Abstract
Immune checkpoint inhibitor (ICI) therapy provides a valuable treatment option for many cancer patients but is associated with immune-related adverse events (irAEs) that can involve any organ system. Managing irAEs can be a challenge, as these AEs differ from those associated with conventional chemotherapy in both appearance and care. Prompt and successful irAE management is important for patient health and the maintenance of effective therapy.
A group of advanced practice providers has developed Care Step Pathways (CSPs) to improve the management of irAEs (see Appendix and aimwithimmunotherapy.org). These CSPs, which combine established guidelines with practical experience, provide information on assessing, grading, and managing irAEs. Proactive strategies, implementation tactics, patient education points, and “red flags” are also featured.
This article provides a brief summary of ICI therapies currently used in oncology and an overview of irAEs that may occur during treatment. The importance of medication reconciliation and a thorough baseline assessment is stressed, and detailed information on baseline clinical and laboratory tests is provided. Specific CSPs for several irAEs, such as gastrointestinal toxicity, adrenal insufficiency, nephritis, and neuropathy, are reviewed in detail. As these CSPs illustrate, advanced practice providers are well positioned to play a key role in collaborative care for oncology patients, particularly with respect to providing in-depth patient education and “owning” AE management.
The introduction of immune checkpoint inhibitor (ICI) therapy as a mainstay of cancer therapy across hematologic and solid tumors has provided valuable new options for patients. However, it has also posed a challenge for the oncology team who must now identify and manage immune-related adverse events (irAEs). Prompt and successful irAE management not only improves patient well-being but may also allow patients to continue effective therapy or return to it more quickly after holds related to irAEs.
In 2017, the Melanoma Nursing Initiative (MNI) developed a series of advanced practice provider (APP)/nurse-focused educational materials to improve the recognition and management of irAEs in the setting of melanoma (Rubin, 2017). Those materials were quickly adopted by health-care providers (HCPs) working in other tumor types. To address the contextualization of the MNI materials for use in various tumor types, the AIM With Immunotherapy Immuno-Oncology Essentials (IO Essentials) initiative was commissioned. This article features a review of the use of the IO Essentials materials available at aimwithimmunotherapy.org in the pan-tumor setting. Companion articles on specific tumor-specific carveouts are also included in this supplement, including one on lung cancer (Davies, 2019) and another on head and neck squamous cell cancer (Fazer, 2019). Finally, this supplement also features a global article on the principles for triaging irAEs via telephone and in the office setting (Hoffner & Rubin, 2019).
CARE STEP PATHWAYS OVERVIEW AND DEVELOPMENT
The CSPs, which debuted in the MNI project, were designed to assist HCPs in identifying, grading, and managing irAEs in patients receiving ICIs. This article will reference all 12 CSPs featured on the IO Essentials site (see Table 1/Appendix). It includes an in-depth discussion of 4 CSPs with special relevance to the tumor types discussed in this article.
Table 1. Care Step Pathways From the IO Essentials Initiative (See Appendix).
| irAE category | Toxicity | Appendix location |
|---|---|---|
| Most common | Skin toxicities (pruritus, rash, etc.) | Appendix A |
| Gastrointestinal toxicities: diarrhea and colitis | Appendix B | |
| Thyroiditis | Appendix C | |
| Hepatic toxicities | Appendix D | |
| Less common but serious | Additional endocrinopathies | |
| Hypophysitis (pituitary) | Appendix E | |
| Adrenal insufficiency (adrenalitis) | Appendix F | |
| Diabetes | Appendix G | |
| Pneumonitis | Appendix H | |
| Easily overlooked | Arthralgia/arthritis | Appendix I |
| Mucositis/xerostomia | Appendix J | |
| Neuropathy | Appendix K | |
| Nephritis | Appendix L |
Note. irAE = immune-related adverse event.
The 11 CSPs developed by the MNI have been updated here, and a 12th CSP has been added on adrenal insufficiency. In updating these CSPs, the IO Essentials faculty reviewed them with an eye toward relevancy across tumor types. In addition, the CSPs were modified to address recently released guidance on irAE management from the Society for Immunotherapy of Cancer (Puzanov et al., 2017), American Society of Clinical Oncology (Brahmer et al., 2018), and the National Comprehensive Cancer Network (NCCN, 2018). The IO Essentials site contains other HCP and patient education tools, which will also be discussed.
IMMUNE CHECKPOINT INHIBITORS IN ONCOLOGY
Immune checkpoints, which may have evolved to prevent autoimmune responses, can be exploited by cancer cells to suppress the immune response to malignant cells (Marshall & Djamgoz, 2018). Therapies designed to inhibit these checkpoints improve tumor-specific immune responses and increase T-cell infiltration into tumors. In recognition of the importance of checkpoint inhibitors, two of the scientists first involved in this groundbreaking research, James P. Allison and Tasuku Honjo, were awarded the Nobel Prize in Medicine in 2018 (Nobel Assembly at Karolinska Institutet, 2018).
The first ICI therapy to reach clinical trials was ipilimumab; in 2011, this therapy was approved by the US Food and Drug Administration (FDA) for the treatment of metastatic melanoma (Dyck & Mills, 2017). Ipilimumab is an antibody that binds to and blocks cytotoxic T-lymphocyte associated protein 4 (CTLA-4), a molecule that suppresses T-cell responses. Other important checkpoint inhibitor targets and corresponding FDA-approved drugs include programmed cell death protein 1 (PD-1), which is blocked by nivolumab, pembrolizumab, and cemiplimab, and the PD-1 ligand (PD-L1), which is inhibited by atezolizumab, avelumab, and durvalumab (Table 2). The combination of nivolumab and ipilimumab has also been approved for certain indications. Currently, all FDA-approved checkpoint inhibitors are antibodies. In addition to the drugs and targets listed here, other agents and checkpoint inhibitor targets are currently being explored for potential oncology applications (Dyck & Mills, 2017).
Table 2. US Food and Drug Administration–Approved Immune Checkpoint Inhibitors.
| Name (target) | Indication | Detail | Biomarker testing required |
|---|---|---|---|
| Nivolumab (PD-1) | 1L unresectable or metastatic melanoma | Single agent or in combination with ipilimumab for BRAF V600 wild-type or BRAF V600 mutation-positive | – |
| Adjuvant treatment for melanoma | Patients with involvement of lymph nodes or metastatic disease following complete resection | – | |
| 2L metastatic NSCLC | Failure on platinum-doublet chemotherapy | – | |
| Failure on targeted agent (if applicable) | |||
| 3L metastatic small cell lung cancer | For patients with progression after platinum-based chemotherapy and at least 1 other line of therapy | – | |
| 2L advanced renal cell carcinoma (1L in combination) | After prior treatment with antiangiogenic treatment | – | |
| In combination with ipilimumab for treatment of intermediate or poor risk, previously untreated advanced RCC | |||
| 4L classical Hodgkin lymphoma | Adult patients | – | |
| After prior auto-HSCT and brentuximab vedotin treatment or after 3 or more lines of systemic therapy that includes auto-HSCT | |||
| 2L recurrent or metastatic HNSCC | Disease progression on or after platinum-based chemotherapy | – | |
| 2L locally advanced or metastatic urothelial carcinoma | Disease progression during or following prior platinum-based chemotherapy | – | |
| Disease progression < 12 months after (neo)adjuvant platinum-based chemotherapy | |||
| 2L metastatic colorectal cancer (MSI-H or dMMR) | Adult and pediatric patients (≥ 12 years) | MSI-H/dMMR | |
| Single agent or in combination with ipilimumab for disease progression following fluoropyrimidine, oxaliplatin, and irinotecan | |||
| 2L hepatocellular carcinoma | Patients treated previously with sorafenib | – | |
| Pembrolizumab (PD-1) | 1L unresectable or metastatic melanoma | Single agent | – |
| Adjuvant treatment for melanoma | Single agent for melanoma patients with involvement of lymph node(s) following complete resection | – | |
| 1L metastatic nonsquamous NSCLC | In combination with pemetrexed and platinum chemotherapy | EGFR, ALK | |
| Patients with no EGFR or ALK genomic tumor aberrations | |||
| 1L metastatic NSCLC with high PD-L1 expression | Single agent | PD-L1, EGFR, ALK | |
| TPS ≥ 50% | |||
| No EGFR or ALK genomic tumor aberrations | |||
| 1L squamous metastatic NSCLC | In combination with carboplatin and either paclitaxel/nab-placlitaxel for squamous NSCLC | – | |
| 2L metastatic NSCLC with PD-L1 expression | Single agent | PD-L1 | |
| TPS ≥ 1% | |||
| Disease progression on platinum-containing chemotherapy | |||
| Disease progression on targeted agent (if applicable) | |||
| 2L recurrent or metastatic HNSCC | Disease progression on or after platinum-based chemotherapy | – | |
| 4L relapsed or refractory classical Hodgkin lymphoma | Adult and pediatric patients | – | |
| Refractory disease or relapse after 3 or more prior treatments | |||
| 3L relapsed or refractory primary mediastinal large B-cell lymphoma | Adult and pediatric patients | – | |
| Relapsed after 2 or more lines of therapy | |||
| NOT RECOMMENDED for patients with PMBCL who require urgent cytoreductive therapy | |||
| 1L/2L locally advanced or metastatic urothelial carcinoma | Ineligible for cisplatin-based chemotherapy and PD-L1 CPS ≥ 10 | PD-L1 | |
| Ineligible for any platinum-containing chemotherapy regardless of PD-L1 status | |||
| Disease progression during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy | |||
| 2L MSI-H or dMMR cancers | Adult and pediatric patients | MSI-H/dMMR | |
| Solid tumors progressed following prior treatment and without satisfactory alternative treatment options | |||
| Colorectal cancer that has progressed following treatment with a fluoropyrimidine, oxaliplatin, and irinotecan | |||
| Limitation of use: safety and effectiveness not established in pediatric patients with MSI-H central nervous system cancers | |||
| 3L recurrent locally advanced or metastatic gastric or gastroesophageal junction adenocarcinoma | Patients whose tumors express PD-L1 (CPS ≥ 1) as determined by an FDA-approved test | PD-L1 | |
| Disease progression on or after 2 or more prior lines of therapy including fluoropyrimidine and platinum-containing chemotherapy and, if appropriate, HER2/neu-targeted therapy | |||
| 1L recurrent locally advanced or metastatic Merkel cell carcinoma | Accelerated approval | – | |
| 2L cervical cancer recurrent or metastatic | Patients whose tumors express PD-L1 (CPS ≥ 1) as determined by an FDA-approved test | PD-L1 | |
| Disease progression on or after chemotherapy | |||
| 2L hepatocellular carcinoma | Patients treated previously with sorafenib | – | |
| Cemiplimab-rwlc (PD-1) | 1L metastatic CSCC or locally advanced CSCC | Patients who are not candidates for curative surgery or curative radiation | – |
| Ipilimumab (CTLA-4) | 1L unresectable or metastatic melanoma | Adult and pediatric patients (≥ 12 years) | – |
| Single agent or in combination with nivolumab (see nivolumab PI) | |||
| Adjuvant treatment of stage IIIa melanoma | Involvement of regional lymph nodes of > 1 mm | – | |
| Undergone complete resection, including total lymphadenectomy | |||
| 1L advanced RCC | Intermediate or poor risk, previously untreated | – | |
| In combination with nivolumab | |||
| 2L metastatic colorectal cancer (MSI-H or dMMR) | Adults and pediatric patients > 12 years | MSI-H/dMMR | |
| In combination with nivolumab | – | ||
| Disease progression following treatment with fluoropyrimidine, oxaliplatin, and irinotecan | |||
| Atezolizumab (PD-L1) | 1L/2L locally advanced or metastatic urothelial carcinoma | Not eligible for cisplatin-containing chemotherapy and whose tumors express PD-L1 (PD-L1 stained tumor-infiltrating immune cells covering ≥ 5% of the tumor area) as determined by an FDA-approved test | PD-L1 |
| Not eligible for any platinum-containing chemotherapy regardless of PD-L1 status | |||
| Disease progression during or following platinum-containing chemotherapy, or within 12 months of (neo)adjuvant chemotherapy | |||
| 1L metastatic NSCLC | In combination with bevacizumab, paclitaxel, and carboplatin for NSCLC with no EGFR or ALK genomic tumor aberrations | – | |
| Atezolizumab (PD-L1; cont.) | 2L metastatic NSCLC | Disease progression on platinum-containing chemotherapy | – |
| Disease progression on targeted agent (if applicable) | |||
| Avelumab (PD-L1) | 1L metastatic Merkel cell carcinoma | Adult and pediatric patients (≥ 12 years) | – |
| 1L/2L locally advanced or metastatic urothelial carcinoma | Disease progression during or following platinum-containing chemotherapy | – | |
| Disease progression within 12 months of (neo)adjuvant platinum-containing chemotherapy | |||
| Durvalumab (PD-L1) | 2L locally advanced or metastatic urothelial carcinoma | Disease progression during or following platinum-containing chemotherapy | – |
| Disease progression within 12 months of (neo)adjuvant platinum-containing chemotherapy | |||
| Unresectable NSCLC | Stage III disease that has not progressed following concurrent platinum-based chemotherapy and radiation therapy | – | |
| Ipilimumab/nivolumab combination (CTLA-4/PD-1) | Unresectable or metastatic melanoma | In adults and pediatric patients 12 years and older | |
| Adjuvant treatment for stage III melanoma | Patients with cutaneous melanoma with pathologic involvement of regional lymph nodes > 1 mm who have undergone complete resection, including total lymphadenectomy | – | |
| Advanced RCC | Intermediate or poor risk, previously untreated | – | |
| MSI-H or dMMR metastatic colorectal cancer | Disease progression following treatment with a fluoropyrimidine, oxaliplatin, and irinotecan | MSI-H/dMMR |
Note. FDA-approved checkpoint inhibitors, indications, and required biomarker testing (as of December 30, 2018). PD-1 = programmed cell death protein 1; 1L = first line; 2L = second line; 3L = third line; 4L = fourth line; BRAF = serine/threonine-protein kinase B-Raf; NSCLC = non–small cell lung cancer; RCC = renal cell carcinoma; HSCT = hematopoietic stem cell transplantation; HNSCC = head and neck squamous cell carcinoma; MSI-H = microsatellite instability-high; dMMR = mismatch repair deficient; EGFR = epidermal growth factor receptor; ALK = anaplastic lymphoma kinase; PD-L1 = programmed cell death ligand 1; TPS = tumor proportion score; PMBCL = primary mediastinal large B-cell lymphoma; CPS = combined positive score; FDA = US Food and Drug Administration; HER2 = human epidermal growth factor receptor 2; CSCC = cutaneous squamous cell carcinoma; CTLA-4 = cytotoxic T-lymphocyte associated protein 4; PI = package insert.
Not only are new ICI therapies being introduced at a rapid pace, but indications and biomarker testing requirements for existing agents are continually being updated on the basis of evolving clinical data. Table 2 addresses the current biomarker testing requirements. Because of the frequent changes associated with these agents, HCPs should review the most recent FDA-approved prescribing information available at Drugs@FDA (accessdata.fda.gov/scripts/cder/daf/) before treating a new patient. Frequently, different indications for a given drug have distinct requirements for biomarker testing. For instance, pembrolizumab requires an FDA-approved test for PD-L1 levels before use in patients with urothelial carcinoma or as a single agent for non–small cell lung cancer, but not for the treatment of other types of cancer, including melanoma and head and neck squamous cell carcinoma (as of November 2018; Merck Sharp & Dohme Corp., 2018).
Combination regimens add to the complexity of managing ICI therapy. Possible combinations include multiple ICIs, ICIs with other immunotherapies, or ICIs with conventional chemotherapy or radiotherapy (Marshall & Djamgoz, 2018). Each combination poses its own challenges with respect to irAE profile and management, and in many cases the database is too small to allow an adequate understanding of possible irAEs. Providing up-to-date information on the evolving knowledge base of checkpoint inhibitors is one of the goals of the aimwithimmunotherapy.org website.
BEFORE YOU START
In addition to reviewing the most recent prescribing information for marker testing requirements and other critical information, the APP should complete several steps before treatment is initiated. One important step is medication reconciliation, with a particular focus on medications with the potential to exacerbate irAEs. For instance, gastrointestinal (GI) hemorrhage has been observed with ipilimumab, so anticoagulants should be used with caution (Association of Community Cancer Centers, 2016). Immune checkpoint inhibitor therapy can lead to nephritis, so potentially nephrotoxic medications should be reviewed (Puzanov et al., 2017). Advanced practice providers should also ask about over-the-counter, complementary, or alternative medications the patient may be taking, as these could potentially intensify irAEs.
Importance of Assessments and Laboratory Tests
Detailed baseline assessments PRIOR TO THERAPY INITIATION are absolutely critical to provide a valid starting point for detecting a change in clinical status during treatment. Table 3 describes recommended bowel, skin, pulmonary, neurologic, and cardiac assessments (Puzanov et al., 2017).
Table 3. Recommended Baseline Assessments Prior to Initiating Immunotherapy With Checkpoint Inhibitors.
| Category | Assessment |
|---|---|
| Patient history | ● Autoimmune, infectious disease, endocrine, and organ-specific disease history |
| ● Bowel function (frequency and consistency) | |
| ● Oncology disease and treatment history | |
| ● Concomitant medications, including over-the-counter, complementary, and alternative medications | |
| ● Energy level, daily activities | |
| ● Fatigue level | |
| Clinical examinations | ● Physical examination |
| ● Skin | |
| » Full skin and mucosal exam, taking note of the extent and type of lesions present | |
| ● Lungs | |
| » Baseline oxygen saturation on room air and during ambulation | |
| » Pulmonary function tests | |
| » 6-minute walk test | |
| ● Heart | |
| » Electrocardiogram | |
| ● Musculoskeletal | |
| » Joint examination/functional assessment | |
| ● Brain | |
| » Neurologic examination | |
| Laboratory tests | ● General blood work |
| » Complete blood count with differential | |
| » Comprehensive metabolic panel | |
| » Fasting lipid profile | |
| » HbA1c | |
| ● Infectious disease screen: HBsAg, HBsAb, HBcAb, HCAb, CMV antibody, T-spot test (tuberculosis), HIV antibody, HIV antigen (p24) | |
| ● Baseline serum creatinine | |
| ● Cardiac tests | |
| » Total creatinine kinase | |
| » Troponin 1 or T | |
| » BNP or NT-proBNP (if indicated) | |
| ● Endocrine tests | |
| » TSH | |
| » Free T4 | |
| - Total T3 | |
| » 8 am cortisol | |
| » 8 am ACTH | |
| Imaging | ● CT imaging |
| ● Brain MRI (if indicated) |
Note. HbA1c = glycosylated hemoglobin; HBsAg = hepatitis B surface antigen; HBsAb = hepatitis B surface antibody; HBcAb = hepatitis B core antibody; HCAb = hepatitis C antibody; CMV = cytomegalovirus; HIV = human immunodeficiency virus; BNP = brain natriuretic peptide; NT-proBNP = N-terminal pro b-type natriuretic peptide; TSH = thyroid stimulating hormone; T4 = thyroxine; T3 = triiodothyronine; ACTH = adrenocorticotropic hormone; CT = computed tomography; MRI = magnetic resonance imaging. Information from National Comprehensive Cancer Network (2018); Puzanov et al. (2017).
Laboratory assessments are a key component of baseline assessments, as some irAEs may present as laboratory abnormalities rather than as clinical changes. Baseline laboratory testing should include a complete blood count (CBC) with differential and a comprehensive metabolic panel (CMP; Table 3). Endocrinopathies can occur, so baseline laboratory testing should include thyroid-stimulating hormone (TSH), triiodothyronine (T3), and free thyroxine (T4).
Treatment monitoring includes a CBC with differential and a CMP before each infusion. Thyroid function studies should be performed every 6 to 8 weeks. Adrenocorticotropic hormone (ACTH) and morning cortisol monitoring should occur at regular intervals during and after termination of therapy (NCCN, 2018). Amylase and lipase testing should also be performed as clinically indicated, as immune-related pancreatitis may be detected early before symptoms appear based on laboratory results (NCCN, 2018). The test can be added to the CMP specimen if clinically indicated.
Finally, it is essential to identify colleagues in other departments and specialties, such as gastroenterology, endocrinology, dermatology, nephrology, and neurology, who can serve as consultants and help manage irAEs. Using their expertise helps APPs manage proactively and minimize the negative outcomes potentially associated with irAEs.
ADMINISTRATION AND PHARMACOLOGIC CONSIDERATIONS
As soon as patients receive their first dose of immunotherapy, the APP should ensure that treatment is documented in the electronic medical record (EMR), if available. In addition, an alert should be placed in the EMR so that patients can be identified immediately if they present to the emergency department or another service. This alert should remain after treatment termination, as irAEs may not occur until much later. At some clinics, patients are also given an immunotherapy wallet card to alert medical providers or emergency personnel to their immunotherapy status and provide oncology contact information (Brahmer et al., 2018). The Oncology Nursing Society and most drug manufacturers provide drug-specific wallet cards for patients.
Currently available ICI therapies are administered as intravenous (IV) infusions over a period ranging from 30 to 90 minutes depending on the agent. For some, dosing is weight based, whereas others are administered at a fixed dosage (Davies & Duffield, 2017). Dosing frequency varies based on the drug, the setting (treatment vs. adjuvant therapy), and, for some drugs, the dose. Infusion reactions, typically consisting of fever and chills, may occur in some patients. They are more common in patients receiving agents that block CTLA-4 (Kumar et al., 2017).
For avelumab, premedication with an antihistamine and acetaminophen is recommended prior to the first 4 infusions. Premedication for subsequent doses is based on clinical judgment and the presence/severity of prior infusion reactions (EMD Serono, 2017). Other ICIs do not have premedication recommendations in their prescribing information.
Use of concomitant corticosteroids such as prednisone at treatment initiation is a debated topic. A recent analysis found that lung cancer patients who received ≥ 10 mg of prednisone or equivalent daily at the start of PD-1 or PD-L1 blockade had less favorable outcomes than patients who received < 10 mg/day at baseline, even if those patients were ultimately treated with corticosteroids (Arbour et al., 2018). Similarly, a preliminary study found that cumulative antibiotic use at baseline is associated with poorer outcomes in cancer patients treated with ICIs (Tinsley et al., 2018). Both analyses were retrospective studies that need confirmation in randomized trials. Nevertheless, the data suggest that, if possible, corticosteroids and antibiotics should be avoided at immunotherapy initiation and reserved for use as later treatment if necessary.
BEST PRACTICES IN MANAGING IMMUNE-RELATED ADVERSE EVENTS
Management Begins With Early Recognition
The widespread use of immunotherapy in oncology patients has dramatically changed the way APPs screen for and manage AEs. Unlike typical chemotherapy-associated AEs, irAEs have unique presentations and affect different body systems. Because of this, the learning curve for HCPs can be daunting. This article, along with the CSPs in the Appendix, is designed to help minimize the unexpected and provide information on best practices in managing irAEs. In a way, detecting irAEs is like working a puzzle—all the pieces of the puzzle are needed to achieve a successful outcome (Figure 1).
Figure 1.
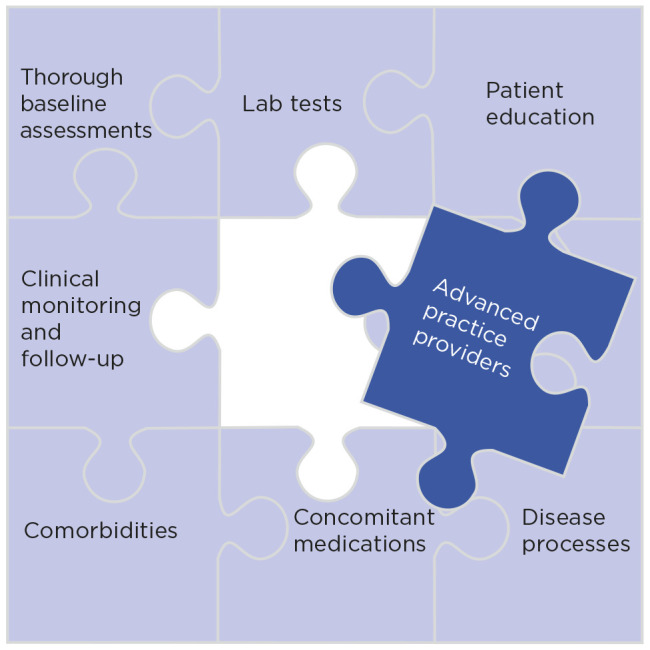
Representation of the role of the advanced practice provider in detecting immune-related adverse events.
Advanced practice providers need to be vigilant and aware of subtle presentations, such as symptoms attributed by the patient to “the flu” or a cold. It is important to follow up on all AEs, as the patient’s condition can deteriorate rapidly. Patients need to be educated about common symptoms, such as rashes, shortness of breath, and changes in urination or bowel movements. The printable, customizable patient action plans featured on the IO Essentials site are helpful educational primers on irAEs to share with patients and encourage dialogue and active communication about irAEs (see aimwithimmunotherapy.org/patient-resourcesaction-plans).
Advanced practice providers should develop laboratory panels for potential irAEs so that when symptoms occur they are prepared to pursue investigations without delay. Sometimes, changes from baseline can be the piece of the puzzle that alerts the APP to a potential irAE, even if the laboratory value is within the normal range. Of course, these changes cannot be detected without thorough baseline assessments (Table 3). Laboratory results need to be considered within the context of clinical assessment. For instance, laboratory values may be within normal limits for some arthralgias, but the patient may still be symptomatic.
Overview of Immune-Related Adverse Events
Immune-related adverse events can affect almost any body system (Brahmer et al., 2018; Puzanov et al., 2017). Although ICIs block the same general immune pathway, irAE profiles appear to differ based on the targeted molecule and the exact structure of the inhibitor (IgG1 vs. IgG4). For instance, CTLA-4 inhibitors are associated with a significantly higher risk of severe colitis than PD-1/PD-L1 inhibitors (de Velasco et al., 2017). However, it is important to remember that accurate comparisons among different agents are difficult because of variations in the definitions used for irAEs in different trials (Maughan, Bailey, Gill, & Agarwal, 2017).
Immune-related adverse event management is based on the specific AE and its severity, which, when possible, is graded by the Common Terminology Criteria for Adverse Events (CTCAE) on a scale from 1 (mild) to 4 (life-threatening). Milder presentations may in some cases require only monitoring, but moderate or severe irAEs often require interruption or discontinuation of immunotherapy along with initiation of corticosteroid therapy (Brahmer et al., 2018; Kumar et al., 2017).
Patients with certain tumor types may be predisposed to certain irAEs. For example, patients receiving ICIs with hematologic malignancies who have undergone allogeneic hematopoietic stem cell transplantation are predisposed to graft-vs.-host disease (Haverkos et al., 2017). Patients with GI malignancies may be predisposed to diarrhea/colitis, whereas those with renal cell carcinoma are predisposed to nephritis, as illustrated below. In the following sections, we provide details about the assessment and management of GI toxicity, adrenal insufficiency, nephritis, and neuropathy.
Gastrointestinal Toxicity (Appendix B)
Gastrointestinal toxicity is a common form of irAE, second only to dermatologic irAEs. Diarrhea occurs in 19% to 33% of patients on checkpoint inhibitor monotherapy and in up to 44% of patients on combination anti–CTLA-4/anti–PD-1 therapy (Puzanov et al., 2017). Before initiating immunotherapy, HCPs should educate patients on how to recognize immunotherapy-related diarrhea. It may not appear as fully liquid bowel movements; increases in frequency and/or loss of consistency suggest a potential onset of diarrhea that should be evaluated and addressed. Patients who have been on previous oncologic therapies may need education concerning the difference in GI manifestations during immunotherapy. For example, patients with metastatic kidney cancer may have received vascular endothelial growth factor (VEGF) tyrosine kinase inhibitors. The diarrhea that patients experience with those therapies is unique compared with that seen with immunotherapy (Schmidinger & Bellmunt, 2010). The oral VEGF tyrosine kinase inhibitors have a short half-life, and diarrhea significantly improves or fully resolves with treatment interruption. In contrast, diarrhea observed with ICI therapy is more prolonged and may continue in spite of treatment interruption and the use of antidiarrheals. It is important for HCPs to understand that distinct difference and incorporate that knowledge into patient education.
The assessment of GI irAEs may be complicated by the underlying malignancy, comorbidities, prior therapy, and surgical procedures, such as resections in patients with colorectal cancer or bariatric procedures in obese patients. As shown in the CSP, other possible causes of diarrhea should always be explored carefully. Patients who present with diarrhea should be asked for detailed information concerning bowel function, such as frequency and consistency of bowel movements, presence of mucus in the bowel movements, and problems with constipation, abdominal pain, or cramping. They should also be asked about their dietary habits and previous surgical history. Another relevant area of inquiry is whether they have tried any interventions, such as over-the-counter loperamide or prescription diphenoxylate/atropine. If so, what impact has it had?
Patients with intestinal metastases are of particular concern, as they may have short bowel syndrome as a result of resection, resulting in malnutrition, diarrhea, and dehydration (Jeppesen, 2014). Immunotherapy-related GI toxicity has the potential to worsen diarrhea in these patients and put them at an increased risk for dehydration.
Advanced practice providers should be alert to recognizing early presentations of colitis (inflammation of the intestinal lining). As described in the CSP, patients with fever, abdominal pain, or blood/mucus in the stool in addition to diarrhea could have colitis and should be evaluated and monitored carefully. Suspected colitis should be evaluated by stool cultures to rule out infectious causes; imaging with computed tomography (CT) and colonoscopy with biopsy may be required.
Mild GI symptoms should be managed by close monitoring, a bland diet, and adequate hydration. Dietary consultations should be initiated by the APP so that dietary recommendations can be made based on history and anatomy. Immunotherapy treatment can usually be continued, and loperamide can be considered for some patients. The use and impact of antidiarrheals should be monitored. If patients are given an antidiarrheal, they should be contacted about 24 hours later to see if they are experiencing continuing diarrhea. If so, reassessment is warranted, particularly in kidney cancer patients, as diarrhea-associated dehydration may increase the risk of chronic kidney disease.
For more serious symptoms, laboratory evaluations should be implemented as clinically indicated, including a CBC, chemistry panel, blood urea nitrogen, and creatinine. Stool tests should include cultures and susceptibilities for Clostridium difficile and other potential infectious etiologies. It may be appropriate to consider a CT scan of the abdomen and/or a colonoscopy.
If diarrhea is refractory to oral antidiarrheal agents for at least 5 days, oral prednisone should be initiated at a dosage of 1 mg/kg/day. The patient should be contacted 24 hours later to ascertain the impact of treatment. Patients who continue to have diarrhea may not be fully absorbing the oral corticosteroids. It may be appropriate to bring the patient in for IV fluids and IV corticosteroids, possibly daily as an outpatient for several days. If their condition improves, they can be converted to oral corticosteroids, but if frequent dehydration and diarrhea persists, the patient should be admitted. Once admitted, the patient would be an appropriate candidate for a gastroenterology consult and further evaluation by CT or colonoscopy while continuing IV corticosteroids and dietary management. Refractory diarrhea from immunotherapy may respond to infliximab (Reddy, Schneider, & Tai, 2018).
The management of colitis also involves the use of corticosteroids. For severe or life-threatening symptoms, the dose of corticosteroids may need to be increased and the patient will likely require hospitalization to manage fluid and electrolyte balance and maintain adequate hydration. Care must be taken with the use of analgesics and antidiarrheals in patients with colitis. For those who do not respond to 72 hours of high-dose IV corticosteroids, infliximab may be considered if bowel perforation or sepsis is not present. For patients who fail to respond to infliximab, vedolizumab is an option (Reddy et al., 2018).
Adrenal Insufficiency (Appendix F)
Adrenal insufficiency is a relatively rare irAE, but it can be difficult to recognize due to its often vague presenting symptoms, including fatigue, appetite loss, and mood changes (Ariyasu et al., 2018; Brahmer et al., 2018). The presentation may be due to primary adrenal insufficiency, which is an inflammation/enlargement of the adrenal gland itself due to immunotherapy, or secondary adrenal insufficiency, stemming from immunotherapy-related pituitary dysfunction or hypophysitis (Girotra et al., 2018). For patients who have had a radical nephrectomy, adrenal insufficiency may be due to the removal of the adrenal gland at the time of surgery. Adrenal insufficiency can be life-threatening; it may lead to hypotension and trigger a cardiovascular collapse (Tsukizawa et al., 2018). Accordingly, routine monitoring and prompt recognition is critical (Girotra et al., 2018).
As shown in the CSP, laboratory tests, including morning cortisol and ACTH, should be initiated in patients presenting with symptoms suggestive of adrenal insufficiency. Both primary and secondary adrenal insufficiencies are associated with low morning cortisol, but patients with primary adrenal insufficiency have high ACTH levels, whereas those with secondary insufficiency have low ACTH levels (Brahmer et al., 2018). Electrolyte abnormalities, including hyponatremia and hyperkalemia, are common in patients with adrenal insufficiency. Confirmation of the diagnosis requires a cortisol stimulation test, typically done in the morning. After ACTH stimulation, cortisol levels are measured at 30 and 60 minutes; a level less than 18 μg/dL at both time points confirms the diagnosis (Bornstein et al., 2016). Once the diagnosis is confirmed, a full endocrine evaluation should be performed to ensure that no other endocrine disorders are involved.
As shown in the CSP, the initial management of adrenal insufficiency requires holding ICI therapy (Min, 2016; Sznol et al., 2017). Adrenal hormone replacement (corticosteroid administration), the treatment of choice, should be completed before any other hormone is replaced to avoid adrenal crisis (NCCN, 2018). In addition, fludrocortisone replacement, at a dosage of 0.1 mg every other day initially and titrated to effect, is appropriate. The overarching goal of adrenal hormone replacement is to establish the lowest possible dose to prevent adrenal insufficiency; doses may be titrated down when patients are stabilized. In the case of adrenal crisis, patients who are hemodynamically unstable may require hospitalization and fluid bolus resuscitation. As with other endocrinopathies, in most cases ICI therapy can be restarted once a patient is hemodynamically stable and adequate hormone replacement has been completed.
As highlighted in the Implementation section of the CSP, patient education is a critical component of adrenal insufficiency management. It is likely lifetime hormone replacement will be necessary, so patients need to be educated on stress dosing of corticosteroids to avoid adrenal crisis; they may need double or triple doses of corticosteroids for 24 to 48 hours in the case of illness, surgery, or trauma. Patients should be advised to wear a medical alert bracelet at all times (Bornstein et al., 2016; Brahmer et al., 2018).
Nephritis (Appendix L)
Nephritis, the chronic inflammation of the kidney tubules that can lead to kidney damage, is a relatively rare but serious irAE (Cortazar et al., 2016). The risk of nephritis is higher in patients on anti–PD-1 or anti–PD-1/anti–CTLA-4 combination immunotherapy compared with anti–PD-L1 drugs (Puzanov et al., 2017). Patients with kidney cancer are at particularly high risk, as kidney tissues become inflamed due to the disease; those who have had a partial or radical nephrectomy are at risk for nephritis simply because they have decreased renal function. Nephrotoxic drugs, including furosemide, thiazide diuretics, triamterene, allopurinol, proton pump inhibitors, and certain antibiotics, can also contribute to nephritis risk. An awareness of concurrent medications helps minimize and manage potential nephritis in patients receiving immunotherapy (Khan, Loi, & Rosner, 2017; Koda et al., 2018).
Because renal toxicity may be asymptomatic, serum creatinine levels should be monitored at baseline and throughout the treatment course (Puzanov et al., 2017). Patient education is also vital: patients should be told to call if they notice decreased urine output, a darker urine color, or the presence of bubbles, foam, or blood in the urine, which may be signs of proteinuria or kidney damage. Vigilance for signs of proteinuria is particularly important for kidney cancer patients, as proteinuria is more common in this population due to decreased renal function at baseline.
Urine changes suggesting potential nephritis should alert the clinician to evaluate further, including ordering laboratory tests with a basic or comprehensive metabolic panel and routine urinalysis to evaluate the osmolality, color, and protein content. It may be necessary to perform a 24-hour urine collection and measure creatinine and/or protein for further evaluation.
As shown in the CSP, the management of moderate-to-severe nephritis usually begins with interrupting immunotherapy. Oral corticosteroids may be required, with frequent monitoring of blood chemistry and urine. Higher doses of prednisone may be needed if no improvement in lab results is detected within a week. If symptoms do not improve with high doses of corticosteroids, additional immunosuppressive medications may be required. Nephrology consults should be considered for patients with severe presentations or persistent elevations in serum creatinine. A renal biopsy may be required, and in rare situations patients may require hemodialysis.
Neuropathy (Appendix K)
Neurologic toxicities associated with immunotherapy range from headaches to encephalitis. Neurologic irAEs should be suspected in patients who develop new sensory or motor symptoms after treatment initiation (Liao, Shroff, Kamiya-Matsuoka, & Tummala, 2014). The most common neurologic toxicity is neuropathy (Larkin et al., 2017). It is difficult to ascertain the incidence of immune-related neuropathy because it has a heterogeneous presentation and is often unrecognized (Liao et al., 2014). Immune-related neuropathy may occur on a backdrop of existing neuropathy, particularly in patients exposed to platinum-based therapies (Banach, Juranek, Zygulska, 2016), or take the form of a transient peripheral sensorimotor neuropathy (Larkin et al., 2017). As with other irAEs, baseline assessments are essential for prompt recognition.
Immune checkpoint inhibitor–induced neuropathies have varied presentations and manifestations, including peripheral or systemic/central. Peripheral neuropathies can be sensory or motor, and symmetric or asymmetric. Numbness or paresthesias may occur with or without pain; sensory ataxia may be present (Brahmer et al., 2018). The more rare but serious central neurologic presentations include myasthenia gravis, Guillain-Barré syndrome, autonomic neuropathy, and encephalitis (Larkin et al., 2017; Puzanov et al., 2017). Both HCPs and patients need to be alert to central neurologic symptoms such as breathing difficulties, severe headache, or mental status changes.
As discussed in the CSP, patients who present with neuropathy symptoms should be evaluated for disease-related causes, such as progression of cancer in the central nervous system and for other infectious and noninfectious causes. In many cases, a brain/spine magnetic resonance imaging will be required. A neurology consult should be arranged to include electromyography or nerve conduction tests if clinically indicated (Brahmer et al., 2018; Puzanov et al., 2017).
Immunotherapy is usually withheld for moderate (grade 2) toxicities or higher. High-dose corticosteroids should be used, and supportive medications such as gabapentin, pregabalin, or duloxetine can be used for symptom management. As shown in the Red Flag section of the CSP, systemic/central neurologic presentations are very concerning. Vasculitis syndromes of both the central and peripheral nervous system have been reported (Daxini, Cronin, & Sreih, 2018). Both HCPs and patients need to be alert to central neurologic symptoms because they can be life-threatening.
ROLE OF THE ADVANCED PRACTICE PROVIDER
As drugs advance through the pharmaceutical pipeline, HCPs face a learning curve in incorporating them into clinical care. Oncology APPs frequently participate in clinical trials that serve as the basis for drug approval, so they have early experience with groundbreaking new therapies. This experience positions APPs as a resource to help educate and support not only patients, but other HCPs as well. The overall goal is to minimize surprise—to proactively prepare for and recognize new AE presentations so they can be managed quickly and effectively.
One of the most important duties of APPs is patient education, which should include family members and caretakers when possible. As discussed, customizable patient resource information packets for each checkpoint inhibitor (Patient Action Plans) are featured under Patient Resources at aimwithimmunotherapy.org. By improving their awareness of possible irAEs, patients are empowered to become participating members of their own health-care team. They are in a position to recognize potential irAEs at the earliest possible time point, which can help minimize side effects and allow them to continue immunotherapy at effective doses.
However, even the best-educated and most motivated patient does not replace the observant eye of an experienced care provider. Frequently, patients on cancer immunotherapy are overwhelmed, tired, or distraught. They may not notice or effectively communicate early signs of irAEs. Advanced practice providers need to probe closely concerning the patient’s condition and any changes or symptom manifestations that have occurred since the last visit. It is particularly important to be aware of subtle presentations.
At the same time, the APP must be aware that not all presentations during ICI therapy are reflective of irAEs. Recently, a patient presented to our office with classic signs of pneumonitis, but during a follow-up phone call, the patient reported that he had not experienced a significant response to steroid therapy. Ultimately, a computerized axial tomography scan showed he was suffering from a bilateral pulmonary embolism that was unrelated to immunotherapy but would have been fatal if not detected.
As this case illustrates, another critical responsibility of the APP is to rigorously follow up on irAEs, both evolving symptoms and responses to management initiatives. Often, a phone call at the right time can be the difference between a quick resolution of an AE and deterioration of a mild event into a potentially life-threatening one. Differential diagnoses frequently evolve over time, so APPs need to reassess and modify treatment decisions based on results.
With the increasing complexity of oncology care, patients are best served when HCPs embrace a multidisciplinary collaborative care model. Advanced practice providers play a critical role in this process by “owning” AE management and sharing their knowledge with less experienced members of the oncology community (Kirkwood & Ribas, 2017). Members of community-based practices may not have expertise concerning the AE management required by new therapies, so they may need to reach out to academic centers or to different specialties. They can also take advantage of digital portals, such as the Facebook forum associated with aimwithimmunotherapy.org, which can be accessed at facebook.com/IOEssentials.
Oncology treatment options continue to expand at a rapid rate, so it has never been more important for oncology APPs to stay up to date and reach out to experts. We hope that the CSPs at aimwithimmunotherapy.org serves as a valuable resource for the oncology community and help improve AE management in patients receiving immunotherapy with ICIs.
Footnotes
Funding for this article was provided by an educational grant from Merck and Co., Inc. Laura S. Wood has served on speakers bureaus for Bristol-Myers Squibb, Genentech, and Pfizer. Writing and editorial support were provided by Lisa Tushla, PhD, H(ASCP), at Terranova Medica and Sharon L. Cross, PhD, on behalf of Terranova Medica. Drs. Tushla and Cross have nothing to disclose.
REFERENCES
- Arbour K. C., Mezquita L., Long N., Rizvi H., Auclin E., Ni A.,…Hellman M.D. (2018). Impact of baseline corticosteroids on efficacy of programmed cell death-1 and programmed death-ligand 1 blockade in patients with non-small-cell lung cancer. Journal of Clinical Oncology, 36(28), 2872–2878. 10.1200/JCO.2018.79.0006 [DOI] [PubMed] [Google Scholar]
- Ariyasu H., Inaba H., Ota T., Yamaoka H., Furukawa Y., Iwakura H.,...Akamizu T. (2018). Thyrotoxicosis and adrenocortical hormone deficiency during immune-checkpoint inhibitor treatment for malignant melanoma. In Vivo, 32(2), 345–351. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/29475919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association of Community Cancer Centers (2016). Drug-drug interactions and the checkpoint inhibitors. Retrieved from https://accc-iclio.org/resources/drug-drug-interactions-checkpoint-inhibitors [Google Scholar]
- AstraZeneca (2018). Imfinzi (durvalumab) package insert. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/761069s002lbl.pdf [Google Scholar]
- Banach M., Juranek J. K., & Zygulska A. L. (2016). Chemotherapy-induced neuropathies—A growing problem for patients and health care providers. Brain and Behavior, 7(1), e00558 10.1002/brb3.558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornstein S. R., Allolio B., Arlt W., Bartel A., Don-Wauchope A., Hammer G. D.,...Torpy D. J. (2016). Diagnosis and treatment of primary adrenal insufficiency: An Endocrine Society clinical practice guideline. Journal of Clinical Endocrinology and Metabolism, 101(2), 364–389. 10.1210/jc.2015-1710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brahmer J. R., Lacchetti C., Schneider B. J., Atkins M. B., Brassil K. J., Caterino J. M.,...Thompson J. A. (2018). Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology Clinical Practice Guideline. Journal of Clinical Oncology, 36(17), 1714–1768. 10.1200/JCO.2017.77.6385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bristol-Myers Squibb (2018a). Opdivo (nivolumab) package insert. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/125554s067lbl.pdf [Google Scholar]
- Bristol-Myers Squibb (2018b). Yervoy (ipilimumab) package insert. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/125377s096lbl.pdf [Google Scholar]
- Cortazar F. B., Marrone K. A., Troxell M. L., Ralto K. M., Hoenig M. P., Brahmer J. R.,...Leaf D. E. (2016). Clinicopathological features of acute kidney injury associated with immune checkpoint inhibitors. Kidney International, 90(3), 638–647. 10.1016/j.kint.2016.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies M. (2019). PD-1/PD-L1 inhibitors for non–small cell lung cancer: Incorporating Care Step Pathways for effective side-effect management. Journal of the Advanced Practitioner in Oncology, 10(suppl 1), 21–35. 10.6004/jadpro.2019.10.2.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies M., & Duffield E. A. (2017). Safety of checkpoint inhibitors for cancer treatment: Strategies for patient monitoring and management of immune-mediated adverse events. Immunotargets and Therapy, 6, 51–71. 10.2147/ITT.S141577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daxini A., Cronin K., & Sreih A. G. (2018). Vasculitis associated with immune checkpoint inhibitors—A systematic review. Clinical Rheumatology, 37(9), 2579–2584. 10.1007/s10067-018-4177-0 [DOI] [PubMed] [Google Scholar]
- de Velasco G., Je Y., Bossé D., Awad M. M., Ott P. A., Moreira R. B.,…Choueiri T. K. (2017). Comprehensive meta-analysis of key immune-related adverse events from CTLA-4 and PD-1/PD-L1 inhibitors in cancer patients. Cancer Immunology Research, 5(4), 312–318. 10.1158/2326-6066.CIR-16-0237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyck L., & Mills K. H. G. (2017). Immune checkpoints and their inhibition in cancer and infectious diseases. European Journal of Immunology, 47(5), 765–779. 10.1002/eji.201646875 [DOI] [PubMed] [Google Scholar]
- EMD Serono (2017). Bavencio (avelumab) package insert. Retrieved from https://www.emdserono.com/content/dam/web/corporate/non-images/country-specifics/us/pi/bavencio-pi.pdf [Google Scholar]
- Fazer C. (2019). Checkpoint inhibitor immunotherapy for head and neck cancer: Incorporating Care Step Pathways for effective side-effect management. Journal of the Advanced Practitioner in Oncology, 10(suppl 2), 37–46. 10.6004/jadpro.2019.10.2.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genentech (2018). Tecentriq (atezolizumab) package insert. Retrieved from https://www.gene.com/download/pdf/tecentriq_prescribing.pdf [Google Scholar]
- Girotra M., Hansen A., Farooki A., Byun D. J., Min L., Creeland B. C.,…Gravell A. E. (2018). The current understanding of the endocrine effects from immune checkpoint inhibitors and recommendations for management. Jnci Cancer Spectrum, 2(3), pky021 10.1093/jncics/pky021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haverkos B. M., Abbott D., Hamadani M., Armand P., Flowers M. E., Merryman R.,...Devine S. M. (2017). PD-1 blockade for relapsed lymphoma post–allogeneic hematopoietic cell transplant: High response rate but frequent GVHD. Blood, 130(2), 221–228. 10.1182/blood-2017-01-761346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffner B., & Rubin K. (2019). Meeting the challenge of immune-related adverse events with optimized telephone triage and dedicated oncology acute care. Journal of the Advanced Practitioner in Oncology, 10(suppl 2), 9–20. 10.6004/jadpro.2019.10.2.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeppesen P. B. (2014). Spectrum of short bowel syndrome in adults: Intestinal insufficiency to intestinal failure. Journal of Parenteral and Enteral Nutrition, 38(1S), 8S–13S. 10.1177/0148607114520994 [DOI] [PubMed] [Google Scholar]
- Khan S., Loi V., & Rosner M. H. (2017). Drug-induced kidney injury in the elderly. Drugs & Aging, 34(10), 729–741. 10.1007/s40266-017-0484-4 [DOI] [PubMed] [Google Scholar]
- Kirkwood J. M., & Ribas A. (2017). Collaborative care in melanoma: The essential role of the nurse. Clinical Journal of Oncology Nursing, 21(4 suppl), 4–6. Retrieved from https://cjon.ons.org/cjon/21/4/supplement/collaborative-care-melanoma-essential-role-nurse [DOI] [PubMed] [Google Scholar]
- Koda R., Watanabe H., Tsuchida M., Iino N., Suzuki K., Hasegawa G.,...Narita I. (2018). Immune checkpoint inhibitor (nivolumab)-associated kidney injury and the importance of recognizing concomitant medications known to cause acute tubulointerstitial nephritis: A case report. Bmc Nephrology, 19, 48 10.1186/s12882-018-0848-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar V., Chaudhary N., Garg M., Floudas C. S., Soni P., & Chandra A. B. (2017). Current diagnosis and management of immune related adverse events (irAEs) induced by immune checkpoint inhibitor therapy. Frontiers in Pharmacology, 8, 49 10.3389/fphar.2017.00049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larkin J., Chmielowski B., Lao C. D., Hodi F. S., Sharfman W., Weber J.,...Reardon D. A. (2017). Neurologic serious adverse events associated with nivolumab plus ipilimumab or nivolumab alone in advanced melanoma, including a case series of encephalitis. Oncologist, 22(6), 709–718. 10.1634/theoncologist.2016-0487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao B., Shroff S., Kamiya-Matsuoka C., & Tummala S. (2014). Atypical neurological complications of ipilimumab therapy in patients with metastatic melanoma. Neuro-Oncology, 16(4), 589–593. 10.1093/neuonc/nou001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall H. T., & Djamgoz M. B. A. (2018). Immuno-oncology: Emerging targets and combination therapies. Frontiers in Oncology, 8, 315 10.3389/fonc.2018.00315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maughan B. L., Bailey E., Gill D. M., & Agarwal N. (2017). Incidence of immune-related adverse events with program death receptor-1- and program death receptor-1 ligand-directed therapies in genitourinary cancers. Frontiers in Oncology, 7, 56 10.3389/fonc.2017.00056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merck Sharp & Dohme Corp (2018). Keytruda (pembrolizumab) package insert. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/125514s035lbl.pdf [Google Scholar]
- Min L. (2016). Immune-related endocrine disorders in novel immune checkpoint inhibition therapy. Genes & Diseases, 3(4), 252–256. 10.1016/j.gendis.2016.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Comprehensive Cancer Network (2018). NCCN Clinical Guidelines in Oncology: Management of immunotherapy-related toxicities. v1.2019. Retrieved from https://www.nccn.org/professionals/physician_gls/pdf/immunotherapy.pdf [DOI] [PubMed] [Google Scholar]
- Nobel Assembly at Karolinska Institutet (2018). The Nobel Assembly at Karolinska Institutet has today decided to award the 2018 Nobel Prize in Physiology or Medicine jointly to James P. Allison and Tasuku Honjo for their discovery of cancer therapy by inhibition of negative immune regulation. Retrieved from https://www.nobelprize.org/uploads/2018/10/press-medicine2018.pdf [Google Scholar]
- Puzanov I., Diab A., Abdallah K., Bingham C. O. III, Brogdon C., Dadu R.,...Ernstoff M. S. (2017). Managing toxicities associated with immune checkpoint inhibitors: Consensus recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group. Journal for Immunotherapy of Cancer, 5, 95 10.1186/s40425-017-0300-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy H. G., Schneider B. J., & Tai A. W. (2018). Immune checkpoint inhibitor-associated colitis and hepatitis. Clinical and Translational Gastroenterology, 9(9), 180 10.1038/s41424-018-0049-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regeneron Pharmaceuticals (2018). Libtayo (cemiplimab-rwlc) package insert. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/761097s000lbl.pdf [Google Scholar]
- Rubin K. M. (2017). Advances in melanoma: The rationale for the Melanoma Nursing Initiative. Clinical Journal of Oncology Nursing, 21(4 suppl), 7–10. Retrieved from https://cjon.ons.org/cjon/21/4/supplement/advances-melanoma-rationale-melanoma-nursing-initiative [DOI] [PubMed] [Google Scholar]
- Schmidinger M., & Bellmunt J. (2010). Plethora of agents, plethora of targets, plethora of side effects in metastatic renal cell carcinoma. Cancer Treatment Reviews, 36(5), 416–424. 10.1016/j.ctrv.2010.01.003 [DOI] [PubMed] [Google Scholar]
- Sznol M., Postow M. A., Davies M. J., Pavlick A. C., Plimack E. R., Shaheen M.,…Robert C. (2017). Endocrine-related adverse events associated with immune checkpoint blockade and expert insights on their management. Cancer Treatment Reviews, 58, 70–76. 10.1016/j.ctrv.2017.06.002 [DOI] [PubMed] [Google Scholar]
- Tinsley N., Zhou C., Villa S., Tan G., Lorigan P., Blackhall F. H.,…Cook N. (2018). Cumulative antibiotic use and efficacy of immune checkpoint inhibitors in patients with advanced cancer. Journal of Clinical Oncology, 36(15 suppl), 3010 10.1200/JCO.2018.36.15_suppl.3010 [DOI] [Google Scholar]
- Tsukizawa Y., Kondo K., Ichiba T., Naito H., Mizuki K., & Masuda K. (2018). Refractory hypotension due to nivolumab-induced adrenal insufficiency. Nagoya Journal of Medical Science, 80(2), 285–288. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5995729/ [DOI] [PMC free article] [PubMed] [Google Scholar]


