Abstract
Background:
Prevention of pre-invasive cervical lesions is an important benefit of HPV vaccines, but demonstrating impact on these lesions is impeded by changes in cervical cancer screening. Monitoring vaccine-types associated with lesions can help distinguish vaccine impact from screening effects. We examined trends in prevalence of HPV 16/18 types detected in cervical intraepithelial neoplasia 2,3, and adenocarcinoma in situ (CIN2+) among women diagnosed with CIN2+ from 2008 to 2012 by vaccination status. We estimated vaccine effectiveness against HPV 16/18-attributable CIN2+ among women who received ≥1 dose by increasing time intervals between date of first vaccination and the screening test that led to detection of CIN2+ lesion.
Methods:
Data are from a population-based sentinel surveillance system to monitor HPV vaccine impact on type-specific CIN2+ among adult female residents of five catchment areas in California, Connecticut, New York, Oregon, and Tennessee. Vaccination and cervical cancer screening information was retrieved. Archived diagnostic specimens were obtained from reporting laboratories for HPV DNA typing.
Results:
From 2008 to 2012, prevalence of HPV 16/18 in CIN2+ lesions statistically significantly decreased from 53.6% to 28.4% among women who received at least one dose (Ptrend <.001) but not among unvaccinated women (57.1% vs 52.5%; Ptrend = .08) or women with unknown vaccination status (55.0% vs 50.5%; Ptrend = .71). Estimated vaccine effectiveness for prevention of HPV 16/18-attributable CIN2+ was 21% (95% CI: 1–37), 49% (95% CI: 28–64), and 72% (95% CI: 45–86) in women who initiated vaccination 25–36 months, 37–48 months, and >48 months prior to the screening test that led to CIN2+ diagnosis.
Conclusions:
Population-based data from the United States indicate significant reductions in CIN2+ lesions attributable to types targeted by the vaccines and increasing HPV vaccine effectiveness with increasing interval between first vaccination and earliest detection of cervical disease.
Keywords: Human papillomavirus, HPV, Vaccine, Cervical intraepithelial neoplasia, CIN, High grade cervical lesion
1. Introduction
The discovery that persistent infection with certain human papillomavirus (HPV) types is causally associated with cervical cancer, and the subsequent development of vaccines to prevent HPV-attributable cancers are among the most important milestones in science and medicine [1,2]. Two HPV vaccines directed against HPV 16 and 18, types that cause 70% of invasive and 50% of pre-invasive cervical lesions worldwide, are currently available [3,4]. In clinical trials, both HPV vaccines were highly efficacious against vaccine type-associated cervical intraepithelial neoplasia grades 2 and 3 and adenocarcinoma in situ (CIN2+), pre-invasive lesions that may progress to cervical cancer if left untreated [5,6].
The real-world benefits of vaccination against associated cancers may not be evident for decades given the slow progression from infection to invasive disease, but population impact against earlier outcomes has already been demonstrated in numerous settings worldwide [7–12]. In the United States, routine HPV vaccination has been recommended since June 2006 for females aged 11 or 12 years, through age 26 years in those not previously vaccinated [13]. However, coverage remains suboptimal. In 2013, fewer than 57% of girls aged 13–17 years had received at least one dose of quadrivalent HPV vaccine, which accounts for about 99% of all HPV vaccines distributed in the United States [14], and only 38% had completed the 3-dose series [15]; coverage in the older age group has been even lower [16]. Despite low coverage, significant reductions in vaccine-type HPV prevalence have been shown in young females [17].
Measuring vaccine impact on screening-detected cervical lesions in the United States is more challenging given incomplete reporting of adolescent vaccination to state-based immunization registries, lack of national screening registries, and changing screening recommendations. Over the past decade, the recommended age for initiating cervical cancer screening has been raised to 21 years and screening intervals have been increased, particularly if HPV-based co-testing is used [18]. Monitoring vaccine-types associated with lesions can help distinguish the impact of vaccination from the effects resulting from changing screening practices.
We previously reported preliminary results in the first few years post-vaccine introduction on HPV vaccine effectiveness against HPV 16/18-type CIN2+, pre-invasive lesions that include a continuum of histologic lesions with increasing severity [19]. In this paper, we extend the analysis to a longer time period in the vaccine era and larger number of cases to produce estimates of vaccine effectiveness on HPV 16/18-attributable CIN2+ as well as on a subset of highest grade lesions (CIN3/AIS), which are most likely to progress to cervical cancer. Additionally, we examined temporal trends in the prevalence of HPV 16/18-related CIN2+ after vaccine introduction in the United States.
2. Materials and methods
Data were obtained from the HPV-IMPACT Project, a population-based surveillance system for monitoring HPV vaccine impact on type-specific CIN2+ among females aged ≥18 years residing in catchment areas in California, Connecticut, New York, Oregon, and Tennessee [20]. The total population of females aged 18 years and older ranges from 230,000 to 330,000 in each participating site according to the 2010 U.S. Census data. This project was reviewed by the US Centers for Disease Control, Oregon Health Authority Public Health Division, and the institutional review boards of Yale University, University of Rochester, Unity Health System, and Rochester General Hospital and determined to be exempt from institutional review board approval as the activity constitutes routine disease surveillance activity for disease control program and policy purposes. The project was approved by the University of California Berkeley, University of California San Francisco, Alameda Health Systems, and State of California Committee for Protection of Human Subjects. Informed consent was not required from any reviewing/approving institution. All patient records and information was anonymized and de-identified prior to analysis.
From 2008 to 2012, local and commercial laboratories serving the catchment areas reported histopathologically confirmed cases of CIN2+ diagnosed in adult (≥18 years) female residents of the areas. Cases were identified through electronic health record searches or manual chart reviews using all classification systems and terminology used for CIN2+ during the monitoring period. Reported cases were stratified by histologic grade into CIN2, CIN2/3 (grade not discriminated), and CIN3/AIS categories for analysis. Reports on the same individual within 6 months of the initial diagnosis date were considered to be related, and the person was classified according to the highest grade diagnosis within that time. For women aged 18–39 years at diagnosis, HPV vaccination history and result and date of the screening test that led to CIN2+ diagnosis (“trigger test”) were investigated. In 2008 and 2009, laboratories were asked to submit specimens on all reported cases. However, in subsequent years, budgetary constraints necessitated that only a sample of specimens be requested from reporting laboratories. Specimens were randomly sampled within each CIN diagnosis stratum to maintain representativeness and to allow analysis of data by CIN grade. The proportion of specimens obtained in the 5-year time period decreased from 77% in 2008 to 40% in 2012. Women were classified as vaccinated if they received ≥1 dose prior to the trigger test, not vaccinated, and unknown status; women vaccinated on/after trigger test were categorized separately and excluded from the trend analysis. To estimate vaccine effectiveness, vaccinated women were classified into groups of increasing time interval between vaccine initiation (receipt of first dose) and trigger test, assuming that longer intervals increase the likelihood that vaccination occurred prior to infection with types responsible for the CIN2+ lesion.
Laboratory methods have been described previously [20]. Briefly, one block representative of the histologic lesion with the highest grade diagnosis was processed and presence of a high-grade lesion was histologically verified. DNA was extracted and tested with the Linear Array HPV Genotyping Assay (LA; Roche Diagnostics, Indianapolis, IN). Samples with inadequate or HPV negative LA results were retested with the INNO-LiPA HPV Genotyping Extra Assay (Innogenetics, Gent, Belgium). Samples negative for the genomic control probe and HPV in LA and INNO-LiPA were considered inadequate and excluded.
HPV 16/18 attribution was defined as detection of either type in a lesion, irrespective of presence of other types. Descriptive analyses included evaluation of differences in categorical and continuous demographic characteristics by vaccination status using χ2 test or Student’s t-test, respectively. The Cochran Armitage test was used to evaluate trends in HPV 16/18-attributable CIN2+ lesions by vaccination status. On a sub-set of women reported to HPV-IMPACT for whom vaccination status was known, vaccine effectiveness against CIN2+ was evaluated using the indirect cohort study design in which individuals with HPV 16/18-attributable CIN2+ are compared to those with lesions attributable to other HPV types [21]. Vaccine effectiveness against CIN2+ incidence was determined for the following vaccination and trigger test intervals: vaccinated on/after trigger test, vaccinated 0, 1–12, 13–24, 25–36, 37–48, and >48 months before trigger test. Vaccine effectiveness was estimated separately for the subset of women diagnosed with CIN3/AIS. Log binomial regression models were used to calculate unadjusted and adjusted prevalence ratios (PRs) and 95% confidence intervals (CIs). Covariates included race/ethnicity, insurance status, age at CIN2+ diagnosis, catchment area, year of diagnosis, and histologic grade (for CIN2+). Associations were considered significant if the P value was <.05 and those variables were retained in the main effects model. Confounding was assessed to ensure that no parameter estimate of significant variables changed by ≥30%. All pairwise interactions in the final model were examined, and were considered significant if the P value for the likelihood ratio test for the interaction term was <.05. Vaccine effectiveness was calculated as 100*(1 – adjusted PR (aPR)). SAS version 9.3 (SAS Institute, Cary, NC) was used for all analyses.
3. Results
From 2008 to 2012, 7346 women who were age-eligible for vaccination (aged ≤26 years in 2006, when HPV vaccine was first recommended in the United States) were reported to HPV-IMPACT. Specimens were tested for 4693 women, and valid HPV DNA results were obtained for 4678 (99.7%). HPV DNA was detected in 4575 (97.8%); 23.3% had ≥1 type detected. Among women with typing results, HPV vaccination status was determined for 2463 (52.7%); 1189 (25.4%) had received ≥1 dose and of those, 667 (56.1%) had completed the 3-dose series. Intervals between vaccine initiation and trigger test could be calculated for 993 women with both dates. Of these, 549 received ≥1 dose more than 30 days prior to their trigger test and were considered to be vaccinated (Fig. 1).
Fig. 1.
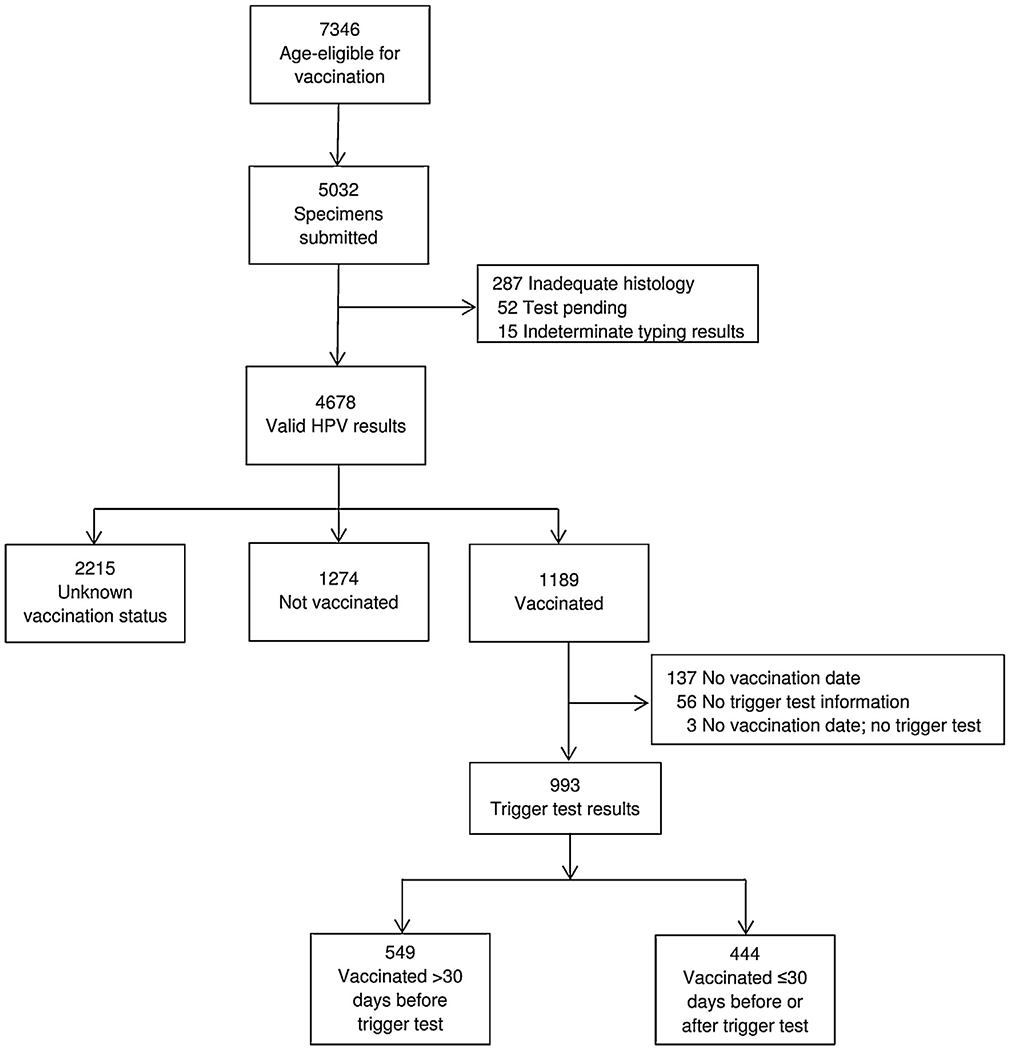
Flow chart of women studied from the HPV-IMPACT project.
Among the 4678 women with typing results, median age at diagnosis was 25 years; CIN2, CIN2/3, and CIN3/AIS accounted for 50.1%, 16.8%, and 33.1% of diagnoses, respectively. Clinical and demographic characteristics of women with typing results, stratified by vaccination status, are described in Table 1. The majority (58.0%) of vaccinated women had a CIN2 diagnosis, compared to 51.1% of unvaccinated women and 46.5% of those with unknown vaccination status. Median age at diagnosis was 23 years in vaccinated, 25 years in unvaccinated, and 26 years in women with unknown vaccination status. Among the 3826 (85.4%) women with known race/ethnicity, vaccinated women were 67.4% non-Hispanic (NH) white, 18.0% NH black, and 10.3% Hispanic, unvaccinated women were 66.1% NH white, 16.5% NH black, and 12.6% Hispanic, and women with unknown vaccination status were 58.8% NH white, 18.8% NH black, and 16.4% Hispanic. Median age at vaccine initiation was 22 years (interquartile range: 20–24).
Table 1.
Select characteristics of women diagnosed with C1N2+ by vaccination status, HPV-IMPACT, 2008–2012.
| Vaccinateda | Not vaccinated | Unknown | P | |
|---|---|---|---|---|
| Total, n | 993 | 1274 | 2215 | |
| Total by year, n (row %) | <.001 | |||
| 2008 | 259 (24.0) | 364 (33.8) | 455 (42.2) | |
| 2009 | 231 (22.7) | 299 (29.4) | 488 (47.9) | |
| 2010 | 213 (22.5) | 257 (26.6) | 496 (51.4) | |
| 2011 | 186 (20.5) | 255 (28.1) | 467 (51.4) | |
| 2012 | 104 (20.3) | 99 (19.3) | 309 (60.4) | |
| Diagnosis, n (col %) | <.001 | |||
| CIN2 | 576 (58.0) | 651 (51.1) | 1030 (46.5) | |
| CIN2/3 | 133 (13.4) | 196 (15.4) | 398 (18.0) | |
| CIN3 | 273 (27.5) | 411 (32.3) | 754 (34.0) | |
| AIS ± CIN | 11 (1.1) | 16 (1.3) | 33 (1.5) | |
| Age, median (IQR) | 23 (21–25) | 25 (23–28) | 26 (23–28) | <.001 |
| Race/ethnicity, n (col %) | <.001 | |||
| NH white | 591 (67.4) | 765 (66.1) | 1054 (58.8) | |
| NH black | 158 (18.0) | 191 (16.5) | 336 (18.8) | |
| Hispanic | 90 (10.3) | 146 (12.6) | 294 (16.4) | |
| Asian | 19 (2.2) | 35 (3.0) | 53 (3.0) | |
| Other | 19 (2.2) | 20 (1.7) | 55 (3.1) | |
| Missing | 116 | 117 | 423 | |
| Insurance, n (col %) | ||||
| Private | 583 (65.1) | 712 (61.9) | 1034 (56.6) | <.001 |
| Public | 250 (27.9) | 337 (29.3) | 615 (33.7) | |
| Uninsured | 21 (2.3) | 49 (4.3) | 69 (3.8) | |
| Other | 42 (4.7) | 53 (4.6) | 108 (5.9) | |
| Missing | 97 | 123 | 389 | |
Abbreviations: CIN2+, cervical intraepithelial neoplasia grades 2, 3 and adenocarcinoma in situ; AIS, adenocarcinoma in situ; NH, non-Hispanic; IQR, interquartile range.
Excludes 196 women without vaccination date and/or trigger test.
HPV 16/18-attributable CIN2+ decreased from 53.6% in 2008 to 28.4% in 2012 among women who received ≥1 vaccine dose (Ptrend< .001). There was no significant decline among unvaccinated women (57.1% vs, 52.5%; Ptrend= .08) or among women with unknown vaccination status (55.0% vs 50.5%; Ptrend= .71) during the same time period (Fig. 2). The proportion of CIN3/AIS lesions attributable to HPV 16/18 decreased from 76.0% in 2008 to 60.9% in 2012 (Ptrend= .06) in vaccinated women but did not change in women in the other 2 vaccination categories.
Fig. 2.
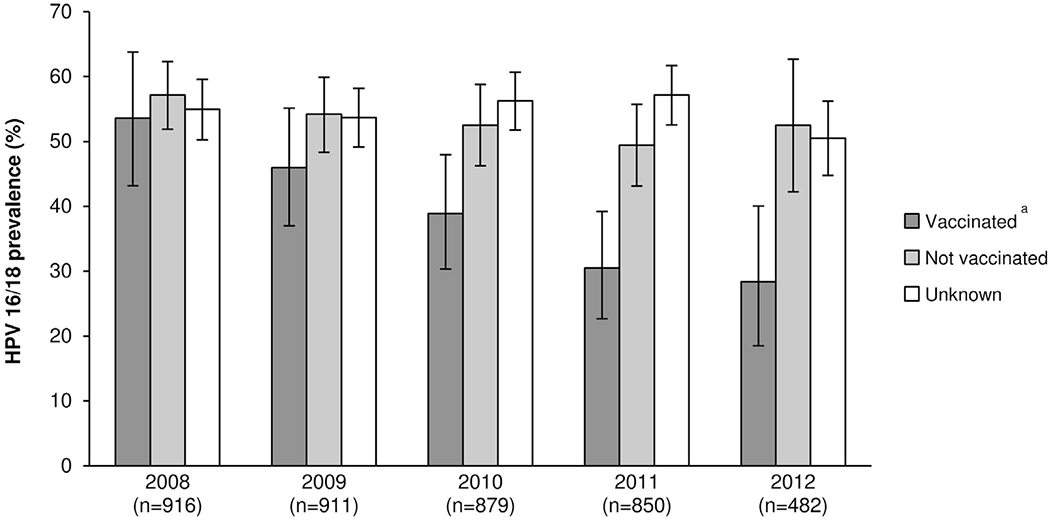
HPV 16/18 attribution to CIN2+ lesions among women age-eligible for vaccination, by year and vaccination status.
Abbreviations: CIN2+; cervical intraepithelial neoplasia grades 2; 3 and adenocarcinoma in situ (AIS).
aVaccinated includes women vaccinated >30 days before trigger test (screening test that led to CIN2+ diagnosis).
Compared to unvaccinated women, the proportion of CIN2+ attributable to HPV 16/18 was significantly lower in women who received ≥1 dose 25–36 months before their trigger test (aPR = 0.79; 95% CI: 0.63–0.99) and the percent attribution decreased with increasing intervals between vaccine initiation and trigger test (Table 2). Estimated vaccine effectiveness was 21% (95% CI: 1–37) in women with 25–36 months between vaccination and trigger test, 49% (95% CI: 28–64) in women with 37–48 months between vaccination and trigger test and 72% (95% CI: 45–86) in those who were vaccinated >48 months prior to the trigger test. Among women with the highest grade lesions (CIN3/AIS), HPV 16/18-attributable lesions were significantly lower in those who were vaccinated 37–48 months prior to their trigger test (aPR = 0.62; 95% CI: 0.44–0.93), an estimated vaccine effectiveness of 38% (95% CI: 7–59).
Table 2.
Vaccine effectiveness against type-specific CIN2+ and CIN3/AIS lesions.
| CIN2+ | n | % 16/18 | PR | 95% CI | aPRa | 95% CI |
|---|---|---|---|---|---|---|
| Not vaccinated | 1274 | 53.6 | Ref. | |||
| Vaccinated ≤30 days/after trigger test | 444 | 54.5 | 1.02 | 0.92–1.12 | 1.01 | 0.92–1.10 |
| Vaccinated before trigger test | ||||||
| 1–12 mos | 152 | 50.0 | 0.93 | 0.79–1.10 | 1.02 | 0.87–1.19 |
| 13–24 mos | 149 | 46.3 | 0.86 | 0.72–1.03 | 0.91 | 0.77–1.08 |
| 25–36 mos | 109 | 39.5 | 0.74 | 0.58–0.93 | 0.79 | 0.63–0.99 |
| 37–48 mos | 85 | 27.1 | 0.50 | 0.35–0.72 | 0.51 | 0.36–0.72 |
| >48 mos | 54 | 13.0 | 0.24 | 0.12–0.48 | 0.28 | 0.14–0.55 |
| CIN3/AIS | n | % 16/18 | PR | 95% CI | aPRb | 95% CI |
| Not vaccinated | 427 | 69.8 | Ref. | |||
| Vaccinated ≤30 days/after trigger test | 132 | 67.2 | 0.97 | 0.85–1.10 | 0.99 | 0.87–1.13 |
| Vaccinated before trigger test | ||||||
| 1–12 mos | 40 | 80.0 | 1.15 | 0.96–1.33 | 1.17 | 0.97–1.40 |
| 13–24 mos | 41 | 65.9 | 0.94 | 0.74–1.17 | 0.92 | 0.74–1.14 |
| 25–36 mos | 32 | 75.0 | 1.07 | 0.86–1.31 | 1.02 | 0.83–1.25 |
| 37–48 mos | 29 | 44.8 | 0.64 | 0.43–0.97 | 0.62 | 0.41–0.93 |
| >48 mos | 10 | 40.0 | 0.57 | 0.27–1.23 | 0.55 | 0.26–1.16 |
Abbreviations: PR, prevalence ratio; aPR, adjusted prevalence ratio; CIN2+, cervical intraepithelial neoplasia grades 2, 3 and adenocarcinoma in situ; AIS, adenocarcinoma in situ.
Adjusted for race, insurance, diagnosis grade, and catchment area.
Adjusted for race, insurance, catchment area.
4. Discussion
Within 6 years of HPV vaccine introduction in the United States, and despite persistently low vaccination coverage, evidence of vaccine impact on early outcomes is emerging, with reported reductions in vaccine-type HPV prevalence [17] and genital warts among adolescent females [22]. A few countries with high vaccine coverage have reported significant decreases in high grade cervical lesions post vaccine introduction [7]. In addition, studies from Australia, Denmark, and Scotland have demonstrated vaccine effectiveness against cervical abnormalities including CIN2+ through linkage of disease, screening, and immunization data from population-based registries [9–12]. Demonstrating vaccine impact on reducing the burden of cervical disease in the United States is more challenging, in large part because of concurrent secular changes in cervical cancer screening recommendations that were implemented independently of vaccine introduction. Monitoring trends in HPV types associated with cervical lesions can help identify vaccine impact on disease burden.
Preliminary data from earlier years of this project showed significant reductions in HPV 16/18-attributable CIN2+ lesions in women who received ≥1 vaccine dose at least 24 months before their trigger test [23]. Using a larger sample size over a longer surveillance period, the current analysis reveals larger declines in CIN2+ lesions attributable to HPV 16/18 in women with longer intervals between vaccination and trigger test, and demonstrates vaccine effectiveness against CIN3/AIS, lesions that are most likely to represent true preinvasive disease. Additionally, the time trend analysis shows significant reductions in HPV 16/18-attributable lesions between 2008 and 2012 among women who received ≥1 dose of HPV vaccine prior to their CIN2+ diagnosis.
The indirect cohort study design we used in this analysis has some limitations. Because there is no negative control group, this design can overestimate vaccine effectiveness if there is type replacement, a phenomenon whereby one or more HPV types may occupy the ecologic niche originally taken by types targeted by the vaccines. However, although theoretically possible, type replacement is unlikely given the extremely stable nature of HPV DNA viruses. Moreover, there has been no evidence of type replacement from HPV type prevalence studies in countries where high vaccination coverage has reduced the burden of vaccine targeted types. Conversely, this study design may underestimate vaccine effectiveness if the vaccines confer protection against non-targeted types. In this case, underestimation would be more likely although the quadrivalent vaccine has only shown minimal cross-protection against some non-vaccine oncogenic types in Phase III clinical trials [24]. Another potential limitation is the exclusion of a sizeable number of women for whom vaccination status was unavailable from the vaccine effectiveness estimates. Obtaining vaccination history is challenging given the incompleteness of adolescent vaccines in state-based immunization databases. However, we made efforts to collect this information from all available data sources. Despite limitations, these findings from a large population-based sample of women in the United States provide compelling evidence of real-world impact and effectiveness of vaccination on reducing cervical disease associated with targeted HPV types.
Acknowledgements
We gratefully acknowledge James Hadler, Jill Sharma, and Danielle Miller for their expert contribution in the planning and design and/or laboratory testing of the project.
Financial support
This work was supported by the U.S. Centers for Disease Control and Prevention cooperative agreement CIU01000307.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflict of interest
L. Niccolai was a consultant/advisory board member for Merck. All other authors declare no conflict of interest.
References
- [1].Munoz N, Castellsague X, de Gonzalez AB, Gissmann L. Chapter 1: HPV in the etiology of human cancer. Vaccine 2006;24(Suppl. 3). S3/1-10. [DOI] [PubMed] [Google Scholar]
- [2].Franco EL, Olsen J, Saracci R, Detels R. Epidemiology’s contributions to a Nobel Prize recognition. Epidemiology 2009;20:632–4. [DOI] [PubMed] [Google Scholar]
- [3].de Sanjose S, Quint WG, Alemany L, Geraets DT, Klaustermeier JE, Lloveras B, et al. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol 2010;11:1048–56. [DOI] [PubMed] [Google Scholar]
- [4].Serrano B, Alemany L, Tous S, Bruni L, Clifford GM, Weiss T, et al. Potential impact of a nine-valent vaccine in human papillomavirus related cervical disease. Infect Agents Cancer 2012;7:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].FUTURE I/II Study Group, Dillner J, Kjaer SK, Wheeler CM, Sigurdsson K, Iversen OE, et al. Four year efficacy of prophylactic human papillomavirus quadrivalent vaccine against low grade cervical, vulvar, and vaginal intraepithelial neoplasia and anogenital warts: randomised controlled trial. BMJ 2010;341:c3493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Lehtinen M, Paavonen J, Wheeler CM, Jaisamrarn U, Garland SM, Castellsague X, et al. Overall efficacy of HPV-16/18 AS04-adjuvanted vaccine against grade 3 or greater cervical intraepithelial neoplasia: 4-year end-of-study analysis of the randomised, double-blind PATRICIA trial. Lancet Oncol 2012;13:89–99. [DOI] [PubMed] [Google Scholar]
- [7].Hariri S, Markowitz LE, Dunne EF, Unger ER. Population impact of HPV vaccines: summary of early evidence. J Adolesc Health 2013;53:679–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Baldur-Felskov B, Dehlendorff C, Munk C, Kjaer SK. Early impact of human papillomavirus vaccination on cervical neoplasia – nationwide follow-up of young Danish women. J Natl Cancer Inst 2014;106:djt460. [DOI] [PubMed] [Google Scholar]
- [9].Gertig DM, Brotherton JM, Budd AC, Drennan K, Chappell G, Saville AM. Impact of a population-based HPV vaccination program on cervical abnormalities: a data linkage study. BMC Med 2013;11:227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Pollock KG, Kavanagh K, Potts A, Love J, Cuschieri K, Cubie H, et al. Reduction of low- and high-grade cervical abnormalities associated with high uptake of the HPV bivalent vaccine in Scotland. Br J Cancer 2014;111:1824–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Crowe E, Pandeya N, Brotherton JM, Dobson AJ, Kisely S, Lambert SB, et al. Effectiveness of quadrivalent human papillomavirus vaccine forthe prevention of cervical abnormalities: case-control study nested within a population based screening programme in Australia. BMJ 2014;348:g1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Baldur-Felskov B, Dehlendorff C, Junge J, Munk C, Kjaer SK. Incidence of cervical lesions in Danish women before and after implementation of a national HPV vaccination program. Cancer Causes Control 2014;25:915–22. [DOI] [PubMed] [Google Scholar]
- [13].Centers for Disease Control and Prevention. FDA licensure of bivalent human papillomavirus vaccine (HPV2, Cervarix) for use in females and updated HPV vaccination recommendations from the Advisory Committee on Immunization Practices (ACIP). MMWR 2010;59:626–9. [PubMed] [Google Scholar]
- [14].Stokley S, Jeyarajah J, Yankey D, Cano M, Gee J, Roark J, et al. Human papillomavirus vaccination coverage among adolescents, 2007–2013, and postlicensure vaccine safety monitoring, 2006–2014 – United States. MMWR 2014;63:620–4. [PMC free article] [PubMed] [Google Scholar]
- [15].Elam-Evans LD, Yankey D, Jeyarajah J, Singleton JA, Curtis RC, MacNeil J, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years – United States, 2013. MMWR 2014;63:625–33. [PMC free article] [PubMed] [Google Scholar]
- [16].Centers for Disease Control and Prevention. Noninfluenza vaccination coverage among adults – United States, 2011. MMWR 2013;62:66–72. [PMC free article] [PubMed] [Google Scholar]
- [17].Markowitz LE, Hariri S, Lin C, Dunne EF, Steinau M, McQuillan G, et al. Reduction in human papillomavirus (HPV) prevalence among young women following HPV vaccine introduction in the United States, National Health and Nutrition Examination Surveys, 2003–2010. J Infect Dis 2013;208:385–93. [DOI] [PubMed] [Google Scholar]
- [18].Centers for Disease Control and Prevention. Cervical cancer screening among women aged 18–30 years – United States, 2000–2010. MMWR 2013;61:1038–42. [PubMed] [Google Scholar]
- [19].Schiffman M, Castle PE,Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet 2007;370:890–907. [DOI] [PubMed] [Google Scholar]
- [20].Hariri S, Unger ER, Powell SE, Bauer HM, Bennett NM, Bloch KC, et al. The HPV vaccine impact monitoring project (HPV-IMPACT): assessing early evidence of vaccination impact on HPV-associated cervical cancer precursor lesions. Cancer Causes Control 2012;23:281–8. [DOI] [PubMed] [Google Scholar]
- [21].Broome CV, Facklam RR, Fraser DW. Pneumococcal disease after pneumococcal vaccination: an alternative method to estimate the efficacy of pneumococcal vaccine. N Engl J Med 1980;303:549–52. [DOI] [PubMed] [Google Scholar]
- [22].Flagg EW, Schwartz R, Weinstock H. Prevalence of anogenital warts among participants in private health plans in the United States, 2003–2010: potential impact of human papillomavirus vaccination. Am J Public Health 2013;103:1428–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Powell SE, Hariri S, Steinau M, Bauer HM, Bennett NM, Bloch KC, et al. Impact of human papillomavirus (HPV) vaccination on HPV 16/18-related prevalence in precancerous cervical lesions. Vaccine 2012;31:109–13. [DOI] [PubMed] [Google Scholar]
- [24].Brown DR, Kjaer SK, Sigurdsson K, Iversen OE, Hernandez-Avila M, Wheeler CM, et al. The impact of quadrivalent human papillomavirus (HPV; types 6, 11, 16, and 18) L1 virus-like particle vaccine on infection and disease due to oncogenic nonvaccine HPV types in generally HPV-naive women aged 16–26 years. J Infect Dis 2009;199:926–35. [DOI] [PubMed] [Google Scholar]


