Key Points
Question
Is early introduction of gluten associated with a reduced prevalence of celiac disease at age 3 years?
Findings
In this prespecified analysis of a randomized clinical trial, the mean quantities of gluten consumed in an early introduction group between age 4 and 6 months was 2.66 g/wk and 0.49 g/wk in a standard introduction group that did not receive gluten until at least age 6 months. Significantly more children in the standard introduction group had a diagnosis of celiac disease confirmed than in the early introduction group (1.4% vs 0%).
Meaning
The findings of this trial indicate that early consumption of high-dose gluten should be considered as a strategy to prevent celiac disease in future research.
Abstract
Importance
There are no strategies for the prevention of celiac disease (CD). Current guidelines stating that the age at gluten introduction does not affect the prevalence of CD are based on the results from several randomized clinical trials, but the doses of gluten and timing of its introduction varied.
Objective
To determine whether early introduction of high-dose gluten lowers the prevalence of CD at age 3 years.
Design, Setting, and Participants
The Enquiring About Tolerance (EAT) Study was an open-label randomized clinical trial. A total of 1303 children from the general population in England and Wales were recruited and followed up from November 2, 2009, to July 30, 2012. For the present study, samples were collected from November 1, 2012, to March 31, 2015, and data were analyzed from April 25, 2017, to September 17, 2018.
Interventions
Infants were randomized to consume 6 allergenic foods (peanut, sesame, hen's egg, cow's milk, cod fish, and wheat) in addition to breast milk from age 4 months (early introduction group [EIG]) or to avoid allergenic foods and follow UK infant feeding recommendations of exclusive breastfeeding until approximately age 6 months (standard introduction group [SIG]).
Main Outcomes and Measures
Evaluation of CD was an a priori secondary end point of the EAT Study, and at age 3 years, all children with available serum samples were tested for antitransglutaminase type 2 antibodies. Children with antibody levels greater than 20 IU/L were referred to independent gastroenterologists for further investigation.
Results
Of the 1004 infants included in the analysis, 514 were male (51.2%). The mean (SD) quantity of gluten consumed between ages 4 and 6 months was 0.49 (1.40) g/wk in the SIG and 2.66 (1.85) g/wk in the EIG (P < .001). Mean (SD) weekly gluten consumption ranged from 0.08 (1.00) g/wk at age 4 months to 0.9 (2.05) g/wk at age 6 months in the SIG vs 1.3 (1.54) g/wk at age 4 months to 4.03 (2.40) g/wk at age 6 months in the EIG. Seven of 516 children from the SIG (1.4%) had a diagnosis of CD confirmed vs none of the 488 children in the EIG (P = .02, risk difference between the groups using the bootstrap, 1.4%; 95% CI, 0.6%-2.6%).
Conclusions and Relevance
In this analysis of infants in the EAT Study, the introduction of gluten from age 4 months was associated with reduced CD prevalence. These results suggest that early high-dose consumption of gluten should be considered as a strategy to prevent CD in future studies.
Trial Registration
isrctn.org Identifier: ISRCTN14254740
This prespecified analysis of a randomized clinical trial compares the development of celiac disease in infants with gluten introduced to their diet before vs after age 6 months.
Introduction
In 2008, the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) issued guidelines recommending the introduction of wheat into infants’ diets between the ages of 4 and 6 months while the infant is still being breastfed for the prevention of celiac disease (CD).1 This recommendation was based on observational studies suggesting that both early (<4 months) and late (>6 months) introduction of wheat was associated with an increased risk of CD.2
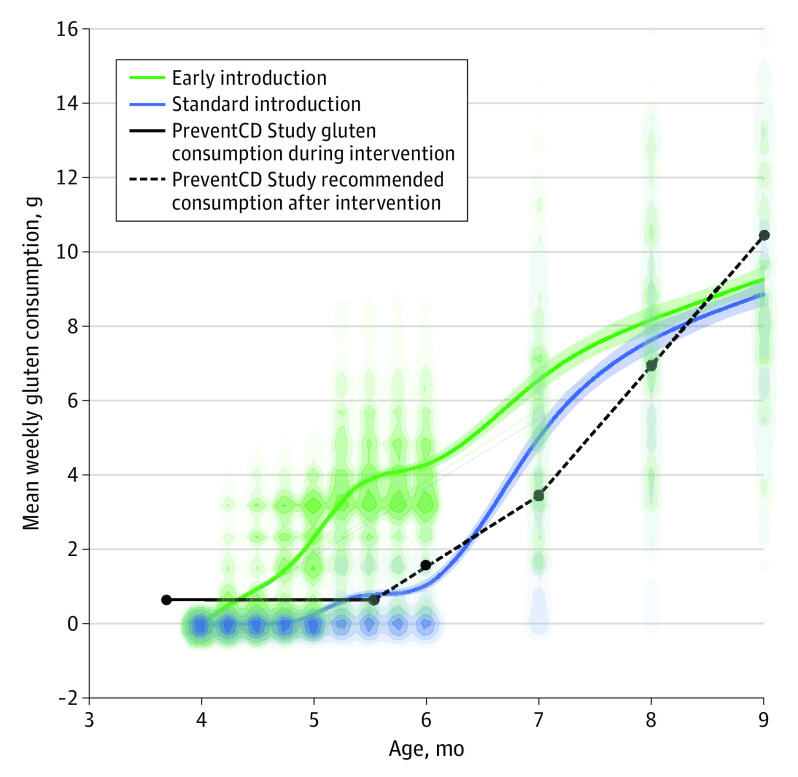
Subsequent to the studies being reported, 4 randomized clinical trials (RCTs) were undertaken to investigate the timing and dose of gluten introduction in preventing CD.3,4,5,6 However, only 1 of the 4 RCTs (PreventCD) introduced wheat before age 6 months at a low daily dose of gluten (100 mg) from age 16 weeks for 8 weeks in comparison with no gluten during this time.3 After the intervention period, participants in both groups were advised to introduce gluten gradually according to standardized recommendations (250 mg/d at 6 months, 500 mg/d at 7 months, 1000 mg/d at 8 months, and 1500 mg/d at 9 months). All infants in this trial were at a high risk of CD. No significant difference in the prevalence of CD at age 3 years was found between the gluten and placebo groups (overall CD prevalence, 5.2%).3 Subsequent systematic reviews and revised guidelines concluded that there was no consistent evidence for an association between timing of gluten introduction and CD.7,8,9,10
The Enquiring About Tolerance (EAT) Study was an open-label RCT of a dietary intervention for the prevention of food allergy that introduced 6 allergenic foods to infants’ diets from age 4 months (wheat from 4 months) alongside breastfeeding (early introduction group [EIG]) vs the continuation of exclusive breastfeeding and avoidance of allergenic foods until age 6 months (standard introduction group [SIG]).11 The EAT Study represented an opportunity to look at the early vs later introduction of high-dose gluten in a general population cohort using a randomized study design. The EAT Study introduced gluten in the key period during which the original observational studies had suggested may confer a protective effect (ie, between ages 4 and 6 months). Furthermore, the recommended dose of gluten was 3.2 g/wk from age 16 weeks, which is a quantity substantially higher than other early-introduction RCTs in which the recommended introduction of gluten at this age was 0.7 g/wk. Despite previous RCTs finding no association between early introduction of gluten and CD and other risk factors playing an important role in disease development (eg, family history of CD, gut colonization, and common infections during infancy), there is still a plausible mechanism for early introduction of gluten as a prevention strategy and, as has been shown with allergic disease, a danger that introducing too small a quantity may sensitize the child to that food while those with a genetic predisposition may need regular, larger doses of the food to induce tolerance.12,13
Methods
A total of 1303 infants from the general population throughout England and Wales were enrolled in the EAT Study between November 2, 2009, and July 30, 2012. For the present study, samples were collected from November 1, 2012, to March 31, 2015, and data for the present study were analyzed from April 25, 2017, to September 17, 2018. All infants were exclusively breastfed until age 13 weeks, at which point they were randomized to consume either 6 allergenic foods (cow's milk, hen's egg, peanut, sesame, cod fish, and wheat) in addition to breast milk or to continue to be exclusively breastfed until approximately age 6 months as per UK government guidelines.14
Ethical approval for the EAT Study was provided by St Thomas’ Hospital Research Ethics Committee, London, UK, and written informed consent was obtained from the parents of all children enrolled in the study. Financial compensation for travel expenses was provided. The trial protocol is available in Supplement 1. This study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline for randomized clinical trials.
Wheat was 1 of the 6 allergenic foods introduced to the EIG. The recommended weekly dose of wheat for a child in the intervention arm was 4 g of wheat protein given as 2 wheat-based cereal biscuits (eg, Weetabix) or equivalent throughout the week.11 Using the calculation that 80% of wheat protein is gluten, this dose is equivalent to a gluten dose of approximately 3.2 g/wk or 500 mg/d. This amount was the recommended minimum quantity; no upper limit was put on wheat consumption. The recommended quantity of gluten was based on the expected amount of wheat protein needed to induce oral tolerance and prevent immunoglobulin E–mediated wheat allergy because this result was the primary aim of the trial.15
Families completed contemporaneous questionnaires on a monthly basis through age 1 year and then every 3 months to age 3 years, which included a food frequency questionnaire allowing wheat consumption to be monitored. These questionnaires also documented a full range of health and behavioral outcomes and symptom reporting, including gastrointestinal symptoms (diarrhea, constipation, and vomiting) and parent-perceived adverse reactions to any foods. Clinic visits were carried out at enrollment, age 12 months, and age 3 years and included detailed anthropometric assessment, including weight, length/height, and body mass index.
Both study groups were followed up with the same schedule for clinical visits, and both received a monthly questionnaire assessing, among other things, wheat consumption. For the primary outcome of the EAT Study (ie, immunoglobulin E–mediated food allergy), we wished to know the exact extent to which the EIG had adhered to the weekly dose of allergenic food protein that we had recommended; hence, parents of children in this group were additionally asked to complete a section that assessed their adherence to having the child consume the recommended weekly dose of each of the 6 early introduction foods, which also allowed us to monitor adherence to the intervention. As a result, we obtained weekly consumption data from the EIG and monthly consumption data from the SIG. Although this greater amount of data potentially gives more detail for the EIG, it is appropriate given the lack of wheat consumption in the SIG who were being asked to avoid all food and exclusively breastfeed until the infant was aged 6 months (93% of the SIG adhered to the study protocol).
Serum antitransglutaminase type 2 (anti-TG2) antibodies were tested at 3 years. This testing for CD antibodies was carried out owing to concern regarding a potential increase in the risk of CD in the EIG owing to the ESPGHAN recommendation to introduce gluten in small amounts and the decision to introduce larger amounts in the EAT Study for induction of tolerance and wheat allergy prevention. Therefore, general practitioners of any children with antibody levels in excess of 20 IU/L received a letter asking them to refer the participant to a pediatric gastroenterologist of their choosing for additional investigation. Results of the subsequent testing were communicated to the study team via the participant's parents or general practitioner. Local diagnostic procedures varied but adhered to ESPGHAN guidelines (Table 1).16 A diagnosis of CD was based on ESPGHAN guidelines. We confirmed frequent intake of wheat in 99.2% of children before antibody testing. Parents of those not consuming sufficient amounts of wheat were advised to increase intake for at least 6 weeks before testing was carried out.
Table 1. Diagnostic Characteristics of Children With Increased Anti-TG2 Antibody Results Referred for Further Investigation.
| Patient | Anti-TG2 antibody results | HLA testing | EMA-positive | Biopsy | Family history | Symptoms | Symptoms improved with gluten-free diet |
|---|---|---|---|---|---|---|---|
| 1 | >128 IU/L | Not performed | Yes | Positive | No | GI symptoms,a fatigueb | Yes |
| 2 | >128 IU/L | Positive for HLA-DQ2 or HLA-DQ8 | Yes | Not performed | None confirmed but suspected by parents | GI symptomsa | Yes |
| 3 | >128 IU/L | Positive for HLA-DQ2 or HLA-DQ8 | Yes | Not performed | No | Slow growth; 25th percentile for weight and height improving to 50th and 75th, respectively, with gluten-free diet | Yes |
| 4 | >128 IU/L | Not performed | Yes | Positive | No | GI symptoms,a fatigueb | Yes |
| 5 | 103 IU/L | Positive for HLA-DQ2 or HLA-DQ8 | Yes | Not performed | No | GI symptoms,a fatigueb | Yes |
| 6 | >128 IU/L | Positive for HLA-DQ2 or HLA-DQ8 | Yes | Not performed | Yes (sibling) | None | NA |
| 7 | >128 IU/L | Positive for HLA-DQ2 or HLA-DQ8 | Yes | Not performed | Yes (grandmother) | GI symptomsa | Yes |
| 8 | 28 (Negative on retesting) | Not performed | No | Not performed | No | No | NA |
| 9 | 87 (7 on Retesting) | Not performed | Yes | Negative | No | No | NA |
Abbreviations: anti-TG2, antitransglutaminase type 2; EMA, endomysial antibody; GI, gastrointestinal; HLA, human leukocyte antigen; NA, not available.
Gastrointestinal symptoms reported included abdominal pain, bloated abdomen, constipation, and diarrhea.
Fatigue symptoms reported included constant tiredness, exhaustion, and poor behavior due to tiredness.
The quantity of gluten consumed was calculated from the monthly food frequency questionnaires and a 5-day food diary. The 5-day food diary was based on a standardized design for assessing diet in birth cohort studies.17 Similar diaries were used by the Avon Longitudinal Study of Parents and Children18 group and the Cambridge Baby Growth Study.19 The diaries were completed on 3 occasions during the study and were entered in dietary analysis software by our team of pediatric dietitians. In this analysis, the food diaries were used to assign appropriate portion sizes before the monthly questionnaires were completed to calculate consumption quantities. The food diaries were validated against our food frequency questionnaire and found to agree with the answers given in the questionnaire.20
Statistical Analysis
Analyses were undertaken using Stata, version 15 (StataCorp LLC) and JMP Pro 15 (SAS Institute Inc). Comparisons between the prevalence of CD in the EIG and SIG were made using a Fisher exact test to account for the small numbers of participants with CD. Bootstrap resampling was also implemented to produce 95% CIs of the risk difference using 2000 replicates as implemented in JMP Pro 15. When testing proportions between the randomized groups with expected cell counts greater than 5, Pearson χ2 tests were used. Mean gluten consumption over the study visits was fit using a cubic spline to allow for nonlinear trends, and 95% CIs were calculated using bootstrap resampling. Complete case analyses were conducted because data were assumed to be missing at random; no imputation was performed for any analyses. Significance testing was at the 2-sided α = .05 level of significance, and randomized group comparisons were unpaired measurements.
Results
A total of 1004 children were tested for anti-TG2 antibodies; of these, 77% of those who initially enrolled in the trial and 84% of those who attended the follow-up visit at age 3 years had sufficient blood samples available for testing (Figure 1). Enrollment characteristics have been reported elsewhere.11 Over 97% of those tested for anti-TG2 antibodies at age 3 years were consuming wheat at least daily for 6 weeks before testing. Of the 33 not consuming wheat daily (19 in the SIG and 11 in the EIG), only 3 children (2 SIG and 1 EIG) were not consuming any wheat at the time of testing.
Figure 1. Flow Diagram of Celiac Testing in 1303 Children Enrolled in the Enquiring About Tolerance (EAT) Study.
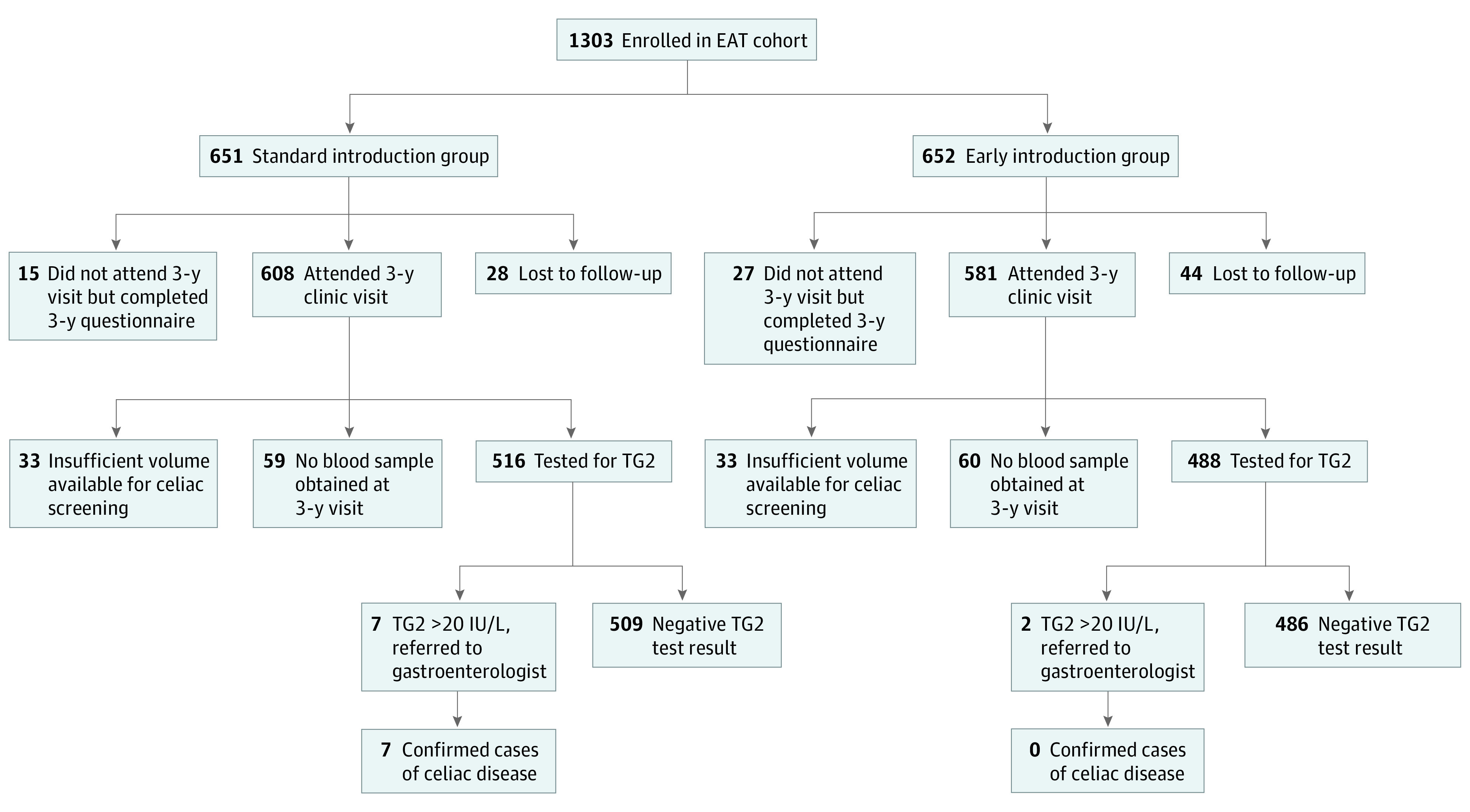
TG2 indicates antitransglutaminase 2 antibody.
Cohort Characteristics
The enrollment characteristics of the 1004 participants who were tested for anti-TG2 antibodies at the 36-month clinic visit did not differ substantially from those in the wider EAT Study cohort, which has been shown previously to be representative of the general UK population. A total of 514 children were male (51.2%) and 490 children (48.8%) were female (eTable in Supplement 2). Parents who reported a history of their child reacting to any foods were significantly more likely to attend the 36-month clinic visit and therefore receive testing for CD antibodies than those who reported no symptoms (25.9% of 1176 attending vs 16.0% of 100 not attending, P = .04). Parent reports of any gastrointestinal symptoms (diarrhea, constipation, and/or vomiting) were available for 224 of 299 children who did not receive testing for CD at age 3 years, and, overall, there was no significant difference in the prevalence of gastrointestinal symptoms reported at age 3 years by those who had testing for the antibodies (315/1004 [31.4%]) and those who did not (76/224 [33.9%]) (P = .56). Among those who did not receive testing for CD but for whom gastrointestinal symptom data were available (n = 224), gastrointestinal symptoms were reported by similar numbers of SIG (36/104 [34.6%]) and EIG (40/120 [33.3%]) participants.
Gluten Consumption
The median age at gluten introduction in the EIG was 4 months (range, 4-33 months) and in the SIG was 7 months (range, 5-21 months) (Wilcoxon rank sum z = 21.84, P < .001). Between ages 4 and 5 months, 12 children (2.3%) of the SIG had begun receiving gluten-containing foods compared with 340 children (69.5%) of the EIG. Among those consuming gluten between ages 4 and 5 months, children in the SIG were consuming a mean (SD) of 0.08 (1.00) g/wk of gluten in comparison with a higher mean of 1.3 (1.54) g/wk of gluten in the EIG (Figure 2). Between ages 5 and 6 months, a mean (SD) of 0.9 (2.05) g/wk of gluten was being consumed by the SIG (37.6% of this group was consuming gluten by age 6 months) and 4.03 g/w (2.40) of gluten by the EIG, among whom 86.7% were consuming gluten-containing foods. Between ages 4 and 6 months, the mean (SD) gluten consumption was 0.49 (1.40) g/wk in the SIG and 2.66 (1.85) g/wk in the EIG (P < .001) (Figure 2).
Figure 2. Gluten Consumption in the Enquiring About Tolerance Study Standard Introduction Group and Early Introduction Group With Reference to the PreventCD Study Gluten Consumption.
After age 6 months, consumption of gluten increased in both groups; at age 7 months, the mean gluten consumption was 5.13 (4.08) g/wk in the SIG and 6.3 (3.68) g/wk in the EIG. At age 8 months, the mean gluten consumption was 7.67 (4.38) g/wk in the SIG and 8.21 (3.76) g/wk in the EIG but remained different until age 9 months when similar volumes of gluten were being consumed by children in both groups (mean [SD] volume: SIG, 8.6 [4.16] g/wk and EIG, 8.8 [3.98] g/wk) (Figure 2).
Adherence to the recommendation for exclusive breastfeeding in the SIG until age 6 months was high: 558 participants (92.1%) adhered to the protocol. Although the early introduction of solid foods prevented exclusive breastfeeding beyond age 4 months in the EIG, 96.8% of this group were still being breastfed, alongside solid food consumption, at age 6 months.
Celiac Disease Diagnosis
Nine children (7 in the SIG and 2 in the EIG) had anti-TG2 antibody levels greater than 20 IU/L and were referred for further investigation. Seven of 516 children (1.4%) tested from the SIG had a diagnosis of CD confirmed by a pediatric gastroenterologist in comparison with none of the 488 children tested in the EIG (P = .02 using the Fisher exact test); the risk difference between the groups using the bootstrap was 1.4% (95% CI, 0.6%-2.6%). Of children diagnosed with CD, all had anti-TG2 antibody levels greater than or equal to 10 times above the reference range and were positive for endomysial antibodies. Five children additionally had human leukocyte antigen (HLA) typing, and all 5 were positive for HLA-DQ2 or HLA-DQ8. The 2 children with no HLA testing performed had biopsies, with the results showing classic signs of CD. Six of 7 children developed gastrointestinal symptoms directly before the diagnosis, and all 6 experienced an improvement in symptoms once a gluten-free diet was introduced (Table 1).
Discussion
The results from the EAT Study cohort imply an effect of early gluten introduction on the prevalence of CD at age 3 years. Four other RCTs did not find an association between the timing of gluten introduction and prevalence of CD (Table 2).3,4,5,6 For 3 of these RCTs, gluten consumption began after age 6 months. The PreventCD study introduced gluten before age 6 months but in very small quantities, equating to approximately 10% of an average portion of wheat (1/10 of a slice of bread) in an infant aged 6 months.3
Table 2. Summary of Gluten Introduction in Prevention RCTs.
| Study | No. | Population | Age at introduction of gluten in intervention vs control groups, mo | Weekly quantity of gluten recommended during intervention period, g | Weekly volume of gluten consumed during intervention period |
|---|---|---|---|---|---|
| PreventCD3 | 944 | High risk (HLA-DQ or HLA-DQ8 positive) | 4-6 vs >6 | 0.7 | No set quantity recorded; 416/475 received at least 0.53 g/wk |
| BABYDIET4 | 150 | First-degree relative with type 1 diabetes and a risk HLA genotype | 6 vs 12 | No set quantity stipulated | No set quantity recorded |
| CELIPREV5 | 707 | First-degree relative with CD | 6 vs 12 | No set quantity stipulated | No set quantity recorded; mean, 3.2 g/d at age 9 mo |
| EAT12 | 1004 | General population | 4-6 vs >6 | 3.2 | 2.89 |
Abbreviations: CD, celiac disease; CELIPREV, the Risk of Celiac Disease and Age at Gluten Introduction study; EAT, Enquiring About Tolerance; HLA, human leukocyte antigen; RCTs, randomized clinical trials.
The EAT Study differs in comparison with these other trials because gluten was introduced from age 4 months and in larger quantities, which is more representative of an age-appropriate portion size. After age 6 months, gluten consumption in the EAT Study continued to increase, with the EIG consuming a mean of 6.3 g/wk at age 7 months in comparison with the 3.5-g/wk amount recommended for the PreventCD cohort at that age. The CELIPREV trial, conducted by Lionetti et al,5 introduced large quantities of gluten (participants were consuming 3.2 g/d of gluten at age 9 months), but gluten was not introduced before age 6 months (Table 2). It may therefore be that both an early introduction and larger quantity of gluten are needed to reduce the prevalence of CD in childhood.
Although CD was a prespecified end point of the trial, the EAT Study was not designed to investigate the effect of early gluten introduction on CD prevalence. With a cohort of 1004 children and an age-specific population prevalence of CD estimated at approximately 0.3%, we were likely to see only a few cases of CD and probably be underpowered to detect any between-group differences. It was therefore unexpected that we had no confirmed cases of CD in the EIG compared with the 1.4% prevalence in the SIG. This larger-than-expected difference between groups and the larger-than-expected prevalence in the SIG contributed to a P value that was lower than anticipated. The unexpected statistically significant difference may be the result of delaying introduction of wheat until after age 6 months, or it may be the result of a type I error.
Although the small number of infants diagnosed with CD limits our ability to further investigate other factors that may have been associated with development of CD, the randomized nature of the cohort and the apparent lack of bias in the population tested should decrease the likelihood of potential confounders. It is possible that a disproportionate amount of CD was present in the EIG participants who did not receive CD screening at age 3 years. While it is not possible to rule out bias caused by incomplete testing of the cohort, our results and study design make the introduction of bias unlikely for several reasons. First, at age 3 years, 43 SIG children and 71 EIG children did not attend a final clinic visit, but reasons for withdrawal (listed in detail elsewhere)14 predominantly included factors related to family circumstances, emigration, loss of contact with the family, and concerns about the study procedures. Loss to follow-up owing to health concerns was not a reason given for withdrawal, and children with a history of any food reactions were more likely to attend a clinic visit. Second, the questionnaire data we had on those not tested showed no substantial difference in both the prevalence of gastrointestinal symptoms at age 3 years and reporting of food-related reactions, making it unlikely that undiagnosed CD was disproportionally present in those not tested. In addition, the prevalence of food reactions and gastrointestinal tract symptoms in those not screened for CD did not differ substantially between study groups, further reducing the likelihood of undiagnosed CD being disproportionately present in the EIG. It is possible that symptoms may not have presented yet, and asymptomatic CD is common at this age, but the prevalence of asymptomatic CD is unlikely to be disproportionately present in the EIG owing to the randomized nature of the cohort. While we cannot exclude the possibility that hidden bias could explain the different prevalence of CD in the 2 study groups, this possibility is less likely given the above observations. Onset of CD in children older than 3 years is likely, and it is possible that the early introduction of gluten delayed presentation of CD rather than prevented it. Longer follow-up of this cohort is underway, with CD being investigated again in children aged 7 to 10 years.
Previous observational studies identified infant feeding practices as playing a role in the increasing incidence of CD in Sweden in the 1980s but could not isolate the role of individual factors.21 In contrast, in the UK in the 1980s, the later introduction of gluten-containing foods and more prolonged breastfeeding were associated with a decline in CD.22 Observational methods and conflicting results make these early studies of gluten introduction inconclusive. All children in the EAT Study were exclusively breastfed until study enrollment, and breastfeeding rates were too high for subgroup analyses in this area.
Limitations
A potential limitation of our trial is that CD diagnoses were made at different clinical centers and biopsies were undertaken in only a small number of the cases. However, biopsy is no longer regarded as necessary to confirm a diagnosis of CD, and all diagnoses were made in accordance with current ESPGHAN guidelines, which have been recently updated with further guidance on non–biopsy-based diagnoses.16,23,24,25
Conclusions
The results of this analysis suggest that it may have been premature to discount the effect of age of introduction of gluten on the development of CD. ESPGHAN also currently recommends the introduction of low doses of gluten initially despite limited evidence to support this recommendation,10 and the results from the EAT Study suggest that a higher dose may be an important prevention strategy. Our study raises the question as to whether the PreventCD study would have obtained different results if infants had consumed greater quantities of gluten, more similar to those consumed by families in the observational literature from which the early introduction hypothesis originated. The results of the present study emphasize the importance of conducting new RCTs to address the question of whether early introduction of high-dose gluten is an effective strategy for prevention of CD.
Trial Protocol
eTable. Baseline Characteristics of the Cohort
Data Sharing Statement
References
- 1.Agostoni C, Decsi T, Fewtrell M, et al. ; ESPGHAN Committee on Nutrition . Complementary feeding: a commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2008;46(1):99-110. doi: 10.1097/01.mpg.0000304464.60788.bd [DOI] [PubMed] [Google Scholar]
- 2.Norris JM, Barriga K, Hoffenberg EJ, et al. . Risk of celiac disease autoimmunity and timing of gluten introduction in the diet of infants at increased risk of disease. JAMA. 2005;293(19):2343-2351. doi: 10.1001/jama.293.19.2343 [DOI] [PubMed] [Google Scholar]
- 3.Vriezinga SL, Auricchio R, Bravi E, et al. . Randomized feeding intervention in infants at high risk for celiac disease. N Engl J Med. 2014;371(14):1304-1315. doi: 10.1056/NEJMoa1404172 [DOI] [PubMed] [Google Scholar]
- 4.Beyerlein A, Chmiel R, Hummel S, Winkler C, Bonifacio E, Ziegler AG. Timing of gluten introduction and islet autoimmunity in young children: updated results from the BABYDIET study. Diabetes Care. 2014;37(9):e194-e195. doi: 10.2337/dc14-1208 [DOI] [PubMed] [Google Scholar]
- 5.Lionetti E, Castellaneta S, Francavilla R, et al. ; SIGENP (Italian Society of Pediatric Gastroenterology, Hepatology, and Nutrition) Working Group on Weaning and CD Risk . Introduction of gluten, HLA status, and the risk of celiac disease in children. N Engl J Med. 2014;371(14):1295-1303. doi: 10.1056/NEJMoa1400697 [DOI] [PubMed] [Google Scholar]
- 6.Sellitto M, Bai G, Serena G, et al. . Proof of concept of microbiome-metabolome analysis and delayed gluten exposure on celiac disease autoimmunity in genetically at-risk infants. PLoS One. 2012;7(3):e33387. doi: 10.1371/journal.pone.0033387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ierodiakonou D, Garcia-Larsen V, Logan A, et al. . Timing of allergenic food introduction to the infant diet and risk of allergic or autoimmune disease: a systematic review and meta-analysis. JAMA. 2016;316(11):1181-1192. doi: 10.1001/jama.2016.12623 [DOI] [PubMed] [Google Scholar]
- 8.Szajewska H, Chmielewska A, Pieścik-Lech M, et al. ; PREVENTCD Study Group . Systematic review: early infant feeding and the prevention of coeliac disease. Aliment Pharmacol Ther. 2012;36(7):607-618. doi: 10.1111/apt.12023 [DOI] [PubMed] [Google Scholar]
- 9.Pinto-Sánchez MI, Verdu EF, Liu E, et al. . Gluten introduction to infant feeding and risk of celiac disease: systematic review and meta-analysis. J Pediatr. 2016;168:132-43.e3. doi: 10.1016/j.jpeds.2015.09.032 [DOI] [PubMed] [Google Scholar]
- 10.Szajewska H, Shamir R, Mearin L, et al. . Gluten introduction and the risk of coeliac disease: a position paper by the European Society for Paediatric Gastroenterology, Hepatology and Nutrition. J Pediatric Gastroenterol Nutr. 2016;62(3):507-513. doi:10.1097/MPG.0000000000001105 doi: 10.1097/MPG.0000000000001105 [DOI] [PubMed] [Google Scholar]
- 11.Perkin MR, Logan K, Marrs T, et al. ; EAT Study Team . Enquiring About Tolerance (EAT) study: feasibility of an early allergenic food introduction regimen. J Allergy Clin Immunol. 2016;137(5):1477-1486.e8. doi: 10.1016/j.jaci.2015.12.1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kahrs CR, Chuda K, Tapia G, et al. . Enterovirus as trigger of coeliac disease: nested case-control study within prospective birth cohort. BMJ. 2019;364:l231. doi: 10.1136/bmj.l231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prescott SL, Smith P, Tang M, et al. . The importance of early complementary feeding in the development of oral tolerance: concerns and controversies. Pediatr Allergy Immunol. 2008;19(5):375-380. doi: 10.1111/j.1399-3038.2008.00718.x [DOI] [PubMed] [Google Scholar]
- 14.Perkin MR, Logan K, Tseng A, et al. ; EAT Study Team . Randomized trial of introduction of allergenic foods in breast-fed infants. N Engl J Med. 2016;374(18):1733-1743. doi: 10.1056/NEJMoa1514210 [DOI] [PubMed] [Google Scholar]
- 15.Du Toit G, Katz Y, Sasieni P, et al. . Early consumption of peanuts in infancy is associated with a low prevalence of peanut allergy. J Allergy Clin Immunol. 2008;122(5):984-991. doi: 10.1016/j.jaci.2008.08.039 [DOI] [PubMed] [Google Scholar]
- 16.Husby S, Koletzko S, Korponay-Szabó IR, et al. ; ESPGHAN Working Group on Coeliac Disease Diagnosis; ESPGHAN Gastroenterology Committee; European Society for Pediatric Gastroenterology, Hepatology, and Nutrition . European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. J Pediatr Gastroenterol Nutr. 2012;54(1):136-160. doi: 10.1097/MPG.0b013e31821a23d0 [DOI] [PubMed] [Google Scholar]
- 17.Emmett P. Assessing diet in longitudinal birth cohort studies. Paediatr Perinat Epidemiol. 2009;23(suppl 1):154-173. doi: 10.1111/j.1365-3016.2009.01015.x [DOI] [PubMed] [Google Scholar]
- 18.Emmett P. Dietary assessment in the Avon Longitudinal Study of Parents and Children. Eur J Clin Nutr. 2009;63(suppl 1):S38-S44. doi: 10.1038/ejcn.2008.63 [DOI] [PubMed] [Google Scholar]
- 19.Prentice P, Acerini CL, Eleftheriou A, Hughes IA, Ong KK, Dunger DB. Cohort profile: the Cambridge Baby Growth Study (CBGS). Int J Epidemiol. 2016;45(1). doi: 10.1093/ije/dyv318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vaugan S. Validation of an infant Food Frequency Questionnaire. MSc dissertation. Imperial College London; UK. [Google Scholar]
- 21.Ivarsson A, Persson LA, Nyström L, et al. . Epidemic of coeliac disease in Swedish children. Acta Paediatr. 2000;89(2):165-171. doi: 10.1111/j.1651-2227.2000.tb01210.x [DOI] [PubMed] [Google Scholar]
- 22.Challacombe DN, Mecrow IK, Elliott K, Clarke FJ, Wheeler EE. Changing infant feeding practices and declining incidence of coeliac disease in West Somerset. Arch Dis Child. 1997;77(3):206-209. doi: 10.1136/adc.77.3.206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Husby S, Koletzko S, Korponay-Szabó I, et al. . European Society for Paediatric Gastroenterology, Hepatology and Nutrition guidelines for diagnosing coeliac disease 2020. J Pediatr Gastroenterol Nutr. 2020;70(1):141-156. doi: 10.1097/MPG.0000000000002497 [DOI] [PubMed] [Google Scholar]
- 24.Werkstetter KJ, Korponay-Szabó IR, Popp A, et al. ; ProCeDE Study Group . Accuracy in diagnosis of celiac disease without biopsies in clinical practice. Gastroenterology. 2017;153(4):924-935. doi: 10.1053/j.gastro.2017.06.002 [DOI] [PubMed] [Google Scholar]
- 25.Liu E, Lee HS, Aronsson CA, et al. ; TEDDY Study Group . Risk of pediatric celiac disease according to HLA haplotype and country. N Engl J Med. 2014;371(1):42-49. doi: 10.1056/NEJMoa1313977 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eTable. Baseline Characteristics of the Cohort
Data Sharing Statement