injury and hyperbilirubinemia in a young male after ingestion of Tribulus terrestris. Clin Nephrol. 2015;83:177–183. doi: 10.5414/CN108324. [DOI] [PubMed] [Google Scholar]
- 79.Willey LB, Mady SP, Cobaugh DJ, Wax PM. Valerian overdose: a case report. Vet Hum Toxicol. 1995;37:364–365. [PubMed] [Google Scholar]
- 80.Bent S, Padula A, Moore D, Patterson M, Mehling W. Valerian for sleep: a systematic review and meta-analysis. Am J Med. 2006;119:1005–1012. doi: 10.1016/j.amjmed.2006.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.MacGregor FB, Abernethy VE, Dahabra S, Cobden I, Hayes PC. Hepatotoxicity of herbal remedies. BMJ. 1989;299:1156–1157. doi: 10.1136/bmj.299.6708.1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cohen DL, Del Toro Y. A case of valerian-associated hepatotoxicity. J Clin Gastroenterol. 2008;42:961–962. doi: 10.1097/MCG.0b013e3180500348. [DOI] [PubMed] [Google Scholar]
- 83.Vassiliadis T, Anagnostis P, Patsiaoura K, Giouleme O, Katsinelos P, Mpoumponaris A, Eugenidis N. Valeriana hepatotoxicity. Sleep Med. 2009;10:935. doi: 10.1016/j.sleep.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 84.Douros A, Bronder E, Andersohn F, Klimpel A, Kreutz R, Garbe E, Bolbrinker J. Herb-Induced Liver Injury in the Berlin Case-Control Surveillance Study. Int J Mol Sci. 2016;17:114. doi: 10.3390/ijms17010114. [DOI] [PMC free article] [PubMed] [Google Scholar]