Abstract
Although several typical manifestation of novel coronavirus disease 2019 (COVID-19) including respiratory symptoms, weakness, fever, and fatigue have been reported, some rare and novel manifestations have also been observed, particularly in children. We report a pediatric case of fulminant hepatic failure associated with COVID-19. Although the patient was treated for acute fulminant hepatic failure in the context of COVID-19, he died following the progression of the disease to stage 4 hepatic failure with encephalopathy and brain death.
Keywords: SARS-COV-2, Novel coronavirus disease 2019, Fulminant hepatic failure, Transplant
1. Introduction
In December 2019, novel coronavirus disease 2019 (COVID-19) caused by a novel coronavirus, SARS-COV-2, emerged in Wuhan, China, and since then has spread around the world. Although at the start of the outbreak it was thought that children were less likely to be infected with COVID-19, over times the number of reports on pediatric patients increased [1], [2], [3]. There are three main categories of SARS-CoV-2 infection including asymptomatic, non-severe symptomatic, as well as severe respiratory and systemic presentations [4], and the incidence of symptomatic infection and critical disease in children is known to be lower than that of adults [3], [5]. The typical manifestations of COVID-19 that have been reported include respiratory symptoms, weakness, fever, and fatigue; however, rare and novel manifestations are also seen, particularly in children [6]. In this study, we report a pediatric case with fulminant hepatic failure associated with COVID-19.
2. Case presentation
The patient, an 11-year-old boy, presented to the emergency department for fever, icterus, and abdominal pain that had started 7 days earlier. He had no past medical history of chronic liver disease or of using potentially hepatotoxic drugs or of food poisoning. None of his family members had symptoms of COVID-19 or of hepatic diseases. On admission, he was icteric, dyspneic, and with a decreased level of consciousness. He had been fully alert and responsive 1 week before admission, but severe fatigue, confusional state, and decreased level of consciousness had gradually developed. He had spent 1 month in quarantine owing to the COVID-19 outbreak; however, approximately 10 days before admission, he visited a ranch and a few hours later had fever, chills, and malaise. After 1–2 days, icterus appeared primarily in the eyes and subsequently spread to the rest of the body. There were no complaints of coughing, sneezing, symptoms of upper respiratory tract infection, vomiting, and diarrhea. Unfortunately, due to a lack of resources, he had not been visited by any physician. After 7 days of illness, he was admitted to a general hospital with the primary diagnosis of hepatitis that led to the diagnosis of fulminant hepatic failure after initial evaluation. He was then transferred to our hospital, an Iranian pediatric referral hospital, for liver transplantation. The laboratory findings are shown in Table 1 . At the original hospital the stage of disease progression was 2 and at our center it progressed to stage 3 or 4. Upon admission to our emergency room, the score on the Glasgow Coma Scale (GCS) was 7–8 and he had active gastrointestinal and nasal bleeding. Thus, immediately after arrival, our decision was to intubate the patient and immediately transfer him to the intensive care unit (ICU) where he underwent mechanical ventilation.
Table 1.
Laboratory results during 5-day hospital stay.
| Parameter | Day in hospital |
Normal range | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 2 | 3 | 3 | 4 | 4 | 5 | ||
| White blood cell count (× 109 cells/L) | 20.5 | 17.41 | 14.59 | 15.07 | – | 7.19 | – | 20.86 | 4–10 |
| Neutrophil count (× 109 cells/L) | 66 | 53.4 | 66 | 78 | – | 84 | – | 86 | 2–7 |
| Lymphocyte count (× 109/L) | 23.5 | 36.1 | 22.7 | 13 | – | 11.7 | – | 8.6 | 0.8–4 |
| Hemoglobin (g/dL) | 11.8 | 10 | 7.2 | 10.4 | – | 7.8 | – | 11.5 | 11–16 |
| Platelet count (× 109 cells/L) | 285 | 276 | 256 | 88 | – | 65 | – | 81 | 150–450 |
| Alanine aminotransferase (U/L) | 1038 | – | – | – | – | – | – | – | 10–40 |
| Aspartate aminotransferase (U/L) | 1260 | – | – | – | – | – | – | – | 10–40 |
| Alkaline phosphatase (U/L) | 662 | – | – | – | – | – | – | – | 180–1200 |
| Albumin (g/dL) | 3.7 | – | – | 3.6 | – | – | – | – | 3.5–5.2 |
| Gamma-glutamyl transferase (IU/L) | 30 | – | – | – | – | – | – | – | 4–50 |
| Bilirubin total (mg/dL) | 19.2 | – | – | – | – | – | – | – | 0.1–1.2 |
| Bilirubin direct (mg/dL) | 16 | – | – | – | – | – | – | – | 0.1–0.4 |
| C-reactive protein (mg/L) | 29 | – | – | – | – | – | – | – | <6 |
| Ammonia (μmol/L) | 186 | 230 | 209 | 252 | 235 | 672 | 490 | – | 16–60 |
| Lactate (mg/dL) | 56 | 39 | 51 | 46 | 70 | 87 | 105 | – | 2–20 |
| Creatine phosphokinase (U/L) | – | – | – | 902 | – | – | – | – | 24–195 |
| D-dimers (pg/mL) | – | – | – | <0.2 | – | – | – | – | <0.5 |
| Troponin (ng/mL) | – | – | – | 1 | – | – | – | – | 0–0.3 |
| Lactate dehydrogenase (U/L) | – | 1670 | – | – | – | – | – | – | 5–746 |
| Ferritin (ng/mL) | – | 2940 | – | – | – | – | – | – | 30–220 |
| Fibrinogen (mg/dL) | – | 160 | – | – | – | – | – | – | 150–350 |
| Prothrombin time (seconds) | 29.4 | – | – | 20.9 | – | – | 24.1 | 38.1 | 11–13.5 |
| International normalized ratio (INR) | 3.8 | – | – | 2.24 | – | – | 2.78 | 5.7 | |
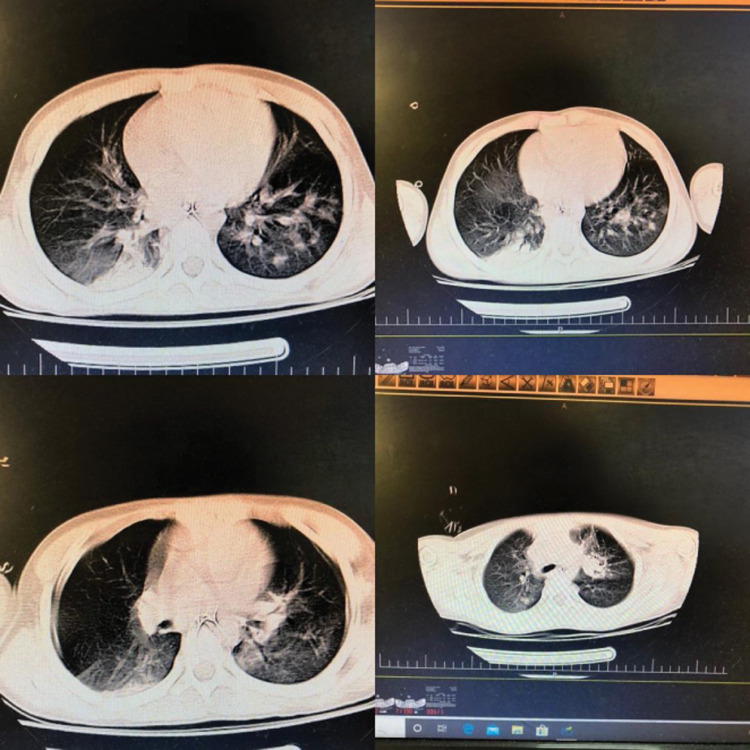
Computerized tomography (CT) showed patchy areas of consolidation in both lungs. On chest X-rays (CXR), there was mild bilateral pleural effusion with bilateral paracardiac ground glass opacity and alveolar opacity in the upper zone of left lung (Fig. 1, Fig. 2 ). A pharyngeal swab sample was collected for COVID-19 real-time reverse transcriptase polymerase chain reaction (RT-PCR) as part of a pretransplantation protocol. Unfortunately, the result of the SARS-COV-2 RT-PCR was positive, which was very surprising because the SARS-COV-2 RT-PCR result at the previous hospital was negative.
Fig. 1.
Computed tomography (CT) scan showing patchy areas of consolidation in both lungs. Mediastinal lymph node is mildly prominent.
Fig. 2.
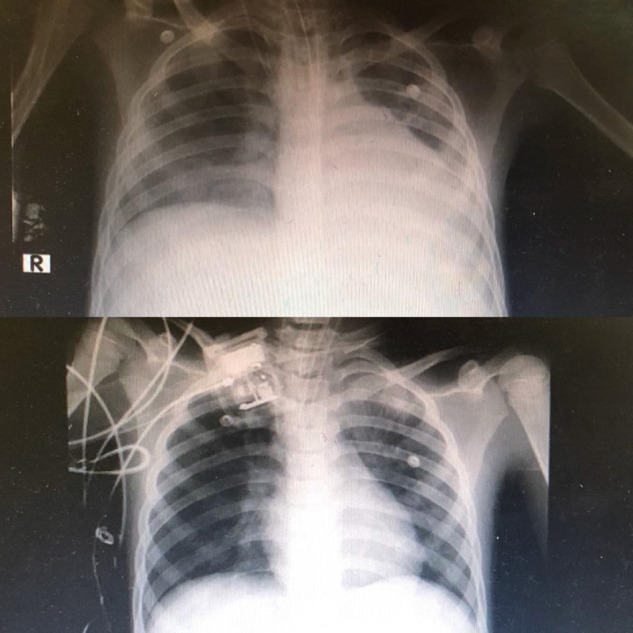
Chest X-ray (CXR) showing bilateral paracardiac ground glass opacity with alveolar opacity in upper zone of left lung and right paracardiac region with mild bilateral pleural effusion.
In addition, to rule out other probable causes of fulminant hepatitis, tests for other viruses including hepatitis A, hepatitis B, herpes virus, Epstein–Barr virus, cytomegalovirus were performed, with all results being negative. Moreover, to rule out metabolic disease, additional tests were run, including amino acid chromatography, organic acid chromatography, and measurement of succinylacetone in urine, all of which yielded negative results.
Treatment for COVID-19 was initiated with hydroxychloroquine and Kaletra, and we also prescribed vancomycin and ceftazidime for other probable bacterial infections. In the ICU, the patient's GCS was 4–5 and decreased further on the following day. Owing to unstable hemodynamics, we added norepinephrine and epinephrine but the patient's condition progressed to hepatorenal syndrome and he underwent dialysis. Unfortunately, after 2–3 days he died in spite of all the medical and supportive measures.
3. Discussion
In this study, we report a novel pediatric case of fulminant hepatic failure associated with COVID-19.
Although there have been a significantly smaller number of reported cases of COVID-19 in the pediatric population compared with the adults, the number of infected children has seen a moderate increase [2], [7]. Children with COVID-19 infection may be asymptomatic or have fever, dry cough, and fatigue with a few upper respiratory symptoms including nasal congestion and runny nose; other patients might show gastrointestinal symptoms including abdominal discomfort, nausea, vomiting, abdominal pain, and diarrhea [2], [8], [9]. In addition to the typical manifestation, rare and novel symptoms have also been seen, particularly in children such as our patient. Fulminant hepatic failure is considered the fourth main cause of liver transplantation in children, preceded by extrahepatic cholestatic liver diseases, intrahepatic cholestasis, and metabolic diseases followed by primary liver tumor and cystic fibrosis [10]. Acute liver failure is a life-threatening condition with sudden onset of liver injury, decreased liver function, hepatic encephalopathy, and coagulopathy in patients without preexisting liver disease. However, etiologic factors might change depending on geographic variation, age, and socioeconomic status. Viral agents and drugs mostly cause acute liver failure, but sometimes no etiologic factor can be found. However, viral infections are the most common reasons [7]. Because of the unusual manifestation of COVID-19 in children, it should be ruled out as the cause of acute liver failure. The incidence of hepatic abnormalities significantly increases after infection with SARS-COV-2 and during the course of the disease [11]. Elevated liver biochemistry profiles may reflect a direct virus-induced cytopathic effect and/or immune damage from the provoked inflammatory response [12]. In addition, SARS-CoV-2 infection might induce rhabdomyolysis with an initial increase in creatinine kinase level [13]. Increasing evidence has demonstrated the frequent incidence of liver injury in COVID-19, especially in patients with multiple organ injury. Liver injury itself often manifests as transient elevation in serum aminotransferases. However, acute liver failure and intrahepatic cholestasis have been reported [14]. Liver damage in patients with coronavirus infections might be directly caused by the viral infection of liver cells. Patients with severe COVID-19 seem to have higher rates of liver dysfunction [15]. Hepatic dysfunction in severe COVID-19 is accompanied by a greater activation of the coagulative and fibrinolytic pathways, relatively lower platelet counts, rising neutrophil counts and neutrophil-to-lymphocyte ratios, and high ferritin levels [16].
In fulminant hepatic failure, hepatic transplantation is the only therapy that has been proven to improve survival in the majority of patients, despite specific therapeutic options for distinct orthotopic etiologies. The result is determined by complications such as severe coagulopathy, infection, renal dysfunction, or increased intracranial pressure. The decision regarding transplantation depends on the probability of spontaneous hepatic recovery, which can be determined by multiple factors. The most important variables for predicting the need for transplantation during fulminant hepatic failure include the degree of encephalopathy, the age of the patient, and the underlying cause of hepatic failure [17]. Owing to the acute fulminant hepatic failure in our patient, the only treatment option was liver transplantation; however, because of the progressive course of the disease and its rapid progression to stage 4 with encephalopathy and brain death, he died.
4. Conclusion
In conclusion, in patients with fulminant hepatic failure, especially in cases with symptoms including fever, respiratory distress, and diarrhea, we should rule out COVID-19 infection as the underlying cause. The need for emergency liver transplantation in fulminant hepatic failure due to COVID-19 and the indications for transplantation should be further evaluated.
Disclosure of interest
The authors declare that they have no competing interest.
References
- 1.Xia W., Shao J., Guo Y. Clinical and CT features in pediatric patients with COVID-19 infection: different points from adults. Pediatr Pulmonol. 2020;55:1169–1174. doi: 10.1002/ppul.24718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mahmoudi S., Mehdizadeh M., Badv R.S. The coronavirus disease 2019 (COVID-19) in children: a study in an Iranian children's referral hospital. Infect Drug Resist. 2020;13:2649–2655. doi: 10.2147/IDR.S259064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.She J., Liu L., Liu W. COVID-19 epidemic: disease characteristics in children. J Med Virol. 2020;92:747–754. doi: 10.1002/jmv.25807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mahmoudi S., Rezaei M., Mansouri N. Immunologic features in coronavirus disease 2019: functional exhaustion of T cells and cytokine storm. J Clin Immunol. 2020:1–3. doi: 10.1007/s10875-020-00824-4. [Online ahead of print. Article in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oualha M., Bendavid M., Berteloot L. Severe and fatal forms of COVID-19 in children. Arch Pediatr. 2020;27:235–238. doi: 10.1016/j.arcped.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ekbatani M.S., Hassani S.A., Tahernia L. Atypical and novel presentations of coronavirus disease 2019: a case series of three children. Br J Biomed Sci. 2020:1–6. doi: 10.1080/09674845.2020.1785102. [Online ahead of print. Article in press] [DOI] [PubMed] [Google Scholar]
- 7.Kirnap M., Akdur A., Ozcay F. Liver transplant for fulminant hepatic failure: a single-center experience. Exp Clin Transplant. 2015;13:339–343. doi: 10.6002/ect.2015.0080. [DOI] [PubMed] [Google Scholar]
- 8.Ludvigsson J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatrica. 2020;109:1088–1095. doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mamishi S., Heydari H., Aziz-Ahari A. Novel coronavirus disease 2019 (COVID-19) outbreak in children in Iran: atypical CT manifestations and mortality risk of severe COVID-19 infection. J Microbiol Immunol Infect. 2020 doi: 10.1016/j.jmii.2020.07.019. [S1684-1182(20)30177-8. Online ahead of print. Article in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spada M., Riva S., Maggiore G. Pediatric liver transplantation. World J Gastroenterol. 2009;15:648–674. doi: 10.3748/wjg.15.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rismanbaf A., Zarei S. Liver and kidney injuries in COVID-19 and their effects on drug therapy; a letter to editor. Arch Acad Emerg Med. 2020;8:e17. [PMC free article] [PubMed] [Google Scholar]
- 12.Diseases AAftSoL . American association for the study of liver diseases; 2020. Clinical insights for hepatology and liver transplant providers during the COVID-19 pandemic. WWW.AASLD.ORG. [Google Scholar]
- 13.Chan K.H., Farouji I., Abu Hanoud A. Weakness and elevated creatinine kinase as the initial presentation of coronavirus disease 2019 (COVID-19) J Emerg Med. 2020;38 doi: 10.1016/j.ajem.2020.05.015. [1548.e1–1548.e3] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Henry B.M., Lippi G., Plebani M. Laboratory abnormalities in children with novel coronavirus disease 2019. Clin Chem Lab Med. 2020;58:1135–1138. doi: 10.1515/cclm-2020-0272. [DOI] [PubMed] [Google Scholar]
- 15.Zhang C., Shi L., Wang F.S. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020;5:428–430. doi: 10.1016/S2468-1253(20)30057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bangash M.N., Patel J., Parekh D. COVID-19 and the liver: little cause for concern. Lancet Gastroenterol Hepatol. 2020;5:529–530. doi: 10.1016/S2468-1253(20)30084-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gotthardt D., Riediger C., Weiss K.H. Fulminant hepatic failure: etiology and indications for liver transplantation. Nephrol Dial Transplant. 2007;22(Suppl 8):viii5–viii8. doi: 10.1093/ndt/gfm650. [DOI] [PubMed] [Google Scholar]